To evaluate the performance of the most widely used SpA classification criteria in a Colombian group of patients with chronic low back pain.
MethodsWe assessed the ASAS and the European Spondyloarthropathy Study Group (ESSG) classification criteria in a group of 133 patients who attended consecutively over a period of six months at outpatient clinic of low back pain. All the patients were evaluated with the same protocol. The patients were divided into two groups according to the diagnosis. The diagnosis was compared with the diagnosis made by a expert rheumatologist blinded to patient information.
Results81 patients with SpA and 52 with other diagnoses were included. There were no differences in age and age of onset of symptoms between the two groups. The SpA group included 55 males and more common clinical findings were: enthesitis, arthritis, sacroiliitis, HLA-B27-positive, previous infection, and dactylitis. The sensitivity and specificity of criteria were: ASAS criteria 96% of sensibility and 80% of specificity, and ESSG criteria 95% and 100% respectively.
The agreement between the classification criteria and the diagnosis established by the rheumatologist showed a Cohen's kappa index of 0.938 for ESSG criteria (95% CI: 0.877–0.998) and 0.790 for the ASAS criteria (95% CI: 0.682–0.898).
ConclusionIn a Colombian group of SpA patients, the new ASAS classification criteria have a good concordance with clinical diagnosis but are not superior to the ESSG criteria.
Evaluar el acuerdo entre los criterios de clasificación para SpA y el diagnóstico de un experto reumatólogo en un grupo de pacientes con dolor lumbar.
MétodosSe evaluó el comportamiento de los criterios de ASAS y del ESSG en 133 pacientes que acudieron de forma consecutiva durante seis meses a la clínica ambulatoria de dolor lumbar. Todos los pacientes se evaluaron con el mismo protocolo. Los pacientes fueron divididos en dos grupos de acuerdo con el diagnóstico. Posteriormente se estableció del acuerdo diagnóstico con el de un experto reumatólogo ciego a la información previa de los pacientes.
Resultados81 pacientes con SpA y 52 con otros diagnósticos fueron incluidos. No hubo diferencias en la edad y la edad de aparición de los síntomas. El grupo SpA incluyó a 55 varones y los hallazgos más comunes fueron: entesitis, artritis, sacroileítis, infección previa, HLA-B27, y dactilitis. La sensibilidad y especificidad de los criterios fueron: ASAS 96% de sensibilidad y 80% de especificidad, y ESSG 95% y 100% respectivamente.
El acuerdo entre los criterios de clasificación y el diagnóstico del reumatólogo mostró un índice kappa de 0,938 con criterios ESSG (IC del 95%: 0,877–0,998) y 0,790 para los criterios ASAS (IC del 95%: 0,682–0,898).
ConclusiónEn un grupo de pacientes colombianos SpA, los nuevos criterios de clasificación ASAS tienen una buena concordancia con el diagnóstico clínico, pero no son superiores a los criterios ESSG.
Spondyloarthritis (SpA) are a group of chronic inflammatory disorders that share clinical, radiological, HLA-B27 association, positive family history and pathophysiological characteristics. SpA affect approximately 1.5% of the general population. Predominantly, SpA begins in individuals younger than 45 years and clinically compromises the axial spine, peripheral joints, tendons and ligament insertions (entheses), having also extra-musculoskeletal manifestations in the skin, mucosa, gut and the eyes, producing impairment of functional capacity.1 The incidence of SpA in the general population is related to the prevalence of HLA-B27. This explains why SpA is most commonly diagnosed in Anglo-Saxon populations where the prevalence of HLA-B27 could reach up to 14%.2
One of the clinical manifestations present in all stages of the disease, is inflammatory back pain (IBP).3 In clinical practice is difficult to differentiate between the mechanical or inflammatory origin of pain. Traditionally clinical and epidemiological studies have used classification criteria to identify the two groups of patients. The frequency of inflammatory back pain has been estimated at 5% of all patients with chronic low back pain (CLBP).4 At the same time, the CLBP is the most common cause of disability in men between 15 and 45 years of age and it is important to differentiate between the sources of pain given the prognostic and therapeutic implications.5
In the last 30 years, several classification criteria for SpA have attempted to include the early stages as well as the undifferentiated forms of the disease (uSpA).6–10 According to the European Spondyloarthropathy Study Group (ESSG) criteria, SpA has been traditionally classified as follows: ankylosing spondylitis (AS), reactive arthritis (ReA), undifferentiated spondyloarthritis (uSpA), psoriatic arthritis (PsA), and arthritis associated with inflammatory bowel disease (IBD).7
The Assessment of Spondyloarthritis International Society (ASAS) proposes a new classification criteria that includes two sets; axial and peripheral according to the prevalence of symptoms. The new ASAS criteria include the use of MRI of the sacroiliac joints and HLA-B27 as a fundamental part of the diagnosis.8,10
There is no gold standard for the diagnosis of SpA because of the heterogeneity of the musculoskeletal symptoms.11 Sometimes epidemiological classification criteria are used as a tool in the diagnosis of these diseases with acceptable clinical performance.12 However, the results may vary depending on the prevalence of the disease. In the Latin American countries uSpA corresponds to the most common form of presentation, with predominance of a mixture of axial and peripheral symptoms, low frequency of HLA-B27 and with less radiological (joint) damage of the axial skeleton.13–15 Other HLA molecules have been implicated as responsible for this variation in clinical presentation. In routine clinical practice, the diagnostic decision depends exclusively on the experience of the rheumatologist who assesses the patient.16
The objective of this study is to establish an agreement between the most widely used classification criteria and a rheumatologist's diagnosis in a group of Colombian patients.
Materials and methodsParticipants and clinical assessment of patientsA total of 133 patients, >18 years, with past or current history of CLBP (≥3 months) occurring before age 45 years, who attended consecutively over a period of six months at outpatient clinic of CLBP were included in the study. These patients were referred by other medical specialties: general practitioner, family medicine, internal medicine, orthopedics, rehabilitation medicine and neurosurgery. All patients underwent in the same diagnostic algorithm that included the use of a structured questionnaire completed by the rheumatologist from the available data at the time of visit with socio-demographic information; history related to pain: date of the onset, trigger, morning stiffness, insidious onset, improved with the exercise, worsening with rest, awakening at night because of pain, good response to no steroidal anti-inflammatory drugs, degree of disability by pain, cervical and thoracic spine compromise, button pain; history of arthritis, enthesitis, dactilitys; personal and family history related to the SpA: infections, uveitis, psoriasis or inflammatory bowel disease. All patients were applied specific instruments related to functional status and activity of the SpA: BASFI,17 BASDAI,18 visual analog scale (VAS) of pain and disease activity. For the physical examination ASAS recommendations were followed and included: occiput to wall distance, thoracic expansibility, Shober test, painful enthesis account by Mander's Index and tender and swollen joints account on a total of 44. HLA typing, PCR and VSG.19
ImagingAll patients underwent MRI of sacroiliac joints using contrast agents and fat suppression techniques (projections in T1, T2 and STIR), radiographs of the pelvis. All images were evaluated by a radiologist with experience in SpA who remained blinded to the clinical information of the patients. Sacroiliitis by images was defined by New York and ASAS criteria for X-ray and MRI respectively. Pre-radiographic sacroiliitis in cases of normal pelvic X-ray with sacroiliitis evidence by MRI.20
Diagnosis and classification of patientsFinally, an expert rheumatologist in the field of SpA evaluated independently the clinical and laboratory findings of the patients and divided the patients into the two groups: SpA and none SPA. No SpA patients were diagnosed with different pathologies: osteoarthritis, postural syndrome, rheumatoid arthritis and fibromyalgia SpA. Using the expert opinion as gold standard for diagnosis of SpA, the operation (sensitivity and specificity) of the EGSS and ASAS criteria were established. In addition, the degree of agreement between the ESSG and the ASAS classification criteria with clinical diagnosis, was calculated using the kappa index.
StatisticsData analysis was performed using Stata 10.0. Measures of central tendency and dispersion for the continuous variables were used for data presentation. Frequency and percentage values were used for the categorical variables. The Student's t-test and the Kruskal–Wallis test were used to compare the continuous variables. For the nominal variables, the chi-squared test was used, and Fisher's exact test was used if necessary. In this study, p<0.05 was considered statistically significant, and 95% confidence intervals (CIs) were calculated.
Ethics approvalThe study followed the norms established by the Helsinki Declaration, The Guidelines for Good Clinical Practice, and the Resolution 8430 (1993) of the Colombian Ministry for Social Protection. Moreover, was reviewed and approved by the Ethics Committees of the University of La Sabana and the Central Military Hospital. Each patient signed an informed consent form, and confidentiality was strictly maintained.
ResultsA total of 133 patients were included, 81 patients with SpA and 52 none SpA. Of SpA patients, 33 (40.7%) had AS, 32 (39.5%) uSpA and 16 (19.8%) ReA. 55 (67.9%) were males, with a ratio male/female of 2:1. The more frequent clinical manifestations were IBP, and enthesopathy. In none SpA patients, 24 had postural syndrome, 14 fibromyalgia, 12 osteoarthritis and two rheumatoid arthritis.
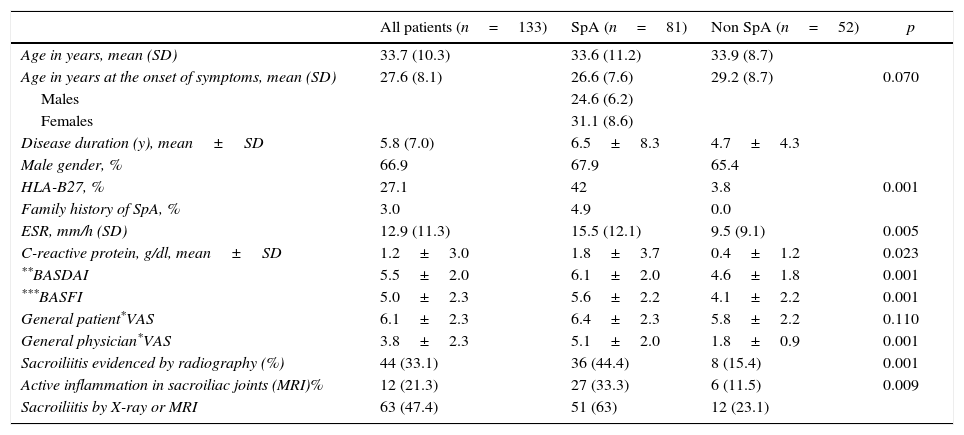
There was no significant difference between the two groups of patients in age at the onset of symptoms, disease duration, age at the time of evaluation and indices of function and activity of disease. HLA-B27 was present in 42% of the patients with SpA (57.6% in AS, 18.8% in uSpA and 56.3% in ReA) and only in 3.8% of the patients with other diseases (p<0.001). In terms of clinical characteristics, there were significant differences in all variables. Arthritis and uveitis were more common in SpA patients and were associated with HLA-B27 allele. Blood markers of inflammation were more elevated in patients with SpA than in controls (p=0.005). IBP, enthesopathy, blood and radiological evidence of sacroiliitis, were the variables with more significance in SpA (Table 1).
Clinical characteristics of the evaluated patients.
| All patients (n=133) | SpA (n=81) | Non SpA (n=52) | p | |
|---|---|---|---|---|
| Age in years, mean (SD) | 33.7 (10.3) | 33.6 (11.2) | 33.9 (8.7) | |
| Age in years at the onset of symptoms, mean (SD) | 27.6 (8.1) | 26.6 (7.6) | 29.2 (8.7) | 0.070 |
| Males | 24.6 (6.2) | |||
| Females | 31.1 (8.6) | |||
| Disease duration (y), mean±SD | 5.8 (7.0) | 6.5±8.3 | 4.7±4.3 | |
| Male gender, % | 66.9 | 67.9 | 65.4 | |
| HLA-B27, % | 27.1 | 42 | 3.8 | 0.001 |
| Family history of SpA, % | 3.0 | 4.9 | 0.0 | |
| ESR, mm/h (SD) | 12.9 (11.3) | 15.5 (12.1) | 9.5 (9.1) | 0.005 |
| C-reactive protein, g/dl, mean±SD | 1.2±3.0 | 1.8±3.7 | 0.4±1.2 | 0.023 |
| **BASDAI | 5.5±2.0 | 6.1±2.0 | 4.6±1.8 | 0.001 |
| ***BASFI | 5.0±2.3 | 5.6±2.2 | 4.1±2.2 | 0.001 |
| General patient*VAS | 6.1±2.3 | 6.4±2.3 | 5.8±2.2 | 0.110 |
| General physician*VAS | 3.8±2.3 | 5.1±2.0 | 1.8±0.9 | 0.001 |
| Sacroiliitis evidenced by radiography (%) | 44 (33.1) | 36 (44.4) | 8 (15.4) | 0.001 |
| Active inflammation in sacroiliac joints (MRI)% | 12 (21.3) | 27 (33.3) | 6 (11.5) | 0.009 |
| Sacroiliitis by X-ray or MRI | 63 (47.4) | 51 (63) | 12 (23.1) |
In the patients with SpA, the pelvic X-ray showed evidence of sacroiliitis in 44%, compared with 43% with MRI. Sacroiliitis in the X-ray was strongly correlated with SpA 44.4% vs 15.4% (p=0.001) and was present in 33 (100%) of the patients with AS, 2 patients with uSpA (6.25%) and 1 patient with ReA (6.25%) and 8 (15.4%) non-SpA patients. The MRI was positive in (35/81) 43.2% of the SpA patients and (6/52) 11.5% of non-SpA patients (p=0.000). MRI provided evidence of pre-radiographic sacroiliitis in 10 of the 30 patients with uSpA (33.3%) and 5 of the 15 patients with ReA (33.3%). Furthermore, the MRI showed pre-radiographic sacroiliitis in 6 patients in the control group, of whom only 1 patient had similar radiographical findings (Table 1).
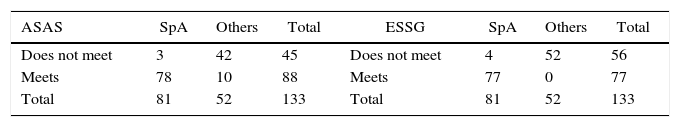
Performance of the ESSG and ASAS classification criteriaWhen we analyzed the performance of the ESSG criteria in this population, we found that 95% of the SpA patients met the criteria. None of the non-SpA patients met the criteria. The results also showed that 96.3% of the SpA patients and 19.2% of the non-SpA patients met the new ASAS criteria. ASAS criteria have 96% of sensibility and 80% of specificity, and ESSG criteria 95% and 100%, respectively.
When we analyzed the agreement of the classification criteria with the diagnosis established by the rheumatologist, we found a Cohen's kappa index of 0.938 for the ESSG criteria (95% CI: 0.877–0.998) and 0.790 for the ASAS criteria (95% CI: 0.682–0.898) (Table 2).
DiscussionThe population described here is a sample of patients who suffer from different forms of SpA. All of the patients were recruited during outpatient consultations at the Rheumatology Department of one national referral hospitals for highly complex diseases. These patients were referred to the Department after having been evaluated by other medical specialties (Orthopedics, Rehabilitation Medicine, Neurosurgery, Ophthalmology and Internal Medicine), when SpA was established as a possible diagnosis due to the presence of chronic low back pain.
As described in other populations, the predominant symptoms among the SpA patients were lower back pain, arthritis and enthesopathy. Other symptoms such as dactylitis and uveitis were observed in the same proportions reported in previous studies.9,21 In the non-SpA patients, the most common symptoms were chronic lower back pain and gluteal pain. The time of disease progression was lower in our group of patients than that reported by Feldtkeller in 2003 (6.5±8.3 years vs. 8.8±7.6 years, respectively).22
HLA-B27 was present in a smaller proportion of our patients (42%) compared with other populations. Although this lower prevalence seems to be the trend in current publications, the lower prevalence may reflect the racial composition of our population and the relatively high number of patients with undifferentiated and reactive forms of the disease.21 In this study, 28 patients fulfilled the new ASAS criteria with axial involvement: 24 patients met the radiological requirement and 15 patients met the requirement contingent on a positive HLA-B27 test (11 patients met both requirements; thus, 4 patients were only positive for HLA-B27, and 13 patients only had images showing sacroiliitis). This difference is an important detail because it appears that imaging offered better results for patient classification than HLA-B27 characterization, with a better performance of plain radiography for sacroiliitis diagnosis than MRI in our study. However, in this group of patients, HLA-B27 positivity was strongly associated with the clinical markers traditionally considered to be associated with more severe forms of the disease (AS, uveitis and arthritis).
As reported by Weber, non-SpA patients may have positive results in the MRI of the sacroiliac joints and spine. Healthy controls can have isolated foci of hyperintensity on STIR (bone pseudo-edema) with a frequency close to 27%.23,24 The other hand, arthrosis is common condition in patients over 40 years old. It can cause unilateral or bilateral, symmetrical or asymmetrical sacroiliac joint inflammation.25 This conditions could explain why several of our patients in whom SpA was ruled out had positive MRI results (n=6) and justifies the increase in the number of false positives that resulted from using this set of criteria. When the sacroiliac joint MRI results were combined with the ESSG criteria, 1 additional patient met the requirements for SpA. These data may justify reconsidering the use of this diagnostic method in patients with a diagnosis of uSpA because the other clinical and laboratory criteria can provide the necessary diagnostic information. This uncommon pre-radiographic sacroiliitis suggests a better prognosis in our population, with less likelihood of progression to AS, which is the more severe form of SpA. However, this progression must be examined using a different study design in larger patient populations.
Nevertheless, after reviewing the most recent literature on this regard Banegas Illescas and collaborators conclude that the ASAS criteria have limitations concerning the diagnostic and prognostic utility of MRI in these patients. Firstly, in absence of bone edema or osteitis the MRI-identified structural lesions are not diagnostic of sacroilitis. This exclusion is contradictory due to the fact that the other radiological marker of sacroiliitis is based on structural changes seen on the simple X-ray according to New York new modified criteria despite the great inter-observer variability.26–28 Several trials have shown that MRI is not only capable of finding structural lesions before they can be seen on the X-ray without active inflammatory lesions,24,29 but it is also capable of increasing its diagnostic sensibility from 67% to 81%, when erosions are analyzed besides bone edema without changes in specificity (88%).24
Considering these observations, the agreement between the classification criteria and the clinical diagnosis was good in this group of patients and also highlighted a better interpretation of the ESSG criteria.
The results obtained in this study should be analyzed with the understanding that there is a higher proportion of reactive and undifferentiated forms of SpA in Latin American patients than in Anglo-Saxon populations. In our populations, peripheral manifestations are predominant compared with axial involvement, and the prevalence of HLA-B27 is low as a result of miscegenation.
The patients who were evaluated and participated in this study were referred to the SpA clinic after an outpatient consultation at the Department of Rheumatology of one tertiary care hospital that are the national referral center for a population of over half a million people. This referral creates a filter so that the patients included in this study represented the most severe forms of the disease. This meant that only patients with more complex were evaluated by the rheumatologist, causing a selection bias. For this reason, the number of patients with SpA is significantly higher than the other diseases. However, in the context of the objective of the present study, the sample size, allowed the agreement between the clinical diagnosis in real life of outpatient care of patients and the classification criteria for SpA used most frequently. This explains why the performance of the classification criteria is greater than previously reported in open community.30–32 Therefore, it is necessary to study in Latin-American countries which really is the performance ESSG and ASAS criteria, where the percentage of patients with HLA-B27 positive and axial compromise is smaller compared with Anglo-Saxon populations.33,34
In conclusion, the ESSG and ASAS classification criteria and the clinical diagnosis made by expert rheumatologists were well correlated in the Colombian population. However, in the present study, the ESSG criteria showed a higher degree of agreement with clinical diagnosis, which should be analyzed in other Latin American populations.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FinancialSupported by the University of La Sabana. No financial support or benefits from commercial sources.
Conflict of interestNot any additional conflict of interest exist with regard to this work.