Registries are essential to keep track of inflammatory bowel disease (IBD) and related arthritis epidemiology, and to provide better care to patients. In Colombia, the health ministry has adopted a tool, SISPRO, to gather all information coming from the whole health system structure. Given that the information collected from SISPRO is available for anyone, it provides an opportunity to get an insight into health topics.
ObjectivesThe data collected from SISPRO were used to analyse the prevalence and specific characteristics of patients with IBD and related arthritis registered between 2012 and 2016.
MethodsThis is a descriptive epidemiological study using the International Statistical Classification of Diseases and Related Health Problem as keywords related to IBD and related arthritis during the analysis of SISPRO data.
ResultsNational records report 42,647 patients with a diagnosis of IBD for an estimated prevalence of 87/100,000 subjects, being more frequent in women. The prevalence of Crohn’s disease was 17/100,000 subjects, and 113/100,000 subjects for ulcerative colitis. The prevalence of arthritis related to inflammatory bowel disease was 5/100,000 subjects.
ConclusionsThis is the first study that describes the demographic characteristics of IBD in Colombia. This study is in accordance with that previously described in the available literature, which supports the theory about increasing global prevalence of IBD. Also, there are some differences between Colombian regions, which could be related to environmental factors and ancestry, which deserve further study.
Los registros son esenciales para seguir la epidemiología de la enfermedad inflamatoria intestinal (EII) y el compromiso articular asociado y brindar mejor atención a los pacientes. En Colombia, el Ministerio de Salud y de la Protección Social utiliza la herramienta SISPRO para recolectar información del sistema de salud, la cual es de dominio público y amerita un análisis como el realizado en este trabajo.
ObjetivosUtilizando los datos de SISPRO se realizó un análisis de la prevalencia y las características de los pacientes con EII y artritis relacionada, con los registros correspondientes a los años 2012 a 2016.
MétodosEstudio descriptivo de corte transversal en el que se tomaron los datos de SISPRO, utilizando como palabras clave los diagnósticos del manual internacional de enfermedades relacionados con el diagnóstico de EII y la artritis asociada.
ResultadosSe documentaron 42.647 individuos con diagnóstico de EII, con una prevalencia estimada de 87 casos por 100.000 habitantes, más frecuente en mujeres. La prevalencia de la enfermedad de Crohn fue de 17 por 100.000 habitantes y la colitis ulcerativa de 113 por 100.000 habitantes. La prevalencia del compromiso articular asociado a EII fue de 5 por 100.000 habitantes.
ConclusiónEste es el primer estudio que describe las características demográficas de la EII en Colombia. Los resultados son acordes con lo reportado en la literatura mundial y la teoría del aumento de la prevalencia de la EII. Así mismo, existen diferencias entre regiones que pueden estar relacionadas con ancestría y factores medioambientales que requieren estudios complementarios.
The term inflammatory bowel disease (IBD) refers to a group of chronic inflammatory diseases referred to as ulcerative colitis (UC) and Crohn’s disease (CD), both of unknown etiology. Genetic and environmental factors have been associated with the pathogenesis of the disease1. These entities are defined in accordance with clinical, radiological, endoscopic and histological criteria. Both are chronic with outbreaks of inflammatory activity2, with a broad range of systemic manifestations such as articular involvement (axial, enthesis-related or peripheral joints), soft tissue, ocular, cutaneous, and hepatic involvement, inter alia. There are also gastrointestinal manifestations including recurrent abdominal pain, weight loss and chronic diarrhea3–5.
In Colombia there are no studies describing the epidemiology of IBD. Actually, there are only 2 studies conducted in populations of Medellín6 and Cartagena4, which are case descriptions including 202 and 29 patients, respectively; these cases show that UC is more frequent than CD in these populations.
This paper was developed based on the data from the Ministry of Health and Social Protection, to analyze the prevalence and the characteristics of patients with IBD and related arthritis, using the records from 2012 to 2016.
Material and methodThe Ministry of Health and Social Protection of Colombia has developed a tool for the collection and storage of information called SISPRO (Comprehensive System of Information on Social Protection). SISPRO comprises 4 components: health, pensions, occupational hazards and social promotion. This is the first system in which basic and minimum data of the General Social Security System are stored and processed por management, regulatory and control purposes. The source of this information is the Individual Registry of Delivery of Services (RIPS, for its Spanish acronym). The information contained in these databases is public. The data for this study were collected accessing the dynamic tables which are available on line from the Ministry of Health and Social Protection. The information was analyzed for the period from January 1st 2012 and December 31st of 2016, using the codes of the international classification of diseases (ICD-10) for IDB associated arthropathy (M074–M076) and for UC and CD (K500, K501, K508–K513, K515, K518, K519); different variables were reported, including sex, type of insurance and distribution into five-year groups in accordance with the official forecasts of the National Administrative Department of Statistics (DANE), based on population forecasts from the national census in 20057.
To estimate the prevalence in Colombia, a 5-year group analysis was conducted of each of the 32 departments during the 5-year period analyzed. A description of the data obtained with measurements of frequencies and percentage for qualitative variables was conducted.
The paper was reviewed and approved by the Central Committee of Research and Institutional Ethics of the School of Medicine of the Pontificia Universidad Javeriana, which fully endorses the ethical and scientific principles of the Declaration of Helsinki, version 64 of the General Assembly (Fortaleza, Brazil), October 2013.
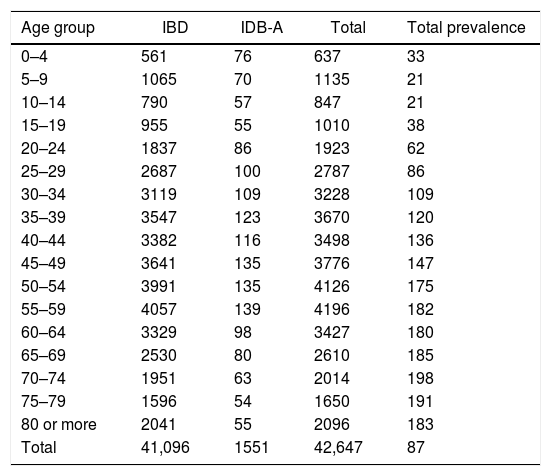
ResultsA total of 42,647 cases were identified (“persons cared for”) with a principal diagnosis of IBD, representing a prevalence of 86 cases per 100,000 inhabitants; a higher prevalence of IBD was also identified in females (58% of the cases), with a female–male ratio of 1.39:1. With the analysis of the IBD prevalence per 5-year groups, a progressive increase was noted in the prevalence starting with the 5-year group of 30–34 years, up to the highest prevalence in the age group between 70 to 74 years old (Table 1). Due to the characteristics of the registry, it is not possible to determine the incidence rate or the time of evolution of the disease. A prevalence for CD was of 17 per 100,000 inhabitants, and for UC of 113 per 100,000 inhabitants. A higher prevalence of these two diseases was documented in females (57.9% and 57.7%, respectively).
Patients receiving care between 2012 and 2016, with a principal diagnosis of inflammatory bowel disease, according to age group.
| Age group | IBD | IDB-A | Total | Total prevalence |
|---|---|---|---|---|
| 0–4 | 561 | 76 | 637 | 33 |
| 5–9 | 1065 | 70 | 1135 | 21 |
| 10–14 | 790 | 57 | 847 | 21 |
| 15–19 | 955 | 55 | 1010 | 38 |
| 20–24 | 1837 | 86 | 1923 | 62 |
| 25–29 | 2687 | 100 | 2787 | 86 |
| 30–34 | 3119 | 109 | 3228 | 109 |
| 35–39 | 3547 | 123 | 3670 | 120 |
| 40–44 | 3382 | 116 | 3498 | 136 |
| 45–49 | 3641 | 135 | 3776 | 147 |
| 50–54 | 3991 | 135 | 4126 | 175 |
| 55–59 | 4057 | 139 | 4196 | 182 |
| 60–64 | 3329 | 98 | 3427 | 180 |
| 65–69 | 2530 | 80 | 2610 | 185 |
| 70–74 | 1951 | 63 | 2014 | 198 |
| 75–79 | 1596 | 54 | 1650 | 191 |
| 80 or more | 2041 | 55 | 2096 | 183 |
| Total | 41,096 | 1551 | 42,647 | 87 |
The column of total patients corresponds to the number of people receiving care at some point during the five-year period. The prevalence is estimated using the mean population for the period as denominator ×100,000 inhabitants.
IDB-A: IDB-related arthropathy; IBD: inflammatory bowel disease.
Assessing the diagnosis of IBD-related articular involvement, in accordance with the diagnoses in RIPS, the prevalence in the general population was of 5 per 100,000 inhabitants, with a higher proportion of female patients (64%). Through a differentiated analysis per each of the 2 types of IBD, the UC-associated joint involvement showed a prevalence of 3 per 100,000 inhabitants and the CD-associated articular involvement showed a prevalence of 1 per 100,000 inhabitants, also with a higher proportion of females (62% in UC and 65% in CD). The analysis of the proportion of patients with IBD and associated articular involvement indicated that this type of extraintestinal compromise is present in 3.77% of the cases.
Analyzing the type of coverage in accordance with the General Health System of Social Security (SGSSS), most of the patients with IBD are part of the contributive regimen (59.4%), followed by the subsidized regimen (32.9%), complementary insurance plans (4.5%) and special regimens (0.76%).
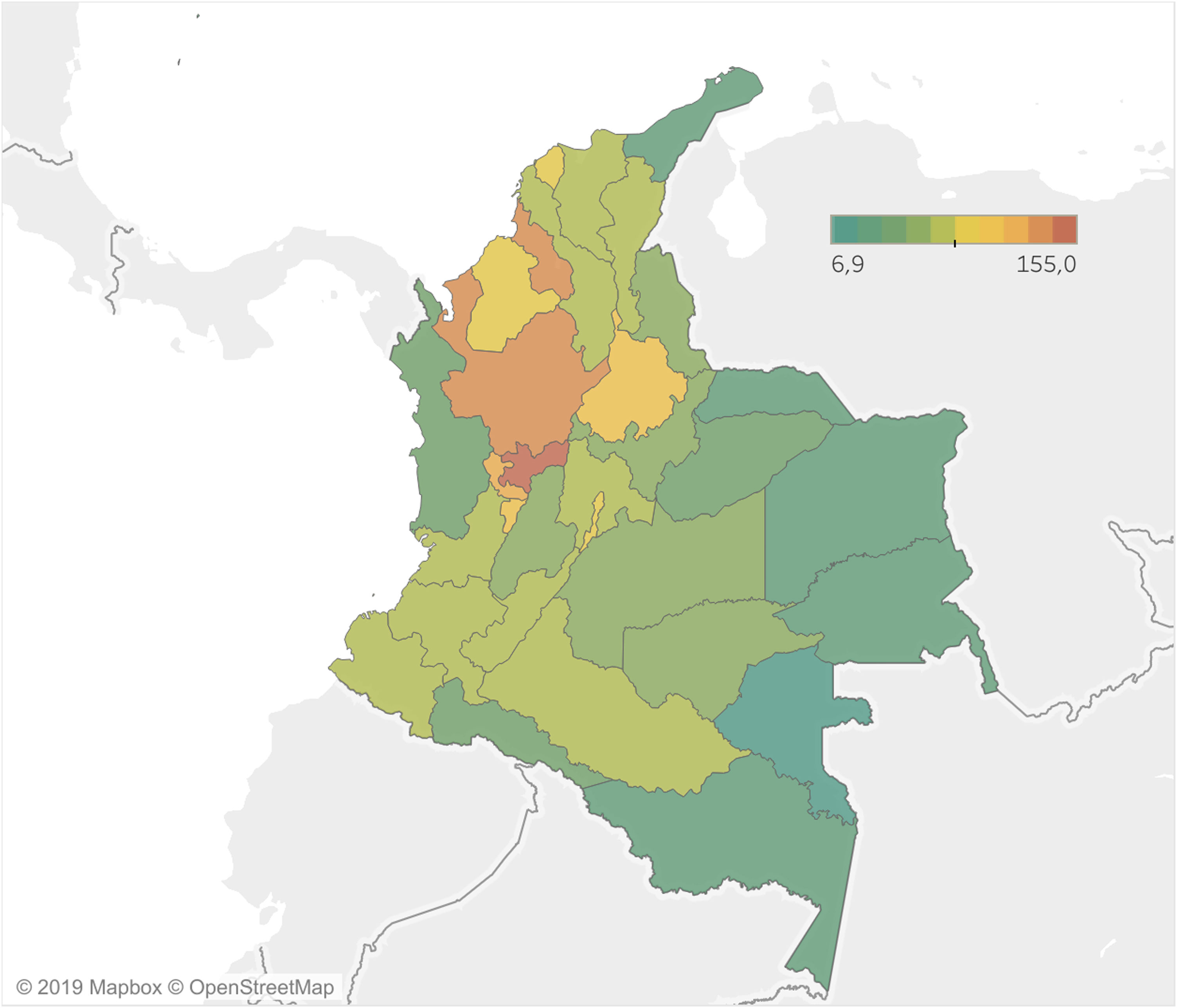
In terms of the distribution of IBD by geographical regions (States), the prevalence ranged from 7 to 155.0 per 100,000 inhabitants (Fig. 1). It was worth noting that the areas with the highest prevalence are concentrated in the Viejo Caldas region (Caldas, Risaralda and Quindío) and Antioquia, which share a similar ancestry in Colombia. The States near the Orinoco region (Arauca, Casanare, Meta and Vichada) and the Amazon region (Amazonas, Putumayo, Guainía, Guaviare and Vaupés) are the States with the lowest prevalence of the disease, but this may be attributed to a lower population density and reduced urban development. The largest number of patients registered are in Antioquia, followed by Bogotá D. C. and Valle del Cauca.
DiscussionThis is the first study conducted in Colombia that determines the prevalence of IDB, and its geographical distribution to be able to compare the data against world statistics, using current official statistics. The most significant contribution of this study is the identification of the population characteristics for a group of diseases characterized by demanding hospital services, surgery and biotechnological therapies8. With regards to the Colombian studies, in Cartagena 77% of the patients had UC and 23% CD, of which 69% were females. This information is consistent with the higher prevalence of UC in Colombia and the larger proportion of females identified in this study4.
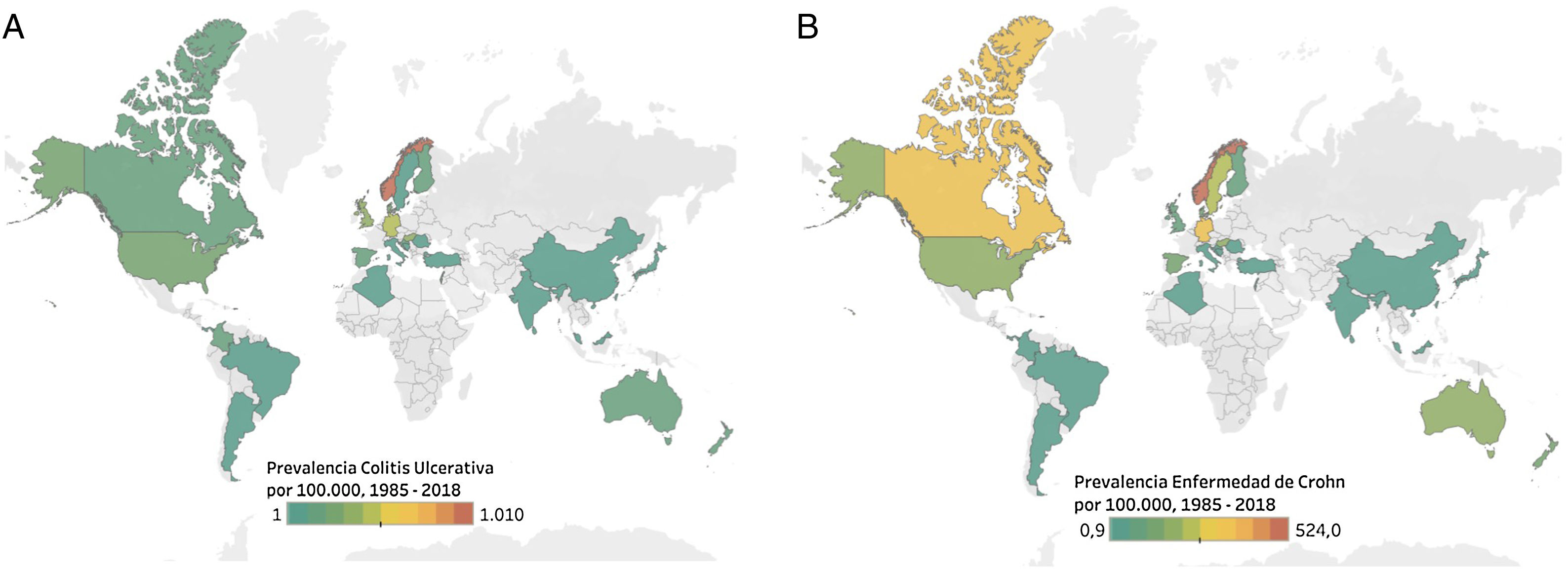
The prevalence of IBD varies in accordance with the geographical area; however, the hypothesis of a change in the prevalence and incidence has been proven based on studies like the one by Molodecky et al., who showed that the highest rates are found in the most developed nations, such as the Scandinavian countries, northern European countries and North America (Fig. 2)1,8–10. The prevalence is increasing in the less developed countries as they become more industrialized; this points to urban development as a potential risk factor. Fig. 2 illustrates the estimated prevalence in research projects conducted in different countries1,10–12.
Prevalence of inflammatory bowel disease in the world. A) Crohn’s disease. B) ulcerative colitis1,8,10–14,19.
When comparing the statistics obtained with the data from other Latin American populations, the conclusion is that there are few studies that reveal the behavior of this disease over the last few years. A study conducted in Puerto Rico reported a prevalence of CD of 41.4 per 100,000 inhabitants for the year 2000 and of 62.2 cases per every 100,000 inhabitants of UC13. Studies conducted in Panama between the 80 s and 90 s reported a prevalence of 1.2 cases per 100,000 inhabitants for UC, and in Argentina the prevalence reported for UC was of 2.2 cases per 100,000 inhabitants14. There are few studies available in Colombia: a case series published in 1991 presented 108 cases of IBD collected over 22 years, of which 98 were UC and 10 were CD15. The last two studies focused on populations in Cartagena4 and Medellín6, with series of 26 and 202 cases, respectively.
In most of the studies the diagnosis of IBD is usually done at a young age. In the case of UC, the most common age of presentation ranges from 30 to 40 years, whilst for CD it is 5–10 years earlier, with a range from 20 to 30 years8. Although, because of the nature of the information in our study it is not possible to determine the incidence, nor the age of presentation, it is striking to find a higher concentration of patients older than 30 years, with a maximum between 70 and 74 years old; this could be related to the overall increase in the life expectancy of the population worldwide. Consequently, due to the chronic nature of IBD and its low mortality, there is a larger number of patients in the older age groups.
The most frequent extraintestinal manifestation is articular involvement with 20.3%6. This extraintestinal manifestations are described in the literature as peripheral arthropathies, affecting between 5–10% in UC and 10–20% in CD; axial involvement may be around 3–5%16, with a heterogeneous presentation depending on the activity of the IBD. There are other extraintestinal manifestations with figures between 20–30%17, more often associated with CD. The research conducted in Medellín showed that 27.7% of the patients with IBD have extraintestinal manifestations, and these were present in 25.8% of the patients with UC and in 40.6% of the patients with CD. This figures are above the numbers described for other populations. The most frequent extraintestinal manifestation was articular involvement (20.3%), and it was more significant in patients with CD6. The data from this study show a lower proportion of articular involvement in patients with IBD, which is different from what is documented in the literature18,19.
The above statement is one of the limitations of the study, since under-registration or misregistration by the physicians when entering the code CIE 10 in the medical records is considered the probable cause. Another weakness of the study, given the characteristics of the registry, is the impossibility to estimate the incidence, the time of evolution of the disease, the severity, the demand for specialized services associated with the disease and mortality. Now then, the source of the information used is the database of the Ministry of Health of the Colombian government; this information is the basis for demographic and epidemiological analysis of the population and for forecasting the care delivered to patients with IBD in our country.
ConclusionsThis is the first study that describes the prevalence of IBD in Colombia, a condition that requires specialized, high-cost therapy. This study shows that IBD does not have a homogeneous distribution in a territory that is wide, with different communities in which ancestry and the environment converge to give rise to this type of pathologies. The prevalence of IBD is similar to what is reported in the literature in other regions, as is higher to the figures reported in similar studies in Latin America. This paper paves the way for future research using different methodologies that allow for a more accurate estimate of the prevalence of IBD and its association to spondyloarthritis in Colombia.
FinancingNo specific grants from the public sector, commercial or non-profit agencies were received for this research project.
Conflicts of interestThe authors have no conflicts of interest to disclose with regards to this paper.
Please cite this article as: Fernández-Ávila DG, Bernal-Macías S, Parra-Izquierdo V, Rincón-Riaño DN, Gutiérrez JM, Rossellie D. Prevalencia en Colombia de la enfermedad inflamatoria intestinal y el compromiso articular asociado, según información del Sistema Integral de Información de la Protección Social. Rev Colomb Reumatol. 2020;27:3–8.