To evaluate the outcome of knee fixation without bone fusion using an intramedullary modular nail and interposed cement.
Materials and methodsRetrospective study of 29 infected total knee arthroplasties with prospective data collection and a mean follow-up of 4.2 years (3–5).
ResultsComplications included 2 recurrent infections, 1 peri-implant fracture, and 1 cortical erosion due to the tip of the femoral component. All of these were revised with successful results. The mean limb length discrepancy was 0.8cm, with 24<1cm. Twenty-five patients reported no pain. The mean WOMAC-pain was 86.9, WOMAC-function 56.4, SF12-physical 45.1, and SF12-mental 53.7. Four patients needed a walking frame, and only two were dependent for daily activities.
ConclusionsThe Endo-Model Link nail is an effective method for knee fixation that restores the anatomical alignment of the limb with adequate leg length.
Evaluar los resultados de la fijación de rodilla sin fusión ósea, con clavo intramedular e interposición de cemento.
Material y métodosEstudio retrospectivo de 29 prótesis total de rodilla infectadas con datos recogidos prospectivamente y seguimiento medio de 4,2 años (3-5).
ResultadosLas complicaciones fueron 2 infecciones recurrentes, una fractura periimplante y una erosión cortical en la punta del componente femoral, siendo todas revisadas con buen resultado. La dismetría media fue 0,8cm, con 24<1cm. Veinticinco pacientes no referían dolor. El valor medio de WOMAC-dolor fue 86,9, WOMAC-función 56,4, SF12-físico 45,1, y SF12-mental 53,7. Cuatro pacientes precisaron andador y solo 2 eran dependientes para actividades diarias.
ConclusionesEl clavo Endo-Model Link® es un efectivo método de fijación de rodilla, restaurando la alineación del miembro y adecuada longitud del mismo.
Arthrodesis following failure of total knee arthroplasty (TKA) is a widely accepted technique for limb rescue when the implantation of another prosthesis is not possible or recommended.1 At present the indication of arthrodesis is infrequent,2 with most cases being due to recurrent infection which cannot be controlled through surgical revisions or extensor apparatus lesion. For this reason, the literature is scarce and practically all studies involve short series, with very few works describing more than 30 cases,2 with the exception of that by Mabry et al.,3 which contained 85 cases. Also, due to this low prevalence, all studies up to the present are retrospective assessments.
The objective of conventional arthrodesis is to achieve knee stability without pain through femorotibial bone fusion. At present, the most commonly used methods are external fixation and intramedullary nailing.2 In general, the results described with external fixation have been inferior compared to those obtained through intramedullary nailing3,4 due to a longer time required to achieve bone fusion and a greater rate of complications. Both methods have the potential disadvantage of producing an excessive shortening of the limb in most cases,2 as well as difficulty in obtaining bone fusion in a previously septic environment.5 Another type of permanent knee fixation can be permanent knee stabilization without bone fusion5 through fixation with intramedullary nailing and interposition of a cement block to maintain the length of the limb, such as that obtained with the Endo-Model Link® nail. We have only found 5 studies in relation to this model of nail,7–11 of which only 2 did not carry out femorotibial bone fusion.
The objective of this study is to analyze the functional results obtained in knee fixation without bone fusion by means of the Endo-Model Link® arthrodesis nail, during revision of infected TKA.
Materials and methodsThis was a retrospective study conducted with prospectively collected data. Our database of arthroplasties included all those implanted at our department, with preoperative and postoperative radiographic and clinical data, collected prospectively in a protocolized manner and with a systematized follow-up. The inclusion criteria described consecutive patients treated between 2001 and 2010 with knee arthrodesis due to an infected TKA. There were no exclusion criteria. We identified 29 cases and in all of them the arthrodesis was conducted through surgical revision in 2 stages, using the Endo-Model Link® (Waldermar Link, Hamburg, Germany) intramedullary, modular nail. The relevant characteristics and surgical technique of this device have been described previously.7,10
All revisions were conducted in 2 stages and 5 intraoperative samples for culture were obtained during each intervention. The first stage consisted in prosthesis explantation, surgical cleaning and placement of a non-standardized cement spacer with gentamicin. Infection was treated with specific antibiotic therapy, intravenously for 1 month and orally up to 3 months. Infection was considered cured by normalization of C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) values, along with at least 2 negative cultures obtained by joint puncture (culture and cell count) during the following 3 months. Thus, the interval for the second surgical stage was at least 6 months. Bone scintigraphy scans with marked leukocytes were only carried out in case of diagnostic doubt. The second stage consisted of reimplantation of the TKA if the extensor apparatus had not been damaged or an arthrodesis nail if it had. In cases where the infection recurred after reimplantation, a new surgical revision for arthrodesis was conducted.
The arthrodesis was carried out in a second surgical stage, once the infection was considered cured. We took 5 intraoperative samples for culture. Subsequently, we started specific, intravenous antibiotic therapy according to the results of the previous cultures, during 2 weeks if the new cultures were negative. The arthrodesis nail consisted of 2 chromium-cobalt components of varying lengths, femoral and tibial, which were joined and screwed on each other at the level of the knee, providing a very robust connection with a fixed femorotibial angle of 5° in valgus in the frontal plane and 5° in flexion in the sagittal plane. The stems were introduced after drilling the medullary canals, in a retrograde direction in the femur and in an anterograde direction in the tibia, applying cement only in the metaphyseal portions. Given the technical difficulty of cementing the entire length of the nails, we ensured that an adequate cement filling of the metaphyseal portion was performed and at least 10cm diaphyseally in each component. After attaching both components, the joint space was filled with a cement block with 80mg of gentamicin (Cerafixgenta, Ceraver, France). Specific antibiotic and antithrombotic prophylaxis was applied, and load with a walking frame was permitted after the second postoperative day if pain allowed it.
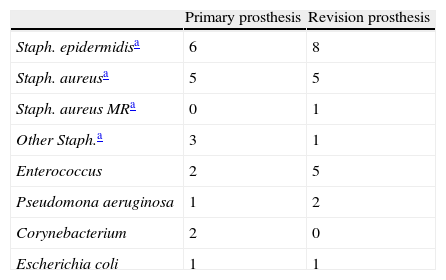
The series consisted of 25 females and 4 males, with a mean age of 74.6 years (range: 59–83 years) at the time of the arthrodesis. The mean body mass index (BMI) was 32.3kg/m2, with 22 patients (75.8%) presenting a BMI≥30, of which 2 cases suffered morbid obesity (BMI≥40). The comorbidities at the time of the arthrodesis were varied, with 11 patients (37.9%) presenting type II diabetes and other associated pathologies, the most frequent being arterial hypertension, cardiopathy and chronic respiratory failure. The initial diagnosis in all cases had been of primary osteoarthritis. In 12 patients, the infection appeared after a primary TKA and in another 17 after an initially aseptic revision. In 12 patients, the infection was associated to a patellar tendon tear (5 cases), skin cover defect (1 case) and severe instability (1 case). All patients presented infection caused by a combination of germs, with some strain of Staphylococcus being identified in 21 patients (Table 1).
All patients had been prospectively examined, clinically and radiographically, at3,6,12 and at least until 36 months after the arthrodesis. The clinical assessment in this study only used the results of the Short-Form (SF1212, physical and mental) and short WOMAC13 (pain and function) questionnaires as variables. The scores of both questionnaires were calculated in a 0–100 scale, so that a higher value indicated a better condition of the patient. Radiographically, we considered the position or change of position of the nail and the loosening through the presence of radiolucent lines. This type of nail did not aim to achieve bone fusion. A radiographic study whilst standing was obtained at 6 months in order to assess length discrepancies between both limbs.
Given the size of the sample, the statistical analysis of results was descriptive. The paired Student's t test and Fisher's exact test were only employed to compare preoperative and postoperative clinical assessments, considering as significant values of P≤.05.
ResultsThe mean follow-up period after the arthrodesis was 4.2 years (range: 3–5 years) and no patients were lost during this time. The mean duration of the surgical intervention, including the extraction of the cement spacer placed in the first stage, was 115min (range: 75–175min).
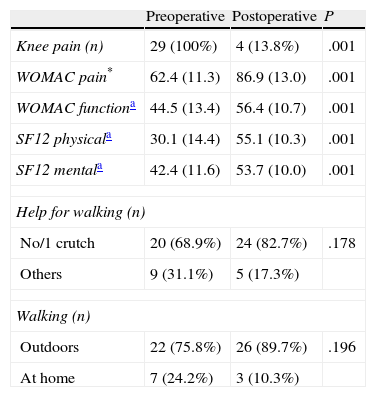
Regarding the condition prior to the arthrodesis, the clinical results improved except for autonomy for walking (Table 2); although it is worth noting that the prior condition was very poor, as it referred to the period in which the cause for arthrodesis was present and before initiating the first stage of surgical revision. In the last assessment, 4 patients reported pain in the knee upon walking, with 3 requiring a walking frame and 1 requiring 2 crutches. One patient reported occasional pain in the thigh and another pain in the lumbar region. The pain was mechanical and constant upon walking in all cases, except in cases of pain in the thigh and lumbar region, when it was occasional. All patients required intermittent analgesic medication of intermediate potency.
Clinical results.
| Preoperative | Postoperative | P | |
| Knee pain (n) | 29 (100%) | 4 (13.8%) | .001 |
| WOMAC pain* | 62.4 (11.3) | 86.9 (13.0) | .001 |
| WOMAC functiona | 44.5 (13.4) | 56.4 (10.7) | .001 |
| SF12 physicala | 30.1 (14.4) | 55.1 (10.3) | .001 |
| SF12 mentala | 42.4 (11.6) | 53.7 (10.0) | .001 |
| Help for walking (n) | |||
| No/1 crutch | 20 (68.9%) | 24 (82.7%) | .178 |
| Others | 9 (31.1%) | 5 (17.3%) | |
| Walking (n) | |||
| Outdoors | 22 (75.8%) | 26 (89.7%) | .196 |
| At home | 7 (24.2%) | 3 (10.3%) | |
In total, 18 patients (62.1%) did not require help to walk, 6 (20.7%) needed 1 cane, 1 (3.4%) needed 2 canes, and 4 (13.8%) needed a walking frame. A total of 26 patients (89.7%) walked outdoors and 3 patients (10.3%) only inside their home. Only 2 patients were dependent for basic, daily life activities. All reported difficulties to climb stairs and to get inside a car.
The mean post-arthrodesis score in the WOMAC-pain scale was 86.9 (range: 55–100), with 4 patients obtaining a score equal to or below 65, and the rest with scores equal to or above 80. The scores in the WOMAC-function scale were notably lower, with a mean value of 56.4 (range: 17–65), with 6 patients obtaining scores equal to or below 50 and the rest obtaining scores equal to or above 55. The patients with the worst function were those who required the most help to walk. The SF12 scales were also notably worse, with a mean SF12-physical score of 45.1 (range: 14–53). Scores lower than 40 corresponded to the 6 patients with the lowest WOMAC-function score. The mean SF12-mental score was 53.7 (range: 28–62), with scores lower than 40 corresponding to the patients who reported pain.
Overall, the arthrodesis was considered to have a poor result in 4 patients (13.8%), due to pain, requiring a walking frame or being dependent for basic, daily life activities.
The last radiographic assessment (Fig. 1) revealed a mean femorotibial alignment of 4.5° in valgus (range: 3°–6°). Two patients presented symptomatic cement-bone radiolucency at the level of the femoral component. Cementing of the femoral nail was insufficient in 2 patients, who presented radiolucent cement-bone lines. The mean length discrepancy between the lower limbs was 0.8cm (range: 0–2cm), with 24 patients presenting a length discrepancy below 1cm, 3 patients with 1.5cm and 2 patients with 2.0cm. These last 5 patients required a lift in their shoes but its use was well accepted by the patients and did not worsen the scores in the WOMAC and SF12 scales.
There were 6 complications after the arthrodesis. The infection recurred in 2 patients, with 1 of them requiring a new revision in 2 stages to place a new arthrodesis nail, cure the infection and eliminate pain, as well as to eliminate the need for walking aids. The other patient was 74 years and was following a palliative treatment program due to severe comorbidities which were not related to the knee and which contraindicated a reintervention. Another patient presented cortical erosion in the proximal end of the nail, with a risk of fracture. The eroded nail was replaced by a longer nail and the patient reported no pain and no need for walking aids. Another patient presented a peri-implant fracture at the level of the proximal end of the nail, due to a fall down a staircase after 3 years, requiring revision and a longer nail, as well as internal femoral fixation with a femoral plate. The patient, who was 95 years, reported no pain but did require a walking frame. Another 2 patients, mentioned previously, presented insufficient cementing of the femoral component, with radiolucent lines at that level. One of them reported pain in the knee and needed a walking frame, whilst the other reported pain in the thigh and needed 2 crutches. There were no cases of implant breakage.
DiscussionThe purpose of this study was to describe the functional results obtained after knee fixation without bone fusion using the Endo-Model Link® intramedullary nail. This method of arthrodesis could not be compared with another, as there was no available cohort with sufficient homogeneity and size, and could not be compared with septic revisions in which a new prosthesis had been implanted due to the bias caused by the different rate of surgical stages on the knee. The clinical assessment did not consider valid the KSS14 scale, as it included variables which were not appropriate for the arthrodesis. Furthermore, there have been doubts regarding the validity15,16 of measurement instruments used in previous arthrodesis studies, such as the Oxford Knee Score17 and Lequesne Algo-functional index,18 in favor of the SF12 and WOMAC questionnaires.
We were only able to find 5 studies in the literature regarding the use of the Endo-Model Link® nail for arthrodesis following TKA failure. Two of them used interposition of cement8,9 and the others reported contact for bone fusion,7,10,11 although there have also been reports of oral communications. Another study19 also used arthrodesis with interposition of a cement block, but with a different modular nail. In our opinion, this was the most extensive study published to date on the use of this nail for arthrodesis following TKA failure for any cause.
At present, the most commonly used techniques for conventional knee arthrodesis are external fixation and intramedullary nailing; although the latter seems to achieve better results3,4 as it provides rigid fixation and enables load immediately.20 Most arthrodesis with intramedullary nailing seek to achieve traditional femorotibial fusion, so it is important to maximize the contact between both bones.3 The nail used in this study sought to achieve mechanical stabilization of the knee without femorotibial fusion,10 so it is difficult to compare it with other techniques except regarding surgical complications and functional results.
In our series, infection did not recur after the arthrodesis in 27 patients (93%), and in the other 2 patients (7%) it was resolved through a new revision in 2 stages and rearthrodesis with a nail. Implantation of an intramedullary nail in a site of previous infection entails a risk of recurrent infection, with a rate of 7–21% for conventional nails,5,21–23 as well as a relevant rate of amputations after arthrodesis failure.5,23 The theoretical advantage of interposing cement with antibiotic in cases of infection has not been demonstrated in previous studies,19,24 with an infection rate of 13%. Our rate of infection was lower and this could be due to the fact that the period of time elapsed between the 2 surgical stages was longer. Like other authors,25 we recommend arthrodesis in 2 stages with a prolonged interval between them in cases of infected TKA.
In order to obtain a stable and painless knee, bone fusion arthrodesis requires gradual and constant compression between the ends of the femur and tibia until the fusion is achieved. Although fusion rates of up to 90% and 100% have been reported,2,21 some of these cases required complementary surgeries for the treatment of consolidation delays and pseudoarthrosis with bone grafts.7,23,25,26
With conventional arthrodesis through nailing it is difficult to achieve an adequate alignment of the limb, which is often21,25 close to 0°, whereas the modular nail without bone fusion has the advantage of its fixed angulation at 5° in valgus, although the result can vary slightly depending on the rotation of the nailing. In our study, the mean femorotibial angulation obtained was 4.5° in valgus, which was similar to other studies using the same implant,8 whereas series using other nails and providing this data report a lower mean angulation, with 0–3° in valgus.23,24
Another drawback is that bone fusion frequently entails an excessive shortening of the limb. None of the patients in our study presented a length discrepancy over 2cm, similarly to other studies which did not use bone fusion.7,8,19 Although a certain degree of shortening is technically desirable to facilitate hip circumduction when walking, several authors recommend that this length discrepancy should not exceed 2cm, as it would hinder normal standing on both legs and entail excessive pelvic balancing, which could cause discomfort at the lumbar level. On the other hand, bone fusion has reported mean shortenings23,25 of 3.0–4.5cm, with 80–100% of the cases presenting over 2cm,24,26 and length discrepancies of up to 6cm.23,24,26
Clinically, 4 patients (14%) in our series reported residual pain in the knee, with 5 patients (17%) needing at least 2 crutches, which represents a discreetly worse result than other studies with a similar technique.7,21 Endomedullary nailing for bone fusion7,21,26 has reported 22–54% of the cases with pain and 33% needing at least 2 crutches. In a series which employed various arthrodesis techniques, Ramazzini et al.9 reported that, at 6 years, 30% of the patients needed 2 crutches or a walking frame. In our study, the functional result was relatively poor, close to 50 points in the WOMAC and SF12 scales, similar to other studies using the same technique.10,19 Nevertheless, a study27 on the validation of the SF12 scale reflected that scores above 50 points represented the mean value among the healthy population, and scores lower than 40 points corresponded to the lower level of 84% of that same population. The use of modular nails to achieve bone fusion9,23 has reported functional values lower than ours.
The Endo-Model Link® arthrodesis nail is associated with the drawback of difficulty to achieve adequate cementing throughout its entire length, so we decided to only cement the first 15–20cm of each component. This had the potential disadvantage of causing pain in the thigh or tibia in cases where an adequate stabilization of the components was not achieved. In our series, only 2 patients reported thigh pain, with this factor not being reported by other authors.
Our study was mainly limited by its retrospective approach and the size of the sample due to the low prevalence. Nevertheless, our series was larger than most in previous reports and the clinical data had been collected prospectively. Another limitation was the mean follow-up time of 4.2 years, because a long-term follow-up would be required to assess potential nail loosening and knee instability.
In conclusion, our results show that most cases of infection can be cured with the knee fixation technique using an Endo-Model Link® nail, as well as its short-term effectiveness to achieve painless stability, provide an adequate length of the limb and facilitate acceptable functional capacity and independence for daily life activities. Nevertheless, further, larger and well-designed studies with a longer follow-up period are required in order to validate the results of this technique.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Miralles-Muñoz FA, Lizaur-Utrilla A, Manrique-Lipa C, López-Prats FA Artrodesis sin fusión ósea con clavo modular intramedular para revisión de prótesis total de rodilla infectada. Rev Esp Cir Ortop Traumatol. 2014;58:217–222.