: Fibromyalgia (FM) is a chronic pain condition that represents a public health problem. It greatly impacts quality of life and affects the psychosocial dimension beyond physical aspects. However, there are insufficient studies aimed at determining the suffering levels of this population and its related factors to propose more comprehensive interventions.
ObjectiveTo determine the levels of suffering and its associated factors in patients with FM treated at the Colombian Institute of Pain.
MethodsA quantitative, analytical observational, and cross-sectional study with a correlational design was carried out. Convenience sampling was used. Variables assessed included levels of suffering (PRISM), FM impact on quality of life (FIQR), loneliness (UCLA), anxiety and depression (HADS), and vital stress (Vital Events Questionnaire). Descriptive and correlational statistics were obtained.
ResultsThere were sixty-two participants, 96.8% were women. Seventy-five percent manifested moderate to severe suffering, 62.9% had clinical indicators of loneliness, 75% clinically significant anxiety, and 25.8% clinically significant depression. Also, they reported a mean of 10 stressful vital events. A direct and significant association between suffering and impact on quality of life was found. This impact on quality of life was also significantly correlated with loneliness, anxiety, and depression. Vital stress was also significantly related to loneliness and anxiety. Although statistically significant, most correlations were moderate.
ConclusionsPatients with FM experience relevant levels of suffering and impact on their quality of life. This impact is directly related with psychosocial factors beyond the well-known anxiety and depression. These results help visualize the intense suffering faced by this population and indicate the relevance of examining more deeply issues such as loneliness and vital stress.
La fibromialgia (FM) es una enfermedad dolorosa, de curso crónico, que representa un problema de salud pública. Impacta significativamente en la calidad de vida y afecta, más allá de la esfera física, la psicosocial. Sin embargo, son escasos los estudios que determinen los niveles de sufrimiento y sus factores relacionados, con miras a generar propuestas de intervención más integrales.
ObjetivoDeterminar los niveles de sufrimiento y los factores psicosociales asociados en pacientes con FM atendidos en una institución de Medellín, Colombia.
MétodoSe realizó un estudio cuantitativo, observacional, analítico, transversal y con diseño correlacional, empleando un muestreo por conveniencia. Se evaluó el grado de sufrimiento (PRISM), el impacto de la fibromialgia (FIQR), la soledad (UCLA), la ansiedad y la depresión (HADS), así como los eventos vitales estresantes (Cuestionario de Sucesos Vitales). Se obtuvieron estadísticos descriptivos y correlacionales.
ResultadosHubo 62 participantes, el 96,8% de ellos mujeres. El 75% presentó sufrimiento moderado a severo; el 62,9% mostró indicadores clínicos de soledad; el 75%, indicadores clínicos de ansiedad; y un 25,8% tuvo indicadores clínicos de depresión. Además, se reportó una media de 10 eventos vitales estresantes. Hubo correlación significativa entre el nivel de sufrimiento y el impacto en la calidad de vida. Dicho impacto también se correlacionó de forma significativa con la soledad, la ansiedad y la depresión. El estrés vital mostró relación directa y significativa con la soledad y la ansiedad. La fuerza de las correlaciones, aunque significativa, fue de moderada en muchos casos.
ConclusionesLos pacientes con FM manifiestan un sufrimiento importante, además del impacto en la calidad de vida. Dicho impacto se relaciona con factores psicosociales, más allá de los conocidos (ansiedad y depresión), como soledad y estrés vital. Los resultados permiten visibilizar el intenso sufrimiento de esta población e indican la importancia de examinar con mayor profundidad temas como la soledad y el estrés vital.
Fibromyalgia (FM) is a chronic pain syndrome that is currently diagnosed using the FM ABC indicators: (A) algesia or hyperalgesia, (B) pattern of pain with bilateral, multilocular, axial symmetrical distribution and (C) Symptoms of chronic anxiety, which show better specificity, lower sensitivity and greater diagnostic effectiveness compared with the criteria used in 2011.1 It is usually accompanied by neuropsychological symptoms such as fatigue, non-restorative sleep, cognitive dysfunction, anxiety and depression, as well as other syndromes such as chronic fatigue, temporomandibular dysfunction, chronic headache and pelvic pain, among others.1–6
This pathology constitutes the main cause of generalized musculoskeletal pain in women between 20 and 55 years of age and is classified as one of the pain syndromes with the worst quality of life. Although it generates a high health care cost and represents a public health problem on a global, regional and national scale, in Latin America there is little information related to its prevalence, costs and economic impact, which makes difficult to manage this disease.1 A study on rheumatic diseases conducted in Colombia in 2018 showed a prevalence of 0.72% for FM, a figure similar to that reported in the Mexican population and lower than that of countries such as Brazil, Ecuador and Portugal. In addition to this, it reported results very similar to those with rheumatoid arthritis (RA) regarding pain, discomfort, difficulty in daily functioning, anxiety and depression, and described a deterioration in quality of life secondary to the compromise of functional capacity due to pain, poor sleeping pattern, low productivity, more comorbidities and chronic consumption of analgesics.2
Despite the problems that FM represents, there is limited awareness of its impact on the population. The lack of knowledge about the disease is evident, both in health professionals3 and in the general community.7 Furthermore, the difficulties of detection through scientific tests and the late diagnosis have generated discomfort in patients for years, as well as an attitude of lack of understanding on the part of their families and their social environment, which leads to stigmatization that contributes to their suffering.3,7,8 Often, people with FM feel alienated and isolated due to the attitudes of disbelief regarding their condition and their personal and mental integrity. Added to this is a progressive tendency to evade social situations in order to avoid greater stressors that increase their pain. Consequently, over time, social isolation and feelings of loneliness tend to increase, which leads to a deterioration of social ties and contributes to emotional distress and focusing on the disease.9
Taken together, the multiple problems posed by FM can imply relevant suffering for people with this diagnosis, which is why is essential to identify the factors associated with this condition. Suffering is defined as "a multidimensional and dynamic experience of severe stress that occurs in the face of events that threaten the integrity of the person and where the regulatory processes, which would normally lead to adaptation, become insufficient, causing exhaustion."10 This experience is closely related to emotional distress, negative affective states and pain. Given that it is a multidimensional experience that integrates physiological and psychosocial phenomena related to stress, problems of a physical, psychological, social or spiritual nature may indicate or be associated with its presence.11 In this sense, Cassell considers that patients must be seen as people, dynamic psychological and social entities, and emphasizes the complexity of their identity, their unique personal history and their sociocultural context.12 In fact, suffering has been linked to factors such as vulnerability, rejection, unemployment and isolation, among others.12
The experience of suffering has been widely studied in oncological and palliative care contexts,13 but little in chronic diseases. Some studies have assessed suffering in patients with rheumatoid arthritis (RA), lupus, vitiligo, chronic pain and diabetes, among others.14 Unfortunately, despite the well-known contribution of persistent pain to this experience, there are no reports of studies on suffering in patients with FM and the scientific literature has focused on its demographic, social and clinical factors.15
For this reason, the exploration of the association of different demographic, social, clinical and psychological factors with the suffering of this population should be initiated. It is essential to take into account comorbidities such as depression and anxiety since their prevalence is high; around 30–45% for anxiety, and depression ranges from 28.6–70%.16 In addition, anxiety and depression are associated with greater pain severity, more physical symptoms and worse functioning in patients with FM.17,18
Loneliness, understood as the subjective experience of not achieving the desired quality in relationships, and social isolation, referring to the quantity of interpersonal interactions and the magnitude of the social network, bring negative consequences for mental and physical health,19 therefore, they should not be overlooked when addressing the suffering of the patient with FM. Growing evidence points to their relationship with body pain, fatigue, negative affect, maladaptive responses to stress and negative perception of social interactions, both in healthy individuals and in those with chronic conditions. Particularly in people with FM, it has been found that both chronic and transient loneliness are associated with more negative social interactions and pain9; likewise, stress is associated with clinical indicators of loneliness, which highlights a reciprocal relationship between loneliness and stress.20 The latter is more frequent in this population (e.g., sexual and physical abuse or being victims or witnesses of highly negative events),21 and it appears that both post-traumatic stress and negative life events can predispose to the appearance of FM.18 This relationship could be explained by alterations in neuroendocrine function,17 or by the biopsychosocial model of variables that interact in the predisposition, triggering and maintenance of FM. It has also been considered that early life events, together with chronic stress, affect the modulatory circuits of pain and affect, which would be the cause of altered responses to pain, difficulties in adaptation and development of social and mental problems that increase the suffering of patients.21
Hence, it is relevant to maintain an expanded vision of this disease, knowing the factors that are associated with suffering and allowing a biopsychosocial conceptualization of the syndrome, which may be important to propose more effective evaluation, preventive and intervention strategies in FM.22 The objective of the study presented here was to determine the level of suffering of patients with FM and its relationship with the impact of the disease, emotional state, life stress, loneliness and demographic factors. Partial results from an ongoing study are presented below.
MethodsType of study and populationQuantitative, observational, analytical, and cross-sectional study, with a correlational design. The population consisted of patients with a diagnosis of FM treated at an institution specialized in pain management in Medellín, Colombia. Convenience sampling was carried out, consecutively selecting patients attended by outpatient consultation or priority care, during the period from March to June 2021, who met the following criteria: patients over 18 years of age, with a diagnosis of FM made by a pain specialist or a rheumatologist (according to diagnostic criteria of the American College of Rheumatology [ACR] 2016), and whose main complaint was this disease. Likewise, they must have attended at least one follow-up consultation having an established treatment, and understand, read and write Spanish. Patients with pain crisis, conditions that limited their cognitive ability to understand the self-administered tests (according to medical criteria), with comorbidity with active oncological disease, multiple sclerosis or other demyelinating diseases, dementia or other neurodegenerative diseases, acute infectious, traumatic or surgical conditions that limited or prevented their participation were excluded.
The project was approved by the Ethics Committee of the Universidad Pontificia Bolivariana and the participating health institution.
Collection techniques and instrumentsData collection was from a primary source: a survey was applied to patients who attended the outpatient clinic at the Instituto Colombiano del Dolor (Colombian Pain Institute) during the year 2021. Those who were in charge of data collection (all health professionals) were previously trained to standardize the process.
A format to collect sociodemographic and clinical data, including age, marital status, sex, number of children, availability of caregivers, origin, occupation, educational level, religion, as well as other data related to diagnosis and treatment was used.
The Revised Fibromyalgia Impact Questionnaire (FIQR), which uses visual analogue scales with scores between 0 and 10, was used to assess the impact of FM. A global impact score was obtained with a range between 1 and 100, where higher scores indicate greater affectation; scores from three subscales: impact on functioning (FIQR-F; sum of items 1–9; range: 0–30); global impact (FIQR-I; sum of items 10 and 11; range: 0–20); and intensity of symptoms (FIQR-S; sum of items 12–21; range 0–50) were also obtained.23 The evaluation of the validity, reliability, and internal consistency of the FIQ in Colombia reported a Cronbach's alpha higher than 0.7 in the dimensions evaluated; the internal consistency and the discriminant validity presented a success rate of 100%. In the convergent/divergent validity, it was observed that the concept of health-related quality of life of the FIQ was congruent with that of two other quality of life instruments.24
The level of suffering was evaluated with the Pictorial Representation of Illness and Self Measure instrument (PRISM). This instrument uses a non-directive graphical approach, which allows us to assess total suffering and obtain a quantitative measure25; it has been widely used and is validated for the Colombian population. The electronic version of the instrument was used and a measure of the distance between the disease and the self was obtained (range 0–27, where lower scores indicate greater suffering).
To determine the degree of loneliness, the UCLA Loneliness Scale, created by Russell et al.,26 which consists of three dimensions: subjective perception of loneliness, family support and social support, with two factors: intimacy with others and sociability, was used. The 10-item version27 validated in Spanish by Velarde-Mayol et al.,28 whose scoring uses a four-point Likert scale (range: 10–40), in which a total score of up to 31 points indicates a clinical state of loneliness, was used for the present study. The Cronbach's alpha of 0.95 revealed high reliability of the scale and all its items.
To examine the degree of anxiety and depression, the Hospital Anxiety and Depression Scale (HADS),29 which consists of 14 items that assess anxiety (HADS-A) and depression (HADS-D) was used. Responses are scored on a four-point Likert scale, where higher scores indicate greater severity. An overall measure of emotional distress (range: 0–42), or from each subscale (range: 0–21), can be obtained. It was used the version validated for Colombia,30 which showed adequate internal consistency and validity. Cronbach's alpha coefficient was 0.85 and the split-half reliability was 0.8. Eight cut-off points were used for HADS-A and nine for HADS-D, which showed greater sensitivity and concordance with the psychiatric interview.
Finally, life stress was examined using the Sandín and Chorot Life Events Questionnaire,31 which consists of a list of 60 life events related to work, academic sphere, health, couple relationships, family and children, social relationships, residence and economic and legal aspects. Patients were asked to indicate the occurrence of each vital event experienced in the course of their life and the impact or degree of stress of each event on a scale between one (no stress) and four (a lot of stress); and were asked to indicate 0 in the case of non-occurrence of the event. The questionnaire obtained acceptable levels of reliability and good levels of convergent, discriminant and predictive validity. In its validation study, the mean obtained in the count of events was 11.68 and for life stress it was 23.30.31
ProcedureOnce the study was approved, a pilot study with 10 patients was carried out to standardize the process of administering the instruments and verify their adequacy, completion time, and understanding of the instructions.
All patients who attended outpatient consultation and priority care of pain and who met the inclusion and exclusion criteria were invited to participate. During the medical consultation, the clinical history was reviewed to verify compliance with the eligibility criteria, and then the patient was invited to participate in the study, the objectives were explained and the patient was asked to sign the informed consent. The information that appeared in the clinical history was collected, as well as the application of the PRISM. The other instruments were self-administered and the researchers were available to resolve doubts during the process.
Analysis of the informationA database was created in the Excel program (Excel version 16.43, Microsoft 2020, USA) and the Jamovi statistical package, version 1.6.23.0 (Jamovi Project, 2022, Sidney, Australia), was used for the statistical analyses. Absolute and relative frequencies were obtained for the discontinuous variables, and measures of central tendency and dispersion for the continuous variables. The distribution of the variables was examined using the Shapiro-Wilk test. Given the non-normal distribution of many of the variables, means and standard deviations as well as medians and interquartile ranges were indicated, and the use of non-parametric tests was chosen for correlational analyzes (Spearman's Rho).
Ethical considerationsThe project complied with the principles contained in current international declarations (Helsinki, CIOMS, UNESCO), was classified as minimal risk research (Resolution 8430 of 1993 of Colombia) and was approved by the Ethics Committee of the Universidad Pontificia Bolivariana (Act n° 07 of 2021).
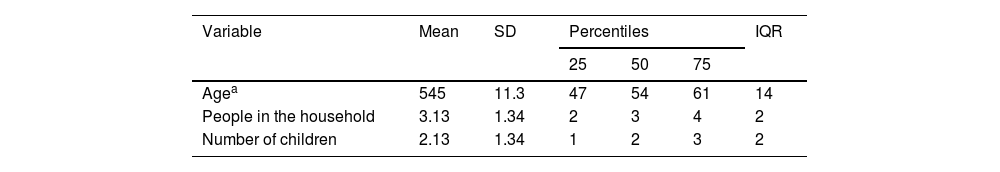
ResultsSociodemographic and clinical characteristicsA total of 62 patients participated, the vast majority of them were women (96.8%), with a median age of 54 years, 48% married or in a free union, with a median of two children and three people living in the household. Almost 80% live in strata 2 and 3 (lower middle class), more than 95.2% live in urban areas, and the majority (78%) have secondary or higher education; 32.5% are employed and 35.5% are dedicated to household chores. Eighty-four percent (84%) are attached to a religion and practice it (Table 1).
Sociodemographic characteristics.
| Variable | Mean | SD | Percentiles | IQR | ||
|---|---|---|---|---|---|---|
| 25 | 50 | 75 | ||||
| Agea | 545 | 11.3 | 47 | 54 | 61 | 14 |
| People in the household | 3.13 | 1.34 | 2 | 3 | 4 | 2 |
| Number of children | 2.13 | 1.34 | 1 | 2 | 3 | 2 |
| Variable | Category | n (%) |
|---|---|---|
| Sex | Woman | 60 (96.8) |
| Man | 2 (3.2) | |
| Marital status | Single | 14 (22.6) |
| Married/free union | 30 (48.4) | |
| Separated/divorced | 12 (19.4) | |
| Widow | 6 (9.7) | |
| Religion | Not attached | 1 (1.6) |
| Attached, does not practice it | 9 (14.5) | |
| Attached and practices it | 52 (83.9) | |
| Stratum | 1 | 3 (4.8) |
| 2 | 34 (54.8) | |
| 3 | 15 (24.2) | |
| 4 | 5 (8.1) | |
| 5 | 3 (4.8) | |
| 6 | 2 (3.2) | |
| Education level | No studies | 3 (4.8) |
| Primary studies | 11 (17.7) | |
| Secondary studies | 24 (38.7) | |
| Higher studies | 24 (38.7) | |
| Occupation | Employee | 20 (32.3) |
| Independent | 4 (6.5) | |
| Housewife | 22 (35.5%) | |
| Unemployed | 6 (9.8) | |
| Student | 0 (0) | |
| Retired/pensioner | 10 (16.1) | |
| Residence | Urban | 59 (95.2) |
| Rural | 3 (4.8) | |
| Caregiver | Does not require a caregiver | 51 (83.6) |
| Occasional caregiver | 6 (9.8) | |
| Caregiver frequently | 2 (3.3) | |
| Permanent caregiver | 1 (1.6) | |
| Requires, but does not have | 1 (1.6) |
SD: standard deviation; IQR: interquartile range.
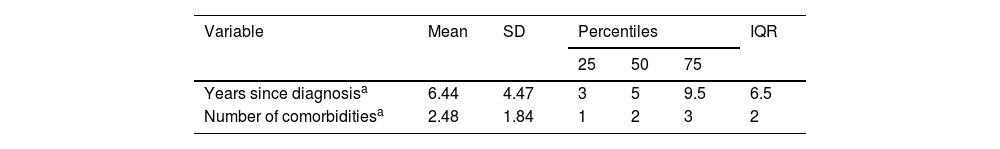
With respect to the clinical profile (Table 2), the mean time since diagnosis is six years and they have a median of two comorbidities, the most frequent being: arterial hypertension, hypothyroidism, depression, anxiety, rheumatoid arthritis, arthrosis, Sjögren's syndrome, gastritis and headache. More than 98% use analgesics and about 62% use antidepressants, while other treatments are less frequent. A little more than half of the participants receive psychiatric treatment, and attendance at physiotherapy or psychotherapy is less frequent. More than half do not exercise or do it only occasionally, while nearly a quarter attend religious groups. Finally, about 84% of the participants indicate that they do not require a caregiver, while less than 12% require a caregiver occasionally.
Clinical characteristics of the participants.
| Variable | Mean | SD | Percentiles | IQR | ||
|---|---|---|---|---|---|---|
| 25 | 50 | 75 | ||||
| Years since diagnosisa | 6.44 | 4.47 | 3 | 5 | 9.5 | 6.5 |
| Number of comorbiditiesa | 2.48 | 1.84 | 1 | 2 | 3 | 2 |
| Variable | Category | n (%) |
|---|---|---|
| Frequency of physical activity | Never | 10 (16.1) |
| Very occasional (1−4 times per month) | 25 (40.3) | |
| Occasional (5−8 times per month) | 12 (19.4) | |
| Frequently (3−5 days per week) | 11 (17.17) | |
| Always (6−7 times per week) | 4 (6.4) | |
| Uses analgesics | Yes | 60 (98.4) |
| Uses antidepressants | Yes | 39 (62.9) |
| Uses anticonvulsants | Yes | 26 (41.9) |
| Uses other medications | Yes | 26 (41.9) |
| Uses complementary treatments | Yes | 12 (19.4) |
| Physiotherapy | Yes | 20 (32.3) |
| Psychiatry | Yes | 32 (51.6) |
| Psychotherapy | Yes | 13 (21.0) |
| Attends religious groups | Yes | 14 (22.6) |
| Other therapy | Yes | 62 (100) |
SD: standard deviation; IQR: interquartile range.
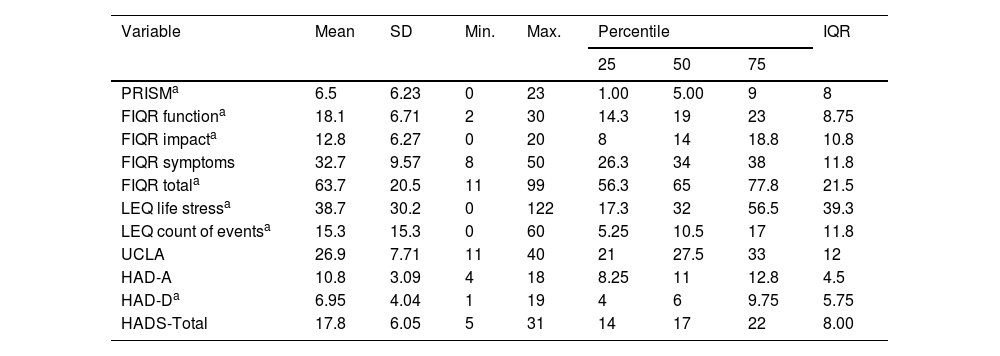
The level of suffering (measured through the PRISM) showed a median of 5.0 and 75% of the population had scores lower than 9.0, in a range of 0–27, which puts in evidence a level of intense to severe suffering (lower scores indicate greater suffering). Similarly, the impact of FM (measured through the FIQR) was medium-high, with a median score of 65 (Table 3).
Descriptive results of the tests administered.
| Variable | Mean | SD | Min. | Max. | Percentile | IQR | ||
|---|---|---|---|---|---|---|---|---|
| 25 | 50 | 75 | ||||||
| PRISMa | 6.5 | 6.23 | 0 | 23 | 1.00 | 5.00 | 9 | 8 |
| FIQR functiona | 18.1 | 6.71 | 2 | 30 | 14.3 | 19 | 23 | 8.75 |
| FIQR impacta | 12.8 | 6.27 | 0 | 20 | 8 | 14 | 18.8 | 10.8 |
| FIQR symptoms | 32.7 | 9.57 | 8 | 50 | 26.3 | 34 | 38 | 11.8 |
| FIQR totala | 63.7 | 20.5 | 11 | 99 | 56.3 | 65 | 77.8 | 21.5 |
| LEQ life stressa | 38.7 | 30.2 | 0 | 122 | 17.3 | 32 | 56.5 | 39.3 |
| LEQ count of eventsa | 15.3 | 15.3 | 0 | 60 | 5.25 | 10.5 | 17 | 11.8 |
| UCLA | 26.9 | 7.71 | 11 | 40 | 21 | 27.5 | 33 | 12 |
| HAD-A | 10.8 | 3.09 | 4 | 18 | 8.25 | 11 | 12.8 | 4.5 |
| HAD-Da | 6.95 | 4.04 | 1 | 19 | 4 | 6 | 9.75 | 5.75 |
| HADS-Total | 17.8 | 6.05 | 5 | 31 | 14 | 17 | 22 | 8.00 |
SD: standard deviation; IQR: interquartile range; PRISM: Pictorial Representation of Illness and Self Measure instrument (PRISM); FIQR: Fibromyalgia Impact Questionnaire; LEQ: Life Events Questionnaire; UCLA: Loneliness Scale; HADS: Hospital Scale of Anxiety and Depression; HAD-A: Anxiety Subscale; HAD-D: Depression Subscale.
As for the level of loneliness, the median obtained on the UCLA scale was 27.5, where scores lower than 31 reflect clinical states of loneliness. With this cut-off point, it was found that 62.9% (n = 39) of the participants presented clinical indicators of loneliness (Table 3). With respect to the emotional distress measured with the HADS, the 25th percentile score on the anxiety subscale exceeds the cut-off point of eight, which is a sign of clinical anxiety problems in approximately 75% of the population studied. Specifically, 74.2% (n = 46) presented clinical problems related to anxiety. Meanwhile, 25.8% (n = 16) of the patients had scores above nine on the HAD-D, which correspond to clinical indicators of depression (Table 3).
Finally, the occurrence and the level of stress of the life events manifested by the participants were assessed, finding a median of 10.5 life events and a median of stress associated with the events of 32 (Table 3).
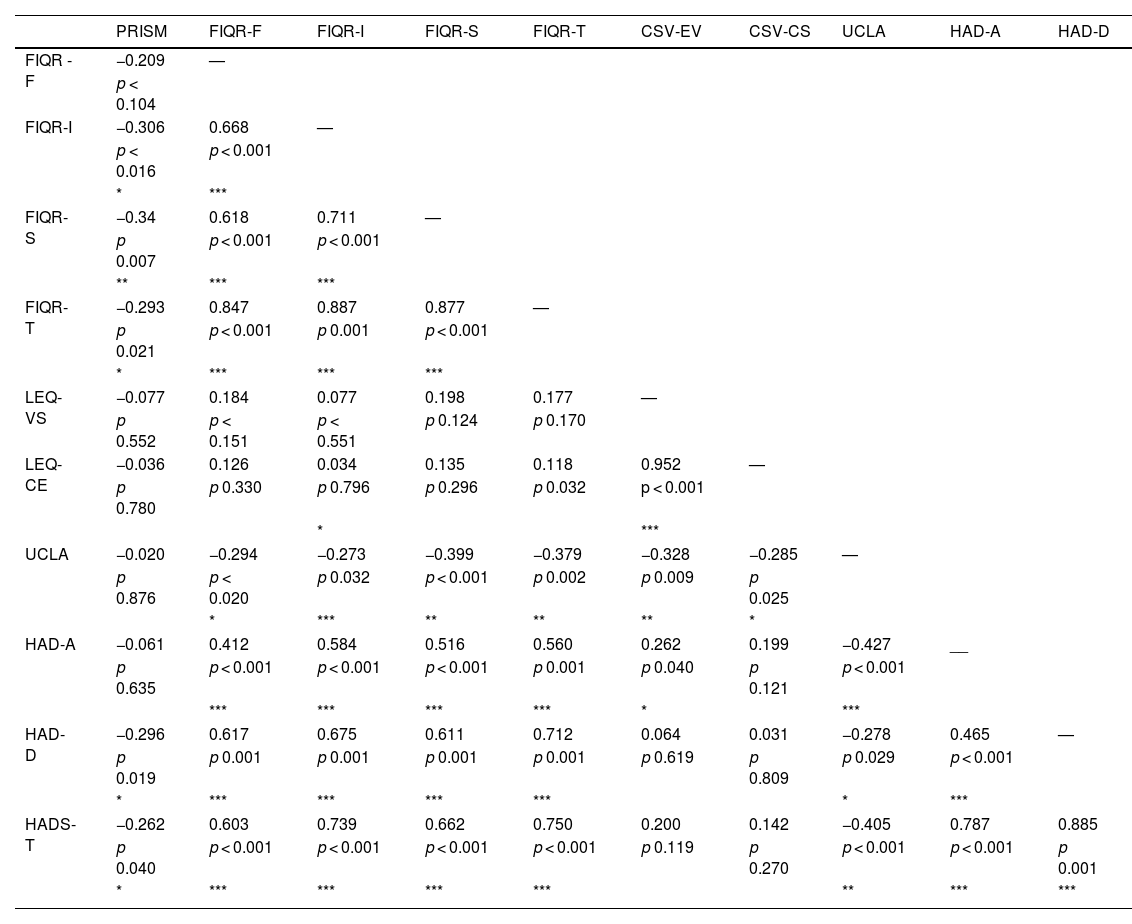
Correlational analysesSufferingSignificant and inverse correlations were found between the PRISM scores and the HADS and the FIQR, in particular with the total score of the FIQR and its subscales of general impact and symptoms, which shows that the higher the levels of suffering, the higher the level of anxiety and depression and greater the impact of FM on quality of life. However, the strength of these correlations was low (Table 4).
Correlation matrix between the scale scores.
| PRISM | FIQR-F | FIQR-I | FIQR-S | FIQR-T | CSV-EV | CSV-CS | UCLA | HAD-A | HAD-D | |
|---|---|---|---|---|---|---|---|---|---|---|
| FIQR -F | −0.209 | — | ||||||||
| p < 0.104 | ||||||||||
| FIQR-I | −0.306 | 0.668 | — | |||||||
| p < 0.016 | p < 0.001 | |||||||||
| * | *** | |||||||||
| FIQR-S | −0.34 | 0.618 | 0.711 | — | ||||||
| p 0.007 | p < 0.001 | p < 0.001 | ||||||||
| ** | *** | *** | ||||||||
| FIQR-T | −0.293 | 0.847 | 0.887 | 0.877 | — | |||||
| p 0.021 | p < 0.001 | p 0.001 | p < 0.001 | |||||||
| * | *** | *** | *** | |||||||
| LEQ-VS | −0.077 | 0.184 | 0.077 | 0.198 | 0.177 | — | ||||
| p 0.552 | p < 0.151 | p < 0.551 | p 0.124 | p 0.170 | ||||||
| LEQ-CE | −0.036 | 0.126 | 0.034 | 0.135 | 0.118 | 0.952 | — | |||
| p 0.780 | p 0.330 | p 0.796 | p 0.296 | p 0.032 | p < 0.001 | |||||
| * | *** | |||||||||
| UCLA | −0.020 | −0.294 | −0.273 | −0.399 | −0.379 | −0.328 | −0.285 | — | ||
| p 0.876 | p < 0.020 | p 0.032 | p < 0.001 | p 0.002 | p 0.009 | p 0.025 | ||||
| * | *** | ** | ** | ** | * | |||||
| HAD-A | −0.061 | 0.412 | 0.584 | 0.516 | 0.560 | 0.262 | 0.199 | −0.427 | __ | |
| p 0.635 | p < 0.001 | p < 0.001 | p < 0.001 | p 0.001 | p 0.040 | p 0.121 | p < 0.001 | |||
| *** | *** | *** | *** | * | *** | |||||
| HAD-D | −0.296 | 0.617 | 0.675 | 0.611 | 0.712 | 0.064 | 0.031 | −0.278 | 0.465 | — |
| p 0.019 | p 0.001 | p 0.001 | p 0.001 | p 0.001 | p 0.619 | p 0.809 | p 0.029 | p < 0.001 | ||
| * | *** | *** | *** | *** | * | *** | ||||
| HADS-T | −0.262 | 0.603 | 0.739 | 0.662 | 0.750 | 0.200 | 0.142 | −0.405 | 0.787 | 0.885 |
| p 0.040 | p < 0.001 | p < 0.001 | p < 0.001 | p < 0.001 | p 0.119 | p 0.270 | p < 0.001 | p < 0.001 | p 0.001 | |
| * | *** | *** | *** | *** | ** | *** | *** |
PRISM: Graphic representation of illness and the self-distance; FIQR: Fibromyalgia Impact Questionnaire; FIQR-F: functioning subscale; FIQR-I: impact subscale; FIQR-S: symptoms subscale; FIQR-T: total score; LEQ: Life Events Questionnaire; LEQ-VS: vital stress subscale; LEQ-CE: count of events subscale; UCLA: UCLA Loneliness Scale; HADS: Hospital Scale of Anxiety and Depression; HAD-A: anxiety subscale; HAD-D: depression subscale; HADS-T: total score.
*p < 0.05.
**p < 0.001.
***p < 0.0001.
On the other hand, the greater the impact of FM on quality of life, there were significantly higher levels of loneliness, general emotional distress, anxiety and depression. These correlations showed statistical significance both with the total FIQR score and with all its subscales, and the strength of the correlations was moderate to strong, especially with the variables measured through the HADS (Table 4).
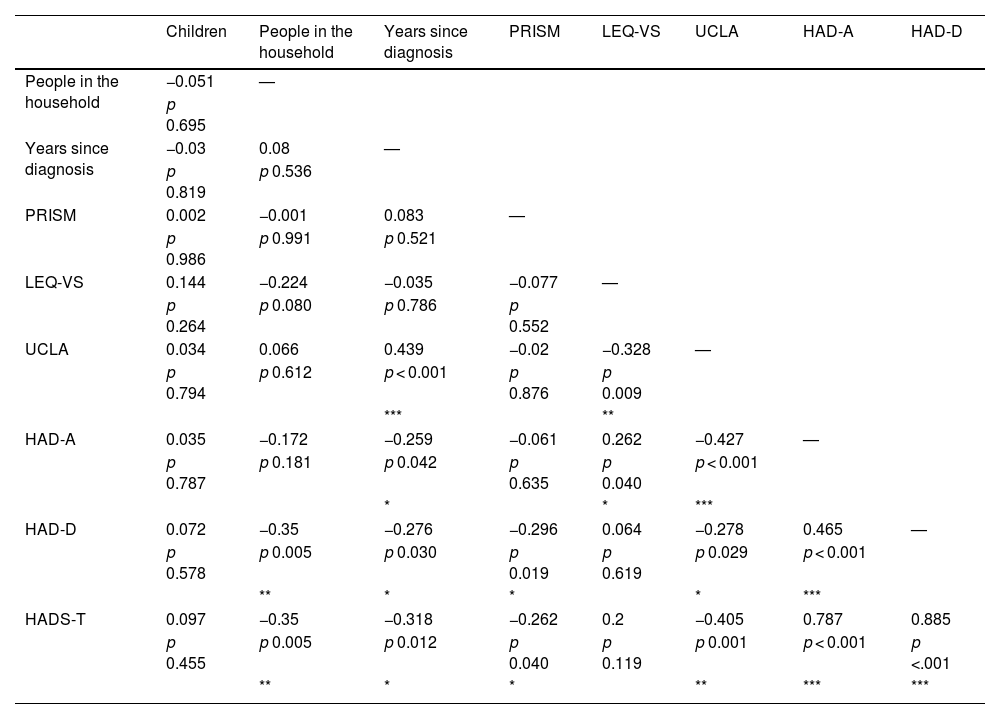
Sociodemographic variablesThe correlations between the scores of the scales and the sociodemographic variables were also analyzed (Table 5), and it was found a statistically significant and inverse relationship between the number of people in the household and the years since the diagnosis with the emotional state, which is an evidence that the fewer people in the household and the less recent the diagnosis, the scores for total general distress and of the depression scale were higher, with a low strength of these correlations. There was also a statistically significant and direct correlation between the score in the UCLA scale and the years since diagnosis, a sign that the shorter the time since diagnosis there was a greater perception of loneliness. Remarkably, the level of loneliness and the number of children or people in the household were not correlated.
Correlation matrix between sociodemographic variables and scale scores.
| Children | People in the household | Years since diagnosis | PRISM | LEQ-VS | UCLA | HAD-A | HAD-D | |
|---|---|---|---|---|---|---|---|---|
| People in the household | −0.051 | — | ||||||
| p 0.695 | ||||||||
| Years since diagnosis | −0.03 | 0.08 | — | |||||
| p 0.819 | p 0.536 | |||||||
| PRISM | 0.002 | −0.001 | 0.083 | — | ||||
| p 0.986 | p 0.991 | p 0.521 | ||||||
| LEQ-VS | 0.144 | −0.224 | −0.035 | −0.077 | — | |||
| p 0.264 | p 0.080 | p 0.786 | p 0.552 | |||||
| UCLA | 0.034 | 0.066 | 0.439 | −0.02 | −0.328 | — | ||
| p 0.794 | p 0.612 | p < 0.001 | p 0.876 | p 0.009 | ||||
| *** | ** | |||||||
| HAD-A | 0.035 | −0.172 | −0.259 | −0.061 | 0.262 | −0.427 | — | |
| p 0.787 | p 0.181 | p 0.042 | p 0.635 | p 0.040 | p < 0.001 | |||
| * | * | *** | ||||||
| HAD-D | 0.072 | −0.35 | −0.276 | −0.296 | 0.064 | −0.278 | 0.465 | — |
| p 0.578 | p 0.005 | p 0.030 | p 0.019 | p 0.619 | p 0.029 | p < 0.001 | ||
| ** | * | * | * | *** | ||||
| HADS-T | 0.097 | −0.35 | −0.318 | −0.262 | 0.2 | −0.405 | 0.787 | 0.885 |
| p 0.455 | p 0.005 | p 0.012 | p 0.040 | p 0.119 | p 0.001 | p < 0.001 | p <.001 | |
| ** | * | * | ** | *** | *** |
PRISM-D: Graphic representation of illness and the self-distance; FIQR: Fibromyalgia Impact Questionnaire; FIQR-F: functioning subscale; FIQR-I: impact subscale; FIQR-S: symptoms subscale; FIQR-T: total score; LEQ: Life Events Questionnaire; LEQ-VS: vital stress subscale; LEQ-CE: count of events subscale; UCLA: UCLA Loneliness Scale; HADS: Hospital Scale of Anxiety and Depression; HAD-A: anxiety subscale; HAD-D: depression subscale; HADS-T: total score.
*p < 0.05.
**p < 0.001.
***p < 0.0001.
Finally, it was found a statistically significant and inverse relationship between the total impact of FM and its symptoms subscale and the years since the diagnosis (r = −0.335, p = 0.008; r = −0.361, p = 0.004, respectively) and the age (r = −0,358, p = 0,004; r = −0,336, p = 0,008, respectively); this indicates that the less time had passed since the diagnosis and the younger the person was, the greater the impact. Likewise, the correlation between age and the impact subscale of the FIQR was inverse and significant (r = −0.289, p = 0.023). On the other hand, the number of comorbidities showed a direct and statistically significant relationship with total FIQR and the functioning and impact subscales (r = 0.346, p = 0.006; r = 0.304, p = 0.016; r = 0.339, p = 0.007, respectively), which indicates that the greater the number of comorbidities there is a greater impact on quality of life. As with many other correlations described, the strength of the relationship was moderate to low.
DiscussionFM entails significant psychosocial and physiological consequences.5 The multiplicity of symptoms and associated problems suggests that suffering may be significant, but the scarcity of studies on the subject in this population is striking. Therefore, the present study sought to determine the levels of suffering of patients with FM and to identify its relationship with some psychosocial factors.
With respect to sociodemographic characteristics, the participants were predominantly women with a mean age of 54 years, married, of Catholic religion, of medium to low socioeconomic status, employed or housewives, and with secondary or higher education levels. These results agree with what has been reported in the literature, particularly regarding gender and age.5,17 However, unlike what was reported by Walitt et al.,6 who sustain that being divorced or separated and not having higher education constitute risk factors, our population was mostly married and with high educational levels.
At the clinical level, the mean time since diagnosis was six years, multiple comorbidities were frequent, the majority of patients used analgesics or antidepressants and approximately half received psychiatric treatment; in general, the participants reported low levels of exercise and only about one-third were doing physical therapy. These results coincide with previous findings that point to the chronicity of the condition, the comorbidities that accompany it and its impact on physical and mental functioning,2 which affects the daily life of patients and brings significant psychosocial and physiological consequences.32 Even so, the majority did not require a caregiver, which denotes minimal affectation on autonomy, despite the interference it generates.
Regarding the levels of suffering, 75% of the people had a score lower than nine and a median of five (range of 0–27, where 0 is equivalent to greater suffering), which shows very high levels of suffering in general. These results coincide with those of Brady et al., in whose study patients with painful neuromusculoskeletal pathologies had a mean PRISM score of 5.5; with scores lower than 6.0, considered "high suffering".33 Specifically in patients with FM, Paschali et al. found a mean score of 6.2 on the PRISM, which also indicates high suffering. As in our study, suffering showed significant correlations with the interference and severity of pain and with the impact of the FM measured with the FIQR.34
The above findings are striking, compared with those obtained in patients with advanced cancer, where the mean PRISM score was 14, a sign of moderate levels of suffering.25 In general, it is considered that patients with catastrophic diseases usually have very high levels of suffering; however, these findings suggest that patients with chronic painful pathologies may have higher levels of suffering. Meanwhile, Garaigordobil and Govillard35 found greater global psychological and psychosomatic suffering in people with FM, when comparing them with people without the disease.
Suffering implies severe stress associated with a threat to integrity, where the mechanisms that would help achieve adaptation are insufficient and lead to exhaustion. It is a subjective and integral experience, where the joint occurrence of physical, psychosocial and spiritual factors is frequent and relevant. Pain is closely associated with suffering, and when it is insufficiently managed, it can contribute significantly. Evidence shows that more and more effective management of pain, both acute and chronic, is being achieved, especially in serious diseases such as cancer.36 Other populations with painful pathologies such as FM face social and even medical stigma and barriers to access effective analgesic management and comprehensive care. The patients describe this disease as "a problematic label, a heavy burden to carry and of low therapeutic priority", which undoubtedly increases their suffering.7
The impact of FM on quality of life was medium-high. The scores in our study were slightly lower than those obtained in the scale validation study conducted by Salgueiro et al.,23 whose mean total score was 70. The scores obtained by them in the subscales of function, impact and symptoms were, respectively, 19, 12 and 37, very close to the 18, 12 and 32 obtained in our study and which indicate the impact that FM generates in the different areas assessed.
There was also an important impact on an emotional level: about 75% of the patients had clinical indicators of anxiety and about 25% of depression. Despite the fact that 50% of the patients received treatment with psychiatry, 20% with psychology, and 63% used antidepressants, the high levels of self-reported depression are remarkable. This may be indicative of the severity of these symptoms in the population, as well as of the need to examine whether the treatments offered are sufficient and targeted to the specific needs of these patients.
Painful pathologies coexist with anxious and depressive symptoms,35 particularly FM, with a prevalence of 30–45 % for anxiety and 28.6−70% for depression.16,37 Problems related to depression, anxiety, obsessive-compulsive disorder (OCD), and post-traumatic stress disorder (PTSD) are common and are associated with triggering events such as early life stressors and traumatic events. With respect to anxiety disorders, the greatest association has been observed with OCD, followed by PTSD, social phobia, panic disorder, agoraphobia, simple phobia and generalized anxiety disorder; unfortunately, our study only used emotional state screening tests, and therefore it is not possible to determine the presence or the types of specific anxiety disorders.
Mood and anxiety disorders in FM are not only common, but also contribute to the negative impact on quality of life,32 and are associated with greater pain severity, more physical symptoms and worse functioning when compared with other patients with painful pathologies.17,18 The foregoing is consistent with what was found in our study, since there was a statistically significant correlation between the levels of anxiety and depression and the FIQR scores, as well as between the levels of depression and general discomfort and the degree of suffering. These results also coincide with those obtained by other authors.34,38
Mental and social problems are often associated with adaptation difficulties and the occurrence of multiple stressful situations, aspects that together can converge in the suffering of patients with FM.39 More than 60% of the participants in our study presented clinical indicators of loneliness, and on average they reported the occurrence of 10 significant life events throughout their lives, which generated significant levels of stress. Loneliness showed a statistically significant correlation, not only with the number of life events and the stress levels associated with them, but also with anxiety, depression and the impact of FM on quality of life (both with the total score of the FIQR as with its function, impact and symptoms subscales).
Loneliness has negative consequences for health, both mental and physical.19 Particularly in people with FM, it has been found that both chronic and transient loneliness is associated with more negative social interactions and pain.9 Added to this are the frequent feelings of alienation and isolation that people with FM experience due to attitudes of social disbelief regarding their diagnosis, the pain and its impact on their personal and mental integrity, both on the part of the professionals as well as by their family members.7,8 In fact, physical pain and social exclusion activate common neural circuits and it has been considered the possibility of a pain imprint in the central nervous system that is activated in response to physical and social stimuli.40
With reference to stress, it is known that negative life events and traumatic experiences are more frequent in this population (e.g., sexual and physical abuse or being victims or witnesses of highly negative events),16 which is corroborated in our study. Furthermore, alterations in social functioning, in this case loneliness, constitute another stressor that is associated with the multiple ones that occur in FM, including frequent and intense pain, different physical and emotional symptoms, and deterioration of physical functionality.
There are different models to explain the relationship between mental problems and FM. The psychosocial model considers FM as a functional somatic syndrome whose symptoms are the consequence of an abnormal response to stressors and behavioral factors.22 Another model proposes that harmful signals can directly provoke the stress response, while psychological stressors can involve stress circuits different than the physiological stressors and entail a greater contribution from areas related to affect and emotions.21
In accordance with the above, the identification of suffering in patients with FM and the contribution of emotional, social and stress-related factors implies a relevant and novel contribution that can favor scientifically supported clinical practices that expand the use of the available therapeutic tools.
Finally, the findings of this study should be read taking into account the context of the COVID-19 pandemic, during which it was carried out, and the potential consequences of this disease. A significant increase in feelings of stress, loneliness, social isolation and impact on mental health has been documented in the general population and, specifically in FM,41,42 musculoskeletal pain derived from COVID-19. Therefore, it is possible that the impact associated with FM, identified in our study, was partly marked by the pandemic context.
In summary, this study allows us to put in evidence the levels of suffering of a population that is frequently invisibilized and ignored and, likewise, demonstrates the multiplicity of related psychosocial factors, as well as its impact on the quality of life, which shows the importance of a comprehensive, pluridisciplinary approach to FM, that recognizes the appropriate value of the contribution of the psychological and social dimensions to pain, beyond physical alterations.32
Limitations of the studyIt is important to recognize the limitations of our study: the cross-sectional nature thereof only allows us to know the behavior of the variables at a given moment and the relationship between them, but not the directionality of said relationship; the sample size was limited, due to the healthcare challenges brought by COVID-19, which is why it was not possible to carry out more complex statistical analyzes or make the findings generalizable; likewise, we do not know how the pandemic context may have influenced emotional and social variables and even pain; data collection was done at a single center and the population had some characteristics (for example, educational level) that are not representative of the general population. Finally, the evaluation carried out is based on self-reports; it would be ideal that future studies include other more objective evaluation strategies for the variables where possible.
ConclusionsDespite the problems that FM represents, there is limited awareness of its impact on a social scale, both among health professionals and the general population. The results of this study allow us to recognize and make visible the intense suffering experienced by patients with FM, in addition to the impact on their quality of life. It is one of the first studies that have determined the relationship of this condition with psychosocial factors such as loneliness and life stress, beyond anxiety and depression. These findings contribute to a better understanding of the aspects involved in FM, which will allow us to propose alternatives to improve the well-being and quality of life of these patients and their social environment.
FundingThis work has not received any type of financing.
Conflict of interestThe authors declare that they have no conflict of interest.
The authors especially thank the patients for their participation in the study; the Instituto Colombiano del Dolor (Colombian Pain Institute) and the human team that supported the data collection process: Y. Barrera, C. Campuzano and M. López.