To compare intracapsular (IC) and extracapsular (EC) hip fractures (HIF) in elderly patients in order to determine if they are different pathologies.
Subjects and methodsLongitudinal, observational, descriptive, analytical prospective design, using a non-probabilistic sample from a full sample collection with 647 subjects (male and female), of 60 or more years old, admitted with HIF to the Department of Orthopedics and Traumatology of the Hospital, between January 1, 2010 and December 31, 2012. Follow-up was for 1 year post HIF. Socio-demographic, etiological, developmental, therapeutic and prognostic variables are compared.
ResultsThis is the first study on this subject with Latin American population. EC HIF incidence was superior to IC, contrary to that published in European/American populations. There are significant differences in etiological variables (χ2=6.34, P<0.042), with traumatic etiology in EC and non-traumatic in IC. There are also differences in therapeutic interventions performed (osteosynthesis for EC, arthroplasty for IC), with the decision on not to operate being lower in IC (both P<0.0000). The variables associated with the decision on not to perform surgery are age, etiology and postoperative mortality.
DiscussionThe results are similar to other studies, adding the IC association with non-traumatic origin, in particular the trend of statistical association between IC and non-primary osteoporotic pathology (neoplasms, renal osteodystrophy, primary hyperparathyroidism). A further analysis was performed on the differences between Latin American and European/American populations in the incidence of either type of HIF. There are important etiological and therapeutic differences between IC and EC HIF; therefore it would be advisable to consider them as distinct disease entities.
Comparar las fracturas de cadera (FC) intra- y extracapsulares (FIC y FEC) en pacientes mayores para determinar si son patologías diferentes.
Sujetos/métodoDiseño prospectivo longitudinal, observacional, descriptivo y analítico. Muestra no probabilística. Muestreo de colección completa. Seiscientos cuarenta y siete sujetos (ambos sexos), 60 o más años, ingresados con FC desde el Servicio de Ortopedia y Traumatología del Hospital (1 de enero de 2010 al 31 de diciembre de 2012). Seguimiento de un año pos-FC. Se comparan variables sociodemográficas, etiológicas, evolutivas, terapéuticas y pronósticas.
ResultadosEs la primera investigación sobre este tema realizada con población latinoamericana. La incidencia de FEC fue superior a FIC, al contrario de lo publicado en población europea/estadounidense. Existen diferencias significativas en las variables etiológicas (χ2=6.34, P<0.042), siendo la etiología traumática en FEC y no traumática en FIC. También hay diferencias en las intervenciones terapéuticas realizadas (osteosíntesis para FEC, artroplastia para FIC); y la decisión de no operar es menor en FIC (ambos P<0.0000). Las variables asociadas con la decisión de no intervención quirúrgica son edad, diagnósticos causales y mortalidad postoperatoria.
DiscusiónLos resultados son similares a otros trabajos, añadiendo la asociación FIC y origen no traumático, especialmente la tendencia de asociación FIC y enfermedad no osteoporótica primaria (neoplasias, osteodistrofia renal, osteoporosis secundaria a hiperparatiroidismo primario). Debemos profundizar en las diferencias entre poblaciones latinoamericana y europea/estadounidense en la incidencia de uno u otro tipo de FC. Existen diferencias importantes, etiológicas y terapéuticas, entre FIC y FEC, por lo que sería conveniente considerarlas como entidades nosológicas distintas.
Hip fractures (HIF) can be considered as a geriatric syndrome, as they are more prevalent after the age of 60 years. Their clinical, social and economic relevance is such that, in the mid-1950s, they gave rise to Orthogeriatrics, the branch of Geriatrics that, along with Traumatology, is in charge of the overall management of elderly patients with pathologies of the locomotor apparatus.1
HIF are by far the most frequent and relevant orthogeriatric disease, with an annual incidence in the USA of 350,000 cases and an economic cost of over 60 million dollars. Demographic projections estimate that the incidence in 2040 will exceed 840,000 cases.2
In addition to traumatology classifications, which seek to facilitate the choice of surgical techniques, HIF can be grouped, according to their anatomical location, into intracapsular (IC) and extracapsular (EC) cases. This anatomical criterion has a physiopathological and therapeutic basis: a critical factor in IC is the terminal vascularization of the femoral head.3 Therefore, a lesion that causes damage to the vessels and increases intracapsular pressure will lead to avascular bone necrosis of the femoral head. Such lesions obtain poor results from orthopedic management, particularly among elderly patients with osteosynthesis. For this reason, particularly when the fracture is displaced and distant from the trochanteric region, arthroplasty is the safest and validated alternative for these patients, offering better results in terms of postoperative functionality, risk of reintervention and complications compared to osteosynthesis.4–6 Osteosynthesis systems could be used in certain IC cases (lower or non-displaced), although further studies would be required in this respect.7,8
On the other hand, EC cases occur in highly vascularized, cancellous bone, with a low risk of malunion or nonunion. Thus, the indication is treatment with reduction-osteosynthesis, and even orthopedic treatment in certain selected cases and conditions.3 The classical literature includes older patients into a more aged group, which suffer difficulty to walk and are more prone to suffering by EC, and a younger group, with no difficulty for movement but suffering from greater osteoporosis and more prone to suffering by IC damage.9 This last feature has raised doubts as to whether these differences between both HIF are significant. Thus, differences have been sought between both pathologies in terms of risk factors, population characteristics, physiopathology, therapeutic methods and final outcomes, both vital and functional. There are very few publications in this respect, all of them conducted on European and US populations.10–17 Although in general significant differences between both kinds of HIF have been reported in terms of several variables, there is currently no overall definition of the topic. Since there are no publications regarding studies conducted on Latin American populations, it is interesting to add new information in this regard, as well as to compare existing data with our own results.
ObjectiveGeneralThe aim is to provide statistical evidence on the diagnoses of IC and EC, which helps to determine whether they are different pathologies or rather different manifestations of the same entity.
SpecificTo compare the independent IC (subcapital, transcervical and basicervical) and EC (pertrochanteric and subtrochanteric) variables of subjects admitted into hospital during the years 2010, 2011 and 2012, with the dependent variables: sociodemographic (gender, age, incidence, comorbidity), etiological (location of occurrence, caused by trauma or not, associated diagnosis indicated as causative), evolutionary (presence of pre- and postoperative complications; period elapsed between surgery and discharge; period elapsed between admission and discharge), therapeutic (type of surgery, decision not to operate, causes of this decision) and prognostic (intrahospital mortality and mortality at 1 year).
Working hypothesisIC and EC fractures are different pathologies. The groups differ significantly in terms of the values of some/all the variable/s used to establish the contrast.
Material and methodsDesignThis study had a longitudinal prospective design, that was observational, descriptive and analytical; it was a single center study. Monitoring of mortality is at 1 year.
SampleThe study sample included a total of 647 patients, both male and female Chileans, aged 60 years and over, who were discharged from the Adult Traumatology and Orthopedic Surgery Service (SOTA) of Hospital Dr. Gustavo Fricke in Viña del Mar, Chile, with a diagnosis of HIF, between January 1st 2010 and December 31st 2012.
SamplingNon-probabilistic sampling of criteria (or full collection) was performed.18 Throughout the studied period, SOTA attended 79% of the HIF in hospital subjects aged 60 or over. All of these subjects were included in the present study.
Description of variablesEtiologyLocation of occurrence (home, public street, place of work, another), type of fracture (ToF: low-energy trauma, high-energy trauma, non-trauma), and diagnosis indicated as causative.
EvolutionQualitative: presence or absence of preoperative (ComPreQ) or postoperative (ComPostQ) complications. Quantitative: total number of pathologies diagnosed upon discharge or death (nPDD); time between admission and discharge (TAD); time between surgery and discharge (TSD).
TreatmentThe treatment was based on type of surgery (ToS), decision not to operate (DNO), and causes of decision not to operate (cDNO).
PrognosisPrognosis was based on intrahospital mortality (IHM) and mortality at 1 year.
Definition of dependent variablesIncidenceWe used the data supplied by the National Statistics Institute for each of the regions covered by the hospital, divided by year and age group.
Diagnosis indicated as causativeWe defined 4 groups: osteoporosis (OP), renal osteodystrophy, neoplasms and massive trauma. In the first one we sought the following causes: protein malnutrition (albuminemia<2.5g%), drugs and other harmful substances that could be used and/or abused (tobacco, alcohol, corticoids, antiepileptic drugs, methotrexate, acenocoumarol, warfarin), primary hyperparathyroidism and other medical conditions (COPD, liver failure, hyperthyroidism, hypothyroidism). Severe hypoalbuminemia (<2.5g%) was considered indicative of the presence of conditions causing a decrease in bone mineral density/secondary osteoporosis.19–21 HIF indicated only as “osteoporotic” were considered to be primary OP.
Total number of pathologies diagnosed upon discharge or deathReferring to the total number of diseases diagnosed upon discharge, death or closure of each case, not counting the diagnosis of HIF.
Presence or absence of preoperative complicationsSet of preoperative situations that influenced the definitive management, thus forcing the following during hospital admission: (a) suspend surgery definitively, (b) postpone/advance the surgery, (c) consultation with another specialty, (d) referral to another service, (e) initiate a laboratory study, and (f) conduct some kind of intervention (on food/diet, drug treatment, social, etc.). Presence/absence was considered as a dichotomous variable and number was considered as an absolute variable.
Postoperative complicationsSet of clinical situations which influenced the postoperative management, leading to the following during hospital admission: (a) extension of hospital admission, (b) referral to another clinical service, (c) consultation with another specialty, (d) request for a study, and (e) conducting some kind of intervention (on food/diet, drug treatment, social, etc.). Presence/absence was considered as a dichotomous variable and number was considered as an absolute variable.
Time from surgery to dischargeDays from surgery to discharge, not counting subjects who were not operated or who died in the hospital following the surgery.
Time from admission to dischargeDays from admission until discharge, counting the day of admission as day 1. Equivalent to the total number of days that each subject was hospitalized for.
Duration of surgeryDescription of the osteosynthesis or prosthetic elements used in HIF surgery: dynamic hip screw (DHS); Gamma nail; dynamic condylar screw (DCS); endomedullary nail; partial hip prosthesis; total hip prosthesis; others.
Decision not to operateDichotomous variable (operated or not operated), excluding deceased subjects.
Causes of decision not to operate- A.
High risk to life: subjects with medical conditions that contraindicated or prevented surgery due to the high risk of death during surgery, as they suffered unrecoverable conditions or were in terminal phase.
- B.
Low/null impact on function or quality of life (independent from the vital prognosis): surgery would not entail a significant functional recovery or the previous functional conditions would not improve with surgery.
- C.
Medical conditions taking a long time to stabilize: subjects suffering unbalanced chronic pathologies or complications that could be balanced but would take a long time to do so, which should be compensated to conduct surgery and that cannot be mitigated or compensated temporarily to favor the surgery.
- D.
Informed decision by patient and/or relatives: only for subjects in whom surgery was indicated and after the decision to operate had been adopted. The patient or groups of people responsible opted for non-surgical management, after being informed by the medical–surgical team of the implications of the decision.
- E.
No surgical indication: with indication of orthopedic management (e.g. consolidated fractures, impacted, with good functionality, etc.).
- F.
Deceased.
- G.
Already operated (at a different healthcare center).
- H.
Others: belonging to another healthcare service, operation must be conducted at a different centers, operation will be carried out by private service, etc.
We used the information contained in the Identification and Civil Registry Service, according to the Unique National Identification of each subject as of January 31st, 2014.
MethodThe data were collected using the same registration template, as subjects were admitted to SOTA. The diagnosis of HIF and description of the anatomical location were conducted by a traumatologist following a clinical analysis and radiographic image study. Radiographs of the pelvis were obtained in PA projection and, in case of doubt, a computed tomography scan of the hip was also obtained. A description of the sample was carried out, comparing each variable for both kinds of HIF and seeking significant differences in 3 levels of analysis:
First level: comparison of frequencies in bivariate tables and mosaic graphs with statistical significance analysis through Pearson residuals, with a maximum level of significance set at P=0.05.
Second level: in the case of categorical qualitative variables a Chi-squared method was applied to differences between more than 2 proportions and the Phi coefficient was calculated to estimate the size of the effect. Values of Phi lower than 0.3 were considered low and values near to or above 0.5 were considered significant. Quantitative variables (parametric) were analyzed with the Student t test, whilst nonparametric variables were analyzed with the Wilcoxon W test, along with calculation of the Cohen d coefficient to estimate the size of the effect. In addition to the work with a full sample, the variable “diagnosis considered as causative” was analyzed with a subsample including only cases due to primary osteoporosis.
Third level: required the adjustment of a binary logistic regression model, taking as criterion variable the presence or absence of intracapsular fracture. The model included not only those variables that presented statistical significance and a high Phi coefficient or d value in previous levels, in order to ensure balance in the model. Qualitative predictors (nominal) were transformed into dichotomous numerical (dummy) variables. The categorical dependent variable was the type of fracture (EC or IC). The model obtained was compared with the null through a Chi-squared analysis, using the difference between residues of both models and with as many degrees of freedom as the number of predictors used.
AnalysisData processing for debugging was carried out using the Calc spreadsheet, from the LibreOffice software suite. Data analysis was conducted in the R programming environment, version 3.1.0 (R Core Team, 2014), along with the software packages Dummies, Psych and Power Analysis.
Weaknesses to considerThe study was conducted at a single center and there was an absence of functional prognosis variables. However, the distribution of the universe in the region studied and the sample selection process afforded the results statistical robustness. Functional prognosis variables were not included because some organizational aspects of the local healthcare system made the clinical follow-up of subjects highly complicated and cumbersome.
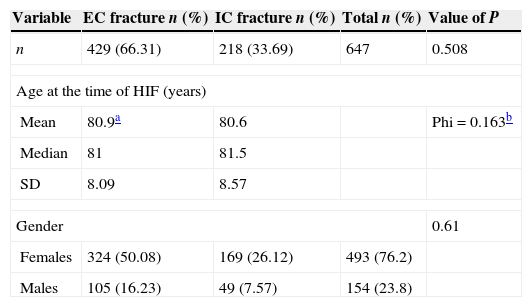
ResultsDescriptiveSociodemographic variablesFemales accounted for 72.2% of the population. The mean age of the sample was 80.8 years, with a standard deviation of 8.25 years. The sample contained 429 (66.31%) EC and 218 (33.69%) IC fractures. During the 3 years of the study, the mean incidence of EC cases was 102.4 per 100,000 subjects aged 60 or over, whereas that of IC cases was 50.5 (Table 1). Both types of fracture increased with age, with incidence peaking around 75–89 years, and gradually decreasing after that age.
Sociodemographic variables.
| Variable | EC fracture n (%) | IC fracture n (%) | Total n (%) | Value of P |
|---|---|---|---|---|
| n | 429 (66.31) | 218 (33.69) | 647 | 0.508 |
| Age at the time of HIF (years) | ||||
| Mean | 80.9a | 80.6 | Phi=0.163b | |
| Median | 81 | 81.5 | ||
| SD | 8.09 | 8.57 | ||
| Gender | 0.61 | |||
| Females | 324 (50.08) | 169 (26.12) | 493 (76.2) | |
| Males | 105 (16.23) | 49 (7.57) | 154 (23.8) | |
EC: extracapsular fracture; HIF: hip fracture; IC: intracapsular fracture; SD: standard deviation.
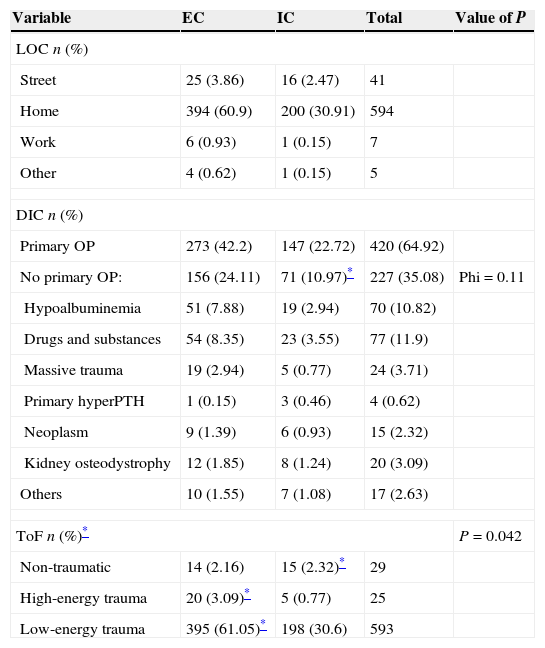
Both HIF occurred primarily at home (91.81%), followed by the street (6.34%) and workplace (1.08%). Up to 91.65% of cases were associated to low-energy trauma and 3.86% to high-energy trauma, mainly falls from a height and traffic accidents. Absence of trauma was documented in 4.48% of cases. The main pathology considered as etiological was primary osteoporosis (64.91%), followed by bone damage associated to drug or substance abuse (11.9%), severe hypoalbuminemia (10.82%) and massive trauma (3.71%). The total number of subjects with hypoalbuminemia was 69.71% (n=451). Kidney osteodystrophy was present in 3.09% of the sample, neoplasms in 2.32%, and primary hyperparathyroidism in 0.62% (Table 2).
Etiological variables.
| Variable | EC | IC | Total | Value of P |
|---|---|---|---|---|
| LOC n (%) | ||||
| Street | 25 (3.86) | 16 (2.47) | 41 | |
| Home | 394 (60.9) | 200 (30.91) | 594 | |
| Work | 6 (0.93) | 1 (0.15) | 7 | |
| Other | 4 (0.62) | 1 (0.15) | 5 | |
| DIC n (%) | ||||
| Primary OP | 273 (42.2) | 147 (22.72) | 420 (64.92) | |
| No primary OP: | 156 (24.11) | 71 (10.97)* | 227 (35.08) | Phi=0.11 |
| Hypoalbuminemia | 51 (7.88) | 19 (2.94) | 70 (10.82) | |
| Drugs and substances | 54 (8.35) | 23 (3.55) | 77 (11.9) | |
| Massive trauma | 19 (2.94) | 5 (0.77) | 24 (3.71) | |
| Primary hyperPTH | 1 (0.15) | 3 (0.46) | 4 (0.62) | |
| Neoplasm | 9 (1.39) | 6 (0.93) | 15 (2.32) | |
| Kidney osteodystrophy | 12 (1.85) | 8 (1.24) | 20 (3.09) | |
| Others | 10 (1.55) | 7 (1.08) | 17 (2.63) | |
| ToF n (%)* | P=0.042 | |||
| Non-traumatic | 14 (2.16) | 15 (2.32)* | 29 | |
| High-energy trauma | 20 (3.09)* | 5 (0.77) | 25 | |
| Low-energy trauma | 395 (61.05)* | 198 (30.6) | 593 | |
DIC: diagnosis indicated as causative; EC: extracapsular; Hyper-PTH: hyperparathyroidism; IC: intracapsular; LOC: location where the fracture took place; OP: osteoporosis; ToF: type of fracture.
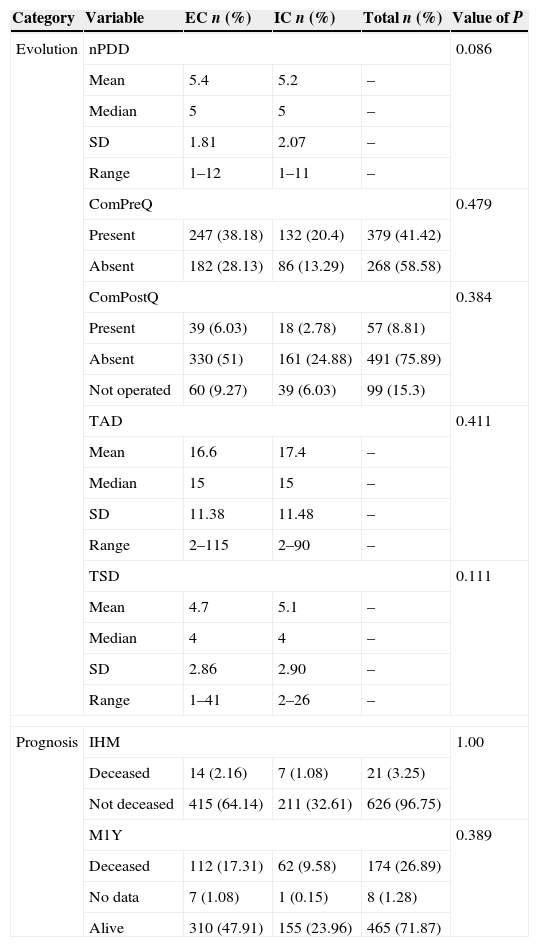
Mean nPDD was 5.4 for EC and 5.2 for IC, (maximum of 12 pathologies). ComPreQ occurred in 58.58% of cases and ComPostQ in 8.81%. The mean duration of hospital stay was 16.6 days for EC and 17.4 for IC. The mean period that elapsed between surgery and discharge was 4.7 days for EC and 5.1 days for IC (Table 3).
Evolution and prognosis variables.
| Category | Variable | EC n (%) | IC n (%) | Total n (%) | Value of P |
|---|---|---|---|---|---|
| Evolution | nPDD | 0.086 | |||
| Mean | 5.4 | 5.2 | – | ||
| Median | 5 | 5 | – | ||
| SD | 1.81 | 2.07 | – | ||
| Range | 1–12 | 1–11 | – | ||
| ComPreQ | 0.479 | ||||
| Present | 247 (38.18) | 132 (20.4) | 379 (41.42) | ||
| Absent | 182 (28.13) | 86 (13.29) | 268 (58.58) | ||
| ComPostQ | 0.384 | ||||
| Present | 39 (6.03) | 18 (2.78) | 57 (8.81) | ||
| Absent | 330 (51) | 161 (24.88) | 491 (75.89) | ||
| Not operated | 60 (9.27) | 39 (6.03) | 99 (15.3) | ||
| TAD | 0.411 | ||||
| Mean | 16.6 | 17.4 | – | ||
| Median | 15 | 15 | – | ||
| SD | 11.38 | 11.48 | – | ||
| Range | 2–115 | 2–90 | – | ||
| TSD | 0.111 | ||||
| Mean | 4.7 | 5.1 | – | ||
| Median | 4 | 4 | – | ||
| SD | 2.86 | 2.90 | – | ||
| Range | 1–41 | 2–26 | – | ||
| Prognosis | IHM | 1.00 | |||
| Deceased | 14 (2.16) | 7 (1.08) | 21 (3.25) | ||
| Not deceased | 415 (64.14) | 211 (32.61) | 626 (96.75) | ||
| M1Y | 0.389 | ||||
| Deceased | 112 (17.31) | 62 (9.58) | 174 (26.89) | ||
| No data | 7 (1.08) | 1 (0.15) | 8 (1.28) | ||
| Alive | 310 (47.91) | 155 (23.96) | 465 (71.87) | ||
ComPostQ: postoperative complications; ComPreQ: preoperative complications; IHM: intrahospital mortality; M1Y: mortality at 1 year; nPDD: number of pathologies diagnosed at discharge; SD: standard deviation; TAD: time from admission to discharge; TSD: time from surgery to discharge.
Preoperative IHM was 16 subjects (2.47%), 13 with EC fractures. EC cases accounted for 3.03% and IC for 1.38%. Postoperative IHM was 0.78%. Total IHM was 21 subjects (3.25%). Mortality at 1 year after the occurrence of HIF was 26.89% (Table 3).
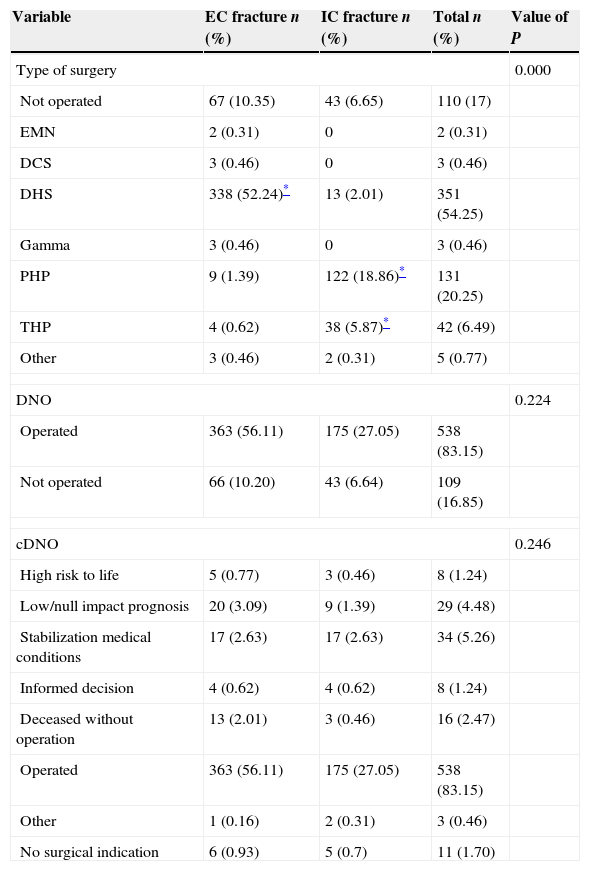
Treatment variablesOut of the total HIF cases, 83.31% were managed surgically. DNO (16.69%) had two main causes: unbalanced medical conditions with scarce probability of balance in the short term (5.26%) and low/null functional impact of surgery (4.48%). Orthopedic management was indicated in up to 1.7%. The main materials used in surgery were DHS and PHP (Table 4).
Therapeutic variables.
| Variable | EC fracture n (%) | IC fracture n (%) | Total n (%) | Value of P |
|---|---|---|---|---|
| Type of surgery | 0.000 | |||
| Not operated | 67 (10.35) | 43 (6.65) | 110 (17) | |
| EMN | 2 (0.31) | 0 | 2 (0.31) | |
| DCS | 3 (0.46) | 0 | 3 (0.46) | |
| DHS | 338 (52.24)* | 13 (2.01) | 351 (54.25) | |
| Gamma | 3 (0.46) | 0 | 3 (0.46) | |
| PHP | 9 (1.39) | 122 (18.86)* | 131 (20.25) | |
| THP | 4 (0.62) | 38 (5.87)* | 42 (6.49) | |
| Other | 3 (0.46) | 2 (0.31) | 5 (0.77) | |
| DNO | 0.224 | |||
| Operated | 363 (56.11) | 175 (27.05) | 538 (83.15) | |
| Not operated | 66 (10.20) | 43 (6.64) | 109 (16.85) | |
| cDNO | 0.246 | |||
| High risk to life | 5 (0.77) | 3 (0.46) | 8 (1.24) | |
| Low/null impact prognosis | 20 (3.09) | 9 (1.39) | 29 (4.48) | |
| Stabilization medical conditions | 17 (2.63) | 17 (2.63) | 34 (5.26) | |
| Informed decision | 4 (0.62) | 4 (0.62) | 8 (1.24) | |
| Deceased without operation | 13 (2.01) | 3 (0.46) | 16 (2.47) | |
| Operated | 363 (56.11) | 175 (27.05) | 538 (83.15) | |
| Other | 1 (0.16) | 2 (0.31) | 3 (0.46) | |
| No surgical indication | 6 (0.93) | 5 (0.7) | 11 (1.70) | |
cDNO: cause of decision not to operate; DCS: dynamic condylar screw, DHS: dynamic hip screw; DNO: decision not to operate; EC: extracapsular; EMN: endomedullary nail; IC: intracapsular; PHP: partial hip prosthesis; THP: total hip prosthesis.
There was no correlation with gender (P=0.61), age (P=0.508) and incidence (P=0.524) (Table 1).
Etiology variablesThere was no correlation with the location of the event (P=0.696) or the diagnosis considered as causative (P=0.412).
Regarding a traumatic origin or lack thereof, there was evidence of a potential association which, though not significant (P=0.079), suggested that the absence of trauma was more common among IC cases, whereas its presence (both high and low energy) was more common among EC cases (Table 2).
Evolution variablesQualitative: there were no differences between both HIF in terms of preoperative (P=0.479) or postoperative (P=0.384) complications.
Quantitative: nPDD: there were no differences between both HIF. TAD and TSD: the mean TAD and TSD were higher among IC cases, and associated to more total days of hospital admission and more postoperative days. However, the median values revealed that these differences were not significant.
Prognosis variablesBoth HIF were independent in terms of intrahospital mortality (P=1) and mortality after 1 year of the incidence of HIF (P=0.389).
Treatment variablesThere was no relationship in terms of the number of HIF operated and not operated (P=0.224) or in terms of the reason given not to operate (P=0.246). Significant differences were found in the type of surgery (P=0.000) (Table 4). IC fractures were associated to arthroplasty (total and partial hip prostheses), whereas EC fractures were associated to osteosynthesis (mainly with DHS), (Table 4).
Analysis of difference of proportionsQualitative variables- a.
Chi-squared: there were two variables with significant differences between both HIF: type of fracture (ToF) and type of surgery (ToS). Regarding the type of fracture, EC were associated with low- and high-energy trauma, whereas IC were associated with absence of trauma (Ji2=6.34, P<0.042). Regarding type of surgery, EC were more associated to the treatment with DHS, whereas IC cases were more associated to partial and total prostheses (Ji2=414.65, P=0.000).
- b.
Size of the effect: when considering Phi, the variable type of surgery once again showed a strong and real difference. In addition, another two results forced us to consider new studies about these relationships: diagnosis indicated as causative (Table 2) and causes of the decision not to operate (Table 4).
The results did not vary significantly with respect to the general sample. However, it is worth highlighting the association with age (EC were related to higher ages) and causes of DNO (IC were related to a higher risk of mortality and informed decision). Therefore, even though Chi-squared was not significant, the size of the effect – despite presenting a moderate/low level – could indicate that they do play a role and should be studied in further detail in new studies (Table 1).
Quantitative variablesStudent t: in the case of TSD, with a P>0.05 it was not possible to reject the null hypothesis of equality between both groups. The same occurred with TAD (P=0.411).
Wilcoxon W: nPDD did not fulfill the contrast to determine homoscedasticity (conducted with the Bartlett test for homogeneity of variance), thus requiring a nonparametric approximation with a Wilcoxon W. The value of P>0.05 (W=50.564, P=0.086) did not allow us to reject the null hypothesis in the case of nPDD.
Size of the effect: we calculated the size of the effect with Cohen d for both types of quantitative variable (values of 0.2 were considered low, 0.5 medium and over 0.8 high). The values obtained were low, so we could not expect to obtain significant results for the possible differences.
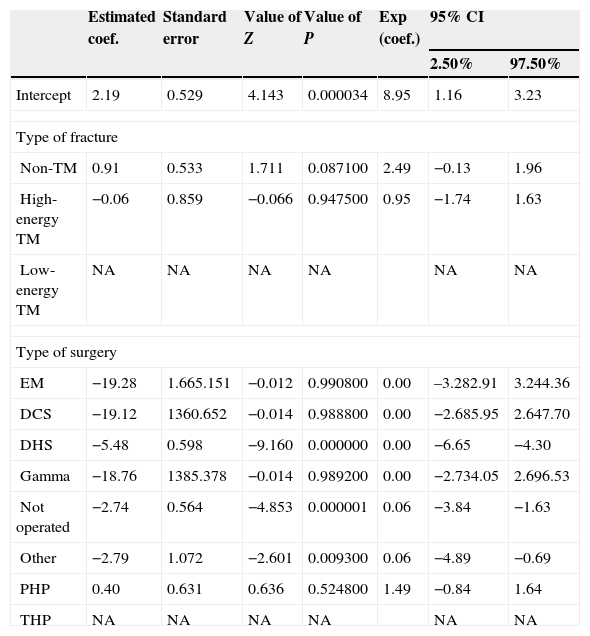
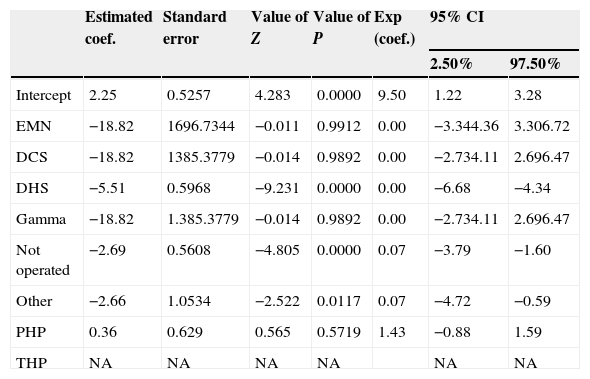
Determination of the predictive model through logistic regressionResultsAfter applying the regression model we obtained a first result on coefficients and their significance (Table 5). In the case of the variable type of fracture, no value was significant. In type of surgery, DHS, other and not operated had a P<0.05. The reason why the last categories of each variable appeared without estimation was because they presented singularity, therefore offering redundant information that did not add to the estimations of the coefficients. The result led us to focus the interpretation only on the variable type of surgery and its dummies. Preliminarily, we could point out that these dichotomous variables contributed significantly to explain the behavior of the dependent variable. Therefore, only the variable type of surgery contributed to determine the type of fracture that could appear (intra- or extracapsular). We repeated the analysis considering only this variable (Table 6), obtaining the same significant coefficients. The advantage of the event “intracapsular fracture” decreased by nearly 100%. In other words, against the presence of DHS the probability of not suffering an intracapsular fracture was nearly 100%. A similar situation occurred in the presence of not operated or another and in both cases, with a decrease of 93% in the advantage of the event “intracapsular fracture”; we established that in the presence of these values of the independent variable an intracapsular fracture was less likely. Specifically, it seemed that when a patient was operated with DHS, with another material (not endomedullary nail, dynamic condylar screw or Gamma nail) or not operated, then an intracapsular fracture was less likely.
Significance of the estimated coefficients and confidence intervals in the logistic regression model.
| Estimated coef. | Standard error | Value of Z | Value of P | Exp (coef.) | 95% CI | ||
|---|---|---|---|---|---|---|---|
| 2.50% | 97.50% | ||||||
| Intercept | 2.19 | 0.529 | 4.143 | 0.000034 | 8.95 | 1.16 | 3.23 |
| Type of fracture | |||||||
| Non-TM | 0.91 | 0.533 | 1.711 | 0.087100 | 2.49 | −0.13 | 1.96 |
| High-energy TM | −0.06 | 0.859 | −0.066 | 0.947500 | 0.95 | −1.74 | 1.63 |
| Low-energy TM | NA | NA | NA | NA | NA | NA | |
| Type of surgery | |||||||
| EM | −19.28 | 1.665.151 | −0.012 | 0.990800 | 0.00 | –3.282.91 | 3.244.36 |
| DCS | −19.12 | 1360.652 | −0.014 | 0.988800 | 0.00 | −2.685.95 | 2.647.70 |
| DHS | −5.48 | 0.598 | −9.160 | 0.000000 | 0.00 | −6.65 | −4.30 |
| Gamma | −18.76 | 1385.378 | −0.014 | 0.989200 | 0.00 | −2.734.05 | 2.696.53 |
| Not operated | −2.74 | 0.564 | −4.853 | 0.000001 | 0.06 | −3.84 | −1.63 |
| Other | −2.79 | 1.072 | −2.601 | 0.009300 | 0.06 | −4.89 | −0.69 |
| PHP | 0.40 | 0.631 | 0.636 | 0.524800 | 1.49 | −0.84 | 1.64 |
| THP | NA | NA | NA | NA | NA | NA | |
CI: confidence interval; DCS: dynamic condylar screw; DHS: dynamic hip screw; EM: endomedullary nail; Estimated coef.: non-standardized estimated coefficient; Exp (coef.): exponentiation of the coefficient; NA: not applicable (singularity); Non-TM: non-trauma; PHP: partial hip prosthesis; THP: total hip prosthesis; TM: trauma.
Significance of the estimated coefficients and confidence intervals for type of surgery dummies.
| Estimated coef. | Standard error | Value of Z | Value of P | Exp (coef.) | 95% CI | ||
|---|---|---|---|---|---|---|---|
| 2.50% | 97.50% | ||||||
| Intercept | 2.25 | 0.5257 | 4.283 | 0.0000 | 9.50 | 1.22 | 3.28 |
| EMN | −18.82 | 1696.7344 | −0.011 | 0.9912 | 0.00 | −3.344.36 | 3.306.72 |
| DCS | −18.82 | 1385.3779 | −0.014 | 0.9892 | 0.00 | −2.734.11 | 2.696.47 |
| DHS | −5.51 | 0.5968 | −9.231 | 0.0000 | 0.00 | −6.68 | −4.34 |
| Gamma | −18.82 | 1.385.3779 | −0.014 | 0.9892 | 0.00 | −2.734.11 | 2.696.47 |
| Not operated | −2.69 | 0.5608 | −4.805 | 0.0000 | 0.07 | −3.79 | −1.60 |
| Other | −2.66 | 1.0534 | −2.522 | 0.0117 | 0.07 | −4.72 | −0.59 |
| PHP | 0.36 | 0.629 | 0.565 | 0.5719 | 1.43 | −0.88 | 1.59 |
| THP | NA | NA | NA | NA | NA | NA | |
CI: confidence interval; DCS: dynamic condylar screw; DHS: dynamic hip screw; EMN: endomedullary nail; Estimated Coef.: non-standardized estimated coefficient; Exp (coef.): exponentiation of the coefficient; NA: not applicable (singularity); PHP: partial hip prosthesis; THP: total hip prosthesis.
When applying the test we obtained the general adjustment, which was statistically significant (χ2gl=9=472.67, P<0.0000), thus allowing us to determine that the proposed model was significantly better adjusted than the null.
DiscussionWe found 8 original works related to this topic published between 1992 and 2010. No works published after 2010 were found,10–17 and samples were between 170 and 2150 subjects. All indicated significant differences between EC and IC fractures, although not always in relation to the same variables or types of variable. None indicated an absence of differences. All the works published were conducted on samples of European or US populations. No works which used a Latin American population were found, thus the present study would be the first to be carried out with this kind of population. Another relevant difference between the literature and the present work lies in the EC/IC ratio: the literature usually favors IC or is very close to 50% for each type. Only the work by Karagiannis, conducted on a Greek population in 2006, reported a higher percentage of EC than IC, and in the same proportion as the present results. This would enable us to consider the existence of genetic and nutritional variables that could influence the incidence of both fractures.
Epidemiological variables: only Tanner10 indicated significant differences between both genders related to age of presentation of EC, higher among females and lower among males. The main difference in terms of age was independent of gender, since Tanner,10 Fox,11 Kesmezacar,12 Karagiannis14 and Parker16 all indicated that EC cases appeared in population groups with higher ages than those suffering IC fracture. This was not confirmed in the present study. However, a trend toward association of EC with higher ages could be observed when taking into account only those subjects with HIF attributable to primary osteoporosis. This result was consistent with the symptoms and the differences in etiology observed, since the damage produced by OP was directly proportional to the time of exposure of the bone to the disease and, in order to take place, EC fractures would generally require the concurrence of a trauma, which would reveal the bone weakness secondary to OP. This would be in contrast to the situation in IC, which was significantly more common without trauma and associated to different diseases, other than OP.
Etiology variables: we could suppose that if there were any differences related to age and prior level of functionality between both HIF, this could translate into differences related to the location of presentation of the fracture, so that those subjects with the best functionality/lowest age would be more prone to suffer fractures in places other than their home. This was not the case in our study or in the literature consulted. However, the association between EC cases and a traumatic origin was significant, thus confirming the report by Fox in 1999.17 Cases of IC fractures in the present study were also significantly associated with a cause other than trauma. The latter observation would be consistent with the difference observed between both types of HIF in relation to the variable “diagnosis indicated as causative”, where IC cases showed a trend toward association with pathologies other than primary osteoporosis, mainly kidney osteodystrophy, primary hyperparathyroidism and neoplastic disease. This should be confirmed with larger samples. If confirmed, prevention of HIF by acting on bone mineral density would have an impact mainly on the incidence of EC cases. This would lead to a revision of the results of prevention programs, differentiating cases according to the incidences of EC and IC.
Evolution variables: comorbidity was significantly different in the studies conducted by Parker16 and Fox.17 However, the first indicated higher comorbidity in IC fractures, whilst the second indicated less. Our own comorbidity variable (nPDD) did not show any differences. However, this variable entails some significant difficulties, since it is highly dependent on the data collection process, difficult to standardize and loses value in retrospective studies. It was easier to measure the onset of complications, in which neither the present study nor the literature found differences. Intrahospital times were not significant in this study. However, the trend pointed toward longer total and postoperative times in the case of IC fractures. The literature was not clear in this respect. While Parker16 indicated longer hospital stays in the case of EC fractures, Karagiannis14 and Fox17 reported that IC fractures led to longer stays. Although this variable was “objective”, it also reflected a set of situations separate from the inherent nature of the pathology, including administrative, organizational and budgetary factors that varied according to each center. This could explain the inconsistency of the results observed by different studies.
Prognosis variables: Karagiannis14 and Haentjens15 reported differences in mortality, higher for EC in both cases. However, this would vary according to years of follow-up, since, except for Haentjens, intrahospital and 1-year mortalities did not show differences in any of the works, and the only one which conducted a follow-up of this variable beyond 1 year was Karagiannis, who observed differences after 5 years of follow-up. Our work included monitoring for up to 1 year after the fracture, and no differences were found. Based on the findings of Karagiannis,14 a longer follow-up period becomes a factor to be investigated for this variable.
Treatment variables: all the studies agreed with the results of this investigation: there are notable differences in terms of the surgical procedure of choice according to the type of HIF, specifically arthroplasty for IC and reduction and osteosynthesis for EC. This also had etiological, therapeutic and prognostic value. This was etiological because the physiopathology and anatomical disposition of the vascularization of the femoral head are the bases to select arthroplasty in IC, therapeutic because the postoperative management will be different and prognostic because the functional results will also be different. This work also found significant differences in this variable. Only Parker16 indicated differences in relation to the decision not to operate, reporting that EC fractures were operated less often. This was confirmed by the present study through a logistic regression model: the decision not to operate was more likely to take place in EC cases. It is not clear why, although the trend observed in EC to occur at more advanced ages could be related to a reduced impact of surgery on functionality and quality of life. We also found a trend, which should be studied further, related to the causes that led to select non-surgical treatment in each type of HIF. According to this, when IC cases were not operated it was due to the fact that relatives and/or patients preferred non-surgical management and/or due to a high risk of short-term mortality. This was consistent with the finding of a diagnostic trend discussed previously which associated IC with potentially fatal diagnoses. A larger sample size would be required to analyze these trends more accurately.
Conclusions and proposals of the workAs conclusions, we could say that there are significant differences between IC and EC fractures in terms of etiological variables (traumatic origin for EC, non-traumatic for IC), as well as therapeutic variables (type of surgery, decision not to operate). There are also trends pointing toward a relationship with epidemiological (age), etiological (diagnoses indicated as causative), prognostic (mortality) and therapeutic (causes of decision not to operate) variables. These were consistent with the significant differences found in this study and in others, consistent among each other and with the clinical presentation of HIF in elderly patients. The trends should be studied with larger samples, preferably in various centers and with the longest possible follow-up periods. Likewise, this research team suggests incorporating pathological anatomy techniques in the study of etiological variables, given the relevance of OP in the genesis of both kinds of HIF. Another point of interest to investigate are the differences between Latin American and European/US populations in terms of presentation of HIF. Lastly, we consider it epidemiologically relevant to regard these fractures as two different nosological entities, even though there still remain some questions to be answered.
Level of evidenceLevel of evidence I.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Dinamarca-Montecinos J, Prados-Olleta N, Rubio-Herrera R, Castellón-Sánchez del Pino A, Carrasco-Buvinic A. Fracturas de cadera intra- y extracapsulares en mayores: ¿dos enfermedades distintas?. Rev Esp Cir Ortop Traumatol. 2015:59:227–237.
This work is part of the publications required to qualify for the title of Doctor in Medicine and Surgery (Gerontology) by the University of Granada.