To analyze the results of an epidemiological study of mandibular fractures treated in a population of the city of Sao Paulo, Brazil.
Materials and MethodsThe population included patients treated by a Department of Oral and Maxillofacial Surgery and Traumatology from January 2008 to September 2010, diagnosed with mandibular fractures. The variables analyzed for the study were gender, age, etiology, clinical signs and symptoms, type of treatment, and postoperative condition.
ResultsA total of 171 patients and a total of 269 mandible fractures were diagnosed, with the majority being the males (84.8%), between the 2nd and 3rd decade of life. The mandibular condyle was the most affected region (32.04%), followed by the mandibular angle (23.38%). The postoperative edema was the most evident clinical sign, and the treatment of choice was the reduction and internal fixation with titanium mini-plates in all cases.
ConclusionThe treatment of mandibular fractures should be aimed at restoring the occlusion and mastication function, with surgery being the most indicated treatment, using reduction and internal fixation with the use of a plates and screws system based on the experience of the authors. Knowledge of surgical techniques and methods of reduction and fixation of fractures, and periodic monitoring allow these patients to receive the appropriate treatment.
analizar los resultados de un estudio epidemiológico de las fracturas mandibulares tratadas en una población de la ciudad de Sao Paulo, Brasil.
Materiales y MétodosLa población incluyó a pacientes tratados por un Departamento de Cirugía Oral y Maxilofacial y Traumatología desde enero 2008 hasta septiembre 2010, con diagnóstico de fracturas mandibulares. Las variables analizadas para el estudio fueron: sexo, edad, etiología, signos clínicos y síntomas, el tipo de tratamiento y la condición post-operatoria.
ResultadosUn total de 171 pacientes fueron diagnosticados de fracturas mandibulares y un total de 269 fracturas, siendo los varones, el género más afectado (84,8%), entre la segunda y tercera década de la vida, el cóndilo mandibular fue la región más afectada (32,04%), seguido por el ángulo de la mandíbula (23,38%). El edema postoperatorio fue el signo clínico más evidente y el tratamiento de elección fue la reducción y fijación interna con miniplacas de titanio en todos los casos.
ConclusiónEl tratamiento de fracturas mandibulares debe estar dirigida para restaurar la función de la oclusión y la masticación, siendo la cirugía el tratamiento más indicado, a través de la reducción y fijación interna con el uso de placas y tornillos de sistema basados en la experiencia de los autores Conocimiento de las técnicas quirúrgicas y los métodos de reducción y fijación de fracturas y el seguimiento periódico de los pacientes permiten un tratamiento adecuado para estos pacientes.
Maxillofacial trauma is one of the leading causes of admission of patients in the emergency department of most hospitals around the world. It is of great interest because of its high incidence, high rate of morbidity, disfigurement and the loss of function involved, and significant monetary cost represented by the need for hospitalization and treatment. Moreover, the possible concomitant fractures of other body parts should also be taken into consideration.1,2
The management of maxillofacial trauma can be very complex, for it includes the treatment of the fractured bones, dentoalveolar trauma and the soft tissue wounds.1
According to many studies and reports, maxillofacial trauma statistics are directly linked to geographic location and cultural aspects. Our goal in the present study is to determine the epidemiology of maxillofacial trauma in patients treated in the OMFST department - Santa Paula Hospital, during the 2008–2010 period of time.1,3
Materials and methodsWe conducted a retrospective study, through the analysis of hospital medical records of victims of mandibular fractures, assisted by the Department of Surgery and Maxillofacial Trauma headed by Dr Leandro Luiz Fernando Lobo, which serves a population that has medical private agreements, with coverage in the city of Sao Paulo, during the period January 2008–September 2010. Data were collected through a specific form, having analyzed the following variables: gender, age, etiology, signs and symptoms, location and fracture classification, associated fractures, type of treatment and postoperative complications in order to compare them with the literature. This study is approved by the Ethics Committee of the Santa Paula Hospital in Sao Paulo Brazil. Number: 1981–2010-V.
ResultsThe total sample consisted of 171 patients. Males were more affected with 145 patients (84.8%) of mandibular fractures and a total of 26 female patients (15.2%) were included in this study.
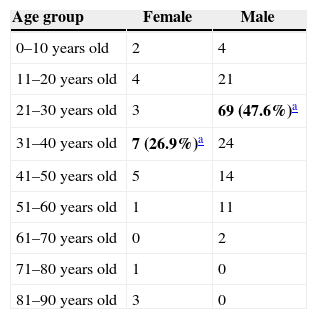
The most affected age group among females was 31–40 years old; in males the most affected age group was between 21 and 30 years old (Table 1). The average age for women was 38.8 years old and for men was 30 years old.
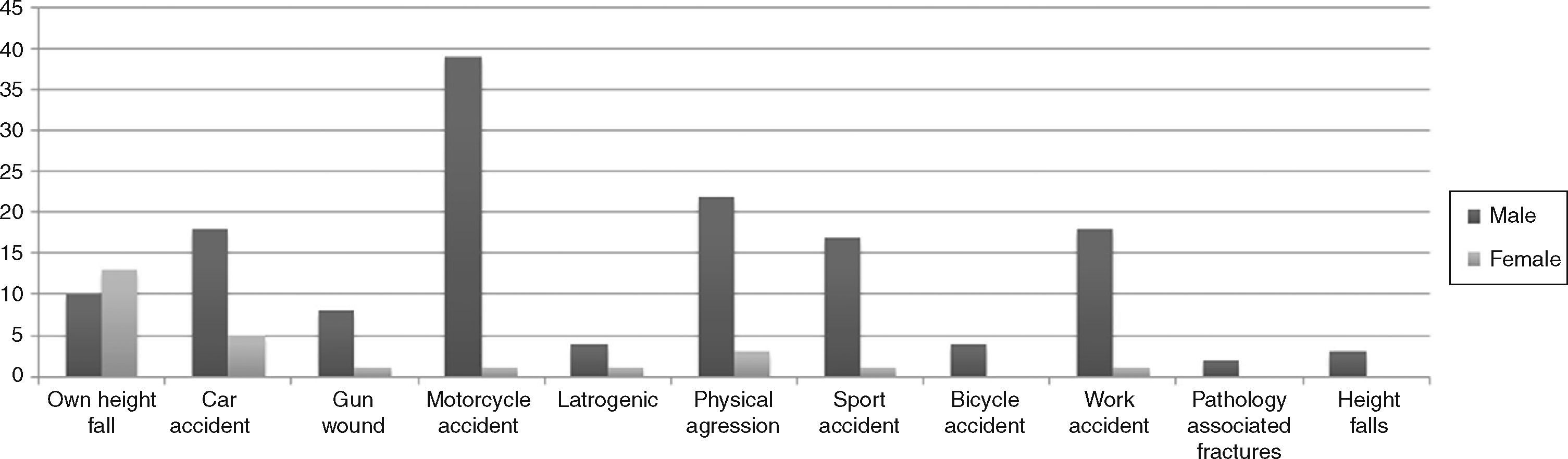
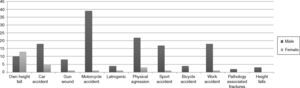
The etiology of mandibular fractures in females was falling from own height in 50% of cases corresponding to 13 patients, and in males, motorcycle accidents with 39 cases (26.9%) (Fig. 1).
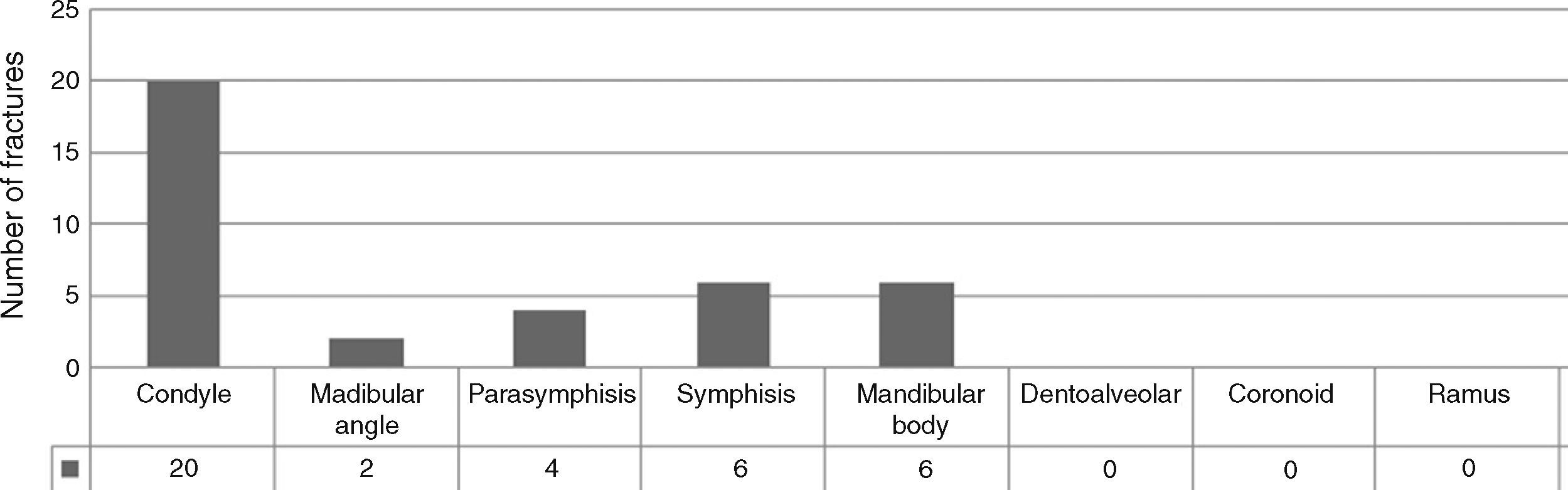
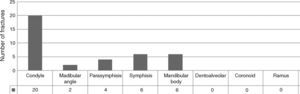
Mandible fractures resulted in a total of 269 fractures, 38 diagnosed in women and 231 in men. The condylar region was most affected in females with 20 fractures (53%), followed by the symphysis with 6 fractures (16%); and mandibular body also with 6 fractures (16%) (Fig. 2).
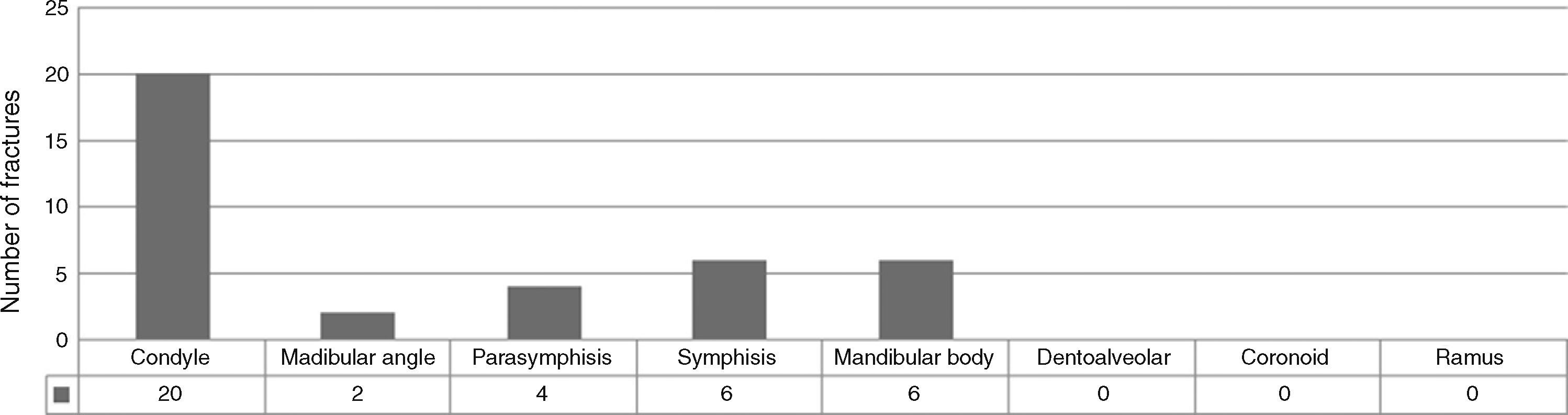
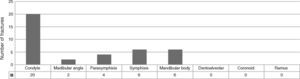
In males, the condyle was also the most affected region with 74 fractures (32.04%), followed by the angle with 54 fractures (23.38%); parasymphysis with 39 fractures (16.89%); and 33 fractures in the symphysis region (14.3%) (Fig. 3).
In our study, 47 fractures were associated with mandibular fractures, zygomatic complex affected with 25 fractures, followed by Le Fort I fractures with 4 cases; nose and orbit with 4 cases each, Le Fort II and III with 3 cases each; Lannelongue fractures with 2 cases; frontal bone and dental alveolar process with 1 case each and 1 case associated with femur and hip fracture. Clinical signs and symptoms of the patients were pain on movement; change in dental occlusion; opening and closing mouth difficulty; edema; ecchymosis; crepitus bone; anterior open bite in bilateral condyle fractures; deviation of the mandible to the affected side in mouth opening in condylar fractures; inability to perform lateral movement to the unaffected side in condylar fractures; intra oral occlusal steps; inferior alveolar nerve paresthesia; trismus; and mobility of bone segments.
Regarding the fractured sites, mandibular fractures showed one site of fracture in 49 cases (28.9%), two sites fractured in 40 cases (23.4%), three fractured sites in nine cases (5.5%). Usually the latter were fractures in symphysis region (direct trauma) associated with bilateral fracture of condyle; four sites were observed in only one case. Comminuted fractures occur in most cases by firearms injury, totaling 8 cases. The remaining 65 patients had fractures in another location site from mandible.
The extra-oral access was performed in fractures of the posterior mandible: body, angle, ramus and condoyle, access Risdon being used for the first three anatomical sites and pre headset for condylar fractures, retromandibular approach was used in only two cases of bilateral condylar fracture; was also used in the anterior region, when comminuted fracture or lacerating wound on skin were present. Intraoral access with bottom of lower buccal sulcus incision was performed in fractures in the anterior mandible and slightly displaced fractures of the mandibular angle.
The treatment of choice is the reduction and internal fixation with titanium miniplates, with use of the 2.0mm system in the compression zone associated with the 1.5mm system in the tension zone; or the use of two 2.0mm plates in each zone, depending on the level of displacement of the fracture; the use of reconstruction plates took place in comminuted fractures or fractures in atrophic jaws, the treatment of mandibular angle fractures using the technique of Champy using a Plate 2.0mm in internal oblique line (tension zone) was performed when no displacement was found (three cases); resorbable plates and screws were used in two cases of mandibular fractures in children, conservative treatment was performed in six cases for condylar fractures through orthopedics with orthodontic elastics, other sixcases of condyle fractures discopexia was performed; arthrocentesis, in other four cases and even two ATM prosthesis. Fixation with steel wire was also held in three cases due to dentoalveolar fractures, removal of the coronoid process in one case of coronoid fracture, two conservative treatments through monitoring in mandibular angle greenstick fracture.
The postoperative edema was the most evident clinical sign; in some cases indication of orthopedics with elastic was necessary in order to improve dental occlusion. Regarding to complications, there were six: infection in two cases due to the presence of the 3rd molar in the fracture, where extraction of the tooth was performed; two malocclusion cases where mandibular osteoplasty and further reduction and fixation were held; one plate fracture in the condyle region, using one titanium plate, being held fractured plaque removal and further reduction and internal fixation with two 2.0mm titanium plates; and one late hemorrhage by intra-oral surgical access in pre symphysis and auricular region, due to systemic pathology presented by the patient (liver cirrhosis), being held intra oral cautery and compressive dressing with tranexamic acid and Tensoplast® in preauricular region.
DiscussionRegarding the etiologyAccording to Lizuka2; Sojat et al4; Vasconcelos et al5; mandibular fractures taken into account were caused by physical attacks, but for Divares et al.,6 traffic accidents was the main cause of mandibular fractures, mainly accidents involving cars and motorcycles, which was confirmed by the studies of Filho et al,7 Bianchini et al.8 Bormann et al.9 and Sawazaki et al.10 However, Gerbino et al.,11 Gray et al,12 stressed that the etiology of trauma, in general, is strongly influenced by socio-economic and cultural factors. Motorcycle accidents among traffic accidents were the main causes of mandibular fractures,13,14 but car accidents contributed to a higher incidence of jaw fractures.15
Regarding accidental falls, they were more common in extreme age groups (children and elderly) according to Koltai et al.,16 Hussain et al17; however, Bertoja18; Qudah,19 Sarmento et al.20 and Motta,21 reported that falls were more frequent in a young population, also presented by Yamamoto et al.,22 with an average age of 51.3 years old for falls from own height and 31.9 years old for falls from heights.
The most frequent etiology of facial trauma to Oji23 were traffic accidents with 83%; assaults and sports with 8.4–4.3%; motorcycle accidents were responsible for 26.4% of facial fractures, followed by 20% for cars, bicycles with 16.8%, falls with 13.6% and 8.8% for assault, in 2003, in Taubaté. Iran Silva et al.,24 reported a study in Recife, in which the most frequent cause of facial fractures were injuries by firearms 30.8%. This study also showed a higher incidence in motorcycle accidents with 17.9%, leaving the car accidents with 15.4%. Traffic accidents were shown to be the main agent of facial fractures to Fonsceca et al.25 In Washington, the etiology of facial fractures varied, getting physical attacks with 79% of the cases reported by Krause et al.3 (2004) and Silva et al.17 (2009) with aggression reaching a percentage of 36%, 43%, 48.1%, 37.1%, 57% and 35.58% respectively.
In our study, the etiology of mandibular fractures in females was fall from own height in 13 cases (50%) cases, and in male, motorcycle accidents in 39 patients (26.9%).
Regarding genderMasculine gender was the most affected by mandibular fractures.4,5,7,13
Our study showed 123 (84.8%) male subjects with mandibular fractures, which is consistent with the literature reviewed.
Regarding ageThe age range of 20 to 30 years old was the most affected by mandibular fractures.4,5,7,8,10,14,15,18,20 However, Bormann et al.,9 prevailed with individuals with mandibular fractures between 16 and 25 years; Yamamoto et al.22 presented subjects with an average age of 51.3 years old, for patients with mandibular fractures from falls from own height and 31.9 years old for patients suffering falls from high falls.
In our survey, 69 (47.6%) male subjects were affected by mandibular fractures in the age group of 21–30 years old, and seven female patients (26.9%) aged 31–40 years old, presenting a resemblance to the literature that shows the 2nd and 3rd decade of life as the hardest hit by mandibular fractures.
Regarding fractured boneThe mandible appears as the most affected facial bone by fractures, an incidence of 36% to 70%.15,18,22,23 In our study, it was the most affected bone (269 cases), followed by zygoma fractures with 142 cases, nasal with 139 cases and orbit with 60 cases.
Regarding the fractured mandibular regionFilho et al.,7 body fractures represented 28.5%, condyle 26.6%, symphysis 19.9%, angle 14.2%, alveolar 1.9%; coronoid 1.15%, whereas for Vasconcelos et al.,5 it was also the body the most affected with 38.3%, followed by the angle with 34%, condyle with 27.7%, parasymphysis with 17.7%, dentoalveolar process with 14.9%, symphysis and parasymphysis with 6.4%; Martini et al.15 also found more fractures in the mandibular body 30.9%.
Condylar fractures were more common, according to Krause et al.3 and Bianchini et al.8 (83.3%) but Bormann et al.,9 in 2009, had a total 42% for condyle fractures. Sawazaki et al.,10 reported 317 condylar fractures diagnosed in 2010. Yamamoto et al.22 (2010) found a higher rate for condylar fractures with 64.5% for victims of falling from own height and 41.9% victims of falls from heights. Bertoja.,18 reported parasymphysis fracture were more common in patients up to 5 years old (37.5%); in mandibular body between 6 and 12 years old (20%); and the angle from 13 to 18 years old (25%).
According to results of the study conducted in our department, the most common fractures in women were the condyle in 20 (52.6%) patients, followed by symphysis and body with 6 fractures each (15.8%). In males, the most affected region was also the mandibular condyle with 74 (32.1%) patients, followed by the angle with 54 (23.4%) cases. Condylar fractures totaled a higher percentage, agreeing with Krause et al.,3 Bianchini et al.,8 Sawazaki et al.10 and Yamamoto et al.22
Regarding fractured mandibular sites and its association with other fracturesPatients had fractures in other bones of the face according to Fonsceca et al.25 and Sarmento et al.20 Our survey showed that 47 fractures were associated with mandibular fractures, zygomatic complex being the most affected with 25 fractures. A single fracture line on the mandibular region was more evident.5,13 Our clinical study showed concordance with the literature where we diagnosed a single fracture site in 49 (28.9%) cases.
In studies of Martini et al.,13 in 2006, 53% of mandibular fractures were unilateral and 47% bilateral. However, 157 men and 52 women had unilateral condylar fracture; 41 men and 13 women had bilateral condylar fracture; 50.95% of patients who were diagnosed with mandibular fracture had condylar fracture and other bones fracture.10 In our survey, bilateral condyle fractures were diagnosed in 43 (15.96%) cases; and bilateral fractures totaled 49 (18, 22%) cases.
Regarding the treatment appliedRigid internal fixation with the use of miniplates and screws was the method of treatment used by most authors4,7,14). Filho et al.,7 Sojat et al.,3 associated this to maxillomandibular fixation.
Surgical treatment in 579 mandibular fractures (83%), 558 intra oral accesses and 21 extra oral accesses being held. 65% used miniplates 2.0mm, 29% Unilock plates and 6% leg screws; 17% were treated by closed reduction.9 However, 14% of mandibular fractures were treated in a non-surgical way.
Sawazaki et al.,10 in 2010, treated 21.5% with surgery and 78.5% were treated non surgically.
In our study the treatment of choice is the reduction and internal fixation with titanium miniplate with use of the 2.0mm in the compression zone associated with the system of 1.5mm in the tension area; or use of 2.0mm two plates in each zone, depending on the degree of displacement of the fracture; as well as the use of reconstruction plates for comminuted fractures or fractures in atrophic jaws. The treatment of mandibular angle fractures through the Champy technique with use of a Plate 2.0mm in internal oblique line (tension zone) is held when displacement is not found. Conservative treatment of condylar fractures was performed in six cases through orthopedics with orthodontic elastics, in other six cases of condyle fractures discopexia was performed; arthrocentesis in other four cases and even two ATM prosthesis; removal of the coronoid process in one case of coronoid fracture; two conservative treatments through monitoring in mandibular angle greenstick fracture; intra-oral surgical approach was performed in symphysis, parasymphysis, body and angle (when not displaced) fractures; and extra-oral in body, angle, ramus and anterior condyle fracture when displaced and comminuted.
Regarding complicationsInfection was the most common cause of postoperative complications7,13 and malocclusion was responsible for 10% of them in studies of Martini et al.13
Complications evidenced in our clinical study were only 6 cases: infections in 2 cases by the presence of the 3rd molar; 2 malocclusions; 1 condyle region plate fracture with the use of 1 titanium plate; and 1 late hemorrhage due to systemic pathology (liver cirrhosis) of the patient.
Regarding the use of safety devicesThe seat belt used by 76.92% of the patients served as a protective factor for the mandible according to Fonsceca et al.,25 however Mantovani et al.15 reported that 45% of patients did not use them during the accident.
Regarding drugs abuseSojat et al.4 reported that 20.6% of the patients were under the influence of alcohol, as well as Mantovani et al.,15 who observed that the use of alcohol was present in 38% of patients suffering from mandibular fractures caused by motor vehicle accidents and 58% by assault.
Regarding Condylar fractures approachSeveral authors in literature describe that the condyle fractures are favorable to closed treatment with intermaxillary fixation, between 7 and 21 days, taking into account the patient's age, the displacement of the fracture and associated injuries. Internal capsular fractures are treated with intermaxillary fixation for 10 to 14 days, followed by physical therapy for the prevention of ankylosis.13,16
The indications for open reduction approach in condylar fractures in adults are based on the principles of Zide and Kent26 classified as the absolute and relative indications. Among those absolute are the inability to have proper occlusion with closed reduction techniques, displacement of the condyle of the middle cranial fossa, the lateral condyle extracapsular dislocation, presence of a foreign body in the joint capsule. Regarding the relative indications bilateral condylar fractures associated with comminuted fractures of the midface, bilateral fractures in edentulous patients where their approach is difficult, patients with medical problems (psychiatric, seizure disorders, alcoholism) are some of the mentioned by the authors.26
In 2003, American Association of Oral and Maxillofacial Surgery suggested an international guideline on the treatment of mandibular condyle fracture. According to the guideline, open reduction is recommended for the cases of mandibular condyle fracture suspected in clinical and radiologic examinations to prevent complications such as functional or growth disorders.27,28
In the past, closed reduction with concomitant active physical therapy conducted after intermaxillary fixation during the recovery period had been mainly used, but in recent years, open treatment of condylar fractures with rigid internal fixation has become more common.28,29
Colleti G et al.,29 described that in their experience with the treatment of the first 100 condylar fractures using the mini-retromandibular approach has demonstrated that this technique has allowed the Authors to safely manage extracapsular condylar fractures at all levels.
The experience of the authors service is based on years of follow ups of condylar fractures treated with open reduction protocols, this as refereed by other authors27–29 to reestablish the function of the temporomandibular joint, preventing osteoarthritis of the condyle by the lack of movement of the joint associated to the jaw's lock during close reduction and avoiding TMJ ankylosis.
The treatment is aimed to restoring the occlusion and mastication, being surgery the most indicated treatment as expressed in the results, through reduction and internal fixation with the use of plates and screws system 2.0mm in the compression zone, associated to the system in the 1.5mm in the tension zone, or another system board of 2.0mm also in the tension zone, depending on the degree of displacement of the fracture.
Knowledge of surgical techniques and methods of reduction and fixation of fractures and periodic monitoring of patients allow an appropriate treatment for these patients.
Ethical approvalThis study is approved by the Ethics Committee of the Santa Paula Hospital in Sao Paulo Brazil. Number: 1981–2010-V.
FundingNone declared.
Conflicting of interestsNone declared.