To compare results in terms of orthopaedic complications and quality of life in elderly patients with subtrochanteric fracture treated with intramedullary nailing according to fracture reduction status.
Patients and methodsA prospective cohort study including 90 elderly patients with subtrochanteric fractures of the femur treated with a cephalomedullary nail, with a minimum 1-year follow up. The inclusion criteria were: aged 60 years or older, without severe cognitive dysfunction and independent ambulatory capability before the fracture. We defined 3 different groups in relation to fracture reduction status: good, acceptable and poor, according to modified criteria from Baumgartner et al. We compared clinical and surgical characteristics and healthy quality of life, social function and mobility according to the EQ-5D, Jensen Index and Mobility Score of Parker and Palmer questionnaires.
ResultsWe found differences in time to union, better in the good reduction group (p=.002); need for open reduction, more frequent in the good reduction group (p<.001), and in postoperative complications, more frequent in the poor reduction group (p=.001). We found no significant differences between the 3 groups regarding scores in quality of life, social function and mobility.
ConclusionsReduction in subtrochanteric fractures in older people is key to obtaining better clinic and surgical results, improving time to union and decreasing surgical complications. Exposure of the focus fracture seems to be a safe manoeuvre. Quality of life had substantially deteriorated n these patients, but a there was a tendency, although not statistically significant, for it to improve in patients after good surgical reduction.
Comparar el resultado en cuanto a complicaciones traumatológicas (osteosíntesis) y calidad de calidad de vida en pacientes adultos de edad avanzada con fracturas subtrocantéreas tratados con enclavado intramedular según el estado de reducción de la fractura.
Pacientes y métodosEstudio de cohortes prospectivo de 90 pacientes con fractura subtrocantérea con mínimo de un año de seguimiento. Los criterios de inclusión son: edad mayor de 60 años, sin disfunción cognitiva y capacidad de deambulación independiente previa fractura. Se establecen 3 grupos según la calidad de reducción: bueno, aceptable y malo, de acuerdo con los criterios modificados de Baumgartner et al. Comparamos grupos en cuanto a características clínicas y quirúrgicas, y los cuestionarios de calidad de vida, función social y movilidad de EQ-5D, Jensen Index y Mobility Score de Parker y Palmer.
ResultadosEncontramos diferencias estadísticamente significativas en tiempo de consolidación, menor en el grupo «bueno» (p=0,002); en apertura del foco de fractura, más frecuente en el grupo «bueno» (p<0,001) y en complicaciones quirúrgicas, más frecuentes en el grupo «malo» (p=0,001). No hemos encontrado diferencias estadísticamente significativas en puntuaciones de calidad de vida, función social y movilidad.
ConclusionesLa reducción en fracturas subtrocantéreas en adultos de edad avanzada es clave a la hora de obtener los mejores resultados, mejorar el tiempo de consolidación y disminuir las complicaciones quirúrgicas. La exposición del foco de fractura parece ser una maniobra segura. La calidad de vida de estos pacientes se deteriora de manera ostensible, con una tendencia, estadísticamente no significativa, a mejorar en aquellos pacientes en los que se consigue una buena reducción.
Subtrochanteric fractures comprise between approximately 5% and 20% of all extracapsular hip fractures. They still pose a surgical challenge due to their particular instability and configuration, with the proximal fragment in abduction, external rotation and flexion, which makes them difficult to reduce and synthesise. Osteoporosis and comorbidities present in elderly patients further complicate treatment of these fractures.1–4
In recent years, various research studies have established that surgery with intramedullary nails is optimal due to the biomechanical advantages that they offer over other devices, with rates of pseudoarthrosis and reoperation of approximately 10%.5–11 However, major reductions in the quality of life of these patients have been observed.12,13
Intramedullary nailing has traditionally been considered not to be an invasive technique, since it is not considered necessary to open the focus fracture to reduce it, and other indirect methods of reduction are used on the traction table or with external elements. Furthermore, there is the potential risk of infection and pseudoarthrosis due to manipulation of the focus fracture. The concept of stabilising and reducing pain in the elderly patient over that of reduction and functionality appeared to be sufficient when treating these fractures given to the dangers that direct manipulation of the focus fracture seemed to entail.14–18 However, recent studies have shown no further complications, even when reduction elements such as clamps and cerclage wires are used.19–26
Some studies12,13 have shown reduced scores in terms of quality of life in these patients, although, to our knowledge none of them directly relate quality of life with fracture reduction.
The aim of this study was to compare results and prognosis in terms of orthopaedic complications (reoperations and pseudoarthrosis) and the quality of life of patients with subtrochanteric fractures treated with intramedullary nailing according to the reduction status of the fracture.
Patients and methodsThis was a prospective cohort study which included 90 patients with subtrochanteric fractures from a series of 726 extracapsular hip fractures treated with intramedullary nailing in our hospital from January 2009 to December 2012, with a minimum of one year's follow-up. The inclusion criteria were: aged over 60 years, with no severe cognitive dysfunction and able to walk independently with or without the aid of a stick or crutches before the fracture. Pathological, tumour and atypical fractures were excluded. This series belongs to a line of research into subtrochanteric fractures in our department that has already been described in other papers.26
Three groups were established according to the quality of reduction: good, acceptable and poor, according to the following modified criteria of Baumgartner et al.27,28: (1) less than 10° angulation on radiographic monitoring (antero-posterior and lateral); (2) less than 5mm displacement of the principal fracture fragments (except the minor trochanter) and (3) less than 5mm separation of the principal fracture fragments. Fractures that met the 3 criteria were included in the “good” group, those that met only 2 were included in the “acceptable” group, and those that met one or none in the “poor” group.
Data on age, sex, size of fracture, type of nailing, surgical delay in days, surgery time, duration of hospital stay and mortality in the first year were included. Infections below the fascia lata that required surgical revision were defined as deep infections or implant infections.
Cognitive status was assessed during the initial assessment of the patients using the Short Portable Mental Status Questionnaire. The patients with severe cognitive dysfunction (3 or fewer correct answers) were excluded from the study. General health status was assessed using the ASA scale (American Society of Anaesthesiologists) by the corresponding anaesthetist.
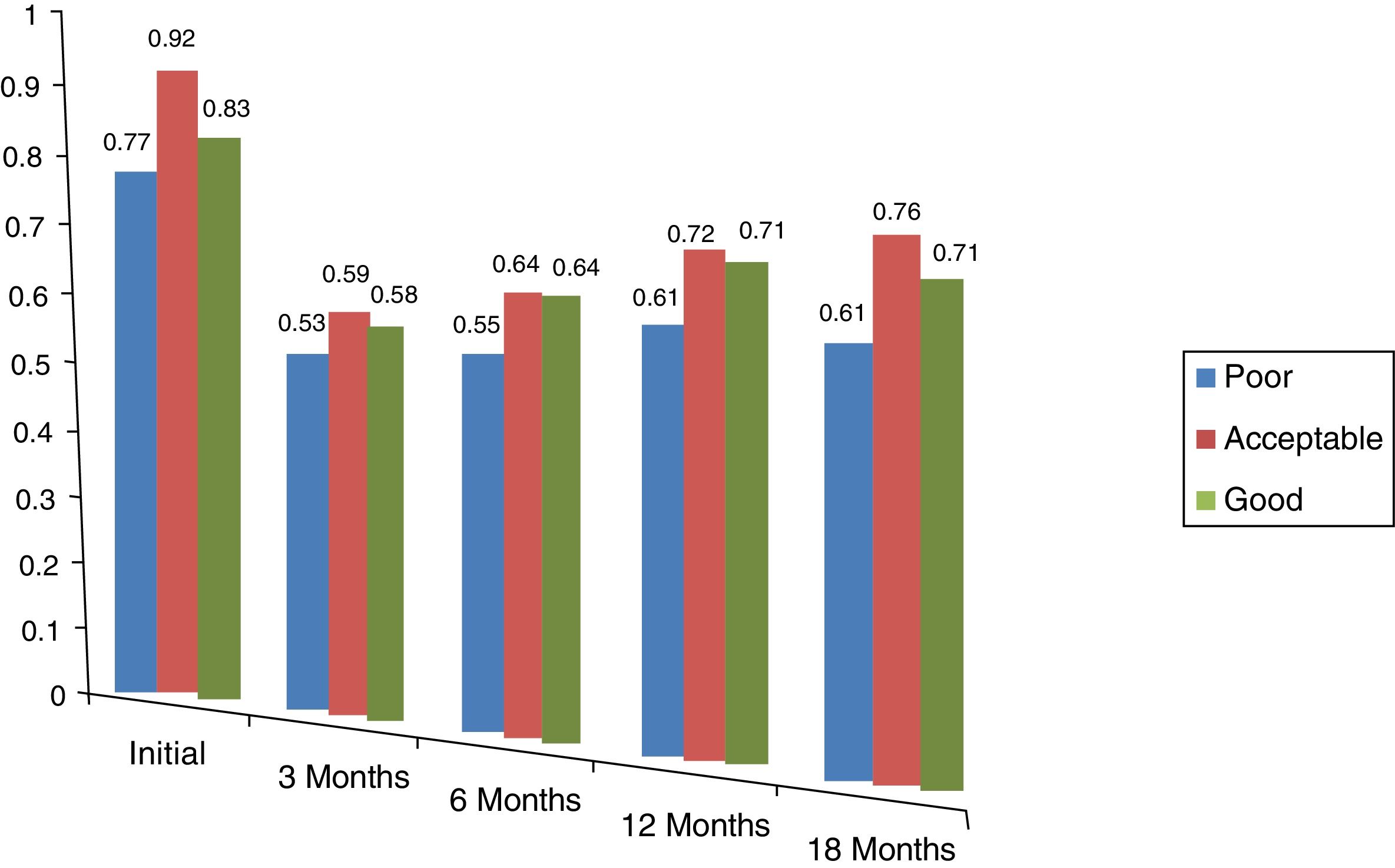
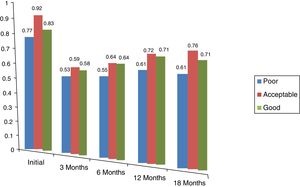
The EuroQol-5D (EQ-5D) questionnaire was used to evaluate quality of life,12,13 determining the status prior to the fracture and repeated at 3, 6, 12 and 18 months following surgery, either by telephone interview or during the follow-up consultations. Each dimension examined was divided into 3 grades of severity: no problems, some problems, and many problems. The scores ranged from 0 to 1 (1 being the best possible health status and 0 the poorest).
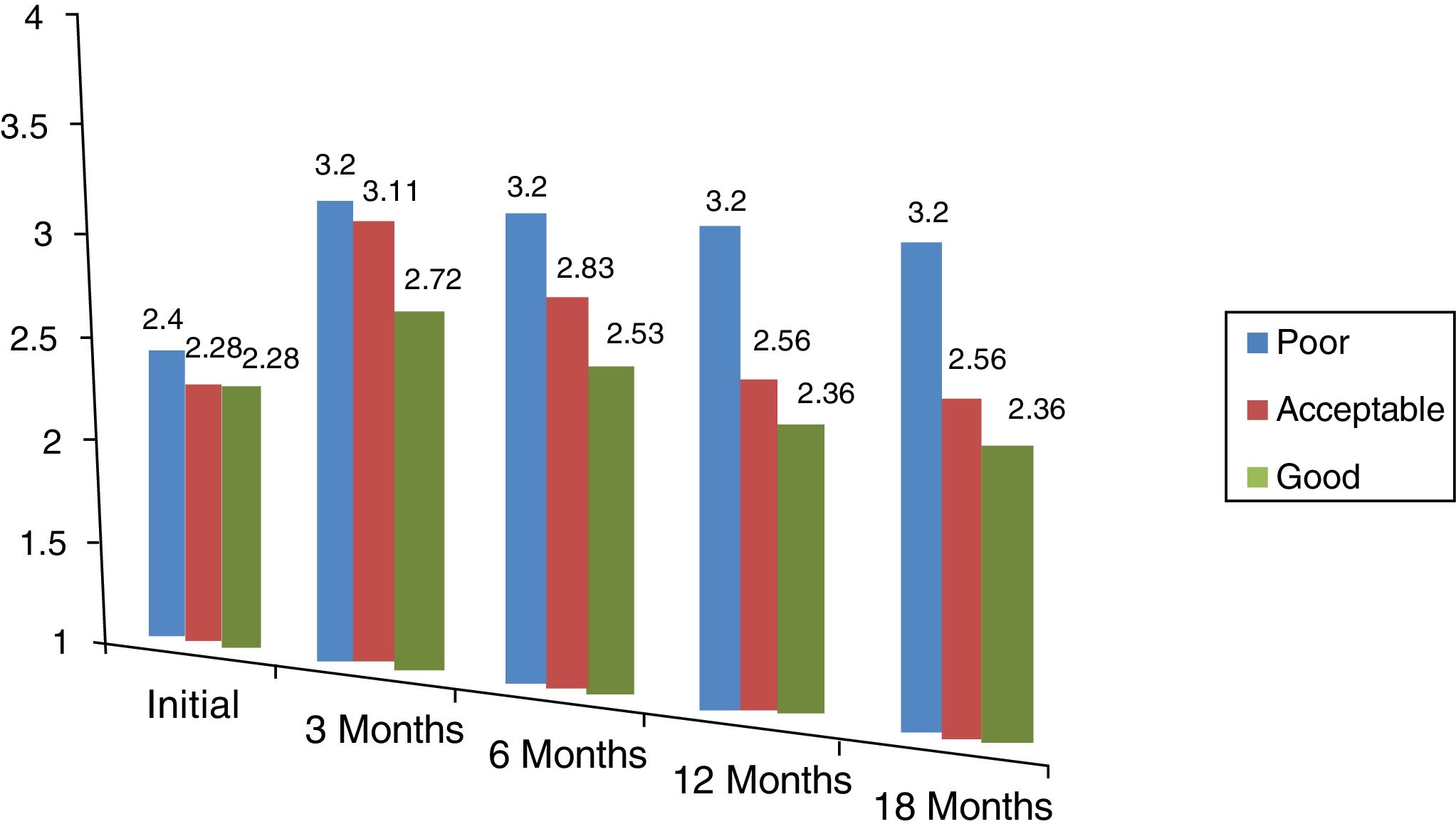
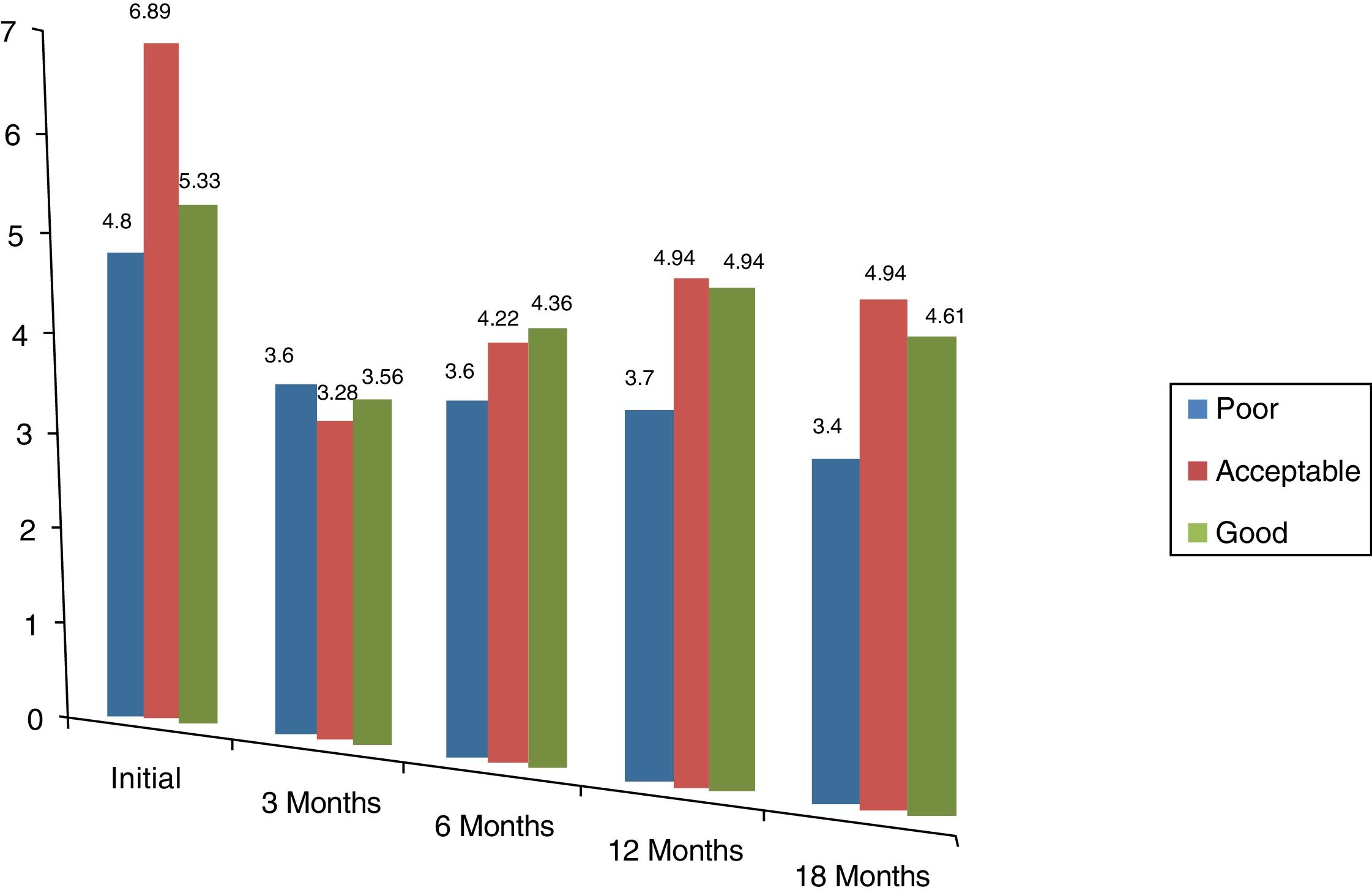
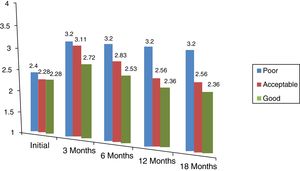
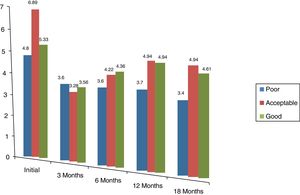
The patient's interaction/social function status was evaluated using the Jensen Index Assessment of Social Function,29 which is divided into 4 grades: independent (1), somewhat independent (2), moderately independent (3) and totally dependent (4). The grade of mobility was also assessed using Parker and Palmer's Mobility Score,30 which ranges between 0 and 9 points from total inability to walk (0) and ability to undertake activities such as the daily shop or going to a restaurant. (9) In both cases, the questionnaires were applied again to determine the status prior to the fracture and were repeated at 3, 6, 12 and 18 months after surgery.
The fractures were classified using the system of the Orthopaedic Trauma Association (AO/OTA) for subtrochanteric fractures (32 A-B-C) and intertrochanteric fractures that extended to the subtrochanteric region (31-A3) including reverse oblique fractures.31 We also used Seinsheimer's classification system for subtrochanteric fractures.32
Complications from traumatic causes that required reoperation, delayed union, defined as a lack of union after a minimum of 6 months’ follow-up, and pseudoarthrosis, defined as a lack of union after a minimum of 9 months’ follow-up, were considered orthopaedic complications.
All the operations were performed on a traction table. Closed or open reduction methods by opening the focus fracture were performed independently by the corresponding surgeon according to their judgement in each particular case. In the cases that underwent opening of the focus fracture, an incision was made on the focus and reduction forceps (Verbrugge) and cerclage wires were used to maintain the reduction and subsequent insertion of the nail. The nails uses were: Gamma nail (Stryker, Kalamazoo, MI, USA), Charfix nail (ChM, Juchnowiec Kościelny, Poland, USA), Zimmer MDN nail (Zimmer, Warsaw, IN, USA), and the PFN nail (Synthes, West Chester, PA, USA). Short nails were used for 23 cases, and long for the remaining 67.
Statistical analysisInitially we performed a descriptive analysis where the qualitative variables were expressed as frequencies and percentages. The continuous variables were expressed as mean±standard deviation, median (minimum–maximum). The Kolmogorov–Smirnov tests were used to establish the normality of the variables.
Parametric and non-parametric tests were performed to determine the potential association between the study variables (Chi-squared, Friedman, Kruskal–Wallis and one-factor Anova).
Differences with a p<.05 were considered statistically significant in all the analyses. The analyses were performed using SPSS 15.0.
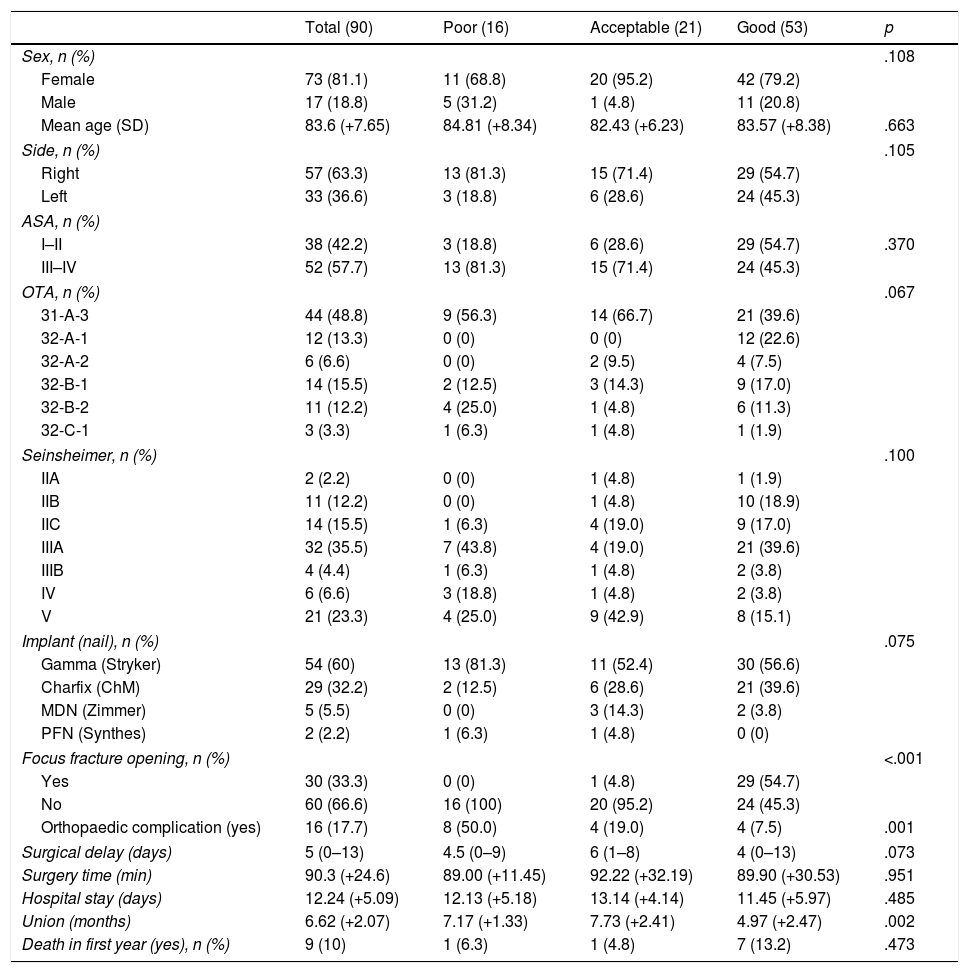
ResultsAccording to the reduction criteria established, 53 cases were considered to be in the “good group”, 21 in the “acceptable” group, and 16 in the “poor group”. The surgical features and data of the patients are shown in Table 1. There were no significant differences in terms of age, sex or side of fracture. In all the groups the fractures were more frequent in women over the age of 80, and on the right side. No significant differences were found in terms of classification of the fracture, type of implant, ASA, mortality in the first year, surgical delay, surgery time or duration of hospital stay. None of the patients developed a deep infection.
Clinical features and surgical data of the 3 groups.
| Total (90) | Poor (16) | Acceptable (21) | Good (53) | p | |
|---|---|---|---|---|---|
| Sex, n (%) | .108 | ||||
| Female | 73 (81.1) | 11 (68.8) | 20 (95.2) | 42 (79.2) | |
| Male | 17 (18.8) | 5 (31.2) | 1 (4.8) | 11 (20.8) | |
| Mean age (SD) | 83.6 (+7.65) | 84.81 (+8.34) | 82.43 (+6.23) | 83.57 (+8.38) | .663 |
| Side, n (%) | .105 | ||||
| Right | 57 (63.3) | 13 (81.3) | 15 (71.4) | 29 (54.7) | |
| Left | 33 (36.6) | 3 (18.8) | 6 (28.6) | 24 (45.3) | |
| ASA, n (%) | |||||
| I–II | 38 (42.2) | 3 (18.8) | 6 (28.6) | 29 (54.7) | .370 |
| III–IV | 52 (57.7) | 13 (81.3) | 15 (71.4) | 24 (45.3) | |
| OTA, n (%) | .067 | ||||
| 31-A-3 | 44 (48.8) | 9 (56.3) | 14 (66.7) | 21 (39.6) | |
| 32-A-1 | 12 (13.3) | 0 (0) | 0 (0) | 12 (22.6) | |
| 32-A-2 | 6 (6.6) | 0 (0) | 2 (9.5) | 4 (7.5) | |
| 32-B-1 | 14 (15.5) | 2 (12.5) | 3 (14.3) | 9 (17.0) | |
| 32-B-2 | 11 (12.2) | 4 (25.0) | 1 (4.8) | 6 (11.3) | |
| 32-C-1 | 3 (3.3) | 1 (6.3) | 1 (4.8) | 1 (1.9) | |
| Seinsheimer, n (%) | .100 | ||||
| IIA | 2 (2.2) | 0 (0) | 1 (4.8) | 1 (1.9) | |
| IIB | 11 (12.2) | 0 (0) | 1 (4.8) | 10 (18.9) | |
| IIC | 14 (15.5) | 1 (6.3) | 4 (19.0) | 9 (17.0) | |
| IIIA | 32 (35.5) | 7 (43.8) | 4 (19.0) | 21 (39.6) | |
| IIIB | 4 (4.4) | 1 (6.3) | 1 (4.8) | 2 (3.8) | |
| IV | 6 (6.6) | 3 (18.8) | 1 (4.8) | 2 (3.8) | |
| V | 21 (23.3) | 4 (25.0) | 9 (42.9) | 8 (15.1) | |
| Implant (nail), n (%) | .075 | ||||
| Gamma (Stryker) | 54 (60) | 13 (81.3) | 11 (52.4) | 30 (56.6) | |
| Charfix (ChM) | 29 (32.2) | 2 (12.5) | 6 (28.6) | 21 (39.6) | |
| MDN (Zimmer) | 5 (5.5) | 0 (0) | 3 (14.3) | 2 (3.8) | |
| PFN (Synthes) | 2 (2.2) | 1 (6.3) | 1 (4.8) | 0 (0) | |
| Focus fracture opening, n (%) | <.001 | ||||
| Yes | 30 (33.3) | 0 (0) | 1 (4.8) | 29 (54.7) | |
| No | 60 (66.6) | 16 (100) | 20 (95.2) | 24 (45.3) | |
| Orthopaedic complication (yes) | 16 (17.7) | 8 (50.0) | 4 (19.0) | 4 (7.5) | .001 |
| Surgical delay (days) | 5 (0–13) | 4.5 (0–9) | 6 (1–8) | 4 (0–13) | .073 |
| Surgery time (min) | 90.3 (+24.6) | 89.00 (+11.45) | 92.22 (+32.19) | 89.90 (+30.53) | .951 |
| Hospital stay (days) | 12.24 (+5.09) | 12.13 (+5.18) | 13.14 (+4.14) | 11.45 (+5.97) | .485 |
| Union (months) | 6.62 (+2.07) | 7.17 (+1.33) | 7.73 (+2.41) | 4.97 (+2.47) | .002 |
| Death in first year (yes), n (%) | 9 (10) | 1 (6.3) | 1 (4.8) | 7 (13.2) | .473 |
We found statistically significant differences in terms of time to union, which was lower in the “good” group (p=.002). The number of cases that underwent opening of the focus fracture was 0 (0%) in the “poor” group, 1 (4.8%) in the “acceptable” group and 29 (54.7%) in the “good” group. Opening of the focus fracture was statistically significant and much more common in the “good” group (p<.001). Surgical complications in osteosynthesis were significantly greater in the “poor” group, at 50% (5 pseudoarthrosis, 2 cut-outs, one peri-implant rupture), 19% in the “acceptable” group (2 pseudoarthroses, 2 delayed unions that required removal of distal screws) and 7.5% in the “good” group (one cut-out, 2 delayed union and one distal screw protrusion that required removal of the distal screw) (p=.001).
We found no significant differences between the 3 groups with regard to quality of life scores in the EQ-5D questionnaire, the Jensen Index or the Parker and Palmer Mobility Score at 3, 6, 12 and 18 months (p>.05). However, we did see more favourable results from the 3 questionnaires in the groups in which the fracture reduction was considered better (Figs. 1–3).
Subtrochanteric fracture reduction is key to its correct treatment in the elderly and to reducing the number of orthopaedic complications and rates of pseudoarthrosis, as has been shown in other studies.5,6,19,20,26 It also produces a clear tendency to improvement in terms of the quality of life of the elderly patient, who often have many baseline comorbidities and diseases that make them difficult to manage clinically. In our study we found shorter times to union and reduced surgical complications the better the fracture reduction (Figs. 4–5).
We know from other studies that these patients’ quality of life deteriorates after this type of fracture12,13: our study is no exception, although none establish a clear relationship between this reduced quality of life and surgical results in terms of reduction. As this study demonstrates, although the results are not significant, there is a clear tendency to improve parameters such as mobility, social interaction and general state of health when a good fracture reduction is achieved. We believe that ours is currently the only study to directly relate the quality of the fracture reduction obtained in surgery with parameters that influence the function and quality of life of these patients long term. This, in short, is our main objective as surgeons. Therefore we highlight the importance of correct reduction and helping other surgeons to pursue this objective.
Closed reduction is often difficult to achieve with subtrochanteric fractures. The traction table can have a paradoxical effect on the proximal fragment, in such a way that the varus and its flexion increase, requiring external elements for correct reduction. In our study, we found that opening the focus fracture was significantly more in the groups with better reduction. It is not our objective to, and neither can we, establish a relationship between opening the focus and improved quality of life, because this technique was chosen at random by the individual surgeon according to intraoperative needs since it had not been possible to perform a good closed reduction previously. However, we can confirm that in some cases where a closed reduction is not achieved, it is necessary to open the focus fracture and achieve the best possible reduction either by using reduction clamps or permanent or temporary cerclage wires.20–26 Cerclage wires have not been shown to increase postoperative complications.18,19,22,24 However, they should be used with care as neurovascular injuries have been described,33,34 although we had none in our study. Their correct use can even re-establish medial cortical support and improve the stability of the fracture. Other studies only use reduction clamps or only recommend the used of cerclage wires if absolutely necessary.21–23 In our routine practice, when opening the focus fracture is necessary, we used reduction clamps with cerclage wires—that act as a framework—even in osteoporotic fractures, because they maintain correct reduction, particularly in fractures with several fragments. Again, one of the strengths of this study is that we focussed on achieving a good reduction above avoiding manoeuvres such as opening the focus fracture for fear of greater complications.
We acknowledge that this study has some limitations. The fact that the reduction method was chosen independently by the individual surgeon, without confirming whether the decision to open the focus fracture was made from the outset or as a rescue method might affect the subsequent clinical results. At present, we recommend achieving a correct reduction before inserting the intramedullary nail. Despite the prospective nature of the study, the interview method can give subjective results in terms of correct interpretation, since these are elderly patients in the majority and it is their family members that help or prompt a specific response. Therefore we should interpret these results with care.
Another limitation that we found in this study and in others, concerned the type of subtrochanteric fracture referred to. The classification of subtrochanteric fractures remains a matter of debate.35,36 The AO classification describes subtrochanteric fractures as those that occur between the minor trochanter and 5cm below it. Seinsheimer's classification includes this area and fractures that extend to the trochanteric region, which in the AO classification are considered intertrochanteric, such as the reverse oblique fracture. We opted to include them all in this study, due to similar biomechanical behaviour (proximal fragment in abduction, external rotation and flexion) which leads us to refer to them as subtrochanteric in daily specialist practice. However, we acknowledge that the management and prognosis of a simple fracture in 2 fragments are not the same as those of a multi-fragmentary fracture with trochanteric extension. Therefore we consider that more individual studies are required according to fracture type and new classifications.
Finally, we recognise that reaching a consensus on definitively determining union using X rays in routine clinical practice is a limitation. With respect to our previous paper published in 2017, we performed a new revision of times to union and found slightly higher figures, which reconfirms the inter and intra-observer variability described in several studies.37,38 In addition, we considered the delayed union of these types of fractures a complication.
ConclusionsReduction of subtrochanteric fractures in elderly adults is key to achieving better clinical and surgical results. If necessary, reduction should be achieved by exposing the focus fracture and using reduction clamps or cerclage wires, since this appears to be a safe manoeuvre. In our study, better fracture reduction was associated with a shorter time to union, a greater need to open the focus fracture and fewer surgical complications. The quality of life of patients with subtrochanteric fracture ostensibly deteriorates, and there is a tendency, not statistically significant, for it to improve for those for whom a good reduction is achieved. This study might encourage surgeons to be more ambitious in terms of achieving better fracture reduction using both closed and open methods in order to improve their patients’ quality of life.
Level of evidenceLevel of evidence II.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Codesido-Vilar P, Mejía-Casado A, Riego-Fernández J, Rodriguez-Casas N, García-Cabanas S, Rivas-Felice J, et al. Consecuencias de la calidad de reducción sobre complicaciones en la osteosíntesis y calidad de vida en pacientes adultos de edad avanzada con fractura subtrocantérea. Rev Esp Cir Ortop Traumatol. 2018;62:240–247.