Smartphone overuse may lead to musculoskeletal manifestations, such as carpal tunnel syndrome (CTS) and arthritis of hand joints, with an increased median nerve cross-sectional area (CSA).
ObjectiveThe aim of this study is the early detection of musculoskeletal hand disorders using ultrasound techniques, and to detect nerve entrapment using clinical evaluation, ultrasound, and electrophysiological studies, in university employees younger than 35 years using mobile phones. Function is assessed using the Michigan Hand Outcomes Questionnaire (MHQ).
Materials and methodsCross-sectional controlled study included 74 smartphone users classified into two groups according to a smartphone addiction scale (SAS), into high and low smart phone users, with 35 non-smartphone users with matched age and gender as a control group. A clinical assessment of nerve entrapment symptoms was performed, and the Michigan Hand Outcomes Questionnaire (MHQ), with a total score from 0 to100, was used to assess hand function. Electrodiagnostic studies of median and ulnar nerves were used to detect early nerve entrapment. Bilateral ultrasound was performed in order to assess the median nerve CSA and involvement of thumb and small hand joints. The data collected were analysed using the SPSS program version 20.
ResultsCSAs of median nerves were significantly higher in the dominant hand of high smartphone users than in low and non-smartphone users (p<0.001). There was a significant positive correlation between CSA and SAS (r=0.45), visual analogue scale (VAS) (r=0.61), and duration of smartphone use (r=0.80), with negative correlation with MHQ (r=−0.63). Significant differences in were found in the electrophysiological studies of median and ulnar nerves. The mean ultrasound score for both hands was higher in the high smartphone users compared to low smartphone users (15.08±4.17 vs. 6.46±1.38, p<.001).
ConclusionsThere is increased median nerve CSAs among high smartphone users associated with prolongation of both sensory and motor latencies and slow conduction velocities. Caution should be exercised when using mobile phones, in order to minimise the risk of developing hand musculoskeletal disorders.
El uso excesivo de teléfonos inteligentes conlleva manifestaciones musculoesqueléticas como el síndrome del túnel carpiano (STC) o la artritis de las articulaciones de las manos, con un aumento del área transversal del nervio mediano (CSA).
ObjetivoEl objetivo de este estudio es detectar oportunamente trastornos musculoesqueléticos de la mano utilizando una ecografía, así como detectar el atrapamiento nervioso mediante estudios clínicos de evaluación, ultrasonográficos y electrofisiológicos en nuestros empleados universitarios menores de 35años que utilizan teléfonos inteligentes, con evaluación del Cuestionario de Resultados de Mano de Michigan (MHQ).
Materiales y métodosEl estudio controlado transversal incluyó a 74 usuarios de teléfonos inteligentes que fueron clasificados en 2 grupos, según la escala de adicción a los teléfonos inteligentes (SAS), en usuarios de teléfonos inteligentes altos y bajos, con 35 no usuarios de teléfonos inteligentes con edad y sexo iguales, como grupo de control. El MHQ se utilizó para evaluar de la función de la mano con una puntuación total de 0 a 100. Se realizaron estudios electrodiagnósticos de la mediana de los nervios y cubitales para detectar el atrapamiento nervioso temprano. La ecografía bilateral se realizó para evaluar la CSA del nervio mediano y la afectación del pulgar y de las articulaciones pequeñas de las manos. Los datos recogidos fueron analizados por la versión 20 del programa SPSS.
ResultadosLas CSA de los nervios medianos fueron significativamente más altas en la mano dominante de los usuarios altos que en los no usuarios bajos de teléfonos inteligentes (p<0,001). Hubo una correlación positiva significativa entre la CSA y SAS (r −0,45), la escala analógica visual (VAS) (r −0,61) y la duración del uso del teléfono inteligente (r −0,80) con la correlación negativa con MHQ (r −0,63). Se encontraron diferencias significativas en los estudios electrofisiológicos de los nervios medios y cubitales. La puntuación ultrasonográfica media para ambas manos fue más alta en altos en comparación con los usuarios de teléfonos inteligentes bajos (15,08×4,17 frente a 6,46×1,38, p<0,001).
ConclusionesExiste una asociación entre la adicción a los teléfonos inteligentes y el área transversal del nervio mediano asociada con el aumento de las CSA entre los usuarios de teléfonos inteligentes altos en comparación con los usuarios bajos y no inteligentes. Se debe tener precaución al usar teléfonos inteligentes para minimizar el riesgo de desarrollo de trastornos musculoesqueléticos de las manos.
Smartphones have a vital role in our life with advantages like internet communication than other devices.1 The rate of smartphone addiction has been very high in the last decades. However, this smartphone addiction can affect our health and cause musculoskeletal manifestations like hand and wrist pain.2
The posture of smartphone use requires fixing the device with hands, looking at the device and the thumb is used to touch the screen.2 Increased duration and frequency of smartphone use with frequent movement of the upper limbs have been found to be major risk factors for musculoskeletal manifestations incidence.3
Musculoskeletal symptoms of smartphone use not only involve the hands but also many areas all over the body including neck, wrists, thumb, and elbows especially with overuse.4 Also, the repeated flexion and extension movements during smartphone use can lead due to narrowing and increase pressure in the carpal tunnel and may lead to carpal tunnel syndrome (CTS). Median nerve is a mixed nerve having contributions from ventral roots of C5–C7 of lateral cord and C8 and T1 of medial cord. Sensory fibers are more prone to damage from nerve compression firstly before the motor fibers.5 In 20–40% of CTS patients, the incidence of pain and paresthesia proximal to the wrist level has been reported. Sensory impairment usually involves palmar surface of the lateral 3½ fingers and spares thenar eminence as the palmar cutaneous sensory branch of the thenar eminence emerges proximal to the carpal tunnel.6 Also, median nerve is mainly involved in muscle movements during smartphone use as it innervates 1st and 2nd lumbrical muscles and thenar muscles by its motor and recurrent branches.4,7
CTS is defined as the most common entrapment neuropathy caused by median nerve compression inside the carpal tunnel.5 The characteristic clinical symptoms of CTS from which we need at least two for diagnosis are nocturnal paresthesias; reproduction of paresthesias or pain by provocative tests (Tinel or Phalen's signs) or aggravation of paresthesias by activities like driving, holding a book or telephone; and relief of symptoms by shaking the hand.8 Electrodiagnostic studies are necessary to confirm CTS diagnosis with electrodiagnostic criteria including, prolongation of the median motor distal latency (MDL) longer than 4.0ms and slowing of nerve conduction velocity (NCV) less than 49m/s with sensory peak latency longer than 3.3ms.9,10
Musculoskeletal ultrasonography is used to assess the cross-sectional area (CSA) of median nerve, but still there is no definitive cutoff value of median nerve CSA to diagnose CTS as it is affected by several demographic factors like height, age, weight, sex, and ethnicity.11 Some studies considered 6.8mm2 as a cutoff point of CSA,11 while others consider 8.5mm2 as a cutoff point,12 and others consider 9mm2 as a cutoff point for median nerve CSA.13
Smartphone overuse affects flexor pollicis longus tendon increasing its thickness, joints of the thumb, hands. Hand musculoskeletal disorders include joint affection such as osteoarthritis of the carpometacarpal joint.14 The aim of this study is to early detect musculoskeletal hand disorders using ultrasonography and detect nerve entrapment using clinical evaluation, ultrasonographic and electrophysiological studies in our university employees younger than 35 years using smartphones with assessment of functional Michigan Hand Outcomes Questionnaire (MHQ).
Materials and methodsStudy design and participantsA cross-sectional controlled study conducted on 74 smartphone users who are employees recruited from our university during the period from March 2018 to July 2019. Their age ranged between 23 and 35 years. The duration of smartphone use is more than 4h per day for more than 6 months, with 35 non smartphone users matched in age and gender as a control group. The study excluded subjects with tendon injuries, radiculopathy, lateral or medial epicondylitis, diabetic patients and patients with hand arthritis or any musculoskeletal problems. The ethical committee guidelines were followed and the study was approved by the ethical committee of our university. An informed consent was obtained from all individuals participating in the study.
ProcedureSmartphone users were classified into two groups according to smartphone addiction scale (SAS): high (SAS>33) and low (SAS<33) smartphone users. Age, gender, dominant hand, and duration of smartphone use in each subject were recorded.15
SAS is a questionnaire with ten items to assess level of smartphone addiction with a 6-point scale from 1 to 6. The total score ranges from 10 to 60, the highest score is the highest smartphone addiction.15
Clinical assessment and functional hand evaluationAll subjects were clinically assessed asking about the symptoms suggestive of nerve entrapment including nocturnal paresthesias, and if it increases with hand activities or not and if shaking of the hand decreases these paresthesias or not. Assessment of the provocation of these paresthesias using the Tinel test in which tapping the nerve in the carpal tunnel elicit pain in median nerve distribution and Phalen's tests in which holding the wrist in flexion for 60s elicit numbness/pain in median nerve distribution was done. These tests are positive upon reproduction of symptoms (numbness, tingling, and pain). Pain felt in the dominant hand during the previous week was recorded on a 10cm visual analog scale (VAS).16
Hand function and disability were assessed by MHQ which includes 12 items with a 1–5 scale. All of the items are totaled and then normalized to obtain a total score from 0 to100. Higher scores indicate better functioning of the hand.17
Electrophysiological studiesBefore starting Electrophysiological studies, temperature should be adjusted and cold hands should be sufficiently warmed with an appropriate method to achieve a surface temperature ≥32°C.18 Before applying the electrodes, 70% alcohol solution was used to clean stimulation and recording areas on the skin.
Median and ulnar nerves electrodiagnostic studies at wrist and elbow were done. Pulse duration of 0.05/0.1 millisecond (ms) was set for sensory nerve stimulation and 0.2/0.5ms for motor nerve stimulation. The filters were set at 20Hz and 2kHz. Sweep speed was 1ms per division. For mixed nerve studies the one-centimeter disc recordings electrodes were used and ring electrodes for sensory studies. A ground electrode was appropriately placed between the stimulating and recording electrodes.19,20 The electrophysiological studies were performed by the same clinician, who was blinded to the SAS scores.
Techniques of electrophysiological studiesMotor NCSOrthodromically median and ulnar nerves stimulation was used. For the median nerve, the active electrodes (A) were placed on the motor point of the abductor pollicus brevis muscle and over the abductor digiti minimi for the ulnar nerve. The reference electrodes (R) were placed 4cm distally over the thumb and 4cm distally over the little finger for the median and ulnar nerves, respectively. The ground electrode (G) is placed on the palm or dorsum of the hand. Distal median motor nerve stimulations were performed 8cm proximal to the A electrode and medial to the flexor carpi radialis tendon. The distal ulnar motor nerve stimulations were performed 8cm proximal to the A electrode medial and posterior to the flexor carpi ulnaris tendon.20,21
Proximal median nerve stimulation is performed over the brachial artery pulse at the antecubital fossa. Proximal ulnar nerve stimulations were performed distal to the medial epicondyle in a position of the upper extremity with the elbow flexion of 90° from horizontal throughout the whole measurement.
Sensory NCSThe median and ulnar nerves were examined antidromically. The second and fifth digits were used to put the active ring electrode to record responses along the median and ulnar nerves, respectively. The reference ring electrode was placed 4cm distal to the active electrode. Median nerve stimulations were performed distally at 14cm proximal to the active electrode and medial to the flexor carpi radialis tendon. Stimulations of ulnar nerve were performed 14cm proximal to the active electrode and posterior to the flexor carpi ulnaris tendon.20,21
For the median nerve, Motor nerve conduction velocities were considered abnormal if less than 49m/s. Distal motor latencies (DML) were considered prolonged if higher more than 4.0ms. Peak latencies were considered abnormal if longer than 3.3ms.9,10,22
For the ulnar nerve, Motor nerve conduction velocities were considered abnormal if below 49m/s. DML were considered prolonged if more than 3.3ms. Peak latencies
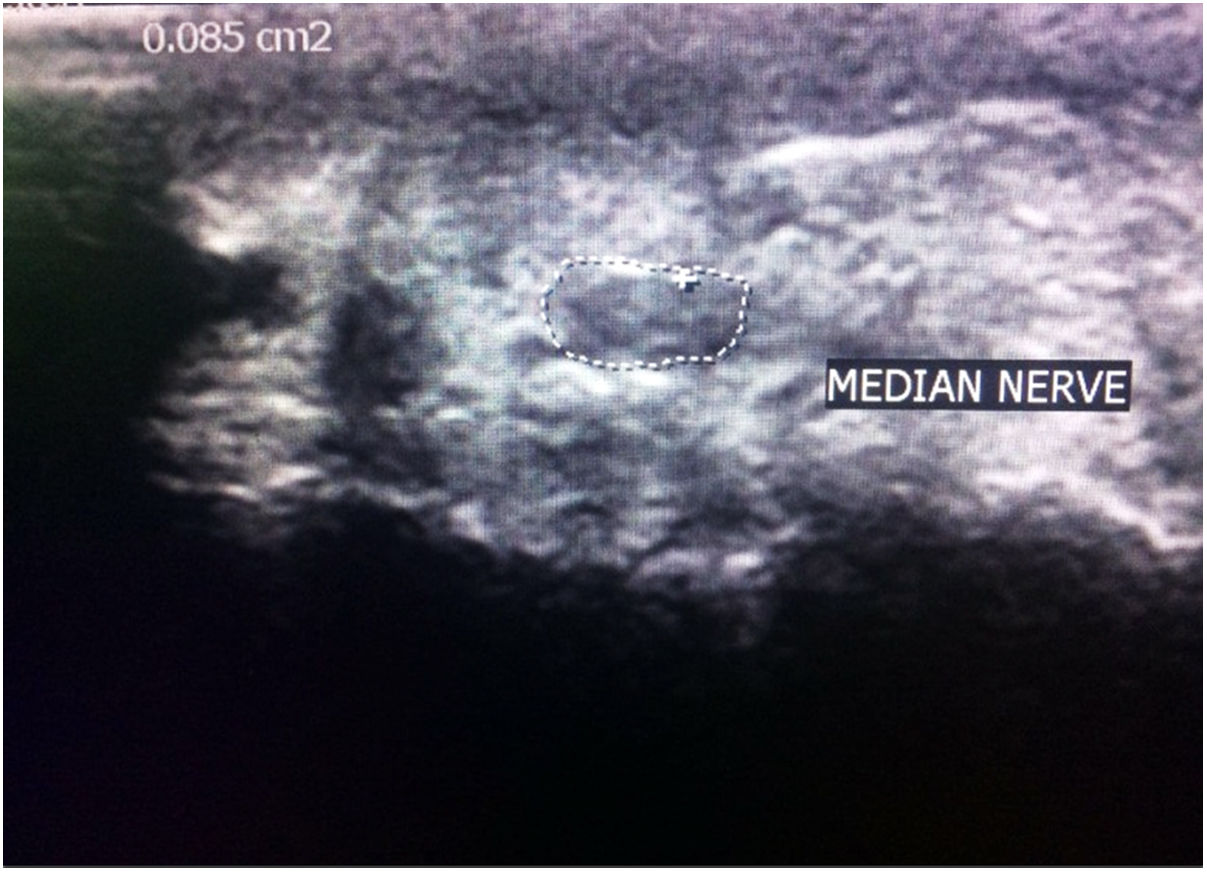
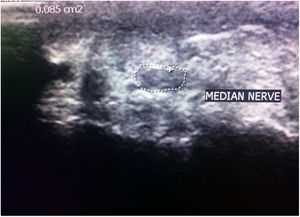
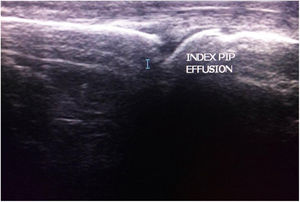
Ultrasonographic evaluationUltrasonographic evaluation of median nerve was done bilaterally with PHILIPS-HD 11 XE linear transducer 7–12MHz array probe placed over the median nerve (Fig. 1). The arms were semi flexed resting on a pillow on the subjects legs with fully supinated hands. CSA of median nerve in mm2 was evaluated just before carpal tunnel entrance with axial imaging.23
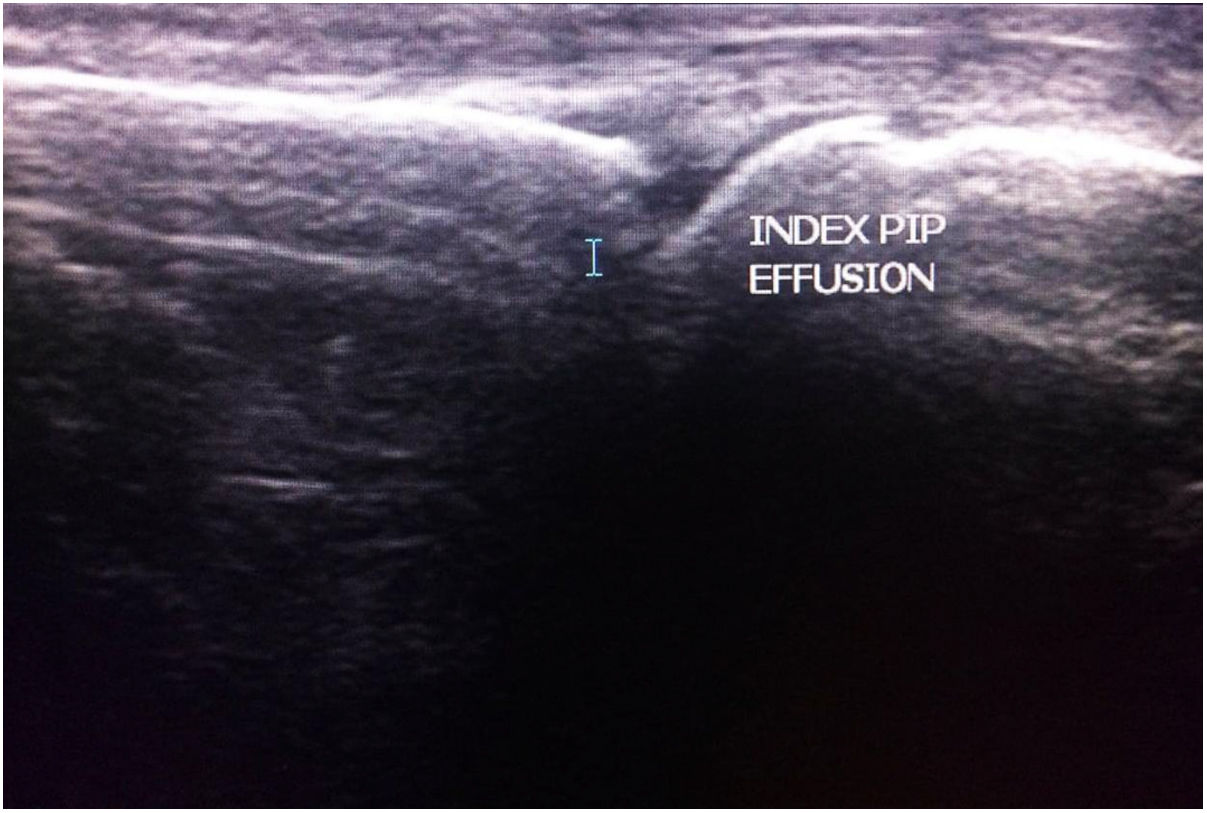
The metacarpophalangeal and interphalangeal joints of the first finger, and the proximal and distal interphalangeal joints of the second, third, fourth and fifth fingers were examined (10 joints per hand examined) (Fig. 2). For each joint, ultrasonographic (U/S) evaluation score with six features (synovial effusion; synovial hypertrophy; tenosynovitis; hyper vascularization; bone erosions; and signs of Enthesopathy) was used assigning 1 point for every feature when present and 0 point when absent (each joint examined has score from 0 to 6; 10 joints examined per hand; so the maximum score for each hand is 60).24 The ultrasound evaluations were performed by the same clinician, who was blinded to the SAS scores.
Statistical analysisThe data collected were analyzed by SPSS program version 20. Student's t-test was used for comparison between groups having quantitative variables. Mann–Whitney test (U) (non-parametric test) was used for comparison between two groups not normally distributed. Chi-squared test (χ2) was used to study association between two qualitative variables. Anova test was used. Pearson correlation coefficient test was used to study the correlation between two quantitative variables. Correlation may be positive (+) or negative (−). Spearman correlation coefficient test (r-test) is used to study the correlation between not normally distributed quantitative variables. p-Value of (>0.05) was considered statistically insignificant. p-Value of (≤0.05) was considered statistically significant. p-Value of (≤0.001) was considered statistically highly significant.25
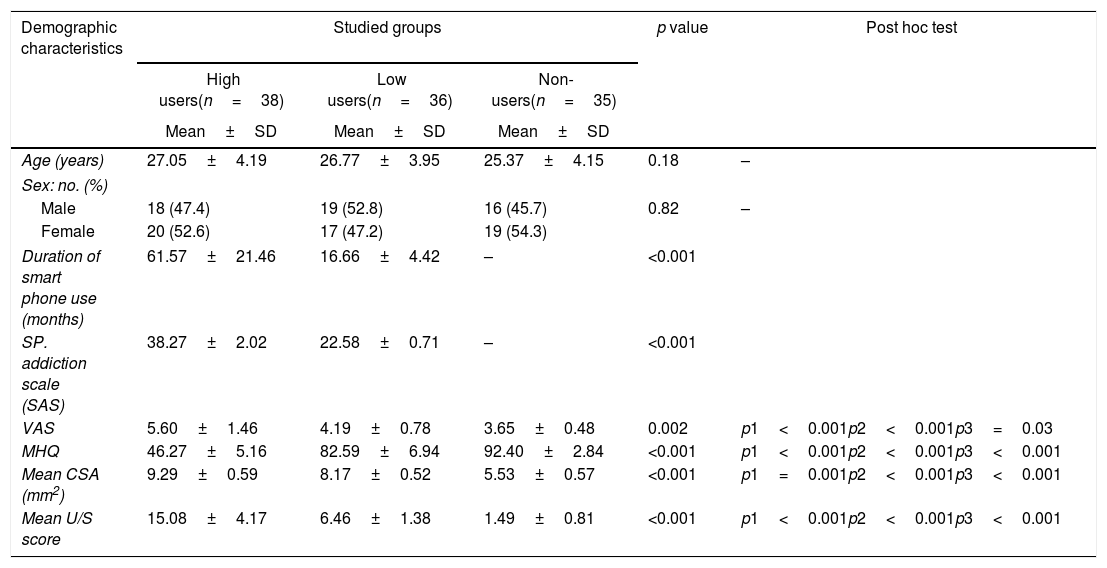
ResultsDemographic and clinical parameters among the studied groupsSeventy four smartphone users were included divided into two groups: high smartphone users 18 male (47.4%), 20 female (52.6%), with a mean age 27.05±4.19 years, low smartphone users 19 male (52.8%), 17 female (47.2%) with a mean age 26.77±3.95 years and non-smartphone users as a control group 16 male (45.7%), 19 female (54.3%) with a mean age 25.37±4.15 years. No significant differences regarding age and gender between the three groups (p=0.18, p=0.82) respectively (Table 1).
Demographic and clinical parameters among the studied groups.
| Demographic characteristics | Studied groups | p value | Post hoc test | ||
|---|---|---|---|---|---|
| High users(n=38) | Low users(n=36) | Non-users(n=35) | |||
| Mean±SD | Mean±SD | Mean±SD | |||
| Age (years) | 27.05±4.19 | 26.77±3.95 | 25.37±4.15 | 0.18 | – |
| Sex: no. (%) | |||||
| Male | 18 (47.4) | 19 (52.8) | 16 (45.7) | 0.82 | – |
| Female | 20 (52.6) | 17 (47.2) | 19 (54.3) | ||
| Duration of smart phone use (months) | 61.57±21.46 | 16.66±4.42 | – | <0.001 | |
| SP. addiction scale (SAS) | 38.27±2.02 | 22.58±0.71 | – | <0.001 | |
| VAS | 5.60±1.46 | 4.19±0.78 | 3.65±0.48 | 0.002 | p1<0.001p2<0.001p3=0.03 |
| MHQ | 46.27±5.16 | 82.59±6.94 | 92.40±2.84 | <0.001 | p1<0.001p2<0.001p3<0.001 |
| Mean CSA (mm2) | 9.29±0.59 | 8.17±0.52 | 5.53±0.57 | <0.001 | p1=0.001p2<0.001p3<0.001 |
| Mean U/S score | 15.08±4.17 | 6.46±1.38 | 1.49±0.81 | <0.001 | p1<0.001p2<0.001p3<0.001 |
N=number, VAS=visual analog scale, MHQ=Michigan hand outcomes questionnaire, CSA=cross sectional area, p1: between high users group and low users group, p2: between high users group and non- users group, p3: between low users group and non-users group, (p-value>0.05) is non-significant, (p-value≤0.05) is significant and (p-value≤0.001) is highly significant.
The VAS was significantly higher in the high than the low and non-smartphone user groups (5.60±1.46, 4.19±0.78 and 3.65±0.48) respectively (Table 1).
Ultrasonographic scores of both hands, were significantly higher in high compared to low and non-smartphone users (15.08±4.17, 6.46±1.38, 1.49±0.81, p<0.001) respectively (Table 1).
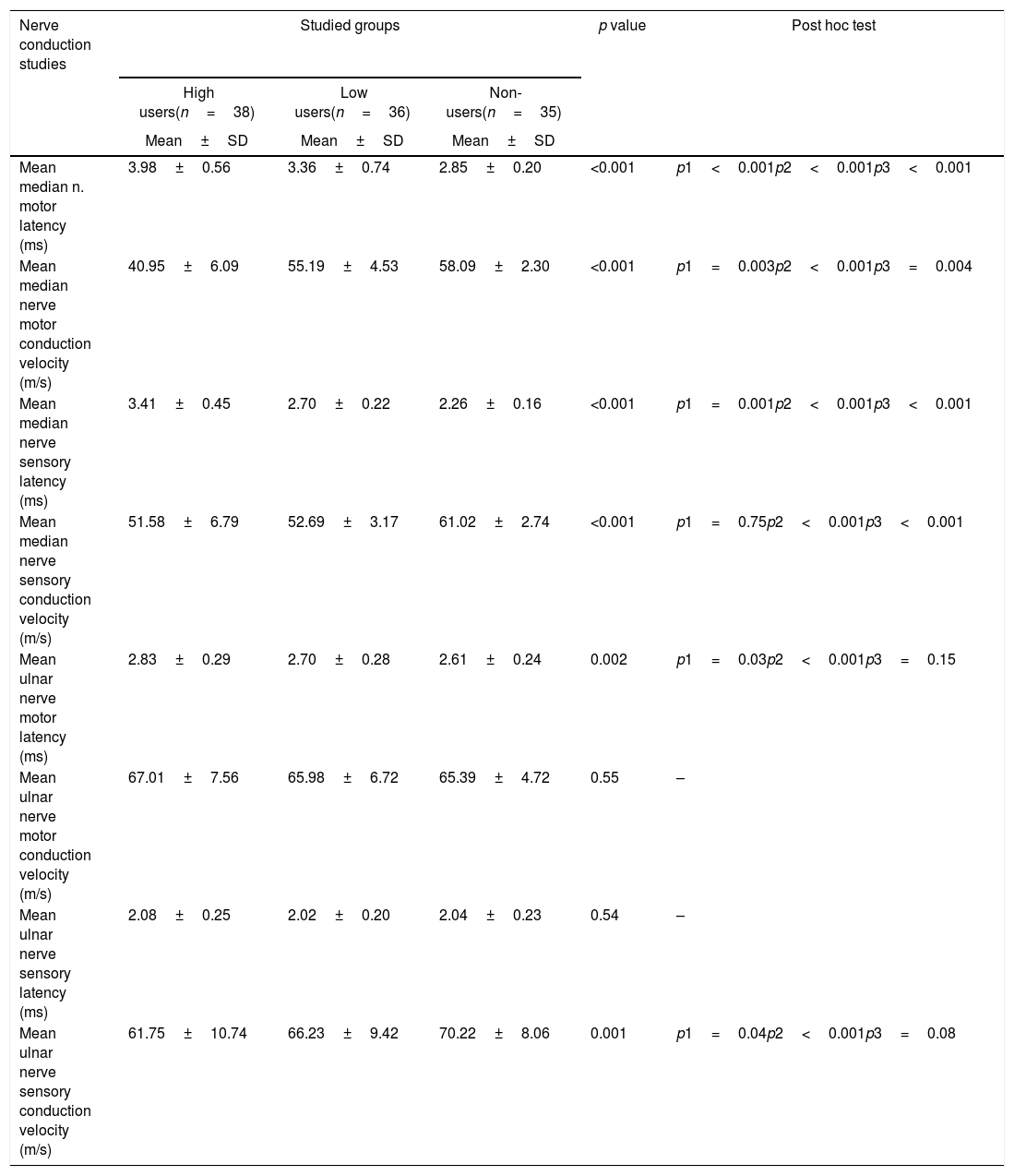
Nerve conduction studies among the studied groupsNerve sensory and motor conduction velocities and sensory and motor latencies of median nerve were compared, there were significant differences between the high, low, and non-smartphone users with non-significant differences of the ulnar nerve between the studied groups regarding motor conduction velocity and sensory latency (p=0.55, p=0.54) (Table 2).
Nerve conduction studies among the studied groups.
| Nerve conduction studies | Studied groups | p value | Post hoc test | ||
|---|---|---|---|---|---|
| High users(n=38) | Low users(n=36) | Non-users(n=35) | |||
| Mean±SD | Mean±SD | Mean±SD | |||
| Mean median n. motor latency (ms) | 3.98±0.56 | 3.36±0.74 | 2.85±0.20 | <0.001 | p1<0.001p2<0.001p3<0.001 |
| Mean median nerve motor conduction velocity (m/s) | 40.95±6.09 | 55.19±4.53 | 58.09±2.30 | <0.001 | p1=0.003p2<0.001p3=0.004 |
| Mean median nerve sensory latency (ms) | 3.41±0.45 | 2.70±0.22 | 2.26±0.16 | <0.001 | p1=0.001p2<0.001p3<0.001 |
| Mean median nerve sensory conduction velocity (m/s) | 51.58±6.79 | 52.69±3.17 | 61.02±2.74 | <0.001 | p1=0.75p2<0.001p3<0.001 |
| Mean ulnar nerve motor latency (ms) | 2.83±0.29 | 2.70±0.28 | 2.61±0.24 | 0.002 | p1=0.03p2<0.001p3=0.15 |
| Mean ulnar nerve motor conduction velocity (m/s) | 67.01±7.56 | 65.98±6.72 | 65.39±4.72 | 0.55 | – |
| Mean ulnar nerve sensory latency (ms) | 2.08±0.25 | 2.02±0.20 | 2.04±0.23 | 0.54 | – |
| Mean ulnar nerve sensory conduction velocity (m/s) | 61.75±10.74 | 66.23±9.42 | 70.22±8.06 | 0.001 | p1=0.04p2<0.001p3=0.08 |
m/s=meter per second, ms=millisecond.
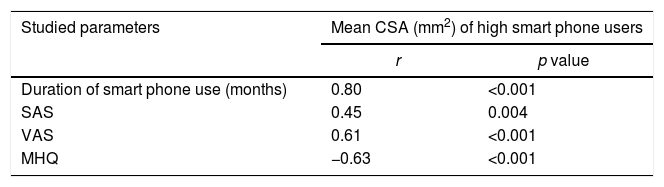
There was significant positive correlation between CSA and SAS, duration of smartphone use and VAS with negative correlation with MHQ in high smartphone users (r=0.45, p=0.004; r=0.80, p=<0.001; r=0.61, p<0.001; r=−0.63, p=<0.001), respectively (Table 3).
Correlation between CSA and SAS, VAS, MHQ and duration of smart phone use in high smart phone user group.
| Studied parameters | Mean CSA (mm2) of high smart phone users | |
|---|---|---|
| r | p value | |
| Duration of smart phone use (months) | 0.80 | <0.001 |
| SAS | 0.45 | 0.004 |
| VAS | 0.61 | <0.001 |
| MHQ | −0.63 | <0.001 |
SAS=smart phone addiction scale, VAS=visual analog scale, MHQ=Michigan Hand Outcomes Questionnaire, CSA=Cross sectional area.
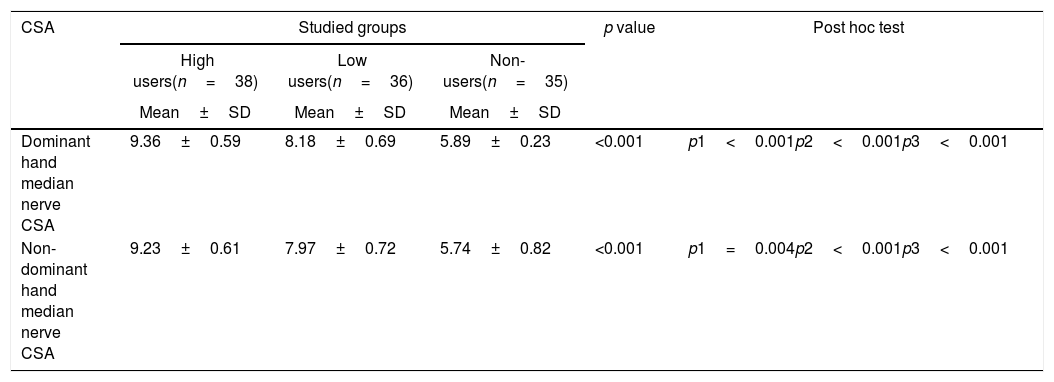
CSAs of median nerves were significantly higher in the dominant hands of the studied groups (9.36±0.59, 8.18±0.69, 5.89±0.23) compared to the non-dominant hands (9.23±0.61, 7.97±0.72, 5.74±0.82), respectively with the highest CSAs in the dominant hand of high smartphone users (9.36±0.59, p<0.001) (Table 4).
Comparison of CSAs of the dominant and non- dominant hands of the studied groups.
| CSA | Studied groups | p value | Post hoc test | ||
|---|---|---|---|---|---|
| High users(n=38) | Low users(n=36) | Non-users(n=35) | |||
| Mean±SD | Mean±SD | Mean±SD | |||
| Dominant hand median nerve CSA | 9.36±0.59 | 8.18±0.69 | 5.89±0.23 | <0.001 | p1<0.001p2<0.001p3<0.001 |
| Non-dominant hand median nerve CSA | 9.23±0.61 | 7.97±0.72 | 5.74±0.82 | <0.001 | p1=0.004p2<0.001p3<0.001 |
CSA=Cross sectional area.
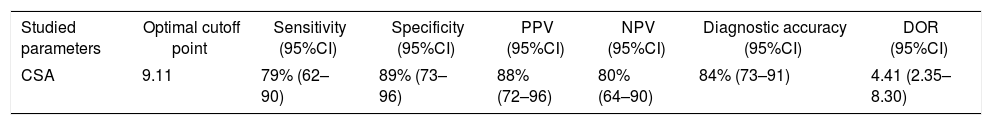
The optimal cutoff point of CSA was 9.11 with sensitivity of 79%, specificity of 89%, diagnostic accuracy of 84% and 95% confidence interval (CI) (Table 5). We evaluated those patients with delayed electrophysiological studies with those with high CSA of median nerve. We found that most patients with clinical suggestion of nerve entrapment already had abnormal electrophysiological studies of median nerve with increased CSA.
Clinical performance of CSA in high smart phone users.
| Studied parameters | Optimal cutoff point | Sensitivity (95%CI) | Specificity (95%CI) | PPV (95%CI) | NPV (95%CI) | Diagnostic accuracy (95%CI) | DOR (95%CI) |
|---|---|---|---|---|---|---|---|
| CSA | 9.11 | 79% (62–90) | 89% (73–96) | 88% (72–96) | 80% (64–90) | 84% (73–91) | 4.41 (2.35–8.30) |
95% CI=95% confidence interval, PPV=Positive predictive value, NPV=Negative predictive value, DOR=diagnostic odds ratio.
Smartphone use has been significantly increased nowadays with both negative and positive advantages. it enables its users to easily communicate with others and send e-mails26 and has been used in medicine especially for drug-addicted or psychiatric patients.26,27
However musculoskeletal symptoms like De-Quervain tenosynovitis may develop in smartphone users. Frequent uses of smartphones and the repeated movements of the hands are the main contributing factors for these musculoskeletal symptoms. Also enlargement of the median nerve, thumb and upper trapezius pain, decreased pinch strength and hand functions, neck disability are musculoskeletal disorders associated with smartphone use.4,13
The prolonged wrist flexion and use of the thumb in a static posture increase the load on its joints, associated muscles and tendons and this explains the ultrasonographic findings of the thumb and hand joints in high smartphone users as documented in this study (15.08±4.17) (Table 1).
Ultrasonographic musculoskeletal disorders were variably distributed among our subjects especially synovitis, tenosynovitis and synovial effusion. No one of the studied subjects had bone erosion.
Xie et al., 2016 and Lippi et al., 2016 reported high U/S hand scores in high smartphone users.28,29 In the other line Koldas et al., 2011 found non-significant differences in ultrasonographic hand scores between high, low and non-smart phone users. This may be contributed to the small number of studied subjects with short duration of smartphone use not affecting their hand joints.30
In this study there was median nerve entrapment in the form of prolonged distal motor latencies and slow conduction velocities in high smart phone users (15 out 38), those patients have the characteristic clinical symptoms suggestive of nerve entrapment with CSA more than 9.11 (cut off point) and fulfilled the electrodiagnostic criteria of nerve entrapment. Ahamed et al., 2015 reported a prevalence of 35.3%.31 You et al., 2014 reported a very high prevalence of nerve entrapment (50%) in high smart phone users.32 This high prevalence is because they included patients who are manual workers and the occupational factors are known to cause nerve entrapment, but in our study we assess young population excluding any risk factors for nerve entrapment.
Significant affection of median nerve is contributed to repeated wrist flexion and extension with prolonged smartphone use which increases the carpal tunnel pressure and decreases the space available for the median nerve inside the carpal tunnel.13 In this study; decreased motor and sensory conduction velocities (40.95±6.09, 51.58±6.79) and prolonged motor and sensory distal latencies (3.98±0.56, 3.36±0.74) in high smart phone users were found. (Table 2)
Several studies have proven the effect of smartphone use on the median nerve as studies by Inal et al., 2015 and Chammas et al., 2014.33 Chammas et al., 2014 reported decreased conduction velocities among the studied groups (51.93±6.32, 54.38±6.42, 58.24±3.53) respectively and prolonged distal motor latencies in high (3.55±0.55) compared to low (3.31±0.41) and non-smartphone users (2.90±0.34).10
In contrast to this study the studies by Chen et al., 2016 and Dillingham et al., 2016. Chen et al., 2016 reported significant differences in all parameters of the ulnar nerves between high and low smart phone users (p=0.001, p=0.003) respectively with non-significant affection of the median nerves (p=0.854, p=0.108), respectively.34,35 This is explained by the origin of both nerves as the ulnar nerve origin is C8, T1 nerve roots which are completely compressed by neck flexion while median nerve origin is C5, C6, C8, and T1 which are partially compressed by the neck flexion.36
This can be explained by the double crush theory which is defined as compressive neuropathy of nerve axon affecting its function because of impaired axoplasmic flow, at 2 distinct sites: proximal in the C-spine, and distal in the cubital tunnel, carpal tunnel, or elsewhere causing disabling pain, numbness, and weakness in the ambulatory and functioning patients. The double crush concept has gained some popularity because it seems to provide a rationale for evaluating the condition of the cervical spine and roots when treating CTS.36
Regarding ulnar nerve dysfunction, the association of a peripheral ulnar neuropathy and cervical radiculopathy (CR) has also been reported. In patients diagnosed with DCS with both cubital tunnel syndrome and CR, have a poorer outcome due to several factors including that ulnar nerve symptoms present for more than a year, multiple electrophysiological studies diagnosed neuropathies and radiculopathies, and anterior cervical discectomy and arthrodesis performed before ulnar nerve release.37
Investigations for DCS are important, as it is a clinically significant consideration which makes the treatment results of patients complaining of upper limbs symptoms less predictable.
Several aspects of smartphone use such as duration, tasks for use and positions during smartphone use cause chronic neck and hand pain and so affecting functional status of the hands causing disability. Our study reported the significant positive correlation between mean CSAs of median nerves and SAS, VAS and duration of smartphone use with negative correlation with MHQ. Pain was more severe with poor hand function and disability in high smartphone users (Table 3).
Ali, Asim et al., 2014 and Inal et al., 2015 reported that the pain was more severe with functional hand impairment in high smartphone users.33,38 Also Inal et al., 2015 found significant positive correlation between SAS and VAS (p<0.05, r=0.345).33 Kim et al., 2016 reported the significant association between the CSAs of median nerves and duration of smart phone use (p<0.05).39
Repeated and sustained wrist flexion with smartphone over use increases the load on the median nerve inside the carpal tunnel and causing increase in its CSAs. This study showed significantly higher CSAs of median nerves in the dominant hands of the three studied groups (9.36±0.59, 8.18±0.69, 5.89±0.23) more than the non-dominant hands (9.23±0.61, 7.97±0.72, 5.74±0.82), respectively with the highest CSAs in the dominant hand of high smartphone users (9.36±0.59, p<0.001) (Table 4).
Inal et al., 2015 and Akkaya et al., 2015 reported enlargement of median nerves in the dominant hands of high smartphone users.33,40 Inal et al., 2015 reported the high CSAs of median nerve in high smart phone users (6.9±1.7, p=0.058) compared to low (6.7±1.2) and non-smartphone users (6.3±1.0).33
Ultrasonographic measurement of median nerve CSA had a considerable variability in diagnostic accuracy of sonographic imaging for carpal tunnel syndrome.13 Median nerve CSA has a wide range (4-12mm2),11 Study by Hersh et al used a 6.8mm2 as a cutoff point of median nerve CSA11 while studies by Mohammadi et al and Boehm et al used 8.5mm2 as a cutoff point of median nerve CSA reporting that it is the best cutoff value of CSA at the tunnel inlet and outlet.12,41 Another study by Klauser et al reported a cutoff value of 8.3mm2.42 In this study, the cut off point for the CSA of median nerve was 9.11 (Table 5).
So, in this study we found that high smartphone users at high risk for developing hand musculoskeletal disorders especially median nerve entrapment,they have high SAS, VAS, prolonged distal motor latency and peak sensory latency with slow conduction velocity and poor hand function represented by low MHQ.
ConclusionIncreased median nerve CSAs among high smartphone users associated with prolongation of both sensory and motor latencies and slow conduction velocities. Caution should be taken upon using smartphones to minimize the risk of development of hand musculoskeletal disorders.
Limitations of the studyThis study has some limitations including the relatively small number of population. The cross-sectional design may lead to false-positive or false-negative results.
Availability of data and materialsThe datasets during and/or analyzed in this study are available from the corresponding author on request.
Authors’ contributionAll authors whose names appear on the submission
1) Made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data; or the creation of new software used in the work.
2) Drafted the work or revised it critically for important intellectual content.
3) Approved the version to be published; and
4) Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
FundingThis research did not receive any specific grant from funding agencies in the public or commercial sectors.
Conflict of interestNone.