We report a case of rare clinical entity, which comes within the spectrum of hip impingements. The case deals with a 36 year old female, Olympic athlete, who developed ischiofemoral impingement 14 months after a surgical hamstring reattachment. She was treated conservatively and fully recovered. When looking into literature on this matter, we found that it is probably an under-diagnosed problem, particularly in patients with no history of prior surgery. To our knowledge, this is the first case reported after a hamstrings tendon reattachment.
Se presenta un caso de una rara entidad clínica que forma parte del espectro de los pinzamientos en la articulación de la cadera. Se trata de una atleta olímpica de 36 años que desarrolló un pinzamiento isquiofemoral 14 meses tras una reinserción quirúrgica de tendón de isquiosurales, en la que se optó por seguir tratamiento conservador constatándose una total recuperación. Revisando la bibliografía probablemente se trata de una entidad infradiagnosticada especialmente en los casos que no existe antecedente quirúrgico. Es el primer caso comunicado después de cirugía de reinserción de tendón de isquiosurales que tengamos conocimiento.
Ischiofemoral impingement is a medical condition that involves narrowing of the space between the lesser trochanter and the ischial tuberosity causing symptomatic changes in the quadratus femoris muscle (QF).
AetiologyThis condition may have congenital and acquired causes. The congenital causes comprise variations of the angles between the femoral shaft/femoral neck/lesser trochanter (e.g., coxa valga), of the lesser trochanter/femoral neck on the axial plane,1 and cases due to mass effect in multiple hereditary exostoses have been described. Acquired aetiology is associated with mass effect (hamstrings, psoas bursitis, osteophytes), QF tendinitis,2 orthopaedic treatment of fracture of femur, hamstring tendon avulsion fracture, and it is also associated with surgical procedures such as hemiarthroplasty (HA), total hip arthroplasty (THA), osteosynthesis of the femoral diaphysis and intertrochanteric osteotomies.
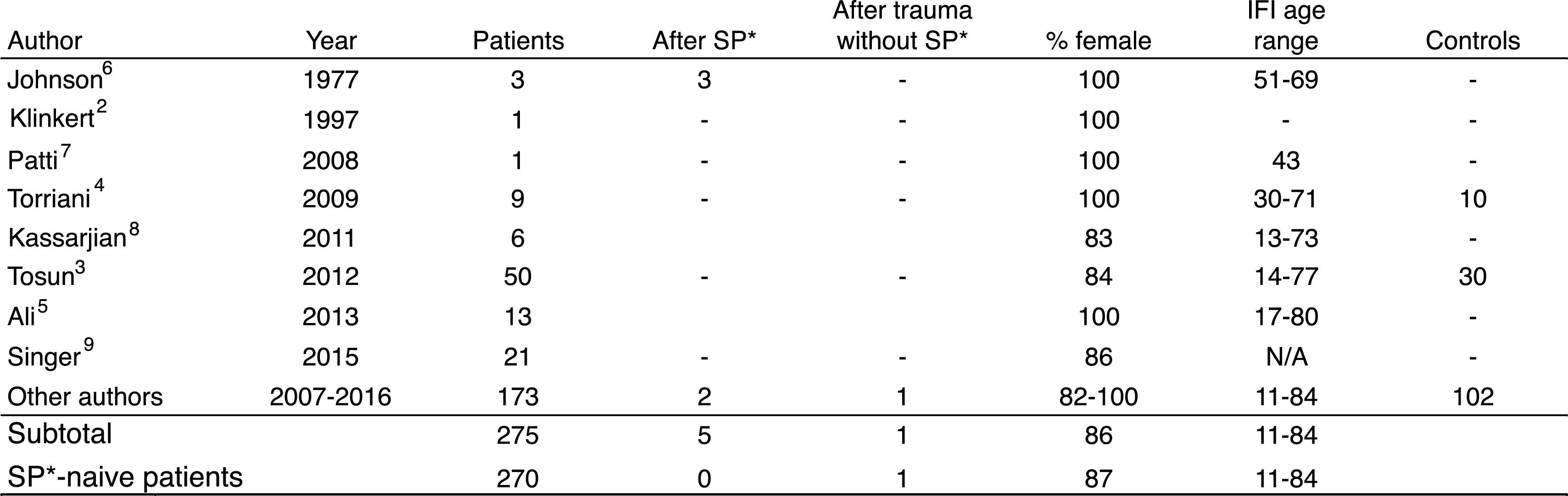
EpidemiologyThe condition affects females predominantly (86%) with no clearly defined age of presentation. Bilaterality3 has been reported in up to 40% of cases. The series we reviewed covered 275 patients, 270 with no previous surgery (Fig. 1).
Reviewed articles of cases of ischiofemoral impingement. Approximately 270 cases are covered with an incidence of 87% in females, with no specified age range in patients who have not undergone previous surgery (see ref. 7). * SP: surgical procedure.
Low back pain of gradual onset is characteristic of the condition, and pain to buttocks, groin, posterior hip surface, occasionally radiating to the knee. It can even be associated with snapping and/or crepitus and/or hip locking.
Any movement that pinches the QF muscle between the lesser trochanter and the ischial tuberosity causes pain. These movements are any combination of EXtension, ADduction and External Rotation (EXADER). The pain can increase with other movements associated with compression or stretching of the QF, such as the Freiberg signs, FADIR, sitting or striding.
Additional informationImaging techniques can be useful. Simple radiography can reveal valgus femoral neck, narrowing of the ischiofemoral space, cysts in the ischium or osteophytes. Ultrasound (US) is of great value in dynamic explorations and also to guide injections for diagnostic and therapeutic purposes (but it is operator-dependent). Magnetic resonance imaging (MRI) can reveal narrowing of both the ischiofemoral space (IFS, between the lesser trochanter and the ischial tuberosity) and the QF space (QFS, between the lesser trochanter and the hamstring tendon) muscular oedema of the QF (increased signal on T24) and atrophy of the muscle belly of the QF.
DiagnosisDiagnosis should be based on clinical, semiological and morphological criteria, although the narrowings can be purely anatomical, or functional,1,5 or a combination of both.
Differential diagnosesSnapping of the psoas tendon, sciatic pain, chronic hamstring injury, fibrillar rupture of the QF, abductor tendonitis, coxofemoral capsule instability, posterior acetabular labral tears, and pain in the sacroiliac joints.
TreatmentGood results have been reported from fluoroscopy/CT/US-guided injections (cortico-anaesthetic, prolotherapy), and with rehabilitation. These are the treatments of choice especially for patients who have not undergone any previous surgery. Open and arthroscopic operations are reserved as an alternative for patients who fail to respond.
Clinical caseWe present the case of a 36-year-old female Olympic long-distance runner, who felt an acute pain in her right buttock after being pushed and having to run forwards in a competition. Ultrasound and MRI showed total avulsion of the hamstring tendon. Tendon reinsertion surgery was performed using a longitudinal posterior transgluteal approach, section of fascia, section of some gluteus maximus fibres to enable better visualisation-location of the ischial insertion footprint of the hamstring, and 2 anchors made with SUTUREFIX ultra Anchor 1.9mm (Smith & Nephew) respecting the insertional anatomy (combined semitendinous tendon/femoral biceps medial-wards and semimembranosus lateral-wards). The patient then started a progressive and sequential 6-month rehabilitation programme, until she regained her previous running scores.
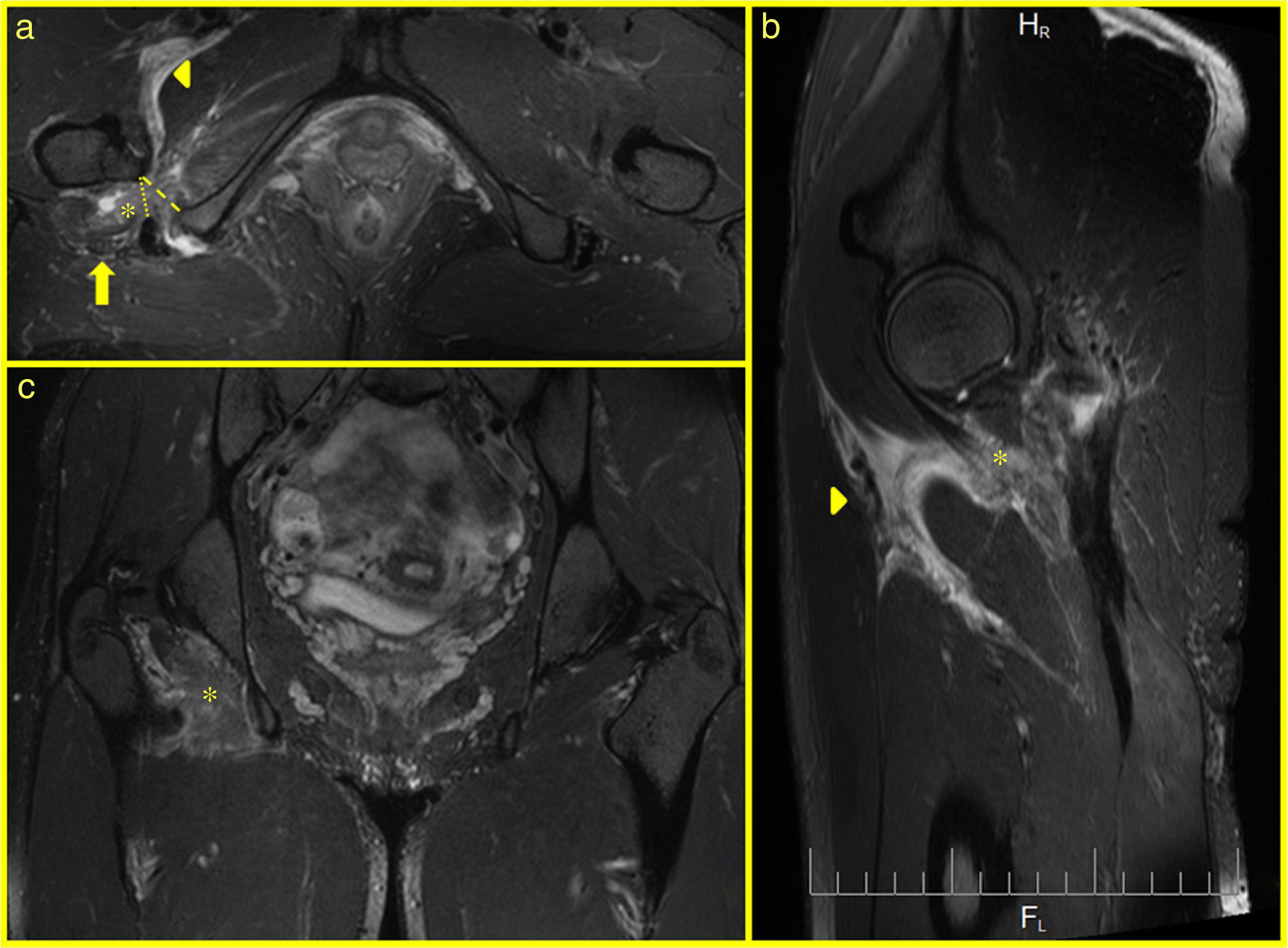
Fourteen months after the operation, the patient noticed an acute pain in her buttock during an intensive downhill race with acute sciatic irradiation. Physical examination revealed poor recruitment of the hamstrings, but the radicular tension manoeuvres of the sciatica were not clear. MRI showed postoperative changes with 2 screws, fluid between the ischium and the hamstring tendon, no osteal-periosteal anchoring was observed, but fibrous bridges in the soft tissues were observed (sacrotuberous ligament). Fibrosis in the proximal hamstrings was also revealed, minimal oedema in the proximal belly of the semitendinosus and femoral biceps, oedema in the QF (belly and adjacent fat), oedema between the pectineus and the psoas, oedema in the gluteus maximus and the adjacent ischial tuberosity, and peri-intraneural oedema in the sciatic nerve. The measurements of both the IFS and the QFS met the criteria of Singer et al.9 (Fig. 2) for bilateral ischiofemoral impingement, although the contralateral impingement was asymptomatic and with no oedema in the QF.
MR images on axial (a), sagittal (b) and coronal (c) planes, showing: changes in the ischiofemoral space with oedema of the quadratus femoris muscle on (a, b, and c) (asterisk). Increased perifascial signal between the flexor and adductor muscles on (a and b) (tip of arrow). Increased perineural signal in sciatic nerve on a (arrow). IFS (lines 18.3mm and QFS (dots) 12.6mm. The unaffected contralateral side measurement was IFS 19.4mm and QFS 14.1mm.
With a diagnosis of ischiofemoral impingement and suspected re-rupture of the hamstring, the sciatic pain determined initial treatment with high doses of oral corticosteroids and subsequent rehabilitation focussing more on reabsorption of the oedema, restoring neuromuscular control and re-educating the running technique. A later tensiomyography caused asymmetry in the contraction time of the femoral biceps, and therefore a further change in physical training was prescribed.
Three months later the patient had completely recovered, and has suffered no relapse over the past 2 years, and participates in international competitions.
DiscussionIschio-Femoral Impingement (IFI) was described in 1977 by Johnson6 in 3 women with persistent postoperative hip pain, 2 after THA and the other after proximal osteotomy of the femur. Soon afterwards many reports of nonsurgical IFI appeared, together with queries and discussions in the literature about findings on MRI of oedema vs fibrillar rupture of the QF8 (expressed as an increased signal on T2 MRI with a gap6 in the fibres). There have been attempts to set limit MRI values in IFS and QFS,3,4,9 and variability has been found in the positioning of the lower limbs, and overlapping of the normal and pathological values depending on the series. In our case, we only found an overlap with the imaging criteria of Singer et al.9 in the bilateral measurement of IFS and AFS, and we only found signs of persistent oedema of the AF with no rupture, which would not be compatible with the post-exercise oedema typical of DOMS that soon disappears.
IFI is a clearly an under-diagnosed entity. There are probably no more cases, since it is generally not considered in the event of atypical hip pain. It is also often paradoxical, because we can find many changes on MRI in asymptomatic people,1,10 and we can find idiopathic cases that might involve neuromuscular control.1,5
In our case, we found extensive fluid on MRI, perhaps due to an acute and partial re-rupture of the proximal tendon of the hamstring causing only slight knee flexion dysfunction. It seems that the reinsertion was stronger in the sacrotuberous ligament whose fibres form a continuum with the hamstring tendons, than the anchor in the ischial tuberiosity. But this does not explain the infiltration of fluid in the sciatic nerve, making sciatica the main clinical symptom. It seems more likely that an abnormal pattern of neuromuscular control in the contraction of the muscles was the cause of the oedema in the quadratus femoris and the irritation of the sciatic nerve, leading us to wonder whether there was indeed an acute ischiofemoral impingement or whether the acute sciatic pain alone highlighted an underlying problem.
As far as we know, this is the first report of an IFI after surgery to reinsert the proximal hamstring tendon. And moreover, these patients must have increased susceptibility due to various factors such as the mass effect caused by local oedema after their injury and after the operation, and even due to postoperative fibrosis. Another predisposing factor might be a loss of neuromuscular conditioning, causing fatigue, a drop in maximum strength or muscular discoordination, causing functional narrowing in the IFS.
A diagnosis of IFI must include clinical, semiological and imaging findings, although there may be clinical and radiological dissociation in that the images show more changes than the clinical symptoms. In our case, we found a gap between the ischium and the tendon with no retractions, and little loss of strength clinically. The aetiology must guide the therapeutic options. Therefore, acute and inflammatory causes require reducing the inflammation, and by contrast a functional aetiology requires rehabilitation and reconditioning based on reabsorption of oedema, restoring neuromuscular control and re-educating sports technique according to the patient.
Although the option to inject the muscular belly of the QF is widely referenced, we prefer treatment with systemic corticosteroids to prevent local effects in the proximity of the reinserted tendon.
Level of evidenceLevel of evidence V.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their centre of work regarding patient data confidentiality and that all the patients included in this report have received sufficient information and have signed their written consent to participate.
Right to privacy and informed consentThe authors declare that no patient data appear in this article. This document is held by the corresponding author.
The authors would like to thank Drs Jakub Jablonski and Gabriel Lupon, and Mrs Anne Louise Thomas for their support and collaboration.
Please cite this article as: García XG, Turmo A, Cos MA, Puigdellívol J, Til Ll. ¿Pinzamiento isquiofemoral agudo? Rev Esp Cir Ortop Traumatol. 2018;62:302–305.