Articular tuberculosis of the ankle joint is a rare presentation of skeletal tuberculosis (10% of cases). This unusual location and the low index of clinical suspicion leads to delays in diagnosis and treatment. Radiographic and analytic studies are unspecific in the first stage. CAT and MRI are useful in diagnosis. Chemotherapy is the mainstay of treatment and surgery is often required to establish the diagnosis and in the treatment.
We report a case of ankle tuberculosis in a 22 month-old child. The diagnosis was confirmed by synovial biopsy. There was no patient or family contact with tuberculosis patients. There was no risk factor. There was no lung disease. Diagnosis was made 1 year after onset of symptoms. The treatment was with chemotherapy and surgery was performed as preventive treatment of equinus deformity and osteoarthritis. Good clinical and functional outcome was achieved after 20 years of follow up.
La tuberculosis osteoarticular del tobillo es una presentación infrecuente de la tuberculosis ósea (10% de los casos). La baja frecuencia de presentación y la clínica inespecífica hace que sea habitual el retraso en el diagnóstico y en el tratamiento. El estudio radiológico es normal en fases iniciales, y la analítica no muestra alteraciones características. La TAC y la RM son útiles en el diagnóstico. La quimioterapia es la base del tratamiento, y la cirugía puede ser necesaria para obtener el diagnóstico y como parte del tratamiento.
Presentamos el caso una niña de 22 meses afecta de tuberculosis de tobillo. El diagnóstico se confirmó mediante biopsia sinovial. No hubo antecedentes de contacto personales ni familiares con enfermos de tuberculosis. No existía ningún factor de riesgo para la enfermedad. No tuvo foco pulmonar. El diagnóstico fue tardío (un año tras el inicio de la clínica). El tratamiento fue médico (tuberculostáticos) y precisó cirugía para evitar actitud en equino y un mayor deterioro articular. El resultado clínico y funcional fue bueno tras un seguimiento de 20 años.
Bone and articular tuberculosis (TB) is a granulomatous inflammation caused by Mycobacterium tuberculosis. It is a localised and destructive disease which is usually carried by the blood from a primary focus (peri-bronchial lymphatic lymph nodes or infected mesenteric lymph nodes). Extrapulmonary TB usually affects people whose immune system is impaired, including children, elderly people and patients with kidney disease or HIV carriers.1
The frequency of TB has dropped greatly in the last few decades, especially in developed countries, although it continues to be a problem in Sub-Saharan Africa and in South East Asia.2 TB continues to be a disease which is considerably prevalent in Spain. The incidence in Spain was 70 cases/100,000 inhabitants in 1990, and around 30/100,000 from 2000 until 2007.3–5
It may affect practically all joints, the most common being the vertebra (50%). Localisation in the foot and ankle is infrequent (between 5% and 10%, according to the literature). Exclusively osteoarticular presentation is rare, making up for around 2–5% of extrapulmonary TB cases.6,7
Although several works have been published on the treatment of tuberculosis and how it affects foot and ankle joints, there are few follow-up studies and long term monitoring of these patients. This article describes the case of a patient who presented with tuberculosis of the ankle joint with a follow-up of 20 years. Difficulty in diagnosis is also noted, which leads to delays in appropriate treatment. A review of the literature was also made.
Clinical caseWe present the case of a patient who consulted initially at 22 months. The patient had been born in Spain and had not presented with any risk factor for the appearance of the disease. The family's socio-economic situation was good. In the clinical interview we were told that neither the patient nor anyone in his close environment had travelled to endemic TB regions.
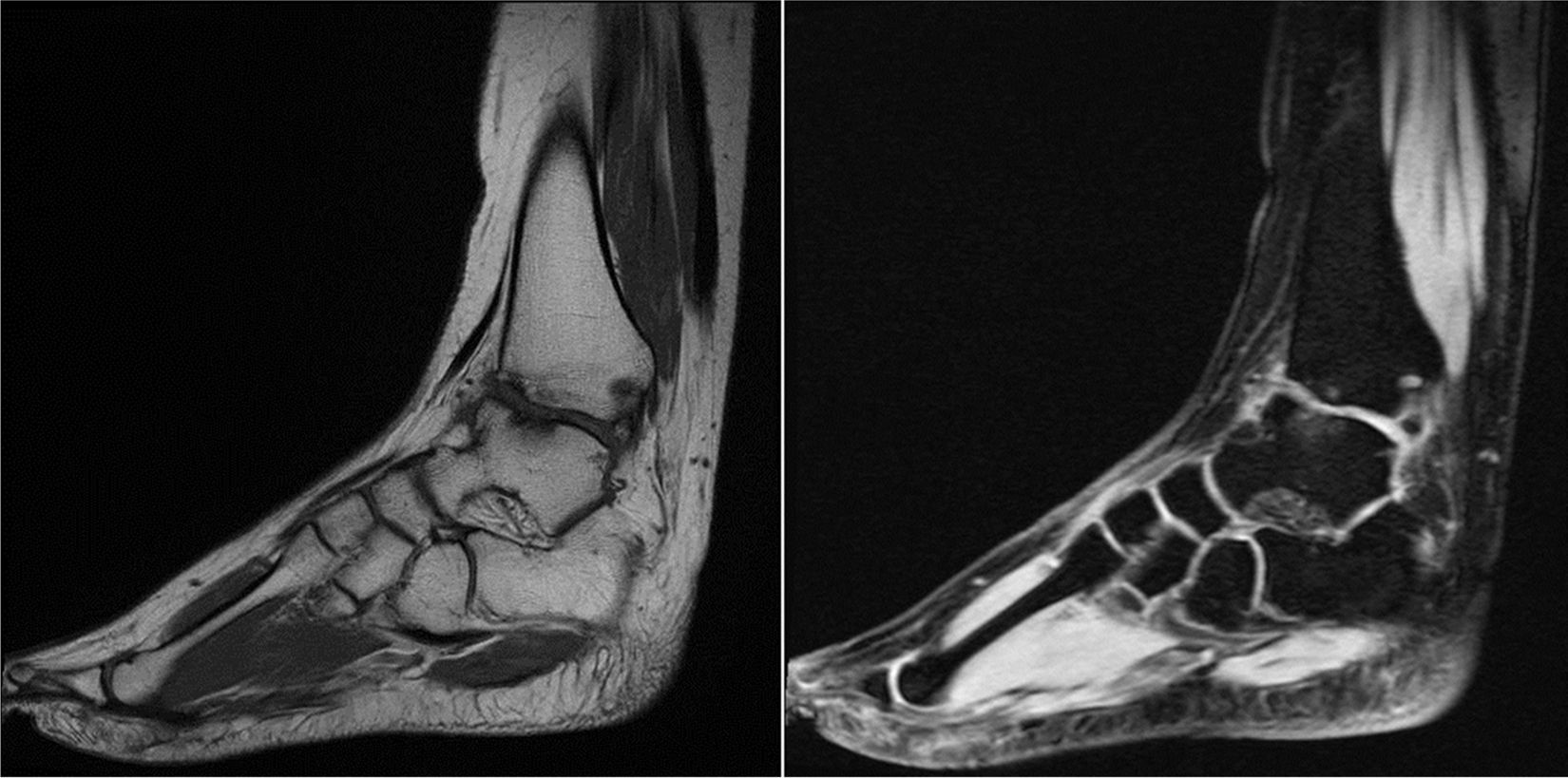
He presented with swelling and pain in the right ankle, a limp, and in the lower right limb in external rotation. Three weeks previously he had been diagnosed with an ankle sprain and the ankle had been immobilised for 2 weeks. All X-rays, analytical and rheumatic studies tested normal. A MRI of the ankle was taken which only showed non-specific synovitis, with no clear diagnosis being made. Analysis and rheumatic tests were normal.
One year after symptoms began and due to their persistence, we decided to perform a synovial biopsy and the outcome was TB of the ankle joint. X-rays were made of the chest and any lung involvement was ruled out. Antibiotic treatment was initiated (isoniazid and rifampicin) for 9 months and relief orthosis for 3 months. The patient was asymptomatic at 4 years of age and the infection resolved.
At 9 years of age ankle mobility was almost complete, but atrophy of the triceps surae muscle and retraction of the Achilles tendon was noted. The EMG was normal. Surgery was performed for an enlargement of the right Achilles tendon with shifting to improve walking. After immobilisation and subsequent physiotherapy the patient improved, although a pain on the anterior side of the right ankle persisted and was controlled with anti-inflammatory drugs.
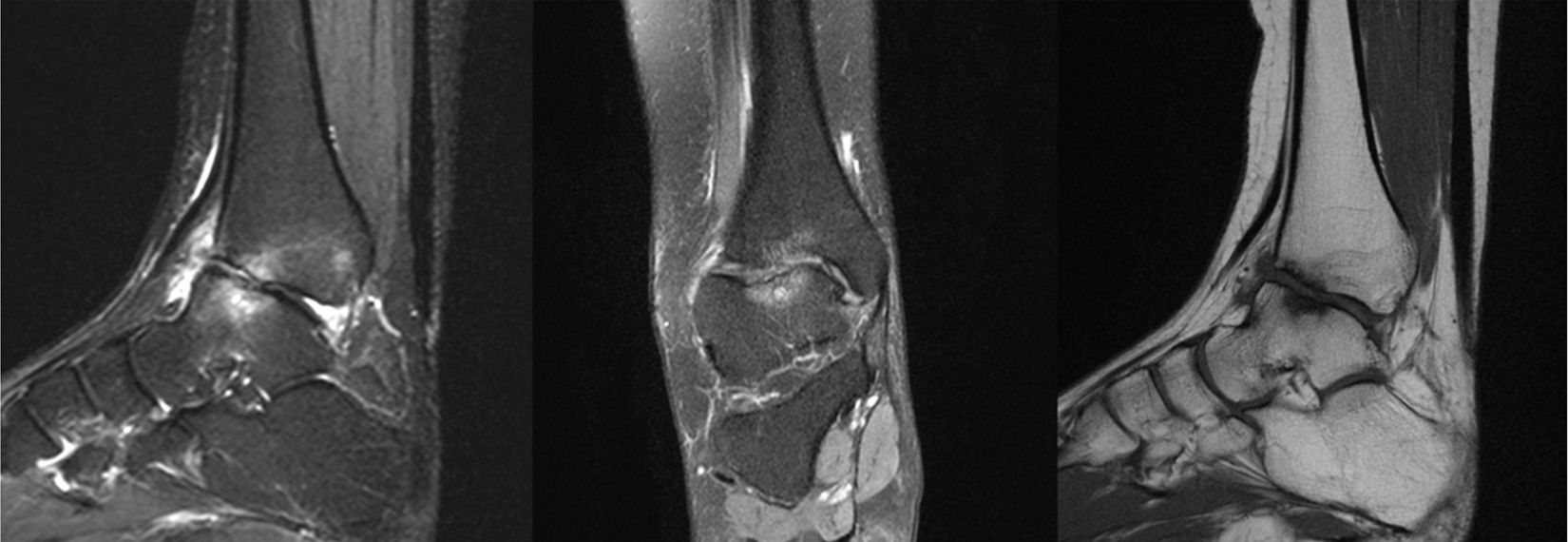
The patient was re-assessed at 12 years of age due to limitation of movement. X-rays with both ankle loads revealed destruction of the articular surfaces of the tibia and astralagus, with osteophytes and involvement of the articular space (Fig. 1). The MRI showed TB sequelae, but with no active synovitis (Fig. 2). Arthroscopy of the ankle was performed, with anterior arthrolysis of the joint, resecting the fibrous tissue and anterior osteophytes.
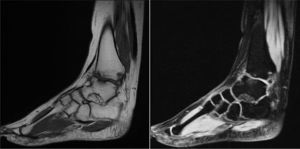
The patient is currently 22 years of age. In the last MRI study TB sequelae appeared (Fig. 3) but he leads a normal life despite this. He is a student and aware of his physical limitations. He swims and cycles and knows he should not run or jump. He occasionally takes anti-inflammatory drugs and has periodic check-ups.
DiscussionThis clinical case is an example of one of the most difficult osteoarticular TB cases to diagnose in its initial stages. For early diagnosis there must be a high degree of clinical suspicion and an early CAT scan and/or MRI should be performed. Despite this, final diagnosis in our case was only reached after the completion of an anatomopathological study one year after symptoms began.
Clinical expressionTuberculous arthritis or osteoarthritis is mono joint in around 90% of cases. It affects the lower limbs in 60–80% of occasions, and the most commonly affected joint in children is the hip. TOA of the foot and ankle represents 10–22% of cases and most commonly compromises the calcaneus and the mediotarsal joint.
Clinical symptoms include swelling, limitation of articular range, moderate intensity pain and limping. Symptoms are subacute or chronic and progressive. The presence of abscesses or fistulisations to the skin is less frequent. Regionally, it is possible to find inguinal or axillary adenopathies.
Additional testsFindings from sample radiography is often non-specific and largely depends on the stage of evolution of the disease. In initial stages radiographies are normal. In evolved cases we are able to observe Pemister's standard triad: juxtaarticular osteoporosis, peripheral localised bone erosion and (progressive) narrowing of articular space.
According to Chen 4 evolutionary levels in TOA may be distinguished.8 At stage 1 there is a synovial lining infection accompanied by mild bone erosion or confined osteoporosis. Stage 2 is characterised by clear bone erosions or tuberculous osteomyelitis, but with no compromise of the articular space. In stage 3 we find greater bone and synovial involvement with loss of the articular space. In stage 4 there is compromise of more than one peritalar joints or the presence of pyogenic arthritis with obvious disorganisation of the bone architecture. Unlike the standard evolution of pyogenic arthritis, in tuberculous osteoarthritis the articular space is preserved up to advanced stages, because the causative agent lacks proteolytic enzymes.
Articular ultrasound scans may show early detection of synovial enlargement, joint effusion, abscesses and bone erosion.
CAT and MRI studies are more reliable for the detection of TOA in its early stages. CAT is useful for assessment of the bone anatomy, to determine whether or not there is cortical discontinuity or joint destruction. The CAT scan is also able to show the existence of abscesses and bone disorders, and is useful as a guide for biopsy puncture. MRI may show up synovial pannus, joint effusion, destruction of joint cartilage, bone erosion, subchondral oedema, abscesses and inflammation. As a result it is considered to be the most useful imaging tool for TOA assessment.9,10
Blood analysis is of little diagnostic value, and may reveal biological inflammatory syndrome of variable intensity. ESR rises in 80–90% of cases. CPR and bone metabolism parameters may also become altered.
DiagnosisThe first consideration to be taken into account for the diagnosis is that on many occasions diagnosis is delayed due to lack of clinical specificity and additional tests. We should therefore consider diagnoses which include pigmented villonodular arthritis, neuropathic arthropathy of the diabetic foot, diseases from deposit of microcrystals (principally gout and chondrocalcinosis), rheumatoid arthritis, sarcoidosis and infectious diseases of subacute evolution, such as Lyme disease, fungal arthritis or secondary syphilis.
The period between the appearance of the initial symptoms and diagnosis is variable, and is on average 18 months. In the review of the literature we found that Dhillon and Nagi11 reported a major diagnostic delay in their series of foot and ankle with intervals between the beginning of symptoms and the final diagnosis of from 2months to 1.9 years. In the review of 70 cases of patients with foot and ankle TOA, made by Gursu et al.2 the mean time for obtaining a final diagnosis since the start of symptoms was 26.4 months.
There are mainly two additional types of tests that can be run to confirm a TB diagnosis in a patient with suspected TOA: the intradermoreaction or Mantoux test and the tests for detection of the production of gamma interferon or blood tests. In his work Shams12 describes that the intradermoreaction test has a sensitivity of 90% in TB, but in cases of tuberculous arthritis there may be up to 15–20% of false negatives according to Pertuiset et al.13
When there is a suspicion of TOA it is recommended that the visceral or lymph node tuberculosis sources be found, since the tuberculous infection test may be quickly provided on demonstration of the BK in the direct sputum sample, bronchial aspiration test, urine test or superficial adenopathy test. These are all sources in which it is must better to search for the BK than in articular fluid or synovial biopsies, due to their paucibacillary nature.14
In the absence of evidence of tuberculosis the systematic search for bacteriological or histological proof is necessary to obtain diagnosis. A sample of articular fluid or synovial tissue is therefore required. For diagnostic confirmation of TOA either the detection of acid-fast bacilli in the direct examination of the sample is required, or the possibility of the culture of the sample in Lowenstein–Jensen medium. It should be noted that in the majority of cases this is a paucibacillary infection and that the growth of the microbacteria is slow, resulting in cultures requiring between 3 and 10 weeks to test positive or negative.2 Rapid TB diagnostic techniques now exist with the use of the CRP, but given the low amount of bacilli in the articular fluid or the synovial tissue, sensitivity to this test is between 53% and 100% according to the series, with specificity generally above 90%.15
TreatmentTOA treatment is mainly medical. All studies converge in that the anti-tubercular drugs most commonly used are isoniazid, etambutol, pyrazinamide and rifampicin. Streptomycin has now fallen into disuse. Recommended duration of treatment is between 6 and 12 months, with the most common recommendation being 9 months of treatment.8
The main indications of surgical treatment for TOA are the presence of soft tissue abscesses (with or without fistulisation) or bone disorders. Other possible reasons for referral to surgery are the lack of response to medical treatment 4–5 months after its initiation.7 Immobilisation of the affected limb is important both to promote pain relief and reduce the risk of breakdown of the articular surface.
At present the rate of cure is above 90%. The main factors governing treatment failure are poor adherence to treatment, malnutrition and the existence of immune deficiency.
With regards to cure criteria, for Dhillon and Nagi10 the following should be met: disappearance of systemic clinical symptoms, normalisation of ESR, radiologic signs of bone reconstruction with osteosclerosis, disappearance of osteolytic lesions and restoration of bone trabeculation. A follow-up of at least 5years is recommended to confirm that curation is definitive.
ConclusionTOA is a disease of complex diagnosis in its initial stages, since its clinical presentation and standard additional tests are often non-specific. This diagnostic difficulty leads to delay in treatment initiation, overshadowing joint prognosis.1,16 MRI is considered to be the most useful tool for diagnosis, and is of great value for assessing the extent of the disease. In any case diagnosis must always be based on a bacteriological and anatomopathological tests. Although surgery must on occasion be used, TOA treatment today is essentially medical.
Level of evidenceLevel of evidence iii.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments have been performed on humans or animals in this research.
Confidentiality of dataThe authors declare that they have adhered to the protocols of their centre of work on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Navarrete FE, Gómez-Alessandri J, Tintó M, Sánchez-González M, Vicent V. Tuberculosis de tobillo. A propósito de un caso en la infancia. Rev Esp Cir Ortop Traumatol. 2017;61:319–323.