The fabella is a sesamoid bone present in 30% of the population and, in the majority of cases, it is shown in the proximal head of the lateral gastrocnemius articulating with the lateral femoral condyle. Fabella syndrome is an uncommon disease and it must be considered when dealing with posterolateral pain that increases with extension of the knee. Because of its rarity and underdiagnosis, the literature reports few articles relating to its therapeutic management. The articles reviewed demonstrate that conservative treatment has high recurrence rates, surgical excision being the most effective treatment to eradicate symptoms. We found exceptional articles in the literature related to the surgical treatment of fabella syndrome in professional athletes. In this article we report the surgical experience of a 21-year-old elite swimmer who achievedcomplete pain relief and fast recovery after surgical excision of the fabella.
La fabela es un hueso sesamoideo presente en un 30% de la población y en la mayoría de ocasiones se encuentra en el vientre proximal del gastrocnemio lateral articulando con el cóndilo femoral postero-lateral. El síndrome de la fabela es una entidad poco frecuente y debe considerarse ante un dolor en el ángulo posterolateral de la rodilla que se exacerba con el extensión de la misma. Dada su rareza e infradiagnóstico, en la literatura se recogen escasos artículos sobre su manejo terapéutico. En los artículos revisados, el tratamiento conservador presenta altas recidivas siendo la exéresis quirúrgica de la fabela el tratamiento más eficaz para la remisión definitiva de los síntomas. La experiencia documentada del tratamiento quirúrgico en deportistas de alto nivel es excepcional. Presentamos el caso de un nadador de élite de 21 años que, tras la exéresis quirúrgica de la fabela, presentó una recuperación completa y una rápida incorporación a la competición.
The fabella (or os fabelae) is a sesamoid bone that is present in 30% of the population. It is more common in individuals of Asian origin, and it is bilateral in 80% of cases.1 This bone is 5–10mm in diameter and it is usually (87%-97%) located in the proximal belly of the lateral gastrocnemius, which is articulated with the posterolateral femoral condyle of the knee.2 The fabella is associated with the common peroneal nerve, which runs laterally, although there may be anatomical variations.3 As a sesamoid bone, it is considered to play a biomechanical role, in this case by redirecting knee flexion forces.4
The clinical importance of this sesamoid bone is hardly documented in the bibliography. Fabella syndrome refers to posterolateral knee pain associated with the presence of the os fabelae. The cause of this pain is attributed to synovial capsule inflammation or the femorofabellar chondral lesion that is caused by the mechanism of friction.5 Other cases have been documented, including fabella stress fracture, impingement following total knee arthroplasty or compressive phenomena such as common peroneal nerve neuropathy.6
Fabella syndrome must be included within the differential diagnosis for all pain in the posterolateral angle of the knee. Characteristically, pain in this entity is exacerbated by knee extension, as it is at this point when the fabella exerts the greatest pressure on the posterior femoral condyle. Problems with the meniscus have to be ruled out, as does injury to the posteroexternal complex stabilisers.
Although the first imaging test should be a simple X-ray, this does not show us the anatomical relationships of the fabella with adjacent neurovascular structures. The use of ultrasound scan is a great help in studying the dynamic behaviour of the fabella with the posterior femoral condyle, identifying possible chondral lesions and detecting the location of the common peroneal nerve. We will use magnetic resonance imaging to study the degree of chondral impact and to rule out associated problems in the meniscus or ligaments. Likewise, in the case of neuropathy of the common peroneal nerve, we will base ourselves on an electromyography.
Regarding treatment, little literature exists on therapeutic management. The articles reviewed describe high rates of relapse for conservative treatments, and surgical exeresis of the fabella is the most effective treatment for the definitive remission of symptoms. Likewise, documented experience of surgical treatment in a high level sports person is exceptional.
Clinical caseWe present the case of a 21 year-old patient, a competitive high-level 200m butterfly stroke swimmer who had pain that had gradually evolved over 6 months in the posteroexternal angle of the left knee which prevented training and competing. The patient described the first symptoms of pain as commencing when thrusting when turning over and kicking against the water. The intensity and frequency of the pain had increased over recent months, with pain when walking during the knee extension phase and continuous orthostatism. The patient mentioned no previous trauma or knee instability symptoms. Physical examination found that the patient had a normal alignment of the lower limbs, with no abnormal lengths or other structural alterations. There was no articular bleeding or any signs of inflammation. Meniscus manoeuvres were negative, and there was no mediolateral or anteroposterior instability. There was no pain when the articular interline was pressed, and nor was there any femoropatellar pain. The patient had selective pain when the posteroexternal angle was pressed when the knee was hyper-extended. Joint balance was complete and there were no symptoms of compressive neuropathy.
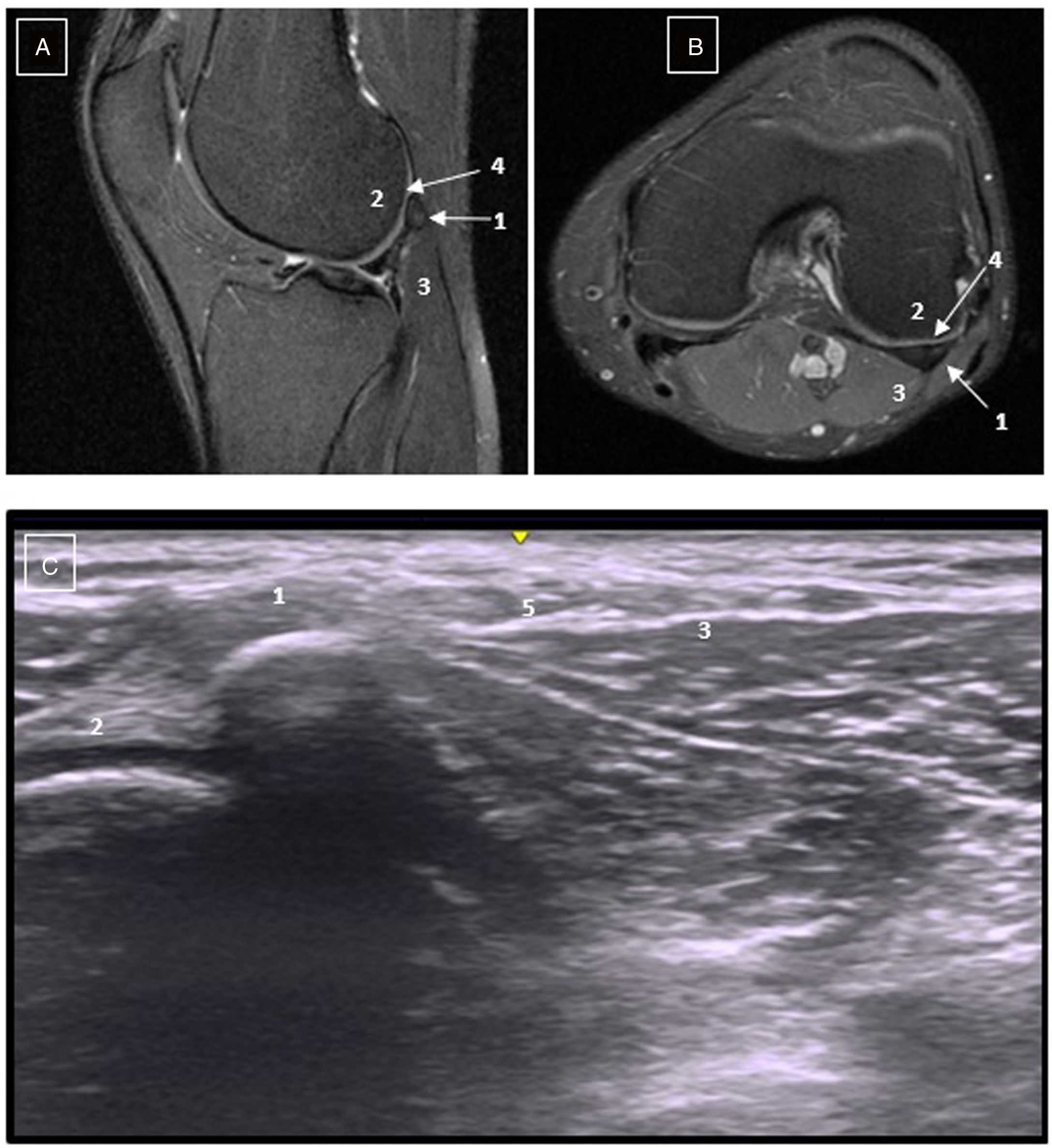
A simple X-ray image shows the presence of the fabella, without any other noteworthy findings in the bones. The NMR study showed chondral irregularity and flattening of the posterolateral femoral condyle caused by contact with the fabella. Problems with the meniscus or ligaments were ruled out. We performed an ultrasound scan in which we observed the dynamic behaviour of the fabella, identifying the articular impression it leaves on the femoral condyle. We also identified the common peroneal nerve, which was, contrary to its usual position,3 in the medial margin of the fabella (Fig. 1).
A) NMR: sagittal slice. B) NMR: transversal slice. C) Ultrasound scan. 1: Fabella. 2: Posterolateral femoral condyle, note the chondral irregularity of the lateral femoral condyle in comparison with the medial. 3: Proximal belly of the lateral gastrocnemius. 4: Femoral condyle chondral flattening. 5: Common peroneal nerve.
After diagnosis, rehabilitation treatment was prescribed using manual therapy, muscular strengthening, masotherapy and radial shock waves. After 3 months of conservative treatment the patient said that there had been no improvement, and an ultrasound-guided infiltration was suggested as a means of reducing discomfort. Nevertheless, given the amount of time spent without competing and seeking a definitive solution, the patient rejected the infiltration and we decided to perform a fabellectomy, based on the experience documented by some authors.
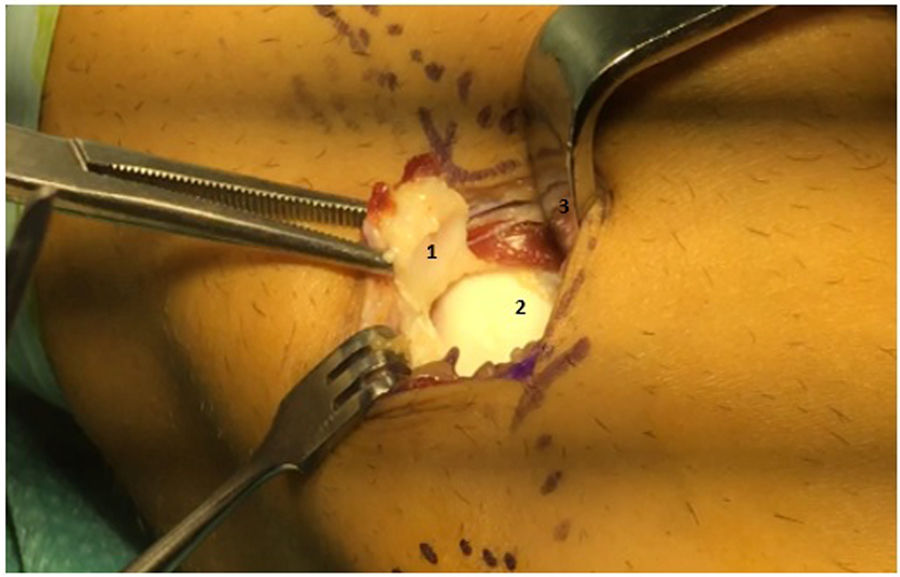
An ultrasound scan was performed prior to the operation, precisely identifying the adjacent anatomical relationships as a sure guide for our surgical approach, and to economise the surgical incision (Fig. 2). The medial location of the common peroneal nerve was confirmed. Under local-regional anaesthetic a longitudinal incision was made in ht e posterolateral edge of the knee, and access was gained through the femoral biceps insertion and belly of the lateral gastrocnemius. The common peroneal nerve was identified and separated medially to protect it during surgery. After identification of the sesamoid bone it was extracted, showing a central chondral lesion and its impression on the lateral femoral condyle (Fig. 3).
The patient was discharged without complications on the same day as surgery, with no neurovascular or surgical wound complications. After the removal of the stitches and bandage the paciente described an immediate improvement, with pain-free complete extension of the leg. He started physiotherapy one week after surgery and commenced readapting to sport in hte water after 3 weeks. The paciente restarted sports training after 6 weeks with gradually increasing intensity, and after 3 months of readaptation he once again started to take part in high level competition, with excellent performance.
DiscussionDue to the rarity and probable under-diagnosis of fabella syndrome, there are few articles about its therapeutic management.
Conservative treatment is documented, with not very encouraging results. Physiotherapy, local infiltration or shock waves are the main treatments that have been described for this syndrome.7 The longest series in the literature presents 16 patients who were treated by physiotherapy and local corticoid infiltration; 11 of these 16 patients did not improve in any way, and they were subsequently subjected to surgical exeresis of the fabella, reporting complete remission of the symptoms after .5–7 years of follow-up.8
A review of the bibliography shows that the majority of patients for whom conservative treatment failed were subjected to surgical exeresis of the fabella. 13 papers have been published to date that describe experience with a total of 27 cases of fabellectomy. The first case described dates from 1929, by Lepoutre, who achieved the complete remission of the patient’s symptoms after attributing their posterolateral knee pain to the presence of the os fabelae.9 The next paper was published in 1981 by Takebe, who performed fabellectomy on 3 patients with fabella syndrome associated with neuropathy of the common peroneal nerve.6 Weiner describes the longest series: he achieved complete recovery in 11 patients after the failure of conservative treatment.8 The other papers published are case reports that describe an excellent clinical result. Erichsen obtained a good result after fabella exeresis in a patient operated for total knee arthroplasty,10 as did Rankin in a patient following femoral desrotational osteotomy.11 The majority of documented fabellectomies use an open posterior approach, although techniques are also described for its arthroscopic exeresis.12 Of all the patients described, only one is an elite sportsman who was able to commence competing again 4 months after surgery.13
The case we present corresponds to a high-level sportsman who, after the failure of conservative treatment which prevented him from competing for a long time, was definitively cured by fabellectomy with a short recovery period. Our result may therefore be added to the encouraging results described in the literature.
Although no neurovascular complications have been described after surgery, we consider that there is the potential risk of common peroneal nerve lesion due to its close relationship and anatomical variability. We therefore believe that the use of ultrasound scan imaging during the operation makes it possible to precisely identify adjacent anatomical structures and ensure a surgical approach that has a lower risk of complications.
ConclusionsFabella syndrome is a rare entity that should be considered in case of pain in the posteroexternal angle that worsens with knee extension. There is little literature on its therapeutic management. In the papers that were reviewed, conservative treatment had a high relapse rate, and surgical exeresis of the fabella is the most effective treatment for the definitive remission of the symptoms. Documented experience of surgical treatment in individuals who practice sport at a high level is exceptional. In our case we obtained an excellent clinical result with swift return-to-play. Given the intraoperative risk of injury to the common peroneal nerve due to its anatomical variability and relationship with the fabella, ultrasound scan imaging should be considered as a useful tool to optimise the surgical approach.
Level of evidenceLevel of evidence V.
Ethical responsibilitiesProtection of people and animalsThe authors declare that no experiments were conducted on human beings or animals for this paper.
Data confidentialityThe authors declare that they followed the protocols of their centre of work regarding patient data confidentiality, and that all of the patients included in this paper received sufficient information and gave their informed consent in writing to take part.
Right to privacy and informed consentThe authors declare that no patient data appear in this paper. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Loscos S, López-Vidriero R, López-Vidriero E. Síndrome de la fabela en un nadador de élite. Rev Esp Cir Ortop Traumatol. 2020. https://doi.org/10.1016/j.recot.2020.04.008