Merkel cell tumour is a rare skin tumour of high malignancy, poor prognosis and low survival. It is characterized by its tendency to lymph node and vascular invasion and by a high percentage of locoregional recurrence in the year following surgical removal. It affects adults between 60 and 80 years of age and often occurs in the head and neck. We present the case of an 85-year-old man presenting with an ulcerated gluteal mass of 4 months’ evolution. Diagnosis was by histopathological and immunohistochemical study. Early diagnosis and appropriate treatment are important to improve the prognosis of these patients.
El tumor de células de Merkel es un tumor cutáneo raro, de elevada malignidad, mal pronóstico y baja supervivencia. Se caracteriza por su tendencia a la invasión ganglionar y vascular, y por un alto porcentaje de recurrencia locorregional en el año siguiente a la extirpación quirúrgica. Afecta a adultos entre los 60 y 80 años, y se localiza preferentemente en cabeza y cuello. Presentamos el caso de un varón de 85 años que acude por masa glútea ulcerada de 4 meses de evolución. El diagnóstico se realizó por estudio histopatológico e inmunohistoquímico. Un diagnóstico precoz y un tratamiento adecuado son importantes para mejorar el pronóstico de estos enfermos.
Merkel cell carcinoma is a rare, highly malignant skin tumour that comprises small cells with endocrine and epithelial characteristics. It affects adults of both sexes between the ages of 60 and 80. Its preferred location is photo-exposed head and neck areas with intense sun damage. It presents clinically as painless, rapidly growing, erythematous or violaceous subcutaneous skin nodules. Diagnosis is based on symptoms, histopathology and immunohistochemistry. Due to its low frequency and the advanced age of the patients, there are no prospective studies available, and there is no clear treatment algorithm.
We present the case of a Merkel cell tumour of atypical location and presentation as a large gluteal ulcerated mass.
Clinical caseAn 85-year-old male with a history of ischaemic heart disease, low-grade bladder carcinoma and various basal cell tumours removed due to gluteal bleeding. Examination revealed an indurated mass 15×15cm, adhering to the deep planes and ulcerated along with satellite lesions on the left buttock (Fig. 1) and adenopathies of pathological size in both groins.
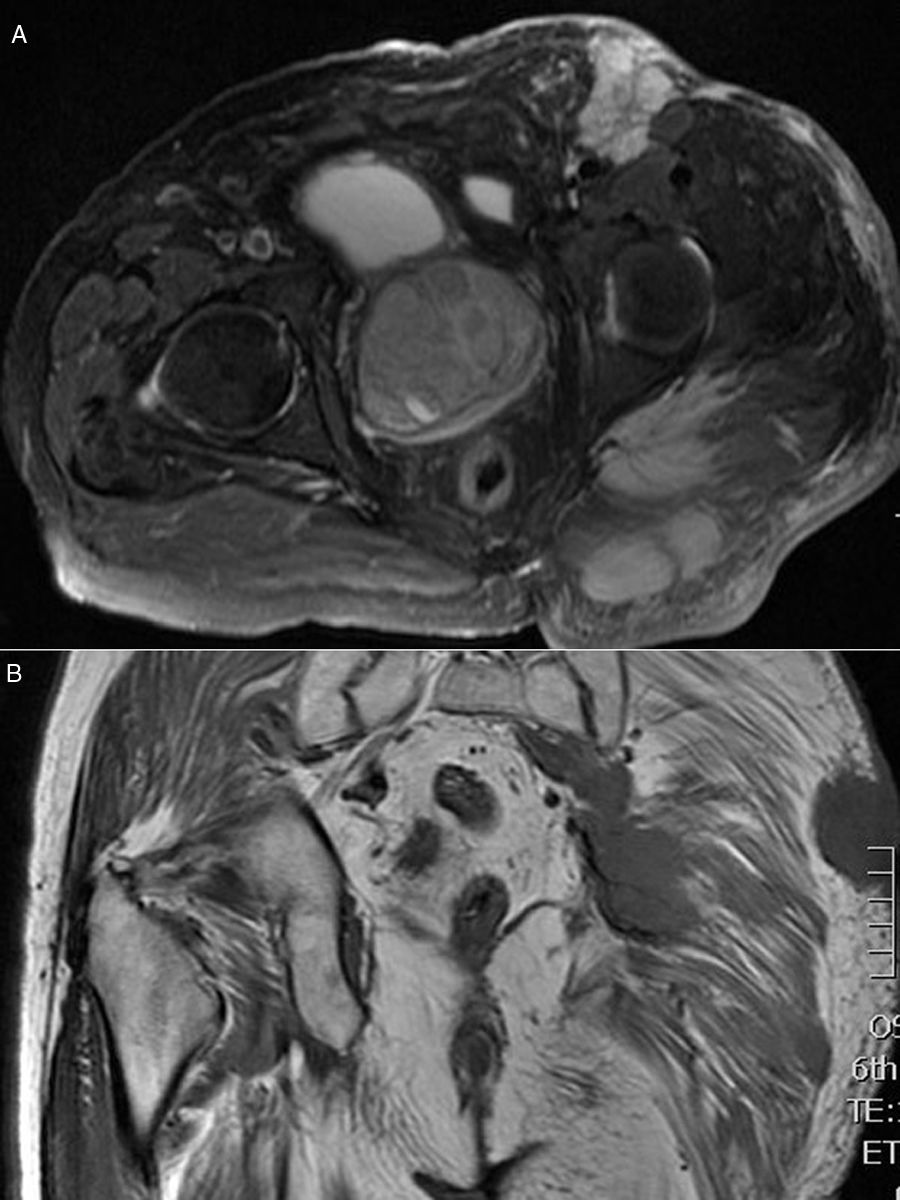
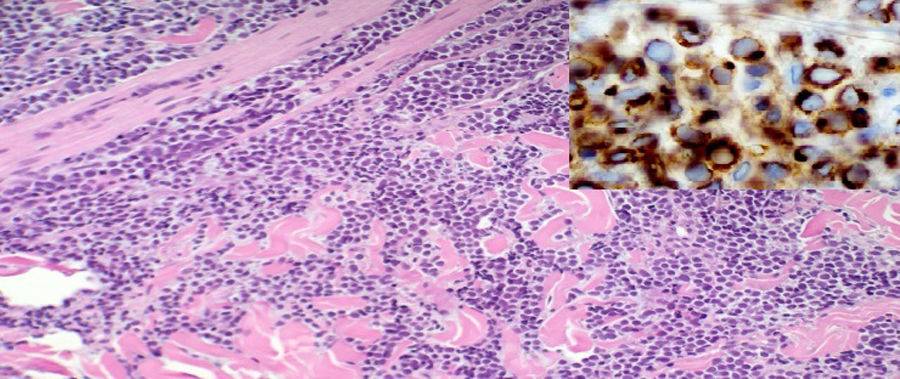
ResultsThoracic and abdominal computed tomography (CT) and MRI showed voluminous soft tissue masses in the left gluteal region, and at least 3 tumour lesions in the subcutaneous cell tissue were visualized, one in the gluteal musculature and another in the left inguinal region, together with an adenopathic block in the left retroperitoneal region extending to the ipsilateral common and external iliac chain (Fig. 2A and B). An incisional biopsy was performed. Pathological anatomy was reported as a primary neuroendocrine carcinoma of the skin, Merkel cell carcinoma (MCC) (Fig. 3).
DiscussionMCC is a rare, primary neuroendocrine tumour of the skin, with poor prognosis and survival. It is characterized as prone to nodal and vascular invasion, both of which are associated with a high percentage of locoregional recurrence within the first year following removal of the tumour.1
It usually presents in white adults over the age of 65, although there are published cases in young people with congenital ectodermal dysplasia.2 It prefers photo-exposed areas: 55% the head and neck, 40% the limbs and 5% the trunk.2–4 In almost a third of cases this tumour is associated with other skin neoplasms such as Bowen's disease, basal cell carcinoma or squamous cell carcinoma, as in our patient.4 More recent studies implicate the polyomavirus in the carcinogenesis of Merkel's carcinoma.5 It can appear as a secondary neoplasm in patients with immunological impairments of various aetiologies: chronic lymphatic leukaemia, B-cell lymphoma, HIV, and also in patients who have undergone organ transplantation or undergoing long-term immunosuppressive therapy6,7; its aggressiveness and mortality is even higher in these patients. Immunocompromise is a risk factor for MCC.
The skin lesion looks flattened (plaque or papule) or raised (nodule), it is red-violaceous in colour and rapid-growing. Epidermal involvement is rare, and therefore it seldom ulcerates.
Anatomopathological diagnosis is difficult since it can be easily confused with skin metastases of other round and small cell tumours: Ewing sarcoma, small-cell (oat cell) lung tumours or neuroblastoma. The use of immunohistochemistry positive to CK20 in a paranuclear dot pattern is required for accurate diagnosis.8
Distant metastases establish the stage, the skin being the most common site, followed by regional lymph nodes, liver, lung, bone and brain. Treatment includes extensive surgery with removal of the sentinel lymph node, radiotherapy, chemotherapy, but there is no established protocol for action due to its low incidence.9,10 For our patient, given his age and the extension of the tumour, we chose symptomatic treatment until the patient died, one month after diagnosis.
Our case is of interest in that it involved the existence of a rare skin tumour combined with an unusual site and presentation, which made initial clinical diagnosis of the lesion difficult.
Please cite this article as: Fernández-Regueiro R, Suárez-Sánchez FJ, Morís-de la-Tassa J. Carcinoma de células de Merkel de localización y presentación atípica. Rev Esp Cir Ortop Traumatol. 2019;63:313–315.