Long term clinical and radiological evaluation of results, survival, and peri-operative and post-operative complications of the patients who have been operated on for revision total hip arthroplasty using the impaction allografting and cemented rod technique.
Material and methodsAn observational, analytical, prospective and non-random study was conducted on 26 patients who underwent revision total hip arthroplasty in our Hospital (1997–1998). They were clinically and radiologically assessed, and a survival analysis of the implant was performed.
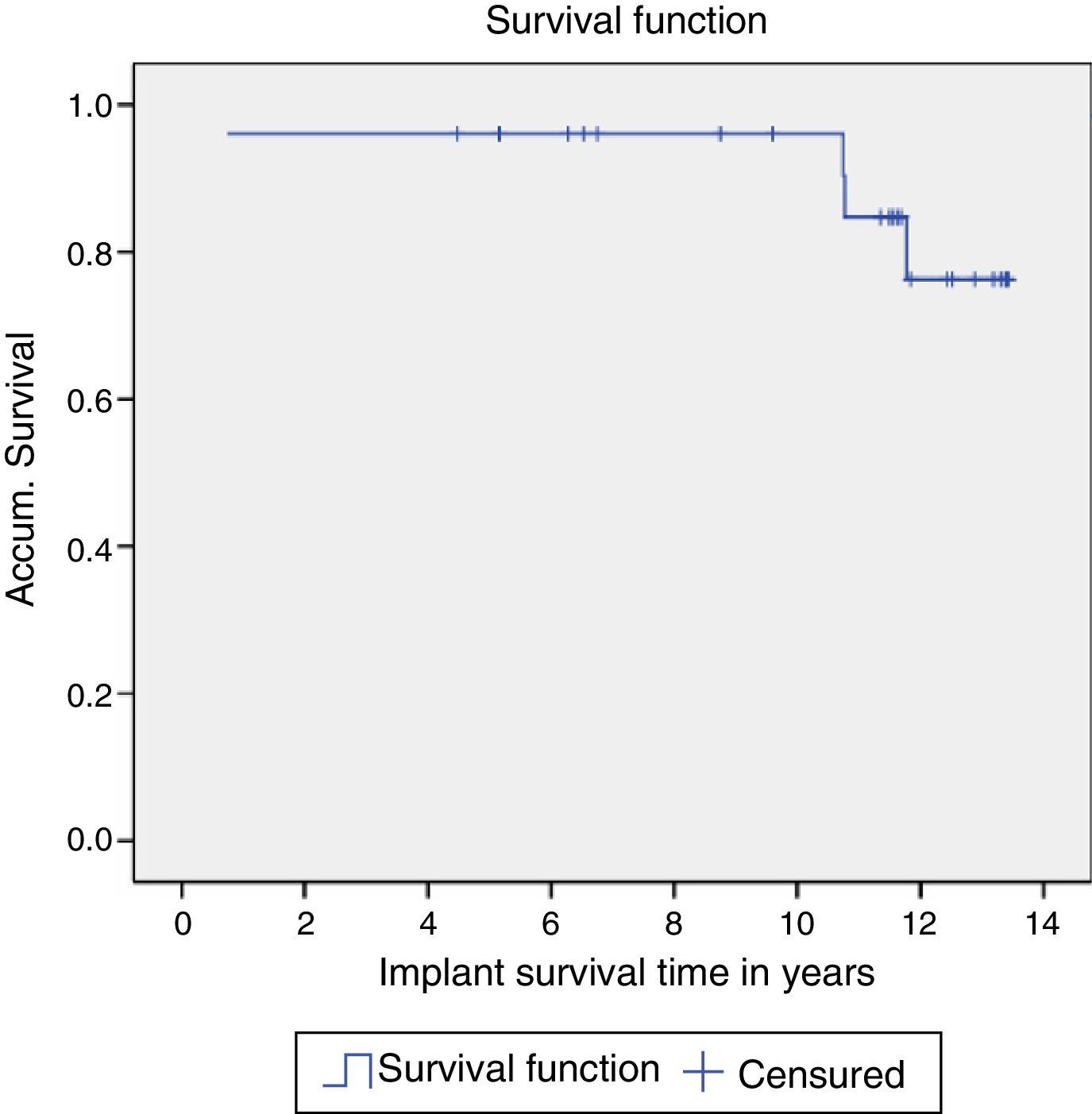
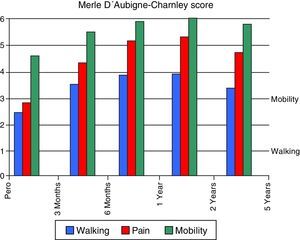
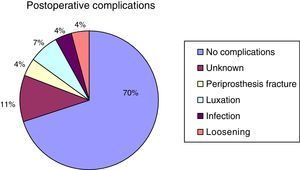
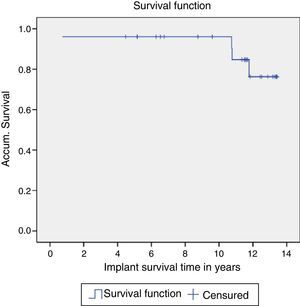
ResultsStatistically significant differences were identified in the pre- and post-operative values, according to Harris and Merle D’Aubigne scores. The femoral components survival was considered as an endpoint of the revision replacement, which was 84% at a mean of 13 years. There were 9 intraoperative complications (6 were fractures) and they significantly affected the length of hospital stay. No post-operative complications were observed in 70% of the patients. None of the analysed variables had any influence on the radiological subsidence of the femoral component.
DiscussionSeveral techniques aim to solve the bone stock deficiency in revision total hip arthroplasty, but only impaction grafting attempts to recover it.
ConclusionsThe Ling's technique shows an improvement over the Merle D’Aubigne and Harris scores, in the medium-long term. The intraoperative complications are mainly an increase in the length of hospital stay and the number of days needed to be able to sit down. Ling's technique is a good option to consider in young patients where it is foreseeable that there is a new revision surgery in the future.
Evaluar a largo plazo, el resultado clínico-radiológico, la supervivencia y las complicaciones intra y postoperatorias de pacientes intervenidos de cirugía de revisión de cadera mediante esta técnica.
Material y métodosEstudio analítico observacional, prospectivo y no aleatorizado de 26 pacientes intervenidos de cirugía de revisión de cadera en nuestro hospital (1997–1998), a los que se les realizó un seguimiento clínico-radiológico y un análisis de la supervivencia del implante.
ResultadosSe observan diferencias estadísticamente significativas en los valores pre y postoperatorios de las escalas de Harris y de Merle D¿Aubigne. La supervivencia del implante teniendo en cuenta como punto final la cirugía de revisión fue del 84% a los 13 años. Hubo 9 complicaciones intraoperatorias (6 de ellas fueron fracturas) e influyeron de forma significativa en la estancia hospitalaria. El 70% de los pacientes no tuvo ninguna complicación postoperatoria. Ninguna de las variables analizadas influyó en el hundimiento radiográfico de los implantes.
DiscusiónDiversas técnicas intentan solventar el déficit de stock óseo en las cirugías de revisión de cadera, pero solo una intenta recuperarlo, el injerto compactado.
ConclusionesLa técnica de Ling ofrece una mejoría clínica tanto en la escala de Merle D¿Aubigne como en la de Harris, a medio-largo plazo. La presentación de complicaciones intraoperatorias incrementa la estancia hospitalaria y los días necesarios para iniciar la sedestación. La técnica de Ling es una buena opción a tener en cuenta en pacientes jóvenes en los que es previsible que haya una nueva cirugía de revisión en el futuro.
The increase in life expectancy and quality of the population over recent years has led to a major increase in the indication for prosthetic hip surgery. The profile of the patients operated has changed over the years, and they are increasingly younger and more demanding about the results.1
Almost 5 decades of technological and surgical innovation have made it possible to improve the duration of primary surgery implants. However, contrary to what may be expected the number of revision surgical operations has also increased enormously in recent years.2 The reasons for this are: the increase in the population operated and the increasing life expectancy of the population. This leads to an increase in the number of load cycles implants are subjected to, while they are also used proportionally more intensely as younger patients are more active.
Based on the results of their study, Kurtz et al. state that the rates of revision surgery in comparison with the total number of prosthetic surgical operations stands at 17% for the hip and 8% for the knee.2
Revision hip surgery is a challenge in itself for any orthopaedic surgeon, due not only to the important bone defects we find and have to overcome, but also because of the need to correctly affix the new implant, even more so in the case of relatively young patients who enjoy good quality of life.
There are several methods that attempt to resolve the problem of bone stock and make it possible to correctly affix a new implant, including cement and special prostheses, etc., but only one method tries to recover the bone, and this is compacted graft.1–4 Compacted and cemented graft prosthesis is now a widely-used technique. A large number of studies reflect how it has evolved clinically, with implant stability and the restoration of bone in revision hip surgery. Good results are obtained over the medium term according to the majority of published series. Nevertheless, it must not be forgotten that this technique is difficult, laborious and not free of complications such as postoperative fractures and excessive subsidence of the implant.1,3–9 With the exception of the Swedish registry and the Exeter school, few studies offer an average follow-up longer than 10 years.3,5
The aim of this study is to evaluate the results of 13 years’ usage of morselized compacted allograft and cemented stem (Ling's technique) in revision hip surgery, evaluating clinical results, implant survival, intra- and postoperative complications and the subsidence of implants as detected by X-ray.
Material and methodThis is a prospective non-randomised observational analytical study. 26 patients operated for revision total hip replacement in the Hospital de Cabueñes, Gijón, were studied. The compacted graft technique had been used in all of them in the femoral component, from August 1997 to December 1998.
All patients were subjected to a survey and clinical evaluation: preoperative, at the moment of hospital discharge, 6–12 weeks after surgery, at 6 months, at one year, 2 years and 5 years, to record the differences on the Harris and Merle D’Aubigne-Charnely scales, if there were any. Afterwards patients were evaluated routinely in annual visits during up to 13 years. Implant subsidence was also measured by comparing immediate postoperative X-rays with those of the most recent check-up. This measured the vertical subsidence of the femoral stem using the method described by Callaghan et al.10 All X-rays were taken using the same protocol, and any possible variations in magnification were corrected by taking the size of the femoral head as reference.1 The centre of the femoral head and the line between the two Köhler tear drops are used to define the height and position of the dome. The blocked holes were used as the reference when Köhler's tear drop was not visible.11 All measurements were made by the same observer, who was a member of the surgical team.
The revision hip surgery patients included in the study were operated due to: loosening of the components, subsidence of the stem, femoral osteolysis, infection, pain and luxation. To eliminate possible distortions the following exclusion criteria were applied: patients whose revision surgery was only of the acetabulum, patients in which a structural allograft or technique other than the one described was used, patients who were implanted with a femoral stem other than the standard Exeter® (Stryker Howmedica, U.S.A.) one.
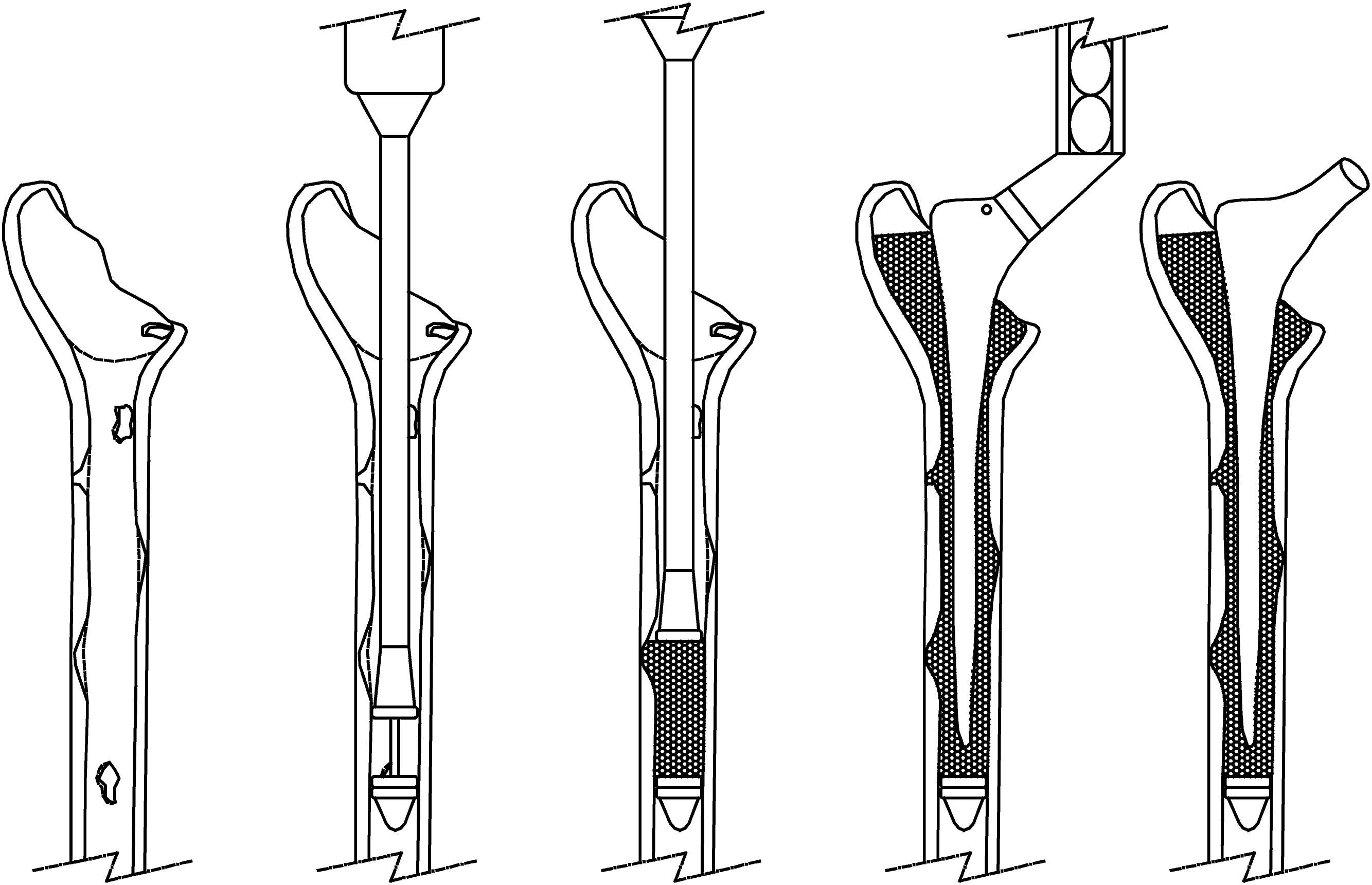
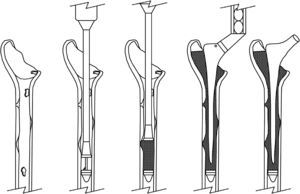
Frozen allografts of femur heads were used that had been preserved in liquid nitrogen in a tissue bank. The allografts were ground in a bone mill (Noviomagus Bone Mill®, Denmark). The femoral channel was prepared and graft insertion commenced. Once compacting had finished (Fig. 1), the stability of the test implants was checked and then it was cemented, pressurised and the definitive stem was inserted.
The following variables were analysed: age, sex, weight, height, BMI, EEII dissymmetry, the side operated, Harris Hip Score or HHS, score on the Merle D’Aubigne- Charnely scale, the duration of surgery, intraoperative bone quality, Paprosky's classification of femoral defects, number of days necessary before sitting, number of days necessary before walking, postoperative hospitalisation and implant subsidence detected by X-ray.
Qualitative variables were compared by means of the chi-squared test. Given the limited number in the sample, quantitative variables were compared using non-parametric tests. Subsequently, in those cases in which statistically significant differences had been observed, the corresponding parametric test was performed to obtain the interval of confidence of the difference as additional information. A 95% interval of confidence was set for comparisons, accepting the differences found as significant when the value of P was below 0.05.
Survival analysis used the Kaplan–Meier procedure. A life table was constructed for this, estimating the accumulated proportion of survival in time ti from the date of the operation until death or the last date of follow-up and drawing the survival curve.
ResultsThe group studied had an average age of 72.6 years, an average BMI of 27.4 and an initial HHS score before the operation of 35.2. 53.8% of the sample were men, in 73.1% the right hip was operated and in 76.9% it was the first revision surgery.
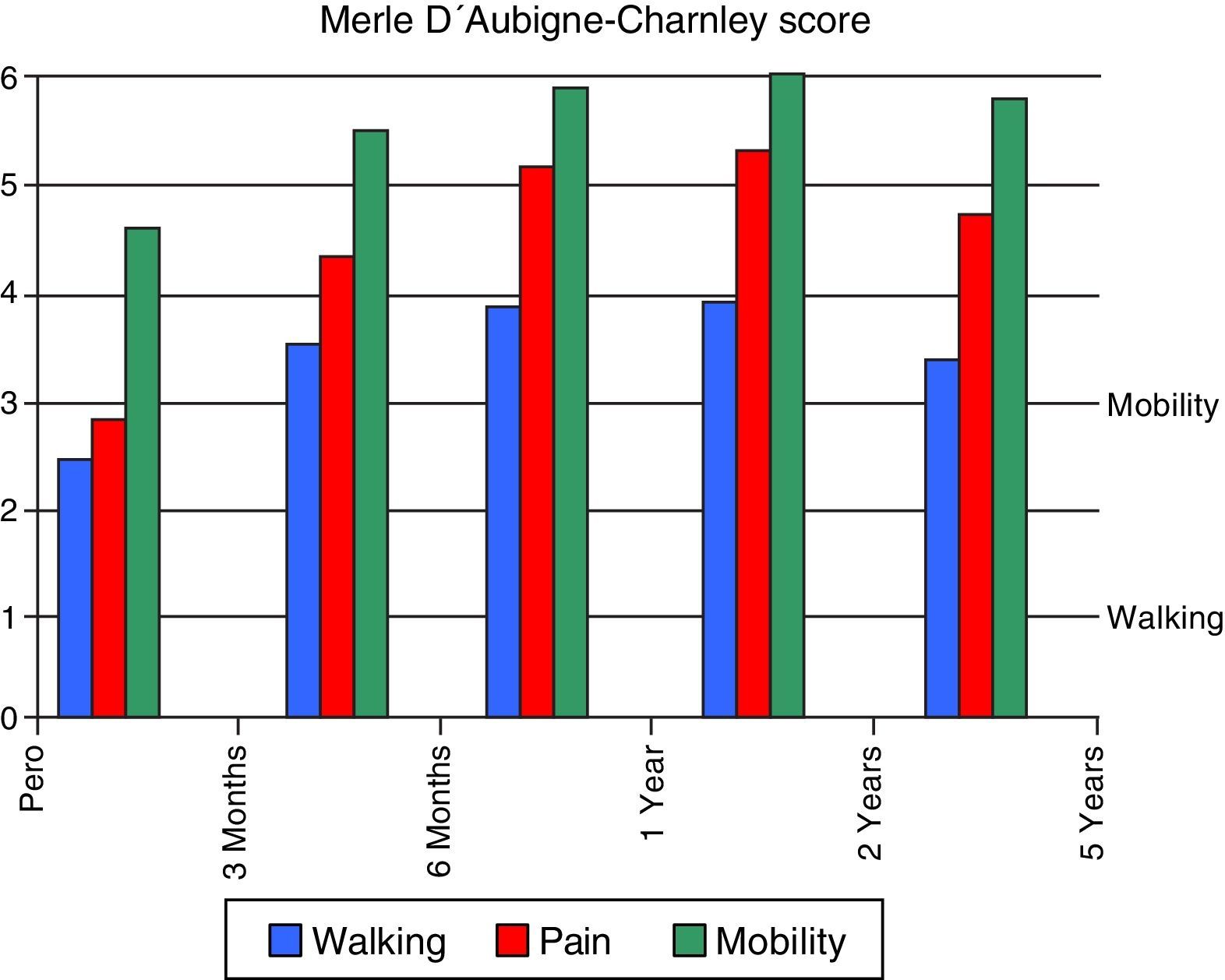
When the variation between the total preoperative and postoperative HHS and Merle D’Aubigne-Charnley scores are analysed, those for mobility and walking rise, with a statistically significant reduction in pain. Final scores are close to double the initial ones for HHS and are notably higher in the 3 categories of the Merle D’Aubigne-Charnley score, above all for pain (Fig. 2).
Of the 26 patients operated, intraoperative complications arose in 9 cases, of which 6 were femoral fractures when compacting the graft with the impactor. The other 3 patients had bone perforations, which although they can be considered fractures their treatment does not involve the same difficulty or risks. The most common location of the fractures was in the femoral calcar (4 cases), while one other fracture occurred in the greater trochanter and the other was at the level of the end of the stem. The possible influence the factors of age, BMI, sex, bone quality, implant size and type of bone defect on intraoperative complications was analysed, and no statistically significant differences were found (P<.05) in any case.
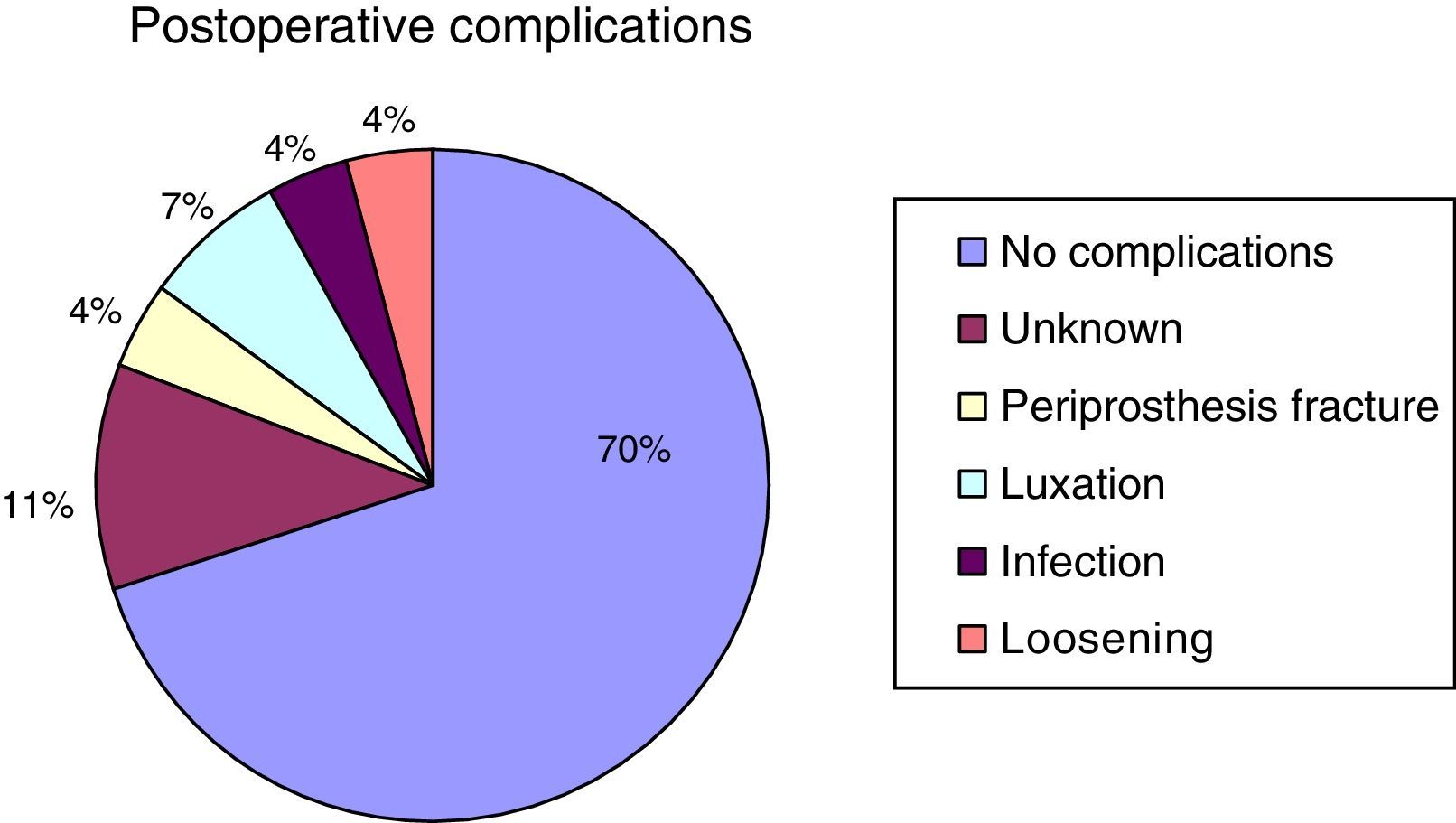
Intraoperative complications were evaluated in terms of their affect on patient progress regarding hospitalisation and time to sitting up and walking. The average time taken achieve sitting was 11.64±5.6 days and this was 17.64±4 days for walking, with an average hospitalisation of 22.3±6.8 days. A statistically significant difference was found in hospitalisation as well as the days necessary to start walking in those patients who had had some type of intraoperative complication.70% of the patients operated had no complications. 3 patients were lost, amounting to 11% of the total. The complications consisted of one infection (4%), one periprosthetic fracture (4%), one case of loosening with clinical involvement (4%) and 2 luxations (7%) which occurred in the same patient, requiring two repeat operations (Fig. 3).
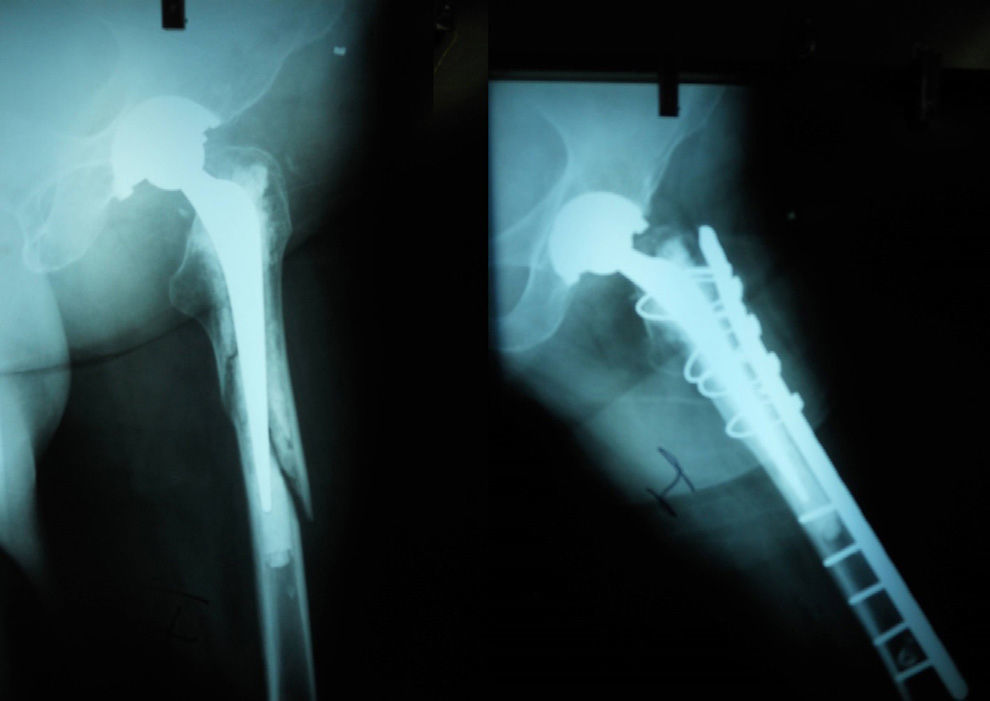
When implant survival is considered to be the final reference, revision surgery for all causes amounted to 84% at 13 years, 88% if we exclude the infection. Only 4 revision surgical operations occurred: one due to infection, one due to fracture and 2 due to luxation (both in the same patient) (Fig. 4).
The last aim was to evaluate the subsidence of implants over time as detected by X-ray, examining whether the different variables recorded influenced this significantly or not. Data analysis showed that in 20 patients radiography detected subsidence of less than 0.5cm, 3 with from 0.5 to 1cm and 3 others with subsidence greater than 1cm. With these results we are able to state that there are no statistically significant differences which would indicate that age, BMI, the duration of surgery, sex, bone quality, the type of bone defect or implant influence the subsidence of implants as detected by X-ray (Fig. 5).
DiscussionBone graft preparation technique is important mechanically as well as biologically. The standard is still fresh-frozen femoral head graft.7 Spongy as well as cortical graft can be used for grinding, although comparative clinical studies such as that by Kligman et al. show that patients with cortical graft have less pain and less subsidence than those with spongy graft.12 The technique used to prepare grafts was that described by Slooff et al., Gie et al. and Schreurs et al., and it is the one used in the majority of the publications on this subject in the literature.1,3–6,8,11–15
The ideal size of bone fragments has yet to be determined, and the only thing that is known is that they have to form a solid base for the implantation of the new prosthesis.8 Tagil and Aspenberg proved that the size is not only important in biomechanical terms, as it is also important biologically, as the more compacted the graft, the less the bone grows.11,16 Halliday et al. showed experimentally that the strength of the compacted graft depends above all on the distribution of the graft itself and correct compacting technique which distributes loads as uniformly as possible.3 Ornstein et al. emphasise that the only thing achieved by vigorous compacting is an increase in the rate of intraoperative fractures. They also stated that incorrect pressurisation of the cement causes rates of subsidence of up to 11% in the series analysed, so that it is necessary to find a balance between correct pressurisation, which reduces the risk of subsidence, and vigorous impacting which affects revascularisation and increases the risk of intraoperative fractures.9
Respecting implant type, in our series Exeter® rods were used in all cases, following the technique described by this school. The latest studies show that correct impacting and graft preparation are more important than the type of stem used.17 (Fig. 6).
Our series shows a significant improvement in the Harris scale as well as in the Merle D’Aubigne-Charnley score. This is so at the first check-up and at 3 months, while it attains the maximum difference at 2 years, after which it falls moderately until 5 years while still leaving a clear margin of difference. These results agree with those of previous studies.1–7 As may be seen in the literature, there is a high risk of fracture during extraction of the cement as well as graft impaction,18 this being the most common cause of new surgery following a revision.3 Intra- and postoperative complications are clearly reduced if patients are carefully selected.6
The calcar is the most frequent location of fractures, and cortical perforations in the most distal part of the stem are also very common.19 Prevalence varies from one study to another, although they range from about 4% to 20% in the majority of publications,3,19,20 and are greater in those with smaller samples. In our series the fracture rate was 23%, which may have been influenced by the sample size and, as in other publications, by the fact that the calcar was the most compromised location.
Greenwald et al. were the first to state in a publication that to prevent fractures when removing the cement it is better to keep the cement that is properly fixed and place the new cemented stem over it.6 At first this practice was strongly questioned in the medical literature, but subsequent studies have shown that this is the technique of choice in appropriate circumstances, as it gives greater levels of strength.21,22 As is described in many articles, in those patients with very deficient bone stock it was necessary to use mesh and cerclage to contain the compacted graft.4
There is very little information in the literature that was revised about hospitalisation times and how many days are necessary before walking and sitting up. Comparison with other European hospitals is very complicated, given the wide differences between healthcare systems. Our analysis shows that there is a statistically significant difference (P<.05) between the existence of complications during surgery and increasing length of hospitalisation. It was also concluded that complications prolong the time that is needed before starting to sit up, although this is not the case for starting to walk.
As was the case for intraoperative complications, the series analysed show widely varying data on implant survival rates. These run from those in series such as Ornstein's, which give survival rates of 94% at 15 years when this is considered to be the end of revision surgery,5 to rates like Halliday's, which falls to 90.5% at 10 years.3 Our series gives an implant survival rate of 84% at 13 years, when this is considered to be the end of revision surgery.
Respecting postoperative complications, a total rate of 19% was found in our series, of which 4% corresponded to periprosthetic fractures, 4% to infections, 4% to loosening and 7% to luxations. These figures are in line with those published by Halliday et al., although in this series there was no luxation.3
Component migration was evaluated by measuring the vertical subsidence of the femoral stem using the method of Callaghan et al.10 Subsidence was termed significant if it were greater than 10mm according to Koldstad's criteria.23 Yan et al.6 state that implant subsidence occurs above all in the first months, stabilising when the graft starts to osteointegrate with the bone. In other publications,4 initial subsidence is associated with poor pressurisation technique, while massive subsidence is associated with previous bone defects.
Ornstein et al.7 studied compacted graft and concluded that subsidence arises in the cement interface, i.e., that the implant sinks into the cement, with average subsidence of 0.3cm, and that it occurs above all during the first 3 months, after which it tends to stabilise. Subsidence of more than 10mm was observed in 11% of cases, and subsidence greater than 5mm was considered to be due to initial stability defects and defective stem alignment. In our series an average subsidence of 0.4cm was observed, while in 76% of patients subsidence was less than 0.5cm, in 12% it was from 0.5 to 1cm, and in 12% it was greater than 1cm.
García-Cimbrelo et al.1 state that subsidence is associated with lower-diameter stems than required, this surely being due to the surgeon's learning curve and possible difficulties in estimating stem size. With our results we cannot state that any of the variables we analyse (age, BMI, duration of surgery, previous bone defect, sex, implant type or bone quality) significantly influence subsequent implant subsidence as shown by X-ray, although the results of the articles which were revised suggest this.
The following limitations to this work should be underlined: its design, as it was not a blind study. This means that the analysis of subsidence detected by X-ray may have been influenced by subjective factors; sample size, which may not have been large enough to give statistically significant results, and the lack of a control group which would show objective results by comparing different population samples.
ConclusionsBased on the results of our work, and as is reflected in the most relevant literature, we can state that the use of compacted graft technique with cemented stems (Ling's technique) in femur revision surgery makes it possible to achieve good results over the medium to long term, with absence of pain and with reconstruction of the bone substrate. Despite its technical difficulty and frequent intraoperative complications, mainly periprosthetic fractures, and the loosening of the implant due to excessive subsidence of the same, it is indicated above all in young patients for whom a second revision operation will be reasonable.
Level of evidenceLevel of evidence iv.
Ethical responsibilitiesProtection of people and animalsThe authors declare that no experiments with human beings or animals were undertaken for this research.
Data confidentialityThe authors declare that they followed the protocols of their hospital on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is held by the corresponding author.
Conflict of interestsThe authors do not have any conflict of interests.
Please cite this article as: Mateo-Negreira J, López-Cuello P, Pipa-Muñiz I, Rodríguez García N, Murcia-Mazón A, Suárez-Suárez MA. Evaluación clínico-radiológica de la técnica de aloinjerto compactado y vástago cementado en cirugías de revisión de cadera. Rev Esp Cir Ortop Traumatol. 2016;60:141–147.