The Pierre Robin syndrome, or sequence, is a triad characterised by micrognathia, glossoptosis and upper respiratory obstruction, with or without cleft palate. Most patients respond to postural treatment, although tracheotomy is necessary on extreme occasions. Mandibular distraction is currently an effective therapeutic alternative that elongates the jaw and resolves the respiratory obstruction. The choice of vector for distraction is essential for modifying the dimensions of the airways.
Patients and methodsThe objective of this study is to evaluate the changes produced in the dimensions of the upper airways in eight children with Pierre Robin sequence, treated with mandibular distraction, depending on the vector of distraction planned. To this end, a lateral cranial X-ray was performed pre- and post-distraction, tracing a line from the mandibular plane to the base of the tongue and as far as the posterior pharyngeal wall, measuring the millimetres of separation between the two structures.
Results and conclusionsThe results showed that the horizontal distraction vector, in the first place, and the oblique vector in the second place, would be the procedures of choice in view of their positive effects on the airways.
La secuencia de Pierre Robin es una tríada caracterizada por micrognatia, glosoptosis y obstrucción respiratoria alta con o sin paladar hendido. La mayoría de los pacientes responden al tratamiento postural, aunque en ocasiones extremas hay que realizar traqueotomía. En la actualidad la distracción mandibular es la alternativa eficaz de tratamiento que elonga la mandíbula y resuelve la obstrucción respiratoria. La elección del vector de distracción es importante en los cambios de dimensión de la vía aérea.
Pacientes y métodosEl objetivo del estudio es evaluar los cambios producidos en las dimensiones de la vía aérea superior en 8 niños, con secuencia de Pierre Robin, tratados con distracción mandibular dependiendo del vector de distracción planificado. Para ello realizamos una radiografía lateral de cráneo pre y posdistracción, trazamos una línea que une el plano mandibular con la base de la lengua hasta la pared posterior de la faringe y medimos los milímetros de separación entre ambas estructuras.
Resultados y conclusionesAnalizando los resultados obtenidos, el vector de distracción horizontal en primer lugar y en segundo lugar el oblicuo son de elección por su repercusión positiva en la vía aérea.
Pierre Robin sequence is a triad characterised by micrognathia, glossoptosis and airway obstruction with or without cleft palate.1 Its incidence is 1:8500 to 1:30,000 live births.2 It is frequent in members of the same family. 25% of patients with Pierre Robin sequence may present alterations in deglutition and breathing.3
In the Pierre Robin sequence, altered mandibular development appears to be the initial condition, which is altered during the development of the embryo at about the 7th and 11th week of gestation. The position of the jaw towards the back keeps the tongue in a higher position, which prevents the joining of the palate plates, causing a cleft palate. Mandibular micrognathia may cause a downward displacement of the tongue (glossoptosis) towards the pharynx, causing airway obstruction,4,5 with clinical manifestations ranging from a minor breathing difficulty to severe respiratory distress with cyanosis.
The Pierre Robin sequence develops in an isolated manner, but it may sometimes be associated with different syndromes, the most frequent being Stickler (44%), velocardiofacial (7%), craniofacial microsomia (3%) and Treacher-Collins (5%).6,7
The upper airway of a new-born is smaller and anatomically different to the upper airway of an adult. The tongue is relatively bigger, completely occupying the oral and oropharyngeal cavity. Newborns have narrow external nares and breathe only through the nose, since the epiglottis is in a very high position, very close to the soft palate, causing oral breathing difficulty; also in the new-born, the tongue is at the level of C3-4, while in adults it is at the level of C4-5.8 In patients with Pierre Robin sequence, since the jaw is smaller, the tongue is retracted, making the pharynx size even smaller.
In the Pierre Robin sequence, there are several functional mechanisms causing airway obstruction9: (1) backward displacement of the tongue, (2) in this position, it compresses the soft palate and takes it closer to the posterior pharyngeal wall, thus obstructing the airflow, (3) displacement of the lateral pharyngeal walls, and (4) the pharynx contracts as a sphincter.
Airway obstruction can cause hypoxia, hypercapnia, acidosis, development problems, daily drowsiness, inability to gain weight, malnutrition and, if not treated, it may lead to exhaustion, cardiac failure and, finally, death.
The treatment of Pierre Robin sequence may be from a conservative therapy to surgical treatment. Most of these children can improve by being placed in a prone decubitus position until proper growth of the mandible to bring the tongue forward and clear the airway.10 In patients with severe mandibular hypoplasia and obstructive crisis, surgical treatment is necessary, such as glossopexy, tracheostomy or mandibular distraction osteogenesis.11,12 A tracheotomy treatment is associated in the long term with a high rate of morbidity and even mortality; also, logically, there are alterations in the learning of the language and social integration.13
McCarthy was the first to use mandibular distraction osteogenesis to elongate the jaw, move the base of the tongue forward, enlarge the retropharyngeal space and improve the airway obstruction.14
The distraction osteogenesis has many advantages over traditional mandibular advancement osteotomies. We can achieve advances of 20mm or more with no bone grafts.15,16 There is consensus that distraction osteogenesis is superior to other techniques because it is a gradual biological process, with positive effects on muscles, nerves and soft tissues. The newly generated bone will be of a better quality bone and can be modelled, and it is a rehabilitation technique for severe craniofacial malformations that we can use at any stage of life.
The distraction vector is critical to the success of the mandibular distraction. The osteotomy site will depend on the distraction vector. However, some anatomical structures must be avoided, such as dental roots,17 the inferior dental nerve and the lingual nerve, as well as germs. Likewise, depending on the vector planned, we can obtain significant changes in the size of the airway.
Materials and methodsIn this study, we have reviewed 8 paediatric patients with diagnosis of life-threatening severe obstructive apnoea, secondary to micrognathia, which were subject to mandibular distraction after failure of traditional treatments, including prone decubitus position, nasopharyngeal intubation and in the case of a premature girl with Treacher-Collins syndrome who was subject to an emergency tracheotomy.
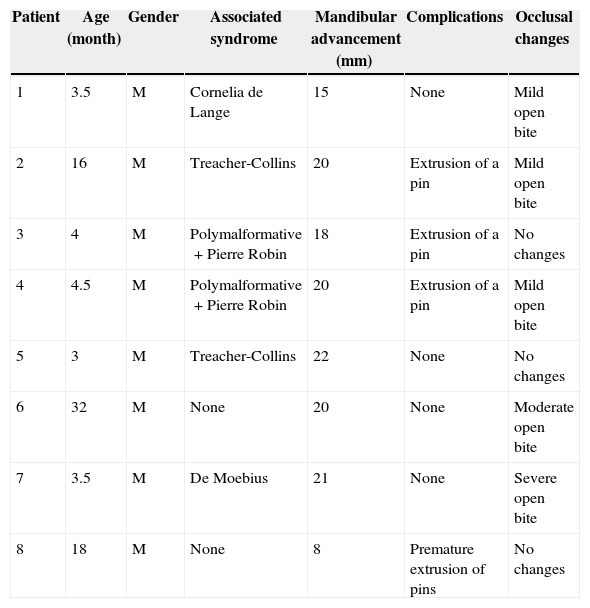
Patients’ data are gathered in Table 1.
Patients data.
| Patient | Age (month) | Gender | Associated syndrome | Mandibular advancement (mm) | Complications | Occlusal changes |
|---|---|---|---|---|---|---|
| 1 | 3.5 | M | Cornelia de Lange | 15 | None | Mild open bite |
| 2 | 16 | M | Treacher-Collins | 20 | Extrusion of a pin | Mild open bite |
| 3 | 4 | M | Polymalformative+Pierre Robin | 18 | Extrusion of a pin | No changes |
| 4 | 4.5 | M | Polymalformative+Pierre Robin | 20 | Extrusion of a pin | Mild open bite |
| 5 | 3 | M | Treacher-Collins | 22 | None | No changes |
| 6 | 32 | M | None | 20 | None | Moderate open bite |
| 7 | 3.5 | M | De Moebius | 21 | None | Severe open bite |
| 8 | 18 | M | None | 8 | Premature extrusion of pins | No changes |
All patients had a Pierre Robin sequence; 6 of them were of syndromic and 5 were associated with cleft palate. A severe difficulty for feeding was detected, which in 4 cases required gastrostomy, in 2 cases feeding through nasogastric catheter and in other 2 cases the feeding was with liquid consistency. Although one patient was more than 18 months and the other more than 2.5 years, a mandibular distraction was performed on these 2 patients due to severe deglutition deficit in absence of clinical signs of obstruction.
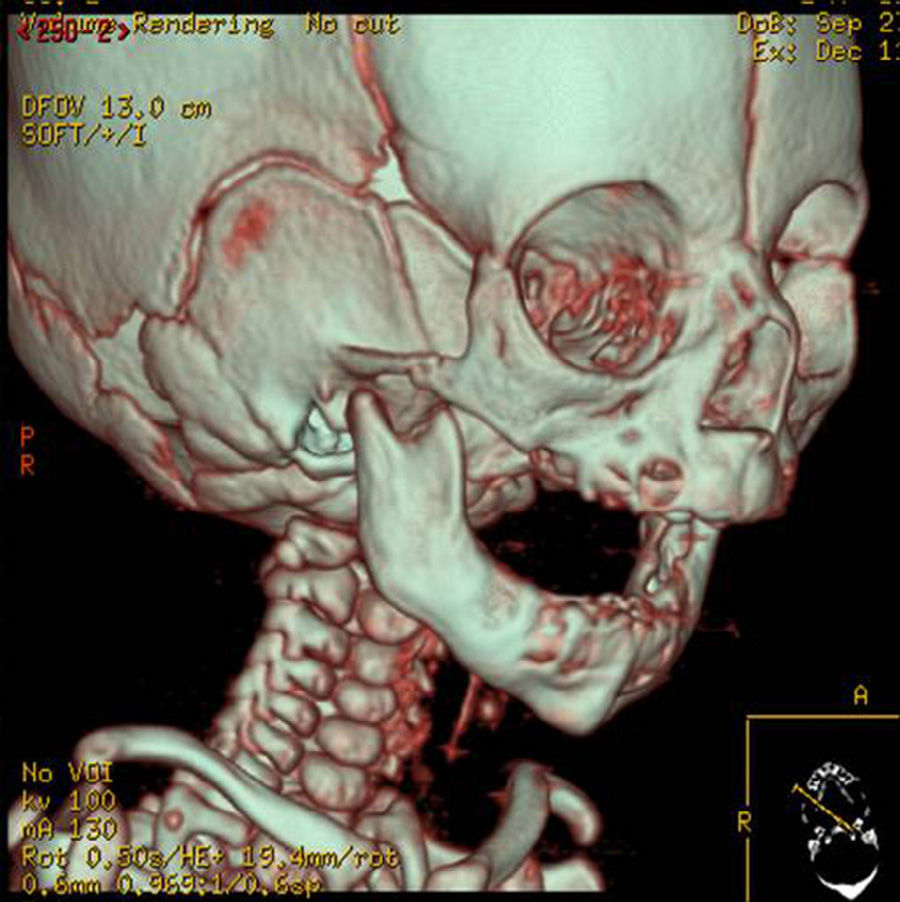
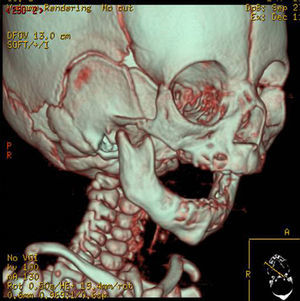
In the clinical examination, we diagnosed the severe mandibular hypoplasia. The severity of the respiratory insufficiency was revealed through oxygen saturation monitoring, which was approximately 40% in prone decubitus. The temporomandibular joint was also assessed (many micrognathia patients have variable grade limitations in mouth opening, directly related to morphological condyle alterations, mechanical factors secondary to the short length of the mandibular body or some degree of joint ankylosis). In all cases we found a limited opening of the mouth due to the short length of the mandibular body and branch. Within supplementary diagnosis studies, a polysomnography was carried out, which was pathological, lateral cranial X-ray to measure the distance of the base of the tongue to the posterior pharyngeal wall, and 2D and 3D CT scans were performed (Fig. 1), which revealed the severity of the hypoplasia. Also, ORL performed a fibroscopical examination to rule out that the cause of the obstruction was glottal or supraglottal. Clinical pictures were taken to document the cases.
The purpose of our study was to assess the changes in airway size after mandibular advancement in patients with obstructive apnoea secondary to micrognathia and treated with mandibular distraction. We have related those changes to the distraction vector planned for each case. To do so, we performed a pre and post-distraction lateral cranial X-ray, and we traced a line joining the mandibular plane to the base of the tongue up to the posterior pharyngeal wall and measured the millimetres separating both structures.
Surgical techniqueIn the 8 cases, a bilateral mandibular distraction was performed through the Molina Uni-diret. Distractor: KLS Martin Group, as described by Fernando Molina and Ortiz Monasterio.18
Under general anaesthesia, an incision of approximately 1.5cm is made in the mucosa along the retromolar area, via intraoral management, to expose the mandibular angle and the initial area of the ascending branch. The dissection must be limited to avoid injury of the vascularisation of the already hypoplastic jaw. The osteotomy site and the place where the pins of the distractor will be inserted are marked with a pen. This is a crucial moment, since the site where pins will be inserted will determine the distraction vector and their position must avoid damage to the mandibular nerve and dental germs.
In the first few cases, we used a fissure drill for the osteotomy, and in the last few cases we used a piezoelectric scalpel. It begins in the retromolar region, severing first the side and medial walls. Then it extends to all the lateral area of the mandibular angle in its most basal portion, where the bone is harder and thicker. When all the exterior corticotomy has been made and the bleeding cancellous bone is exposed, the bone cutting stops. A few millimetres of inner cortical bone are preserved, which is the area protecting both the nerve and the mandibular artery.
The distraction vector planned was oblique in 5 cases and horizontal in 3 cases.
All this was performed bilaterally, inserting, lastly, 2 pins percutaneously, one at each side of the osteotomy. These are always bicortal, controlling through digital palpation that they perforate the lingual cortical plate. They must be very stable to avoid a relatively frequent complication that is losing the pins during the distraction process. The insertion distance of the pins from the osteotomy must be at least 3 to 5mm. To minimise scars, we must take a fold of skin before introducing the second pin to decrease skin tension.
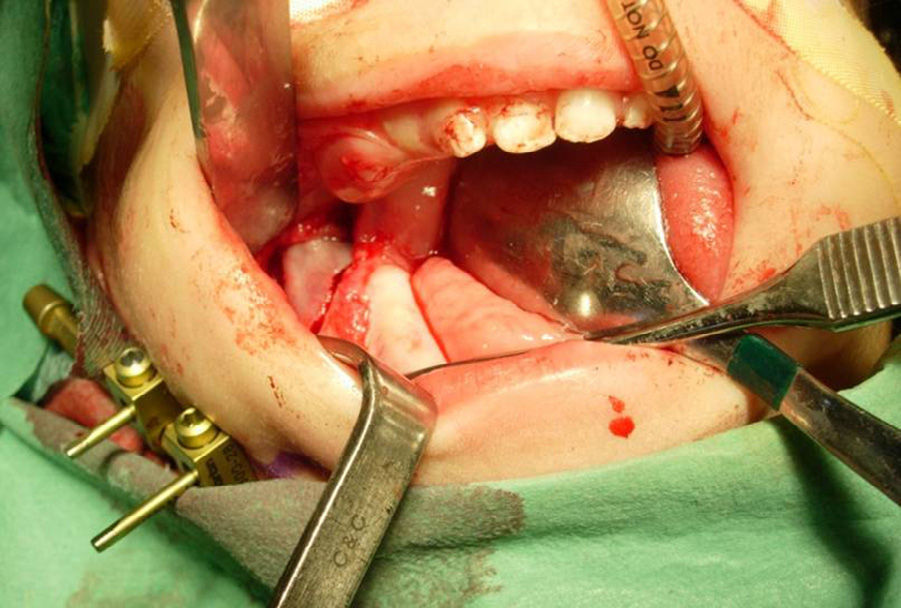
The pins must be parallel to each other to facilitate the introduction and fixing of the distractor. The distractor is activated intraoperatively 3–4mm, verifying there is no cortical bridge preventing mandibular elongation. Then they are deactivated until the active distraction period begins. The incision is closed with absorbable suture (Fig. 2).
The immediate postoperative period continues in a paediatric intensive care unit.
The latency period is from 2 to 3 days and the distraction begins at a rate of 1mm/day; 0.5mm/12h, and there is immediately a sagittal advancement of the mandible and of the base of the tongue. The support period was 4 weeks for patients of less than 6 months and 6 weeks for patients of more than 6 months.
Distractors are easily withdrawn, and patients do not need to be admitted.
ResultsMost of the patients needed, since birth, prolonged admissions into the neonatal intensive care unit until they were treated with mandibular distraction, due to low oxygen saturation levels and fragile clinical situation. The growth and weight gain were scarce. In 2 cases there was severe malnutrition due to the impossibility of deglutition. A gastrostomy in the neonatal period was performed in 4 of those cases (Fig. 3).
The induction of anaesthesia and intubation were performed via fibroscopy and by an anaesthetist specialised in paediatric patients and fibroscopy in patients with predictive criteria for complex airway. There was one patient who could not be intubated after several attempts, and the surgery was postponed for one week later.
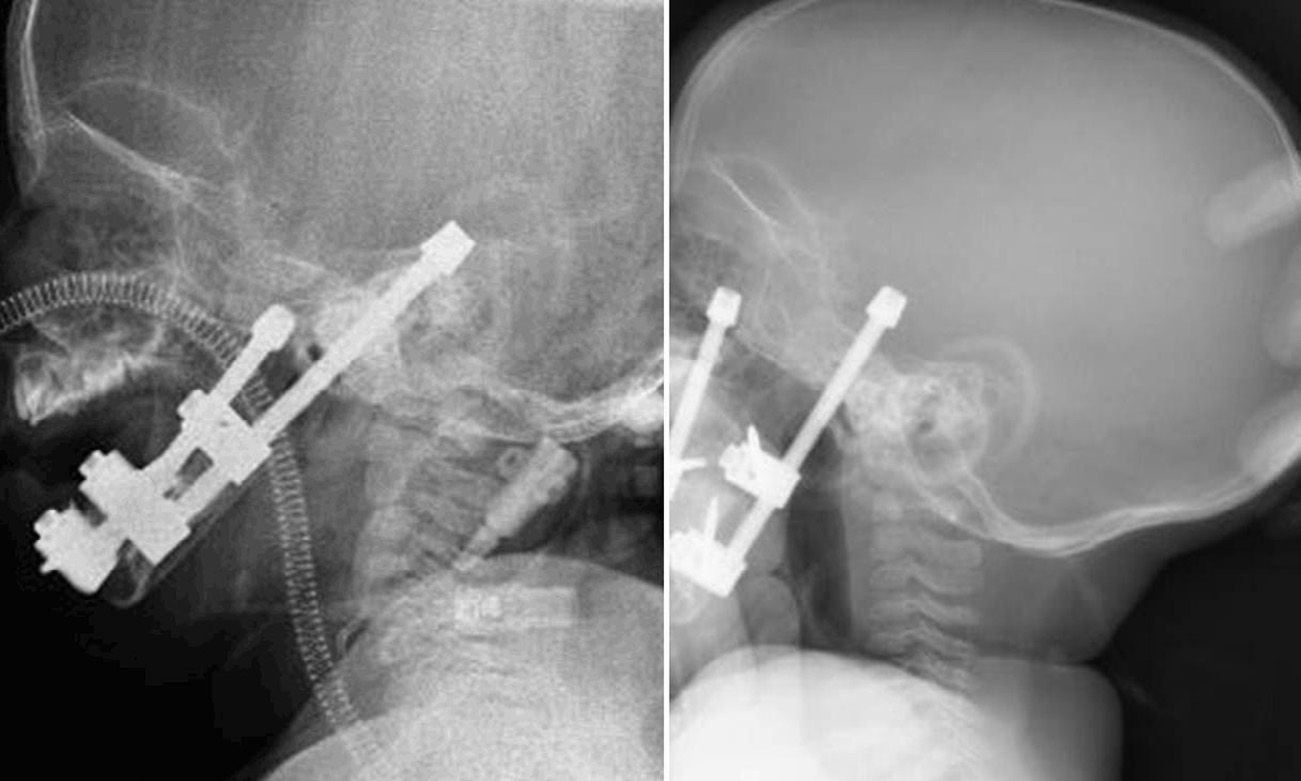
An endotracheal tube was left in the postoperative period and withdrawn once post-surgery oedema disappeared and 4–6 days after the beginning of distraction, since the mandibular elongation attained and its positive repercussion in the airway caused the oxygen saturation levels to normalise. In the patient with Treacher-Collin syndrome previously tracheotomised, the cannula was kept until 2 weeks after the beginning of distraction (Fig. 4).
The mandibular distraction began 3 days after insertion of the distractors at a rate of 1mm/day; 0.5/12h. The elongation rate obtained was 15–22mm. An overcorrection was performed in all cases. In 3 cases there were no occlusal changes, in 3 cases there was a mild anterior open bite which closed spontaneously after the support period, once the distractors were removed; in one case the open bite was moderate, and since the patient was on the deciduous teething period, brackets were placed and the bite was closed with elastic bands (Fig. 5). One patient with Moebius syndrome had a severe open bite; the parents were recommended to use a big pacifier so that the suction reflex and the attempt to keep the pacifier in the mouth make the perioral muscles exercise the strength contrary to the mandible translation vector and thus favour the closing of the bite. Also, due to its big muscular tone, diazepam was prescribed with a paediatric dose. In the case of the 18-month old patient, the desired advance was not attained, since after opening the device 8mm at a rate of 0.5mm/12h it stopped working, in other words, although it was activated, there was no more bone elongation. This led us to believe that the osteotomy was incomplete and/or that the pins were loose inside the bone and, although they remained in place, they did not elongate. After 5 weeks, they began to extrude spontaneously. The programmed oblique distraction vector could not be achieved either, and therefore we could not achieve a significant improvement in the patient.
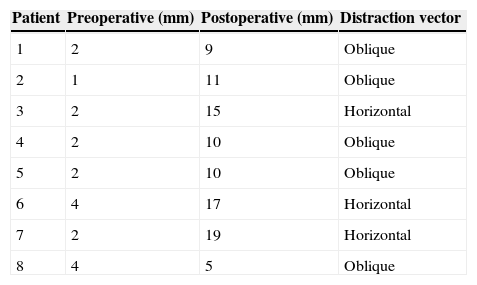
As the bone distraction advanced, the clinical status of the children surprisingly improved, oxygen saturation levels normalised and patients started to swallow, and thus to gain weight. After 8 days of the beginning of the bone distraction, a lateral cranial X-ray was performed to control the airway, which revealed an air column noticeably different to the initial one (Fig. 6). When distraction ended, a new lateral cranial X-ray was performed, and the airway between the base of the tongue and the posterior pharyngeal wall was measured again (Table 2).
Distance of the posterior pharyngeal wall to the base of the tongue measured in a lateral cranial X-ray and distraction vector.
| Patient | Preoperative (mm) | Postoperative (mm) | Distraction vector |
|---|---|---|---|
| 1 | 2 | 9 | Oblique |
| 2 | 1 | 11 | Oblique |
| 3 | 2 | 15 | Horizontal |
| 4 | 2 | 10 | Oblique |
| 5 | 2 | 10 | Oblique |
| 6 | 4 | 17 | Horizontal |
| 7 | 2 | 19 | Horizontal |
| 8 | 4 | 5 | Oblique |
Four out of 8 patients needed physiotherapy to rehabilitate chewing muscles, perioral muscles and suction and swallowing reflexes.
In 3 patients, one of the pins was extruded, in 2 of them it occurred in the 4th week of the support period and a replacement was not considered. In another case, it was extruded in the active bone distraction period and was reinserted one week later; during this time, there was recurrence and the distraction was only performed on the side where the pin had been lost until symmetry was achieved. In the case where the device stopped working, the pins were lost one by one after 4 weeks.
No inferior alveolar nerve injury was revealed.
Infection-type complications were scarce, and presence of skin crust and serous secretion in the skin around the pins were treated with chlorhexidine brush-strokes.
Skin scar was acceptable and in most patients it has blurred out with massages and silicone gel.
The 5 patients with cleft palate associated with Pierre-Robin sequence were subject to cleft palate repair with intravelar veloplasty after 6 months of the mandibular distraction, with no complications.
DiscussionFor many years, patients with obstructive apnoea secondary to micrognathia who did not respond to postural treatment were tracheotomised. The tracheotomy was the “gold standard” of treatments until the 90s. It is associated with a high morbidity as tracheomalacia, chronic bronchitis, laryngeal stenosis and risk of death due to mucus plugs or extrusion/dislocation of the cannula. Also tracheotomised patients require nursing care and family training that is not always available.
Other procedures, such as glossopexy,19 where the tongue is displaced to an anterior position and fixed to the jaw or lip to keep the airway free; transfixion of the tongue with Kirschner20 needle, located in front of the mandibular angle; and hyomandibulopexy, were designed to move the hyoid bone and the base of the tongue to a more anterior position. There are no studies proving the benefits of these techniques, and the related local aggressiveness and morbidity are evident.
There are different degrees of severity for clinical signs of obstruction. Many children with micrognathia have a low airflow which does not prevent them from leading a relatively normal life; however, when they have problems such as upper respiratory tract infections, they may develop respiratory obstruction and require endotracheal intubation. Sometimes, these upper respiratory tract obstructions, if prolonged, can lead to hypoxia, hypercapnia, pulmonary heart disease and pulmonary hypertension. They also have flat or insufficient growth curves, frequently associated with malnutrition and long hospitalisations and readmissions; therefore, they also suffer from psychosocial and family problems. All of that become more severe in syndromic cases.
Gradual enlargement of the jaw through bone distraction is a technique that allows increasing the sizes of the jaw at the expense of the local bone. No bone graft is necessary, allowing a simultaneous gradual elongation of soft tissues, muscles, vessels, nerves, skin, leaving the base of the tongue in a more anterior position and increasing the sizes of the retropharyngeal airway.
Advancing the base of the tongue with bone distraction is a challenge. The surgical decision-making in a child comes with great responsibility. There are a series of key questions posed before deciding to perform a bone distraction. We know that children with micrognathia improve with natural mandibular growth, but, can we predict which children will improve spontaneously and how long they will take to do so? Only the jaw size predicts the need for a surgical intervention? When is the right time to perform it? Is there a diagnosis algorithm for the decision-making? Dauria and Marsh21 try to answer some of these questions. Recently, Ow and Cheung22 analysed the feasibility of osteogenesis by distraction in the treatment of airway problems through a wide meta-analysis. All of that justify performing a mandibular distraction in new-borns when there are severe airway problems.
The criteria we have followed for the surgical decision-making are supported by the results obtained with the functional and anatomical assessment of the airway. We believe, together with other authors,23 that the polysomnography is very helpful in the decision-making process. We prescribe the performance of a mandibular distraction when apnoea pauses are longer than 10s, the apnoea/hypopnoea index is higher than 20 and desaturations are below 85%, together with the impossibility of feeding and flat or insufficient growth curves. The 3D CT scan revealed the hypoplastic mandible morphological characteristics and, like Shen et al.,24 we consider that the assessment of another parameter, which is the measurement of the airway at the retropharyngeal space level, is interesting; thus, we prescribe mandibular distraction when the distance from the base of the tongue to the posterior pharyngeal wall is 2mm or less as measured in a lateral cranial X-ray.
An important aspect to consider is the distraction vector. In all patients, we want to obtain a symmetric elongation of the mandible body in both sides and in sagittal direction parallel to the occlusal plane. The effect of the distraction is directly related to the vector and the osteotomy, considering its location and direction; the position of the pins determines the distraction vector and the osteotomy will be perpendicular to the vector. Therefore, the location of the osteotomy varies based on the severity and location of the hypoplasia. The result of planning a horizontal vector is to increase the anteroposterior size of the mandibular body with sagittal increase of the projection of the symphysis; with this vector, we have to highlight the tendency of the mandible to rotate clockwise, sometimes causing an anterior open bite.25 Also the suprahyoid muscles play an important role in this adverse event. But we have to highlight the positive effect on airway sizes at a retropharyngeal space level when a horizontal distraction vector is used.
We have to know the function of the oblique distraction vector when we plan the treatment of obstructive apnoea; the result is an increase in the sizes of both the branch and the mandible body and less occlusal changes.
In the cases analysed, we see that when we plan a pure horizontal vector we obtain an airway of higher sizes than when the selected vector is oblique. However, with the first, the occlusal changes caused are more severe.
We believe that, regardless of the location of the hypoplasia, in branch vs. in body, the distraction vector selected will be horizontal vs. oblique based on the severity of the clinical signs of obstruction. However, despite careful planning, the ideal vector is not achieved, due to the technical problem posed by small sizes of the mandible in children.
Regarding the lineal measurement we have performed, in a lateral cranial X-ray, from one point in the posterior edge of the tongue and another point in the posterior pharyngeal wall, over the prolongation of the mandibular plane (Me-Go), it is only an aid for the diagnosis which gives us an idea of the size of this space, but it is only a bidimensional and static image which does not include the airway's dynamic function.
Aesthetic results were excellent (Figs. 7 and 8) with an important anterior projection of the chin and a considerable expansion of the soft tissues of the lower third of the face and the upper portion of the neck, marking the cervico-mandibular angle.
Orthopantomography of patient in Fig. 3 at 5 years old. Note the elongated branch and body, corrected antegonial notches and poor definition of mandibular angles.
We have overcorrected our patients to compensate the scares genetic information on growth, although we stated that bone distraction may reconduct future mandibular growth, or, to the contrary, the mandible will continue to grow in a very small proportion. We are conducting a follow-up of the growth and facial development of patients treated with distraction, and we will compare the sizes of their mandible with standardised measures for a certain age; this future study will, maybe, give us the answer.
ConclusionsMandibular distraction is currently the “gold standard” for the treatment of obstructive apnoea secondary to micrognathia. It avoids the tracheotomy and/or other aggressive surgical procedures and treats the aetiology of the disease, improving oxygen saturation and changes in feeding in a few days. For the surgical decision-making process, supplementary explorations are helpful, such as polisomnography, lateral cranial X-ray and 2 and 3D CT scans. The horizontal or oblique distraction vector will be the vector of choice due to its positive effects on the sizes of the airway. It is a procedure whose results can be planned and reproduced, with minimum short-term complications.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: Martínez Plaza A, Fernández Valadés A, España López A, García Medina B, Capitán Cañadas LM, Monsalve Iglesias F. Cambios en la dimensión de la vía aérea en pacientes con secuencia de Pierre-Robin asociada a síndromes malformativos tras distracción mandibular. Planificación del vector de distracción. Rev Esp Cir Oral Maxilofac. 2015;37:71–79.