To non-invasively assess tissue lesion secondary to ischaemia applied during knee replacement surgery. Secondary objectives: to assess whether this lesion correlates with the duration of ischaemia and whether instrumental and gender variables influence it.
Material and methodsProspective cohort study. Pre and postoperative serum lactate levels have been determined as an indicator of glycolytic activity secondary to ischaemia in 88 patients. Serum lactate determination was performed by reactive strips of enzymatic–amperometric detection on capillary blood.
ResultsPreoperative serum lactate levels (mean and SD): 2.467±1.036mmol/L. Postoperative serum lactate levels: 3.938±2.018mmol/L. Ischaemia time 102.98±18.25min. Postoperative serum lactate levels were significantly higher than preoperative lactate levels. There are no statistical differences according to the time that the ischaemia was prolonged, gender or type of instrumentation used.
ConclusionsIn our study, postoperative serum lactate values were significantly higher than preoperative lactate values, with no correlation to the duration of ischaemia during knee replacement surgery.
Evaluar de forma no invasiva la lesión tisular secundaria a la isquemia aplicada durante la cirugía sustitutiva de rodilla. Objetivos secundarios: evaluar si dicha lesión se correlaciona con el tiempo que se prolonga la isquemia y la influencia de las variables instrumental y sexo.
Material y métodoEstudio de cohortes prospectivo. Se han determinado los niveles pre- y postoperatorios de lactato sérico, como indicador de actividad glucolítica secundaria a isquemia, en 88 pacientes. Se han empleado tiras reactivas de detección enzimático-amperométrica sobre sangre capilar.
ResultadosNiveles preoperatorios de lactato sérico (media y DE): 2,467±1,036mmol/L. Niveles postoperatorios de lactato sérico: 3,938±2,018mmol/L. Tiempo de isquemia 102,98±18,25min. Los niveles postoperatorios de lactato sérico han sido significativamente mayores que los preoperatorios. No existen diferencias atendiendo a las variables tiempo que se prolonga la isquemia, sexo o tipo de instrumentación empleada.
ConclusionesEn nuestro estudio, los valores de lactato sérico postoperatorios han sido significativamente mayores que los preoperatorios, sin una correlación con el tiempo que se ha prolongado la isquemia durante la cirugía sustitutiva de rodilla.
The use of the ischaemia cuff in orthopaedic surgery is routine practice. Bloodless limb surgery was introduced by Johannes Friedrich August von Esmarch in 1873, using an elastic bandage. In 1908 Harvey Williams Cushing improved the technique with the introduction of the pneumatic tourniquet.
The ischaemic cuff in knee replacement surgery provides a bloodless surgical field, enabling anatomical dissection, the visualisation of structures and optimal surgical conditions,1 with better bone penetration of the cement layer.2 However, it is not free from potential risk, therefore there is controversy surrounding its use and we cannot conclude uniform recommendation with sufficient evidence from the different systematic reviews and meta-analyses.3–9 The published disadvantages of the ischaemic cuff during knee replacement surgery are: increased postoperative bleeding,4 increased incidence of thromboembolic complications,5 increased rate of neuromuscular10 or skin complications,11 and delayed rehabilitation immediately after surgery.12
Ischaemia increases capillary permeability, causes alterations in coagulation and increases levels of proinflammatory cytokines. Added to the metabolic tissue alterations secondary to hypoxia is the increase in glycolytic activity and decreased pH in the tissues subjected to ischaemia. Muscular tissue is more likely to suffer metabolic injury due to ischaemia. The interruption of blood supply to the myocyte hinders oxidative phosphorylation in the mitochondria and inhibits the generation of aerobic energy. Muscle cells are forced to rely on anaerobic metabolism, and the production of adenosine triphosphate (ATP) is reduced. The continuous need for energy conditions ATP hydrolysis to adenosine diphosphate and the latter to adenosine monophosphate, whose metabolism plays an important role in the genesis of the so-called ischaemia-reperfusion syndrome. Anaerobic glycolysis causes an accumulation of lactate and protons, which triggers progressive acidification of the intracellular medium. This acidification, together with the reduction of ATP, is responsible for the decreased activity of the Na+/K+-ATPase and Ca2+-ATPase pumps, which causes an increase in intracellular Na+ and Ca2+ levels and, eventually, cellular lysis if the duration of ischaemia exceeds a critical level. With reperfusion, in tissues subjected to injury by ischaemia a series of agents come into play that will increase local damage and will extend the damage to the rest of the organism: the proinflammatory cytokines (interleukin 1 and 6, thromboxane A2 and tumour necrosis factor), the complement system, the activated polymorphonuclear leukocytes (basically neutrophils), oxygen free radicals and alteration of capillary permeability.
Some authors defend implanting knee prostheses without ischaemia,13 in order to prevent the vascular, neurological and metabolic complications described, but most orthopaedic surgeons choose to use it.
The primary objective of the study was to assess tissue damage secondary to ischaemia applied during knee replacement surgery in a non-invasive way (using an indirect, simple-to-determine indicator, such as serum lactate levels). Our secondary objectives were to assess whether this injury correlates with the duration of the ischaemia during the intervention and the influence of the instrumental and sex variables.
Material and methodA prospective, cohort study performed in a single centre that comprised testing for serum lactate levels in capillary blood preoperatively (5min before expressing the limb to be operated and the application of ischaemia, and postoperatively (5min after releasing the ischaemia) in 88 patients who had undergone knee replacement. All the interventions were performed by the same surgical team that comprised 2 senior surgeons, with wide experience in knee replacement surgery. The study followed the ethical principles for medical research on human beings of the World Medical Assembly, ratified in October 2013, and was accepted by the Clinical Research Ethics Committee. The patients included in the study gave their informed consent.
The lactate tests were performed using enzymatic–amperometric test strips. The Lactate Scout+(SensLab GmbH, Germany) model was used. The measurement range of this device is estimated from .5 to 25mmol/L and requires a blood volume of .2μL for testing. Specific orthopaedic surgery and trauma nursing staff took the capillary blood samples and managed the device for testing the samples.
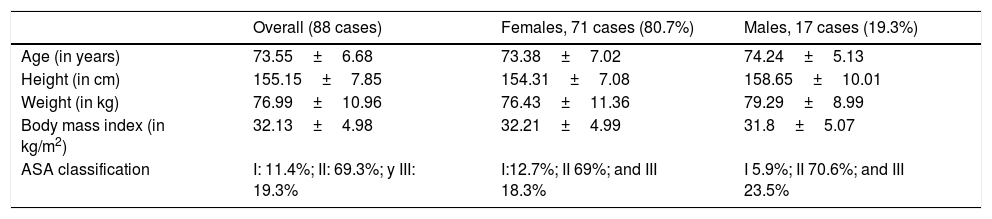
The MART™ or HemaClear® (OHK Medical Devices, Haifa, Israel)14,15 ischaemia system was used for all the cases. This system consists of a silicone ring that exerts radial pressure distributed around the complete circumference of the limb. The properties of silicone are used to create a supra systolic pressure distribution on the limb. Sizes L or XL were used for all the cases studied according to the circumference of the muscle of the limb to be operated (with pressure provided by the manufacturer of 286±54mmHg for size L and 321±21mmHg for size XL). The demographic and anthropometric features of the series are shown in Table 1. The pharmacological management of the patients did not differ from the protocol for knee replacement surgery, except for the saline drip used, which was .9% physiological saline solution exclusively. Antibiotic prophylaxis was used in all cases during anaesthetic induction with 2g intravenous cefazolin (Cefazolin Normon, Laboratorios Normon S.A., Madrid, Spain) or 1g Vancomycin (Vancomycin Pfizer, Pfizer S.L., Madrid, Spain) in patients allergic to betalactamics. Tranexamic acid was used (Amchafibrin®, Meda Pharma SL, Madrid, Spain) in all the patients, administering one dose of 15mg/kg weight before removal of ischaemia.
Demographic and anthropometric features of the series.
| Overall (88 cases) | Females, 71 cases (80.7%) | Males, 17 cases (19.3%) | |
|---|---|---|---|
| Age (in years) | 73.55±6.68 | 73.38±7.02 | 74.24±5.13 |
| Height (in cm) | 155.15±7.85 | 154.31±7.08 | 158.65±10.01 |
| Weight (in kg) | 76.99±10.96 | 76.43±11.36 | 79.29±8.99 |
| Body mass index (in kg/m2) | 32.13±4.98 | 32.21±4.99 | 31.8±5.07 |
| ASA classification | I: 11.4%; II: 69.3%; y III: 19.3% | I:12.7%; II 69%; and III 18.3% | I 5.9%; II 70.6%; and III 23.5% |
Values in means and standard deviation.
ASA classification: physical status classification updated in 2014 by the American Society of Anaesthesiologists (ASA I: normal, healthy patients, ASA II: patients with mild systemic diseases and ASA III: patients with severe systemic diseases).
The iMNS-Medacta Navigation System (Medacta International S.A., Castel San Pietro, Switzerland) was used to implant the prosthesis in 20 cases (22.7%) and patient-specific cutting blocks after designing the intervention on 3-dimensional virtual models using computerised tomography with the MyKnee® system (Medacta International S.A., Castel San Pietro, Switzerland) in 68 cases (77.3%). The same prosthesis model was implanted in all cases, Global Medacta Knee (GMK®, Medacta International S.A., Castel San Pietro, Switzerland) cemented with ultracongruant insert. The patella was replaced in the cases where a surgical navigation system was used and in those where patient-specific cutting blocks were used it was not.
Patients with severe arterial hypertension, a recent history of trauma and diseases that cause tissue hypoxia, alterations of the acid–base balance or increased lactate production were excluded from the study. Patients operated in one stage for prostheses in both knees and patients operated using anaesthesia other than spinal were also excluded from the study.
The data analysis was performed using IBM SPSS v.24 for Windows. Given the normal distribution of the values, the Student's t-test was used for related and independent variables. Bivariate correlations were used with Pearson's correlation. Confidence intervals of 95% and significance level of .05.
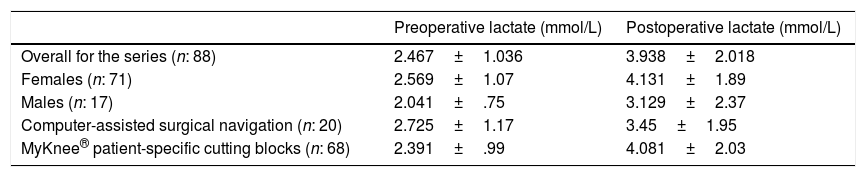
ResultsWe obtained a mean preoperative serum lactate level of 2.467±1.036mmol/L. The mean postoperative serum levels were significantly higher than the preoperative levels. Table 2 shows the results in terms of gender and type of instrumentation system.
Preoperative and postoperative lactate levels in terms of gender and instrumentation system.
| Preoperative lactate (mmol/L) | Postoperative lactate (mmol/L) | |
|---|---|---|
| Overall for the series (n: 88) | 2.467±1.036 | 3.938±2.018 |
| Females (n: 71) | 2.569±1.07 | 4.131±1.89 |
| Males (n: 17) | 2.041±.75 | 3.129±2.37 |
| Computer-assisted surgical navigation (n: 20) | 2.725±1.17 | 3.45±1.95 |
| MyKnee® patient-specific cutting blocks (n: 68) | 2.391±.99 | 4.081±2.03 |
Results in means and standard deviation.
In the time margins in which the operations included in this study were undertaken, there was no linear correlation between the duration of the ischaemia and the postoperative lactate levels.
We found no significant difference between the postoperative lactate levels when contrasting the instrumentation system used. The duration of the ischaemia was significantly longer for the cases where computer-assisted surgical navigation was used (119.7±12.21min) than for those where patient-specific cutting blocks were used (98.06±16.79min) as instrumentation.
Both preoperatively and postoperatively, we found higher serum lactate levels in the females than in the males but with no statistically significant difference. We found no significant correlation between BMI levels and serum lactate levels, either pre or postoperatively.
DiscussionTolerance of ischaemia is variable in the different body tissues. Different critical ischaemia times have been established (maximum ischaemia time at ambient temperature that each tissue can tolerate, remaining viable after reperfusion).16 The muscle tissue in the extremities is more sensitive and a critical ischaemia time of 4h is indicated compared to other tissues such as the peripheral nerve (8h), fat (13h), skin (24h) or bone tissue (4 days).16 It is currently recommended that 120min of ischaemia should not be exceeded in surgery to the lower limbs,17 although there is insufficient evidence to contraindicate prolonging ischaemia to 3h. Even if this conventional safety margin of 120min is not exceeded, biochemical changes occur in the muscle tissue, which is the focus of our paper. Ischaemia applied to the lower limb during knee replacement surgery can cause tissue injury through three mechanisms: mechanical injury due to the compression exerted by the device itself to maintain ischaemia,18,19 anoxia injury caused by tissue ischaemia over the duration of the intervention,16 and inflammatory and oxidative injury caused by reperfusion of the tissues previously subjected to ischaemia.20 At the level of the muscles, interruption of blood supply to the myocyte inhibits oxidative phosphorylation in the mitochondria and the generation of aerobic energy. Anaerobic glycolysis causes an accumulation of lactate and protons, which causes progressive acidification of the intracellular medium. In our paper we used serum lactate as a marker of increased anaerobic glycolysis secondary to ischaemia.
Increased serum lactate is a common indicator of severity for critical patients with sepsis21 although it has also been shown to be useful in stratifying risk for patients with other non-infectious diseases such cardiac arrest, acute myocardial infarction with ST elevation, pulmonary thromboembolism, severe trauma (with or without vascular involvement) and different alterations of tissue perfusion status.22,23 Elevated serum lactate levels can be found in different pathological conditions such as liver cirrhosis, chronic kidney failure, diabetes mellitus, certain neoplasms, convulsive states, cholera, acute pancreatitis and with the used of some drugs such as biguanides, isoniazid, nitroprusside, ethanol and salicylates.
Lactate is easy to test and there is a strong correlation between arterial and venous lactate levels.23 We did not know, before our study, of lactate being used through capillary blood samples as a marker of glycolytic activity secondary to ischaemia to the limb after protocolised use of a tourniquet for knee replacement surgery. Ejaz et al. used microdialysis to determine metabolic changes of ischaemia and reperfusion in patients who underwent knee prosthesis implantation with and without a tourniquet.24 They describe an immediate increase in lactate and a change in the lactate/pyruvate ratio in patients operated using an ischaemia tourniquet, and the normalisation of levels after 60min of reperfusion.
Our study's greatest weakness is that it lacks determination of a baseline serum lactate level in the absence of a stress factor in the patients in the series. If we consider a normal venous serum value in non-stressed patients to be .5–2.2mmol/L (4.5–19.8mg/dL) (normality in arterial plasma is established at between .5 and 2.2mmol/L or between 4.5 and 14.4mg/dL), we obtained significantly higher values preoperatively in our series. Given that testing took place immediately preoperatively we cannot consider our patients to be non-stressed. We think, therefore, that this preoperative elevation might be due to a metabolic change as a response to the patients’ stress before their operation.
A second weakness is that there is no consensus with regard to the validity of capillary blood lactate testing using enzyme-based amperometric reactive strips. Bouzat et al. compared capillary blood lactate levels tested using a portable device and reactive strips with arterial or venous blood values tested using conventional laboratory techniques in adult patients with severe trauma and concluded a significant discrepancy.25 In contrast, other studies such as those published by Purcarea et al.26 or Baig et al.,27 performed on patients with sepsis, confirmed that testing capillary blood serum lactate levels is a method as sensitive as conventional laboratory tests, with the advantage of immediacy. A third weakness of our paper is that none of the portable devices marketed is absolutely accurate, but it has been estimated, in different studies, that these types of devices are sufficiently reliable to test capillary blood lactate levels.28,29
The most relevant observations of our study are that there is a significant postoperative increase in serum lactate levels, as translation of the increased glycolytic activity secondary to ischaemia, with no correlation with the duration of ischaemia during knee-replacement surgery.
Level of evidenceLevel of evidence iib.
Ethical disclosuresProtection of people and animalsThe authors declare that no experiments were performed on humans or animals for this study.
Data confidentialityThe authors declare that they have followed the protocols of their centre of work regarding the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
To the team of Surgical Orthopaedic and Trauma nurses in charge of serum lactate testing, comprising Guadalupe Buitrago, Víctor Calvo, Guillermo Escribano and Josefa Lucas.
Please cite this article as: León-Muñoz VJ, Lisón-Almagro AJ, Hernández-García CH, López-López M. Monitorización de la actividad glucolítica secundaria a isquemia en cirugía sustitutiva de rodilla. Rev Esp Cir Ortop Traumatol. 2018;62:359–364.