Many postoperative complications have been described after a total hip arthroplasty, with early and acute, as well as late, complications being reported. Two cases of compartment syndrome of the buttock are described following a hybrid total hip arthroplasty (cemented stem and press-fit and screwed acetabulum) performed on 2 patients of 60 and 68 years old, both diagnosed and treated 24–48h after the surgery. Both cases had a primary prosthesis with no previous significant pathological findings. This condition is still rare, and few cases have been described at the medical literature.
Numerosas complicaciones posquirúrgicas tras la implantación de una artroplastia total de cadera han sido descritas a lo largo de los años, diferenciándose entre las precoces o postoperatorias inmediatas y las tardías. Presentamos 2 casos de síndrome compartimental glúteo como complicación de la implantación de prótesis total híbrida (vástago cementado y cótilo impactado atornillado) en 2 pacientes de 60 y 68 años respectivamente, en los cuales se diagnosticó y trató el proceso a las 24-48h de la cirugía. En ambos casos se trataba de prótesis primarias y ninguno de ellos presentaba antecedentes patológicos de interés, siendo estos casos poco frecuentes y, en consecuencia, con escasas publicaciones en la literatura médica.
Two male patients, aged 60 and 68 years, respectively, were operated of total hip arthroplasty under spinal anesthesia between November and December 2000. Patients 1 and 2 showed no previous history of disease and were not following any medical treatment. Both had a normal weight (patient 1 weighed 76kg and measured 174cm; patient 2 weighed 65kg and measured 169cm). Both cases had right osteoarthritic hips and were implanted a total hybrid prosthesis with cemented stem and impacted acetabulum, with 2 screws in the ileum. Both cases were approached by the Moore posterolateral route, separating the external rotators and dislocating the femoral head by a posterior route. Both patients remained hemodynamically stable during the intervention, with no abrupt changes in their vital signs. Bleeding was considered normal and customary in these interventions (patient 1: 70cc; patient 2: 80cc). We did not observe significant intraoperative or postoperative blood loss and it was not necessary to transfuse any of the 2 patients. This fact is important to rule out the rare intraoperative possibility of injury to the femoral circumflex artery. We placed a subfascial drain in both cases and referred patients to the postoperative control room. Both remained stable during the immediate postoperative period. Drains were scarcely productive (350 and 380cc) and were removed in the first 24h. Both patients followed a postoperative recovery in their corresponding wards, with no incidents or immediate complications, and remaining in bed for the first 12h. Assisted ambulation on crutches with partial load was allowed in the following 12h. Antithrombotic prophylaxis with low molecular weight heparin (dalteparin sodium: 3500IU/24h/subcutaneously) was initiated at 6h of surgery. Postoperative analgesia consisted of paracetamol 1g/8h/intravenously, alternating with metamizole 2g/8h/intravenously, leaving morphine as a rescue therapy.
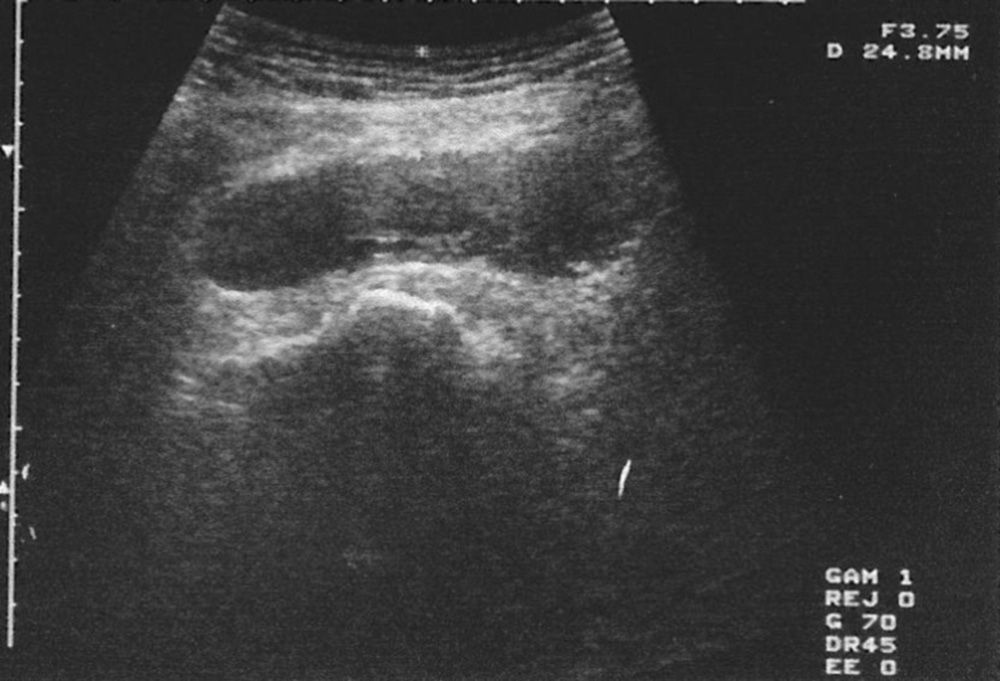
Postoperative radiographs showed a correct implantation and placement of the prosthetic implants, as well as the position of the screws, without protrusion thereof. During the second postoperative day (approximately at 36h), the patients complained of severe pain and swelling in the surgical wound, as well as in the outer part of the thigh, with numbness in the ipsilateral limb to the operated hip. One patient presented inability for foot dorsiflexion. He underwent an urgent electromyogram (EMG) which showed neuropathy by compression of the sciatic nerve. Due to a suspected diagnosis of massive hematoma, both cases underwent ultrasound scans (Fig. 1). Clinically, none of the 2 patients suffered fever syndrome and their constants were normal at the time of study.
As the pain increased abruptly after 3h in parallel to peripheral neuropathy symptoms, the diagnosis of compartment syndrome by hematoma was established, affecting gluteal compartments by tension. Surgical revision was the preferred treatment.
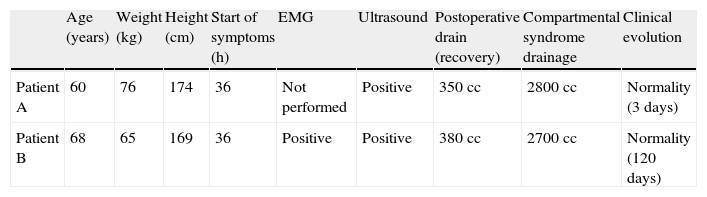
ResultsIn both cases we conducted fasciotomies and drained hematomas of 2.8 and 2.7l, respectively, without finding active bleeding of any relevant vessel (Table 1). The contents were calculated by weighing, after subtracting the weight of the gauzes.
Evolution of the two cases.
| Age (years) | Weight (kg) | Height (cm) | Start of symptoms (h) | EMG | Ultrasound | Postoperative drain (recovery) | Compartmental syndrome drainage | Clinical evolution | |
| Patient A | 60 | 76 | 174 | 36 | Not performed | Positive | 350cc | 2800cc | Normality (3 days) |
| Patient B | 68 | 65 | 169 | 36 | Positive | Positive | 380cc | 2700cc | Normality (120 days) |
Both patients followed a correct postoperative control, dramatically improving their pain and neurological symptoms in the first hours after the end of spinal anesthesia. In one patient, paresthesias persisted until the eleventh week after surgery, albeit decreasing in symptoms and electromyography, and with recovery ad integrum.
We did not use a manometer to measure compartment pressure in any of the 2 patients due to the controversy existing about its usefulness, to a lack of availability and so as not to delay the therapeutic surgical drainage.
These patients have been clinically and radiologically assessed every year and both present scores of 6/6/6 on the Merle d’Aubigné scale at 12 years, with correct radiological adaptation of the implants and with no signs of osteolysis or loosening.
DiscussionCompartment syndrome involves an increase in interstitial pressure in an osteofascial compartment caused by an increase of its contents (hematomas, bleeding, increased capillary permeability) and decrease of the continent (tight bandages or localized external compression),6,7 which produce an increase of tissue pressure which affects microcirculation, causing ischemia mainly in muscles and nerves.
Gluteal compartment syndrome is a rare entity among compartment syndromes, with very few literature references on the subject and in most cases referring to isolated instances. It has been described in association with numerous diseases, especially traumatic (in femoral fractures1 and their treatment with intramedullary nailing, pelvic fractures and soft tissue contusions1,2), spontaneous or posttraumatic lesions of the superior gluteal artery3 and medial femoral circumflex artery,1 in patients with impaired consciousness or prolonged immobilization,3–5 and in connection with intramuscular drug abuse4,5 and rhabdomyolysis6 induced by exercise,3 among others. Although the general causes of bleeding are well known (alcoholism, anticoagulant therapy, liver pathology, etc.), they have not been reflected as direct causes of gluteal compartment syndrome. There are even reports of occurrence in the contralateral gluteal region,6 mainly caused by obesity, prolonged surgical time and lateral decubitus position during surgery, as well as poor positioning of the posterior gluteal support.6 Nevertheless, our patients had no relevant history of disease.
There are several approach routes for the implantation of a total hip arthroplasty, with the posterolateral, anterior and anterolateral being the most common. In the present cases, we used the posterolateral route, as is habitual in our service. While this approach route may have a higher index of iatrogenic sciatic nerve injuries, there are no literature references regarding an increase in bleeding, compared to other routes. There are currently no works mentioning the approach route, the surgical time and the type of anesthesia as risk factors, perhaps because of their extreme rarity.
The gluteal region is broad and consists of 3 compartments,3,7 the gluteus maximus, the gluteus medius/minor, and the fascia lata compartment, all with non-distensible osteofascial limits. Appearance of a compartment syndrome in this region necessarily requires a massive accumulation of edema or blood.
The diagnosis is not simple and involves a high degree of clinical suspicion based on clinical history and detailed physical examination. The most common symptom is intense pain at rest3 and disproportionate with the underlying pathology,8 resistant to analgesic treatment,1,3 worsening with passive stretching of the limb and presenting swelling and ecchymosis1,6,8 in the region (although some cases have been described which had a normal skin appearance5).
Neurological disorders may also appear and manifest as paresthesias and even sciatic nerve paralysis.3,6,8 It is important to highlight that anesthesiological procedures such as nerve blocks, continuous epidural anesthesia and regional anesthesia may hinder clinical assessment.5,6,8 The most common laboratory data7 in this disease are blood loss anemia, metabolic acidosis with hyperkalemia and an increase in creatine kinase count (due to muscular necrosis caused by ischemia) with myoglobinuria.6
The recommended aids for diagnosis in unconscious, multiple trauma patients or when there is doubt about the clinical diagnosis, include arteriography, Doppler ultrasound, computed tomography (CT) and magnetic resonance imaging (MRI) scans. Nevertheless, one of the most widely known and accepted is the measurement of pressures within the compartment. There is some controversy3,4 regarding the threshold for determining the diagnosis, but 2 criteria are generally accepted: absolute compartment pressure (decompression is recommended when this is greater than 30mmHg) and differential pressure (when diastolic arterial pressure minus compartment pressure is less than 30mmHg), although some cases of gluteal compartment syndrome with normal pressures have also been described. The use of EMG may be useful to evaluate sciatic nerve injury during subsequent monitoring.
Nevertheless, we believe that, upon clinical suspicion of this condition, conducting these additional tests should not be a reason to delay treatment through surgical drainage and decompression by fasciotomies, so as to avoid irreversible neurological and muscle lesions. Rapid intervention is vitally important for the survival and viability of the affected tissue. Whitheside et al. reported that the muscle could survive a temporary ischemia for about 4h before histological lesions occurred, whilst neurons only 33min.
Two approach routes to the gluteal region have been described for decompression.8 The route of Henry (in the shape of a question mark starting in the posterior superior iliac spine and descending to the trochanteric region) and the route of Janzing (posterior curved access, similar to the posterior approach route to the hip). However, we used the same surgical route as for the primary surgery. If there is paralysis of the sciatic nerve, then it should be exposed and decompressed.8 It is important to highlight that, even after fasciotomy, the viability of marginal tissue is not resolved immediately, especially in cases with hypotension.
Performing early fasciotomies prevents complications such as myoglobinuria, which can lead to acute renal failure, sepsis, ischemic contractures, amputations and even death.
ConclusionsGluteal compartment syndrome is an infrequent disorder. Orthopedic surgeons should be aware of it and learn how to treat it promptly, as it can lead to severe complications and even death. A conscientious surgical technique regarding dissection and hemostasis, as well as a preoperative study of coagulation, appears essential in order to avoid this rare postoperative complication during total hip arthroplasty.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation adhered to the ethical guidelines of the Committee on Responsible Human Experimentation, as well as the World Medical Association and the Declaration of Helsinki.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Villalba Modol J, Solernou Soler X. Síndrome compartimental glúteo tras el implante de artroplastia total de cadera. A propósito de 2 casos. Rev Esp Cir Ortop Traumatol. 2013;57:296–9.