We report a case of fever of unknown origin, in its classical presentation. A wide range of studies were unrevealing, but finally a positron emission tomography/computed tomography allowed us to establish the diagnosis of rhabdomyosarcoma in the pelvic region.
Describimos un caso de fiebre de origen desconocido, en su forma clásica de presentación. Numerosos estudios diagnósticos llevados a cabo mostraron resultados no concluyentes, pero finalmente la tomografía de emisión de protones/tomografía computarizada nos permitió llegar al diagnóstico de rabdomiosarcoma de la región pélvica.
Fever of unknown origin (FUO) has classically been defined as the existence of fever in excess of 38.3°C lasting for at least three weeks and without any aetiological diagnosis, following at least one week of diagnostic studies.1 However, the appearance of new illnesses and new diagnostic procedures in recent decades has meant that the classic concept of FUO is no longer applicable to all cases of prolonged fever and, as a consequence of this, new concepts have been developed, such as FUO in HIV infection, nosocomial FUO or FUO associated with neutropenia.2We present a case we have had an occasion to deal with and which corresponds well with a classic form of FUO, in that the prolonged fever was the most striking symptom and in which numerous diagnostic tests were normal or non-conclusive. Finally, a relatively new imaging procedure, namely proton emission tomography/computed tomography (PET/CT), turned out to be very useful in establishing the diagnosis. There are several examples similar to ours in recent literature, where this same technique has demonstrated its usefulness in the diagnosis of FUO.3–5
Case reportA female, 42 years old, with a personal history of smoking and scoliosis, was admitted due to a mainly evening-time fever lasting for two months, along with asthenia, anorexia with a loss of about 6kg in weight, nausea, vomiting, irritative cough, cephalea and diffuse abdominal pain. Physical examination only highlighted slight paleness, while the rest was normal.
Laboratory analyses gave the following results: haemoglobin 8g/dL with normal mean corpuscular volume, platelets 756,000mm−3, fibrinogen 685mg/dL, activated partial thromboplastin time 42s, protein C reactive 90mg/L, globular sedimentation velocity 110mm in the first hour, iron 19μg/dL, folic acid 2ng/mL, calcium 8.3mg/dL, phosphorus 2.4mg/dL and albumin 2.2g/dL, whereas the rest of the results in the blood panel, biochemistry, clotting, proteinogram, thyroid hormones, vitamin B12 and anti-nuclear antibodies were normal. Urine analysis was also normal. The microbiological studies, including cultures of urine, blood and bone marrow, and the serology for hepatitis B and C, HIV infection, syphilis and brucellosis, were all negative.
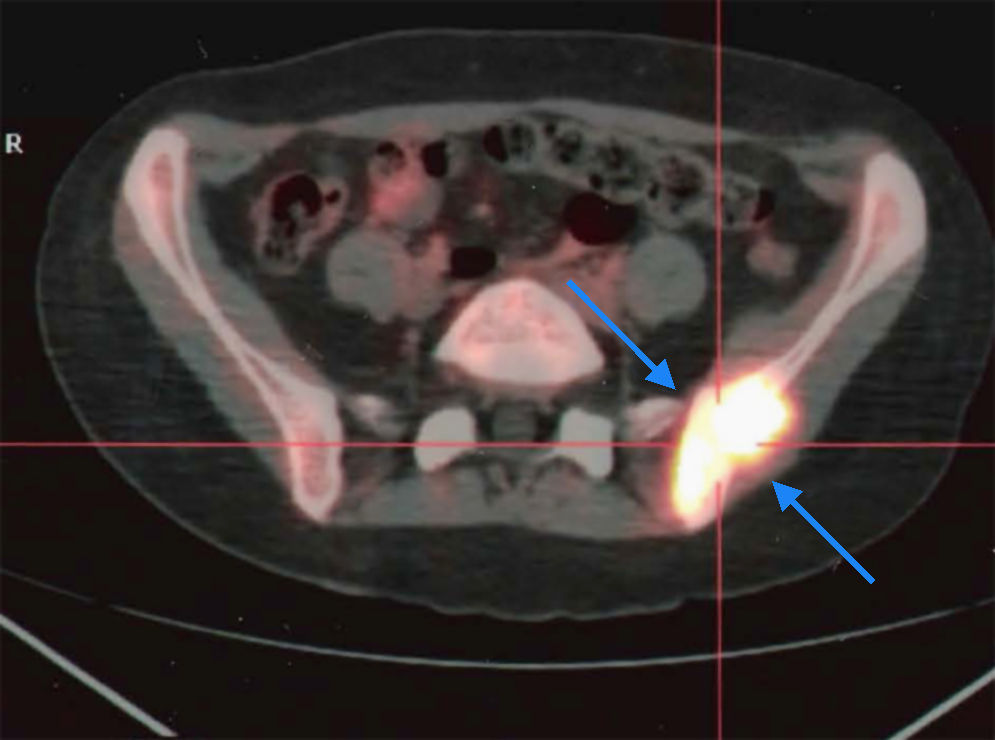
The following complementary tests also gave normal results: chest X-rays, electrocardiogram, abdominal ultrasound, gastroscopy, colonoscopy, echocardiogram and computed tomography of the chest, abdomen and pelvis. A bone marrow aspiration showed polyclonal plasmocytosis. ENT and gynaecological examinations were normal. Finally, a PET/CT scan was performed and showed a hypermetabolic mass in the left iliac bone, left medial gluteal muscle and adjacent parts, measuring 48mm×25mm (Fig. 1). The biopsy of the mass revealed the presence of nests of poorly differentiated round cells separated by fibrovascular septa, typical of alveolar rhabdomyosarcoma.
Throughout the study, the patient remained stable, with persistence of fever and anaemia. No response was seen to empirical antibiotic treatment against a possible inflammatory disease of the pelvis. Several transfusions of haematite concentrate were given.
DiscussionCertain infections, a numerous group of inflammatory diseases and several neoplasias are the main causes of FUO.1,6 In our case, the cause of the FUO finally turned out to be a rhabdomyosarcoma.
Sarcomas are neoplasias originating in various types of connective tissue, such as bone, cartilage, fat, muscle, tendons and blood vessels.7 They constitute a heterogeneous group of tumours, with more than a hundred pathological variants. They can occur at any age. They most frequently present as a tumour that usually grows quickly. They may cause a wide variety of local symptoms, but it is not unusual for them to be painless so they may achieve a large size without being noticed by the patient. It is also quite typical for them to be confused, when they cause pain, with a degenerative pathology, which may entail delays in their detection. Diagnosis of these tumours is by biopsy. Their treatment may require surgery, radiation therapy or chemotherapy, depending on the circumstances. Most sarcomas are quite resistant to conventional chemotherapy but some new drugs, such as gemcitabine or taxanes, are beginning to provide encouraging results.8
With regard to rhabdomyosarcomas, these are highly malignant tumours that usually appear before 20 years of age and may present practically anywhere in the body. They are histologically classified as embryonal, alveolar and pleomorphic. The alveolar type presented by our patient is usually associated with several chromosomal alterations, including translocation t(2;13)(q35;q14), forming a chimeric fusion of fragments of chromosomes 2 and 13.9
Level of evidenceLevel of evidence V.
Protection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the responsible Clinical Research Ethics Committee and in accordance with those of the World Medical Association and the Helsinki Declaration.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Please cite this article as: Roca B, Reinoso I. Fiebre de origen desconocido y anemia como forma de presentación de un rabdomiosarcoma. Rev Esp Cir Ortop Traumatol. 2011; 55(5):382–384.