Isolated arthroscopic subacromial decompression (IASD) is a widely used surgical procedure with high success rates. However, up to 25% of patients experience residual pain. It is unclear whether aberrant central nervous system processing of pain as described in fibromyalgia (FM) could have a detrimental effect on outcomes.
To test this hypothesis, the authors conducted a retrospective case–control study of patients undergoing IASD.
Material and methodsBetween 2008 and 2015, 26 patients with preoperative diagnosis of fibromyalgia and an IASD procedure were identified. Six patients were lost to follow-up. Each fibromyalgia patient was matched with one control patient (n=20) recruited from the remainder with IASD. Outcomes were assessed by DASH score (Disability Arm Shoulder and Hand), Constant (CS), relative Constant score (rCS) and Visual Analogue Scale (VAS). Patient satisfaction was determined with a single 2-level question. Failure of the IASD was defined as persistent pain (VAS>3) at last follow-up.
ResultsThe average age of the sample was FM/Control group 51/48, with a mean follow-up of 36/42 months respectively. Both groups exhibited significant clinical improvement in the pain VAS, DASH and rCS at final follow-up (p<001) compared with the preoperative scores.
Mean postoperative scores FM/Control group were: Constant 63.5/74 (p=.07), rCS 82/88 (p=18), DASH 38.9/20.7 (p=009), VAS 3.8/2.8 (p=2). Eighty-five percent of patients in the control group were satisfied with the surgery compared with 55% in the FM group (p=03). Failure of the procedure was 60% in the FM group, and 30% in the control group (p=.056).
ConclusionsFibromyalgia can be considered a prognostic factor of a poor postoperative outcome after an IASD. However the clinical improvement experienced by these patients over their preoperative situation leads us to recommend their surgical treatment when indicated.
La descompresión subacromial artroscópica aislada (DSA) es un procedimiento quirúrgico ampliamente utilizado que presenta un elevado porcentaje de éxito. Sin embargo, hasta un 25% de los pacientes puede presentar dolor residual tras la intervención. No está claro si el procesamiento aberrante del dolor, como ocurre en la fibromialgia (FM), podría ejercer un efecto deletéreo en los resultados obtenidos. Para testar esta hipótesis hemos realizado un estudio casos-controles retrospectivo de los pacientes en los que se ha realizado una descompresión subacromial artroscópica como procedimiento quirúrgico único.
Material y métodosSe seleccionaron 26 pacientes con diagnóstico preoperatorio de fibromialgia de una serie de 293 pacientes intervenidos mediante DSA entre 2008-2015. Seis pacientes se perdieron durante el seguimiento. Cada paciente con diagnóstico de fibromialgia fue emparejado con un control (n=20). Los resultados fueron evaluados mediante la escala DASH, Constant, Constant relativo a la edad y sexo (rCS) y la escala visual analógica (EVA). La satisfacción del paciente fue evaluada con una pregunta dicotómica. Se consideró fracaso del procedimiento la presencia de una puntuación superior a 3 en la EVA en el último seguimiento.
ResultadosLa media de edad de los grupos FM/control fue de 51/48 años, con un seguimiento medio de 36/42 meses respectivamente. Ambos grupos experimentaron una mejoría postoperatoria significativa en las escalas de EVA, DASH y rCS (p<0,001) en comparación con los valores preoperatorios. Los valores medios postoperatorios FM/control fueron Constant 63,5/74 (p=0,07), rCS 82/88 (p=0,18), DASH 38,9/20,7 (p=0,009), EVA 3,8/2,8 (p=0,2). El 85% de los pacientes del grupo control manifestaron estar satisfechos con los resultados de la cirugía frente al 55% del grupo FM (p=0,03). La tasa de fracasos en el grupo FM fue del 60% frente al 30% en el grupo control (p=0,056).
ConclusionesLa fibromialgia puede ser considerada como factor pronóstico que condiciona un peor resultado postoperatorio tras DSA. Sin embargo, debido a la mejoría clínica que experimentan estos pacientes frente a su estado preoperatorio, recomendamos realizar este tratamiento quirúrgico cuando exista indicación.
Subacromial pain syndrome is a common cause of anterior shoulder pain. Surgical treatment is reserved solely for those cases that do not respond to conservative treatment, which has a success rate of 77–90%.1,2 However, up to 25% of these patients experience residual pain following surgery, which can call into question the overall effectiveness of the procedure. Several studies have been carried out in an attempt to determine the causes for arthroscopic acromioplasty failure,4 and most associate the poor outcome to technical failures or incorrect indication for the surgery. There are no studies that assess whether or not the patient's preoperative characteristics may play a role in the postoperative result or in the identification of those patients who might be prone to having a worse postoperative outcome. Fibromyalgia is an illness that associates aberrant pain processing,5,6 which can influence the result of the surgery.
The study hypothesis is that aberrant pain processing, as fibromyalgia patients suffer, might negatively affect the postoperative results achieved after performing a subacromial decompression (SAD) as a separate procedure. The objective of the study is to ascertain if the preoperative diagnosis of fibromyalgia can have negative effects on surgical outcomes.
Material and methodsThis study was approved by the hospital's ethic committee (protocol code CI 17/024-43 E_TFG). Patients gave their consent in writing to participate in the study; said consent was drafted as per the Helsinki charter.
A retrospective case–control study was carried out. Using the institutional computer registry, 293 subjects between 2008 and 2015 were identified who had been treated with SAD as a single procedure. Those in who an operation was performed associated to the arthroscopic subacromial decompression were excluded: acromioclavicular resection, any procedure performed on the long portion of the biceps, labrum repair, rotator interval or suture of the rotator cuff tendons. Individuals who had suffered recent trauma, previous surgery on the shoulder affected, and those who were over the age of 65 years (due to the possibility of presenting degenerative joint changes that could create artefacts in the result) were likewise excluded.
Of the 293 patients, 26 had a preoperative diagnosis of fibromyalgia established by a Rheumatologist on the basis of the 2010 criteria of the American College of Rheumatology Classification Criteria for Fibromyalgia.7,8 Of the 26 patients previously mentioned, 6 were excluded due to lack of follow-up. Twenty patients were included in the final study. For each patient diagnosed with fibromyalgia a control patient was chosen without a diagnosis of FM and having a similar demographic profile.
All the participants exhibited preoperative clinical signs of subacromial syndrome with anterior pain on abduction and positive Neer and Hawkins tests,9,10 and were treated conservatively with rehabilitation for at least 4 months with no improvement. The preoperative radiographic study includes X-rays of the shoulder involved in 2 projections (anteroposterior and axillary) and an NMR.
Surgical techniqueAll of the surgeries were performed by one of the 3 senior authors following the hospital's standard protocol and instrumentation. Following general anaesthesia and ultrasound-guided inter-scalene block, the patient was placed in the lateral decubitus position with traction of the upper limb involved. By means of a posterior portal, an anterior portal in the rotator interval, and a third lateral portal, the joint and the subacromial space were examined. Subsequently, a bursectomy was performed, the coracoacromial ligament was released, and the anteroinferior acromioplasty was drilled using a motorised burr. The patients were discharged on the same day as the surgery and initiated pendular movements immediately, beginning rehabilitation at 3 weeks following surgery.
Postoperative measurementsPreoperatively, the patients were evaluated by means of the Visual Analogue Scale (VAS), the Disability Arm Shoulder and Hand scale (DASH)11 and the Constant scale (CS).12 Given the difference in parameters such as joint range of motion and strength on the basis of age and gender, the relative CS (rCS) was also administered.13 The mean follow-up was 36.8 months (23–84 months). Patients were evaluated and interviewed face-to-face at the hospital by 2 independent examiners, blind to the cohort, and who had not participated in any of the surgeries. The same protocol was used as in the preoperative assessment (VAS, DASH, CS, rCS, and measurement of joint range of motion). Strength was quantified by means of a digital dynamometer (Lafayette Manual Muscle Testing System, Lafayette Instrument Co, Lafayette, IN, USA) as the mean of 3 recordings. The joint range of motion (antepulsion, abduction, internal rotation, and external rotation) was quantified using a goniometer. The control group was evaluated by a Rheumatologist to assure the absence of criteria of fibromyalgia. The surgical procedure was considered to have failed when the person indicated a score of more than 3 on the VAS.2 The yes/no question, “Are you satisfied with the result of the surgery?” was asked to appraise patient satisfaction. Likewise, the success or failure of the surgery as per the CS was determined with a combination of the rCS and the need for revision surgery, as reported by Jaeger14; a satisfactory result was established as a 70% on the rCS without the need for revision surgery in the first 24 months following the surgery.
Statistical analysisTo determine the sample size, a prior analysis was carried out, establishing an alpha error of 0.5. With the previously-mentioned data,15 a sample size of 18 patients was deemed necessary to detect a minimum change of 17 points on the CS, assuming a standard deviation of 15 and a 10% loss.
Non-parametric tests were used to compare continuous variables between groups (Student's t for matched samples, U-Mann–Whitney). A difference with a p value of less than .05 was considered statistically significant. The statistical analysis was conducted using the IBM SPSS Statistics Software, version 22.0 (SPSS Inc., Chicago, Illinois).
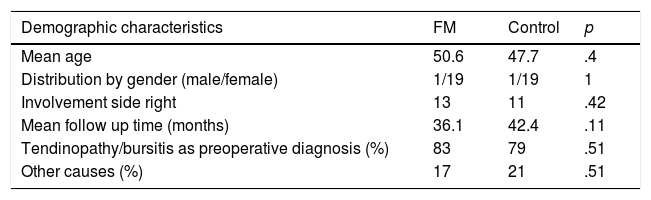
ResultsEpidemiological resultsAn isolated arthroscopic subacromial decompression (IASD) was performed on 293 patients; 78% (229 patients) were female and 26 (8.8%) were diagnosed with FM. The mean age of patients with fibromyalgia included in the final study (n=20) was 50.6±6.2 (range 28–59); 95% were female and the mean follow-up was 36 months (range 23–60). The mean age of the control group (n=20) was 47.7±8.6 (range 36–61); 95% were women with a mean follow-up of 42 months (range 21–84). There were no statistically significant differences in the demographic characteristics studied (Table 1). Insofar as the indication for the acromioplasty is concerned, the most common cause was tendonitis and bursitis without a tear of the rotator cuff in both group. Other causes were calcific tendonitis and a partial tear of the bursal surface.
Demographic characteristics of the fibromyalgia (FM) and control groups.
| Demographic characteristics | FM | Control | p |
|---|---|---|---|
| Mean age | 50.6 | 47.7 | .4 |
| Distribution by gender (male/female) | 1/19 | 1/19 | 1 |
| Involvement side right | 13 | 11 | .42 |
| Mean follow up time (months) | 36.1 | 42.4 | .11 |
| Tendinopathy/bursitis as preoperative diagnosis (%) | 83 | 79 | .51 |
| Other causes (%) | 17 | 21 | .51 |
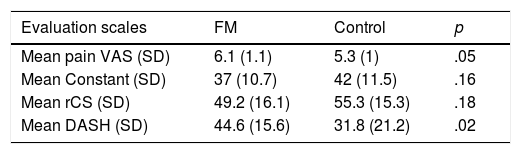
The mean preoperative CS score among participants with FM versus the control group was 37/42 (p=.16), the mean rCS was 49.2/55.3 (p=.18), the mean DASH was 45/32 (p=.02), and the mean VAS was 6.1/5.3 (p=.05). The only parameter in which significant preoperative differences were found between both groups was on the DASH. Table 2 summarises the preoperative measurements.
Preoperative results.
| Evaluation scales | FM | Control | p |
|---|---|---|---|
| Mean pain VAS (SD) | 6.1 (1.1) | 5.3 (1) | .05 |
| Mean Constant (SD) | 37 (10.7) | 42 (11.5) | .16 |
| Mean rCS (SD) | 49.2 (16.1) | 55.3 (15.3) | .18 |
| Mean DASH (SD) | 44.6 (15.6) | 31.8 (21.2) | .02 |
FM: fibromyalgia group; rCS: relative Constant score (adjusted for age and sex); SD: standard deviation.
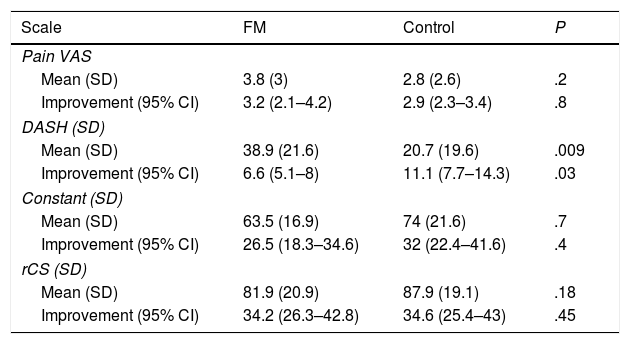
The mean postoperative values on the VAS, DASH, CS, and rCS scales are to be found in Table 3. There was a statistically significant improvement on all the mean values of both groups with respect to the mean preoperative values. The mean postoperative DASH was significantly worse (higher score) among the patients in the FM group when compared with the control group (38.9 vs. 20.7; p=.009).
Functional outcomes at the end of follow up and improvement with respect to the preoperative situation.
| Scale | FM | Control | P |
|---|---|---|---|
| Pain VAS | |||
| Mean (SD) | 3.8 (3) | 2.8 (2.6) | .2 |
| Improvement (95% CI) | 3.2 (2.1–4.2) | 2.9 (2.3–3.4) | .8 |
| DASH (SD) | |||
| Mean (SD) | 38.9 (21.6) | 20.7 (19.6) | .009 |
| Improvement (95% CI) | 6.6 (5.1–8) | 11.1 (7.7–14.3) | .03 |
| Constant (SD) | |||
| Mean (SD) | 63.5 (16.9) | 74 (21.6) | .7 |
| Improvement (95% CI) | 26.5 (18.3–34.6) | 32 (22.4–41.6) | .4 |
| rCS (SD) | |||
| Mean (SD) | 81.9 (20.9) | 87.9 (19.1) | .18 |
| Improvement (95% CI) | 34.2 (26.3–42.8) | 34.6 (25.4–43) | .45 |
FM: fibromyalgia group; rCS: relative Constant score (adjusted for age and sex); SD: standard deviation.
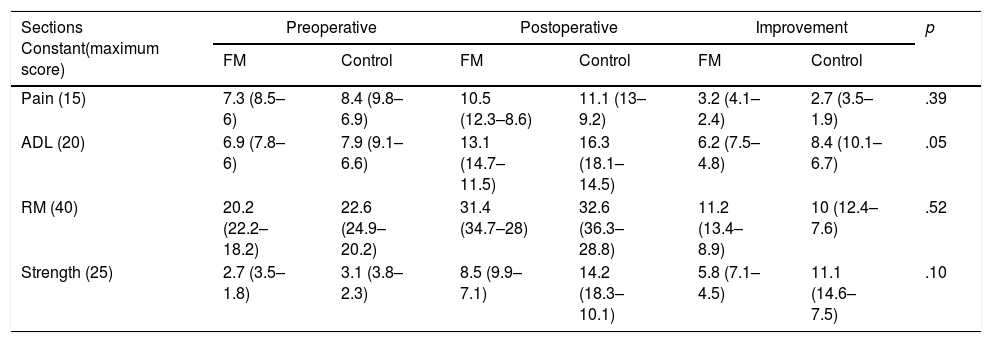
The CS scores from each group broken down by items are found in Table 4. There were no statistically significant postoperative differences in the range of movement, strength, or pain between the FM group and the control group. A trend towards signification was seen (p=.05) on the section of activities of daily living, the item having the worse score in the FM group.
Score obtained on the sections of the Constant scale before and after surgery (last follow up) and percentage of improvement in the group of patients with fibromyalgia (FM) and control group.
| Sections Constant(maximum score) | Preoperative | Postoperative | Improvement | p | |||
|---|---|---|---|---|---|---|---|
| FM | Control | FM | Control | FM | Control | ||
| Pain (15) | 7.3 (8.5–6) | 8.4 (9.8–6.9) | 10.5 (12.3–8.6) | 11.1 (13–9.2) | 3.2 (4.1–2.4) | 2.7 (3.5–1.9) | .39 |
| ADL (20) | 6.9 (7.8–6) | 7.9 (9.1–6.6) | 13.1 (14.7–11.5) | 16.3 (18.1–14.5) | 6.2 (7.5–4.8) | 8.4 (10.1–6.7) | .05 |
| RM (40) | 20.2 (22.2–18.2) | 22.6 (24.9–20.2) | 31.4 (34.7–28) | 32.6 (36.3–28.8) | 11.2 (13.4–8.9) | 10 (12.4–7.6) | .52 |
| Strength (25) | 2.7 (3.5–1.8) | 3.1 (3.8–2.3) | 8.5 (9.9–7.1) | 14.2 (18.3–10.1) | 5.8 (7.1–4.5) | 11.1 (14.6–7.5) | .10 |
The mean improvement between both group is expressed as a mean score with a 95% confidence interval in parenthesis.
ADL: activities of daily living; RM: range of movement.
At the end of the follow-up period, failure of the procedure, previously defined as an rCS of less than 70% and the need for revision surgery, was 28% in the FM group compared to 15% in the control group (p=.45) and failure of the procedure on the basis of pain (VAS>3 points) was 60% in the FM group versus 30% in the control group (p=.056). Only 35% of the patients in the control group reported taking analgesics following the surgery in contrast to 60% of the patients in the FM group (p=.11).
As regards the patients’ subjective satisfaction as appraised by means of the yes/no question “Are you satisfied with the result of the surgery?”, 85% of the patients belonging to the control group stated that they were satisfied in comparison to 55% of the subjects in the FM group (p=.03).
DiscussionArthroscopic subacromial decompression is an effective treatment for subacromial pain syndrome2; however, some studies report rates of residual pain in patients who have undergone the procedure of around 25%. The precise amount of time needed before the postoperative clinical evolution plateaus is arbitrary, but generally, by 6 months, most patients should have achieved the maximum medical improvement. Failure of the procedure has been related to several factors: technical mistakes, incorrect diagnosis, improper rehabilitation, or unrealistic postoperative expectations,3,4 but it is not clear as to whether or not certain preoperative patient characteristics, such as aberrant pain processing and modulation, can play a negative role in postoperative outcomes.
The clinical condition most often associated with aberrant pain processing is FM. This syndrome is characterised by generalised chronic pain in the absence of any underlying organic illness, and despite the fact that it is being diagnosed more and more, there are still many undiagnosed patients. The shoulder is one of the anatomical regions that is most affected in FM, giving rise to symptoms that are very similar to those of other illnesses, such as glenohumeral osteoarthritis, bursitis, or tears of the rotator cuff. This particularity can lead us to two different scenarios in the treatment of a painful shoulder not diagnosed with FM: (1) months of futile conservative treatment and (2) worse outcomes following surgical treatment.
However, we may also find specific involvement of the shoulder in patients diagnosed with FM. This study focuses on the particular group of patients, since there is no information about whether or not FM can cause worse clinical outcomes following surgical treatment for subacromial pain syndrome.
The prevalence of FM in the population is estimated to be between .2% and 5%.16 In our cohort, the prevalence rate was much higher (9%). This fact may be related to a higher prevalence of FM among women (in our series of 293 patients, 78% were female) and a greater involvement of the shoulder in patients diagnosed with FM (10 of the 18 trigger points are found in the shoulder and in the cervical region). Due to these factors, it is not uncommon for many patients diagnosed with FM to end up consulting a specialist in surgery of the shoulder; however, studies in this regard are scant. We only found a single study that evaluates the influence of this syndrome on treatment for shoulder pain.17 The authors conclude that it might be a cause for treatment failure; nevertheless, the previously mentioned study included all kinds of diagnoses and treatments (conservative and surgical treatments) and does not include a control group.
This is the first study that examines the influence of fibromyalgia on postoperative functional results following an isolated arthroscopic subacromial decompression and endorses the impression that the procedure is less successful when the patient has a diagnosis of FM. Only 55% of the subjects in the FM group were satisfied with the result, versus 85% in the control group, despite displaying similar improvement on the functional section. The low rate of satisfaction among patients with fibromyalgia has already been reported in earlier studies in the context of prosthetic surgery of the knee.18
Satisfaction following the surgery has been related with patient expectations19; FM patients are more demanding as regards postoperative results, as far as pain relief is concerned, and return to the activities of daily living, in comparison with the control group. The authors maintain that management of postoperative expectations is critical in this group of patients in particular in light of achieving better perception of postoperative results.
No statistically significant differences were found with respect to the mean postoperative CS between both groups; albeit on the DASH scale, the FM group exhibited worse results. This fact appears to be related with the presence of more subjective items on the DASH scale in comparison with the parameters evaluated by the CS. The DASH questionnaire consists of 30 items that are scored from 0 (no difficulty) to 100 (not able). The CS is divided into 4 sections: 2 subjective (pain and limitation to carry out the activities of daily living) and 2 objective (range of movement and strength). Therefore, when more objective scales are used the result in both groups tends to be similar.
The lower results on the postoperative DASH in patients diagnosed with FM may be related with the fatigue these patients perceive when conducting the activities of daily living. Fatigue is a very common symptom in this syndrome and is present in 100% of the cases.20 Fibromyalgia has been reported to be associated with greater perception of pain intensity, which manifests as greater cognitive and physical fatigue with healthy patients, not affected by this syndrome.21
With respect to the different sections evaluated by the CS, the increase in the parameters of pain, range of joint movement, and strength, from the preoperative to the postoperative situation was not statistically significant between the 2 groups. In the section of the activities of daily living in the FM group, worse results were attained versus the control group, with a trend towards signification. Likewise, both groups revealed significant improvement on all sections following surgery. Other authors have published similar outcomes in other orthopaedic procedures. Bican et al.,18 in a review of patients diagnosed with FM who underwent prosthetic arthroplasty of the knee for osteoarthritis, conclude that said patients exhibited lower rates of postoperative satisfaction with respect to the control group, despite objectifying comparable functional results. Dailey et al.21 demonstrated that the range of motion of the joint and strength in response to tasks to quantify physical fatigue was similar in patients with fibromyalgia when compared to a control group.
If we explore the pain quantified by means of the VAS, preoperative and postoperative pain was greater in the FM group in comparison with the control group. If we take into account the definition of failure of the SAD (VAS>3), it is concluded that there is a trend towards signification between the failure rate in the FM group versus the control group (60% vs. 30%); however, and in spite of the fact there is an increase in pain due to physical fatigue in the FM group,22 the objective items of the CS (strength and range of movement) were similar in both groups.
Therefore, patients diagnosed with FM experience a significant clinical improvement and better preoperative condition. For this reason, fibromyalgia cannot be considered a criterion to dismiss surgical treatment for subacromial syndrome. Nevertheless, the potential negative effects this syndrome can have on postoperative outcomes must be explained, so that expectations can be managed more realistically.
LimitationsThis study presents several limitations, including its retrospective design, although a prospective postoperative clinical evaluation was carried out, as well as the small size of the cohort; likewise, no information was available regarding the severity of the fibromyalgia (type, duration, and treatment). No system was used to select the controls beyond that of the similarity in demographic characteristics.
ConclusionsFibromyalgia can be considered as a prognostic factor that conditions worse postoperative outcomes following SAD. However, due to the clinical improvement these patients experiences in comparison to their preoperative status, we recommend applying surgical treatment when it is indicated.
Level of evidenceLevel of evidence III.
AuthorshipThe authors I. Lópiz and H. Marcelo have contributed equally in drafting this manuscript.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Lopiz Y, Marcelo H, Arvinius C, Rodriguez-Rodriguez L, García-Fernández C, Marco F. ¿Es la fibromialgia causa de fracaso de una descompresión subacromial artroscópica? Rev Esp Cir Ortop Traumatol. 2019;63:275–280.