Total hip replacement (THR) is challenging in octogenarians due to associated comorbidities and controversy regarding fixation type. We ask whether cemented THR is superior to uncemented THR in patients above the age of 80 years.
Methods382 patients (441 hips) aged 80 years or older who underwent THR between 2004 and 2015 were analysed. A cemented THR was implanted in 196 hips (group 1), an uncemented THR with a grit-blasted stem in 121 (group 2), or with a porous-coated stem in 124 (group 3). Patients in group 1 had a higher mean age, more comorbidities and osteoporotic bone. Survival analysis was calculated using cumulative incidence function to account for the competing risk of death.
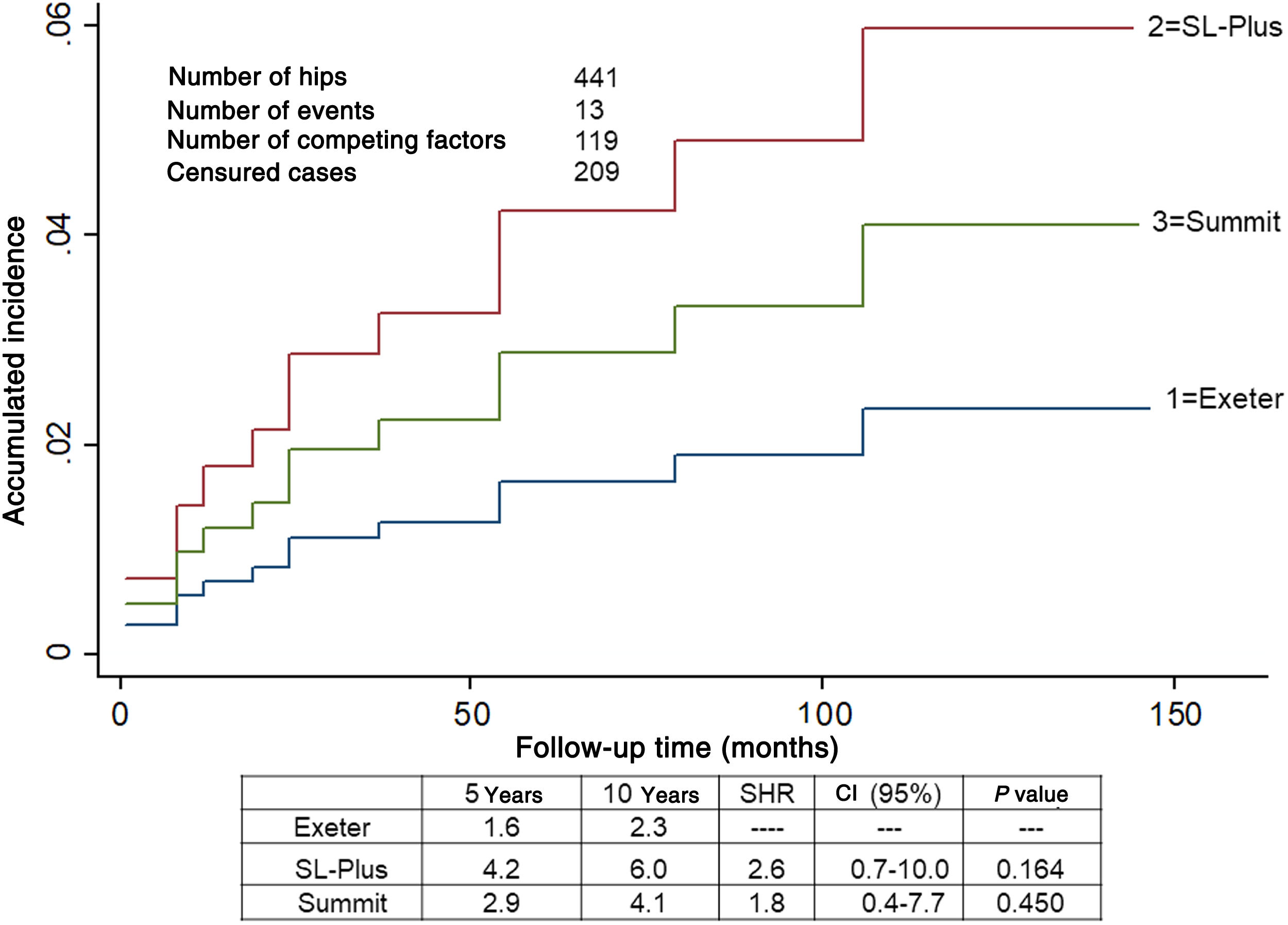
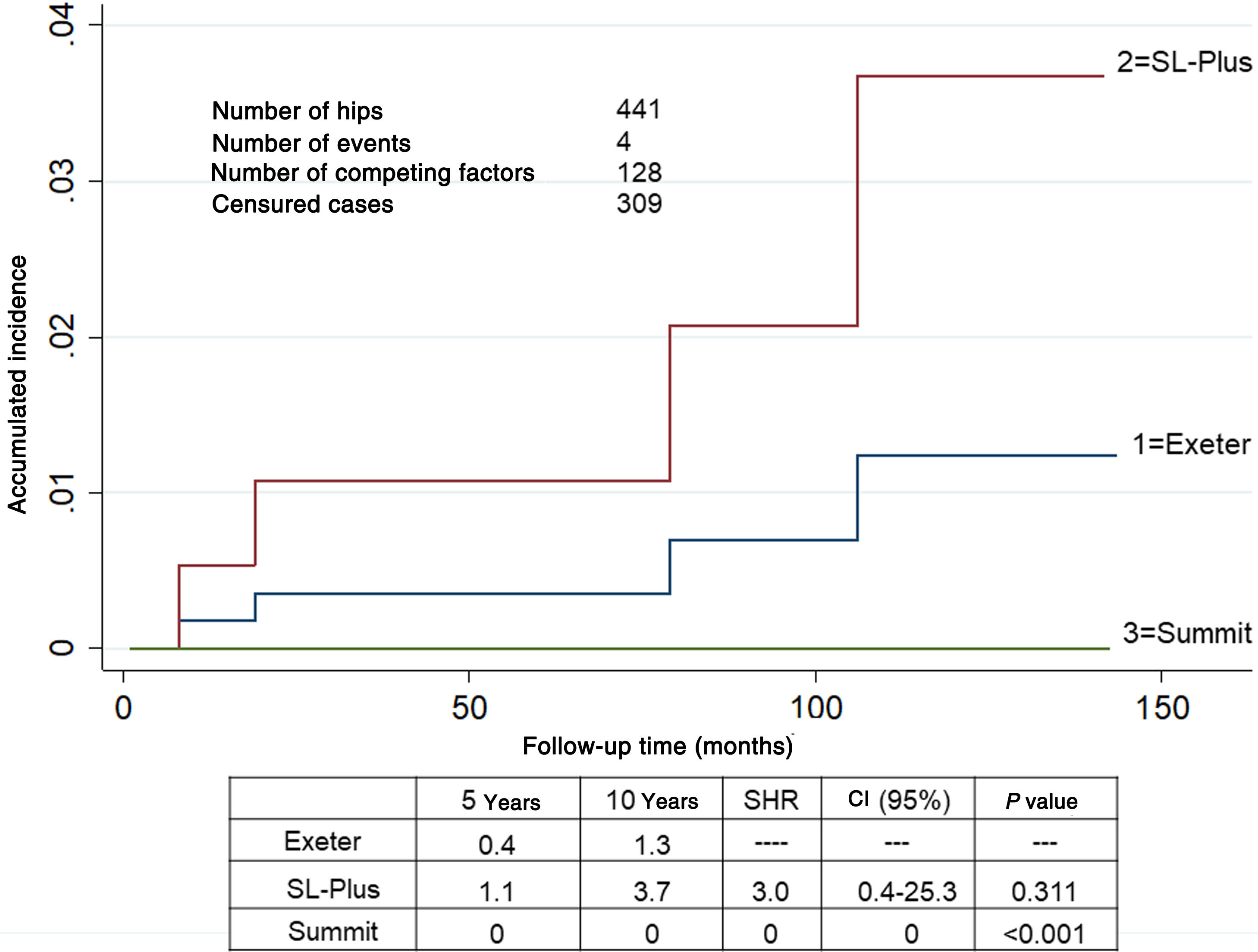
ResultsMedical complications rate was similar. There were three post-operative fractures: one in group 2 and two in group 3. Competing risk analysis showed that the cumulative incidence of revision for any cause was 2.3 in group 1, 6.0 in group 2 and 4.1 in group 3 at ten years, and the cumulative incidence of revision for aseptic loosening was 1.2 in group 1, 3.7 in group 2 and 0 in group 3 at the same period.
ConclusionsTHR presents an acceptable number of adverse events for octogenarian patients. Despite uncemented fixation was satisfactory, the higher peri-prosthetic fracture rate worsens results in this group.
La prótesis total de cadera (PTC) en pacientes octogenarios presenta dificultades debido a las comorbilidades asociadas y al tipo de fijación a utilizar. Nos preguntamos si los resultados de la PTC cementada son mejores que la PTC no cementada en pacientes mayores de 80 años.
Material y métodos382 pacientes (441 caderas) de 80 o más años de edad fueron intervenidos de PTC entre 2004 y 2015. Se comparan tres grupos: grupo 1, PTC cementada, 196 caderas; grupo 2, PTC no cementada con vástago de superficie rugosa, 121 caderas; grupo 3, PTC no cementada con vástago de recubrimiento poroso proximal, 124 caderas. En el grupo 1 la edad media, el grado de osteoporosis y el número de comorbilidades fue mayor. Se calculó la incidencia acumulada de cirugía de revision y aflojamiento teniendo en cuenta la mortalidad como factor de riesgo por competencia.
ResultadosLas complicaciones médicas fueron similares entre los grupos. Hubo tres fracturas periprotésicas, una en el grupo 2 y dos en el grupo 3. El análisis mediante el riesgo por competencias mostró una incidencia acumulada de revisión por cualquier causa a los 10 años del 2,3% en el grupo 1, 6%, en el grupo 2 y 4,1% en el grupo 3, y por aflojamiento aséptico para el mismo período del 1,2% en el grupo 1, 3,7% en el grupo 2 y 0% en el grupo 3.
ConclusionesLa PTC presenta resultados fiables con bajas tasas de cirugía de revision en pacientes octogenarios. La fijación no cementada es satisfactoria en pacientes octogenarios, sin embargo, el mayor número de fracturas periprotésicas empeoran los resultados.
The increase in the elderly population coincides with greater demand for total hip prosthesis (THP).1 In spite of the higher risk of the procedure in octogenarian patients, the overall rate of adverse effects is low, so that THP is considered to be reliable in this population in the majority of cases.2–4 Different early recovery protocols have been shown to be effective, even in patients older than 85 years, once the risks have been identified.5
On the other hand, although cemented THPs have been shown to give excellent results, in elderly patients above all, the indication for cementless prostheses continues to grow in popularity in all age groups.6,7 Another controversy in this group of patients centres on the type of survival analysis which should be used to evaluate the results in populations with a higher rate of mortality.8,9
We ask whether the rate of complications and results of cemented THPs are better than those of cementless THPs in patients over the age of 80 years, taking mortality into account as a competing risk factor. This study compares the complications, clinical and radiological results between one group of patients given a cemented THP and 2 groups who were given cementless THPs.
Material and methodsStudy designIn this cohort study 382 patients aged 80 or more years were identified who had received a primary THP (441 hips) from January 2004 to December 2015. Only patients with primary osteoarthrosis, avascular femoral head necrosis, slight hip dysplasia according to Hartofilakidis10 or post-traumatic arthrosis were included. Patients with other diagnoses were excluded, as they require implantation techniques other than the implantation of a conventional acetabular component with its associated surgery (the use of bone autograft for acetabular reconstruction and reconstruction rings). The excluded diagnoses were advanced hip dysplasia (lower or upper Hartofilakidis luxation) and other entities involving severe acetabular defects, patients with femoral neck fractures, bone tumours, pathological fractures or ones with a double mobility cup as well as hybrid or inverse THP. The preoperative variables analysed included patient demographic data, radiological femur type according to Dorr11 and associated comorbidities. The state of health of the patients was evaluated according to the American Society of Anaesthesiologists (ASA) classification system.12 Given that life expectancy is less in this age group, the minimum follow-up for inclusion of the patients in the study, once those lost due to other causes before this period had been excluded, was 4 years for live patients who had not received a check-up. The average follow-up lasted for 6.5 years. All of the patients were informed about the intervention before their operation and the approval of the Ethics Committee of our institution was obtained (PI-3845).
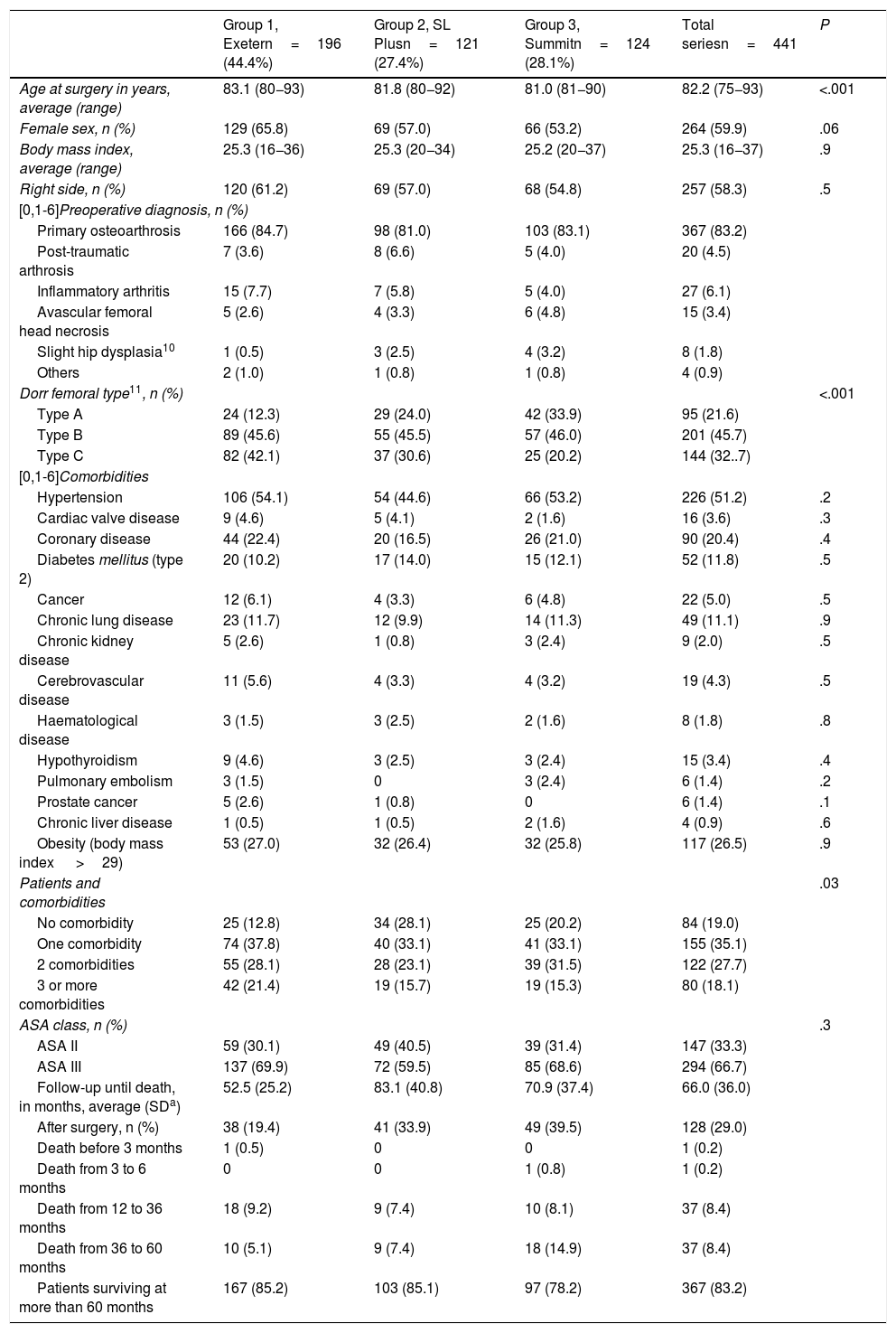
Three groups were considered, depending on the type of THP: group 1 included 172 patients (196 hips) with a cemented THP, a Contemporary cup and an Exeter stem (Stryker Orthopedics, Mahwah, NJ, U.S.A.); group 2 contained 103 patients (121 hips) with a cementless rectangular straight dual taper roughened stem, a Bicon or EP-Fit cup and SL-Plus stem (Smith & Nephew, Memphis, TN, U.S.A.), while group 3 contained 107 patients (124 hips) with a cementless stem with a proximal porous coating, a Pinnacle cup and Summit stem (De Puy-Johnson & Johnson, Warsaw, IN, U.S.A.). The ball and cup materials were always metal - polyethylene. The femoral head diameter was 28mm in 193 group 1 hips (93.4%), 94 hips in group 2 (77.7%) and 121 hips in group 3 (97.6%), and it was 32mm in the other. The patients included in group 1 had an older average age and with more type C femurs according to the Dorr classification, and a higher number of associated comorbidities (Table 1).
Demographic data in each group.
| Group 1, Exetern=196 (44.4%) | Group 2, SL Plusn=121 (27.4%) | Group 3, Summitn=124 (28.1%) | Total seriesn=441 | P | |
|---|---|---|---|---|---|
| Age at surgery in years, average (range) | 83.1 (80−93) | 81.8 (80−92) | 81.0 (81−90) | 82.2 (75−93) | <.001 |
| Female sex, n (%) | 129 (65.8) | 69 (57.0) | 66 (53.2) | 264 (59.9) | .06 |
| Body mass index, average (range) | 25.3 (16−36) | 25.3 (20−34) | 25.2 (20−37) | 25.3 (16−37) | .9 |
| Right side, n (%) | 120 (61.2) | 69 (57.0) | 68 (54.8) | 257 (58.3) | .5 |
| [0,1-6]Preoperative diagnosis, n (%) | |||||
| Primary osteoarthrosis | 166 (84.7) | 98 (81.0) | 103 (83.1) | 367 (83.2) | |
| Post-traumatic arthrosis | 7 (3.6) | 8 (6.6) | 5 (4.0) | 20 (4.5) | |
| Inflammatory arthritis | 15 (7.7) | 7 (5.8) | 5 (4.0) | 27 (6.1) | |
| Avascular femoral head necrosis | 5 (2.6) | 4 (3.3) | 6 (4.8) | 15 (3.4) | |
| Slight hip dysplasia10 | 1 (0.5) | 3 (2.5) | 4 (3.2) | 8 (1.8) | |
| Others | 2 (1.0) | 1 (0.8) | 1 (0.8) | 4 (0.9) | |
| Dorr femoral type11, n (%) | <.001 | ||||
| Type A | 24 (12.3) | 29 (24.0) | 42 (33.9) | 95 (21.6) | |
| Type B | 89 (45.6) | 55 (45.5) | 57 (46.0) | 201 (45.7) | |
| Type C | 82 (42.1) | 37 (30.6) | 25 (20.2) | 144 (32..7) | |
| [0,1-6]Comorbidities | |||||
| Hypertension | 106 (54.1) | 54 (44.6) | 66 (53.2) | 226 (51.2) | .2 |
| Cardiac valve disease | 9 (4.6) | 5 (4.1) | 2 (1.6) | 16 (3.6) | .3 |
| Coronary disease | 44 (22.4) | 20 (16.5) | 26 (21.0) | 90 (20.4) | .4 |
| Diabetes mellitus (type 2) | 20 (10.2) | 17 (14.0) | 15 (12.1) | 52 (11.8) | .5 |
| Cancer | 12 (6.1) | 4 (3.3) | 6 (4.8) | 22 (5.0) | .5 |
| Chronic lung disease | 23 (11.7) | 12 (9.9) | 14 (11.3) | 49 (11.1) | .9 |
| Chronic kidney disease | 5 (2.6) | 1 (0.8) | 3 (2.4) | 9 (2.0) | .5 |
| Cerebrovascular disease | 11 (5.6) | 4 (3.3) | 4 (3.2) | 19 (4.3) | .5 |
| Haematological disease | 3 (1.5) | 3 (2.5) | 2 (1.6) | 8 (1.8) | .8 |
| Hypothyroidism | 9 (4.6) | 3 (2.5) | 3 (2.4) | 15 (3.4) | .4 |
| Pulmonary embolism | 3 (1.5) | 0 | 3 (2.4) | 6 (1.4) | .2 |
| Prostate cancer | 5 (2.6) | 1 (0.8) | 0 | 6 (1.4) | .1 |
| Chronic liver disease | 1 (0.5) | 1 (0.5) | 2 (1.6) | 4 (0.9) | .6 |
| Obesity (body mass index >29) | 53 (27.0) | 32 (26.4) | 32 (25.8) | 117 (26.5) | .9 |
| Patients and comorbidities | .03 | ||||
| No comorbidity | 25 (12.8) | 34 (28.1) | 25 (20.2) | 84 (19.0) | |
| One comorbidity | 74 (37.8) | 40 (33.1) | 41 (33.1) | 155 (35.1) | |
| 2 comorbidities | 55 (28.1) | 28 (23.1) | 39 (31.5) | 122 (27.7) | |
| 3 or more comorbidities | 42 (21.4) | 19 (15.7) | 19 (15.3) | 80 (18.1) | |
| ASA class, n (%) | .3 | ||||
| ASA II | 59 (30.1) | 49 (40.5) | 39 (31.4) | 147 (33.3) | |
| ASA III | 137 (69.9) | 72 (59.5) | 85 (68.6) | 294 (66.7) | |
| Follow-up until death, in months, average (SDa) | 52.5 (25.2) | 83.1 (40.8) | 70.9 (37.4) | 66.0 (36.0) | |
| After surgery, n (%) | 38 (19.4) | 41 (33.9) | 49 (39.5) | 128 (29.0) | |
| Death before 3 months | 1 (0.5) | 0 | 0 | 1 (0.2) | |
| Death from 3 to 6 months | 0 | 0 | 1 (0.8) | 1 (0.2) | |
| Death from 12 to 36 months | 18 (9.2) | 9 (7.4) | 10 (8.1) | 37 (8.4) | |
| Death from 36 to 60 months | 10 (5.1) | 9 (7.4) | 18 (14.9) | 37 (8.4) | |
| Patients surviving at more than 60 months | 167 (85.2) | 103 (85.1) | 97 (78.2) | 367 (83.2) | |
After evaluation by the Anaesthesiology Department all of the procedures were performed in patients classified as ASA II or III, and under spinal anaesthesia. A posterolateral approach with repair of the capsule was used the most frequently in group 1 (160 hips, 91.8%) and in group 3 (98 hips, 79%), while an anterolateral approach was more frequent in group 2 (70 hips, 57.9%). Cemented THP were implanted according to current technical principles13,14 and the cementless THP were implanted following the recommendations for each design.15,16 All of the patients received antibiotic and thromboembolic prophylaxis, following the recommendations of our hospital. The indication for postoperative erythrocyte concentrate transfusion was a value lower than 8g/dl or lower than 9g/dl in patients with symptoms of anaemia or at cardiological risk, according to the recommendations of the Geriatric Department. Assisted walking was permitted on the day after the operation, depending on pain level and under the guidance of the physiotherapist. Patients walked with sticks during 3–6 weeks, depending on the conditions of the wound and their stability while walking.
Clinical evaluationThe frequency of all adverse effects was considered, defined as any unexpected complication which prolonged hospitalisation or caused temporary or permanent sequelae. The clinical results of the patients were evaluated using the Harris Hip Score (HHS).17
Radiographic evaluationAnteroposterior X-ray images of the pelvis and lateral images of the hip were taken after the operation, at 3, 6 and 12 months, and then annually while following the same protocol. Measurements were made by the same author (EGR). Data were recorded on the position of the cup (abduction angle and the vertical and horizontal distance)18 and anteversion.19 Data were also recorded on whether cups were positioned outside or inside the safety zone defined by Lewinnek et al.,20 reconstruction of the centre of rotation of the hip21 and the abductor mechanism.22 Lastly, the position of the femoral stem and the possible appearance of radiotransparent lines were analysed, together with osteolysis on the acetabular and femoral sides.23,24
Statistical analysisQualitative data were expressed in numbers and percentages, and quantitative data were expressed as an average and standard deviation (SD) or ranges. Qualitative data were compared using the χ2 test or Fisher’s exact test, and qualitative data were compared using the Mann-Whitney U test. Survival for revision for any reason or because of aseptic loosening of any component was calculated in the form of accumulated incidence, taking death into account as a competing risk factor.25 This technique was used because Kaplan-Meier analysis overestimates survival figures when mortality is high.9 The level of significance was P<.05. Statistical analysis was performed using the SAS 9.1 statistical package (SAS Institute Inc., Cary, NC, U.S.A.).
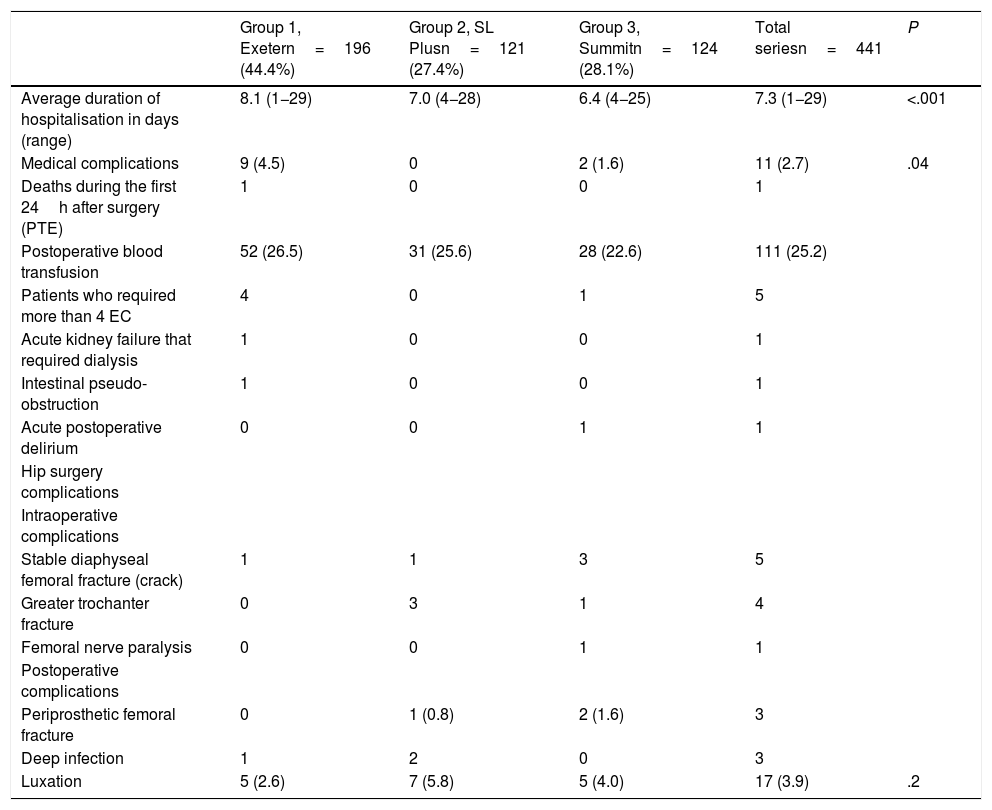
ResultsComplicationsOne patient in group 1, an 81 year-old male, ASA III class with cardiovascular disease and arterial hypertension, died 6h after surgery due to pulmonary embolism. The total number of medical complications and blood transfusions was similar in all 3 groups; however, in group 1 the average duration of hospitalisation and the number of patients who required more than 4 erythrocyte concentrates during the immediate postoperative period were higher (Table 2).
Duration of hospitalisation, medical complications and complications arising from hip surgery, n (%).
| Group 1, Exetern=196 (44.4%) | Group 2, SL Plusn=121 (27.4%) | Group 3, Summitn=124 (28.1%) | Total seriesn=441 | P | |
|---|---|---|---|---|---|
| Average duration of hospitalisation in days (range) | 8.1 (1−29) | 7.0 (4−28) | 6.4 (4−25) | 7.3 (1−29) | <.001 |
| Medical complications | 9 (4.5) | 0 | 2 (1.6) | 11 (2.7) | .04 |
| Deaths during the first 24h after surgery (PTE) | 1 | 0 | 0 | 1 | |
| Postoperative blood transfusion | 52 (26.5) | 31 (25.6) | 28 (22.6) | 111 (25.2) | |
| Patients who required more than 4 EC | 4 | 0 | 1 | 5 | |
| Acute kidney failure that required dialysis | 1 | 0 | 0 | 1 | |
| Intestinal pseudo-obstruction | 1 | 0 | 0 | 1 | |
| Acute postoperative delirium | 0 | 0 | 1 | 1 | |
| Hip surgery complications | |||||
| Intraoperative complications | |||||
| Stable diaphyseal femoral fracture (crack) | 1 | 1 | 3 | 5 | |
| Greater trochanter fracture | 0 | 3 | 1 | 4 | |
| Femoral nerve paralysis | 0 | 0 | 1 | 1 | |
| Postoperative complications | |||||
| Periprosthetic femoral fracture | 0 | 1 (0.8) | 2 (1.6) | 3 | |
| Deep infection | 1 | 2 | 0 | 3 | |
| Luxation | 5 (2.6) | 7 (5.8) | 5 (4.0) | 17 (3.9) | .2 |
EC: Erythrocyte Concentrates; PTE: Pulmonary Thromboembolism.
There was one intraoperative stable proximal femur fracture in group 1, another one in group 2 and 3 in group 3. All of them were resolved by wire cerclage, without subsequent complications. There were also 3 non-displaced greater trochanter fractures in group 2 and another one in group 3 which cured without any subsequent intervention. There were 3 postoperative periprosthetic femoral fractures, one in group 2 24 months after surgery which consolidated with conservative treatment, and 2 in group 3 after one month and after 54 months. These required revision of the stem and the implant of a long porous stem with cerclages. There were 17 early luxations in the first 7 months after the operation, 5 (2.6%) in group 1, 7 (5.8%) in group 2 and 5 (4.0%) in group 3. Four luxations required surgery with double mobility cups (one in groups 1 and 2 and 2 in group 3). There were 3 deep infections, one in group 1 and 2 in group 2.
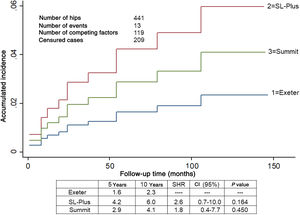
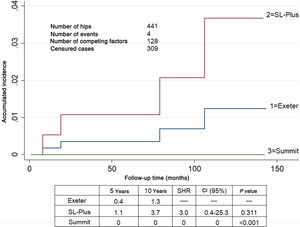
SurvivalOne stem was revised due to aseptic loosening in group 1 as were 2 in group 2. No loose components were found in group 3. A total of 12 hips were revised. The accumulated incidence of revision of one or both components due to any cause, considering death as a competing risk factor, was lower than 6.0% at 5 and 10 years in all 3 groups (Fig. 1). The accumulated incidence of revision due to aseptic loosening, considering death as a competing risk factor, was significantly lower in group 3 (Fig. 2).
Accumulated incidence of revision surgery in one or both prosthetic components due to any cause, taking mortality into account as a competing risk. Estimated at different intervals of 5 and 10 years in 441 hips. The Exeter group is taken as the reference.
CI: Confidence Interval; SHR: Subdistribution Hazard Ratio.
Accumulated incidence of revision surgery due to the loosening of one or both prosthetic components for any cause, taking accumulated mortality into account as a competing risk. Estimated at different intervals of 5 and 10 years in 441 hips. The Exeter group is taken as the reference.
CI: Confidence Interval; SHR: Subdistribution Hazard Ratio.
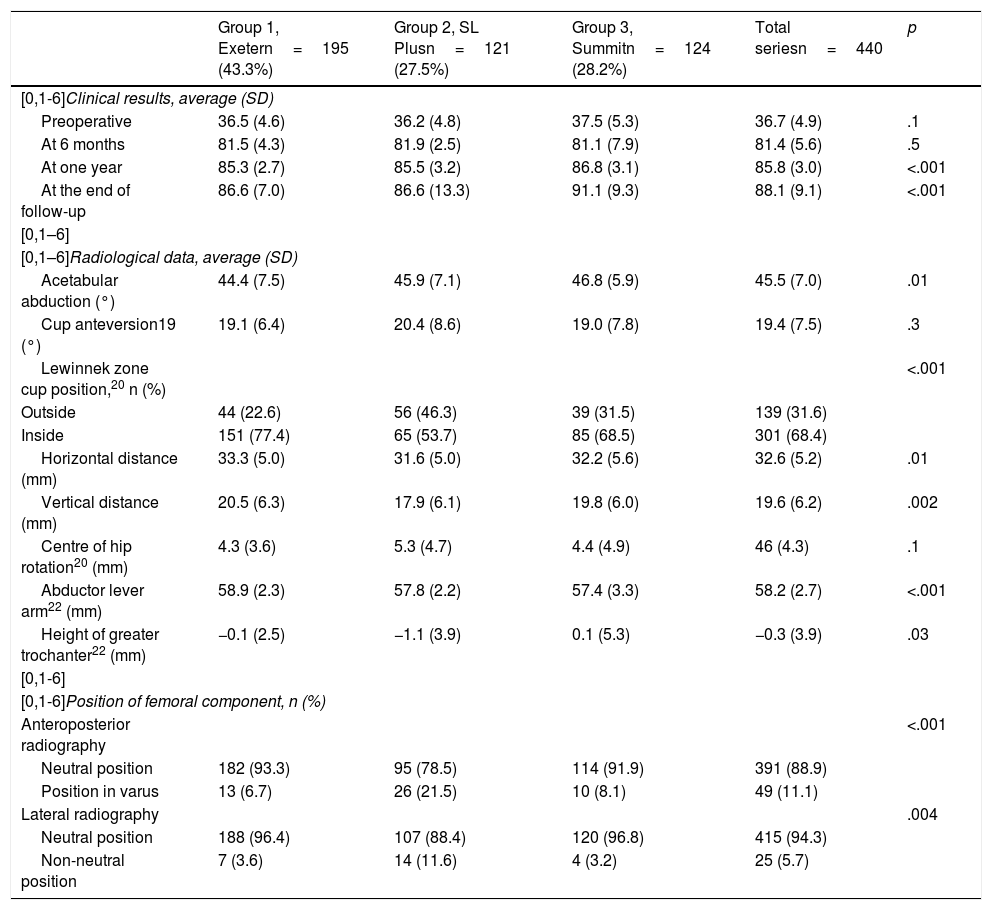
On the Harris scale at the end of the follow-up period, the patients in group 3 had a better average score (91.1) than the patients in groups 1 and 2 (86.6 in both cases) (P<.001). Respecting the radiological analysis, the postoperative position of the acetabular component was better in group 1 for the majority of the parameters studied, as was the case for the frequency of stems implanted in a neutral position, which was higher in groups 1 and 3 than it was in group 2 (Table 3). Postoperative X-ray images of cemented group 1 showed a thick layer of cement (more than 1cm) around the cup in 33 hips (16.8%), in 15 in the 3 De Lee and Charnley zones, in 11 in zones 2 and 3, in 4 in zone 2 and in 3 in zone 3. They showed extrusion of the periacetabular cement from the mid wall in 7 hips (3.6%). Around the femoral stem, 56 hips (28.6%) showed a layer of cement of less than 5mm in the Gruen zones. There were no changes of position of the acetabular components or radiotransparent lines larger than 2mm. On the femoral side, signs of loosening or sinking were only detected in the above-mentioned cases that required revision.
Clinical results on the Harris Hip scale and postoperative radiological results for the acetabular and femoral components.
| Group 1, Exetern=195 (43.3%) | Group 2, SL Plusn=121 (27.5%) | Group 3, Summitn=124 (28.2%) | Total seriesn=440 | p | |
|---|---|---|---|---|---|
| [0,1-6]Clinical results, average (SD) | |||||
| Preoperative | 36.5 (4.6) | 36.2 (4.8) | 37.5 (5.3) | 36.7 (4.9) | .1 |
| At 6 months | 81.5 (4.3) | 81.9 (2.5) | 81.1 (7.9) | 81.4 (5.6) | .5 |
| At one year | 85.3 (2.7) | 85.5 (3.2) | 86.8 (3.1) | 85.8 (3.0) | <.001 |
| At the end of follow-up | 86.6 (7.0) | 86.6 (13.3) | 91.1 (9.3) | 88.1 (9.1) | <.001 |
| [0,1–6] | |||||
| [0,1–6]Radiological data, average (SD) | |||||
| Acetabular abduction (°) | 44.4 (7.5) | 45.9 (7.1) | 46.8 (5.9) | 45.5 (7.0) | .01 |
| Cup anteversion19 (°) | 19.1 (6.4) | 20.4 (8.6) | 19.0 (7.8) | 19.4 (7.5) | .3 |
| Lewinnek zone cup position,20 n (%) | <.001 | ||||
| Outside | 44 (22.6) | 56 (46.3) | 39 (31.5) | 139 (31.6) | |
| Inside | 151 (77.4) | 65 (53.7) | 85 (68.5) | 301 (68.4) | |
| Horizontal distance (mm) | 33.3 (5.0) | 31.6 (5.0) | 32.2 (5.6) | 32.6 (5.2) | .01 |
| Vertical distance (mm) | 20.5 (6.3) | 17.9 (6.1) | 19.8 (6.0) | 19.6 (6.2) | .002 |
| Centre of hip rotation20 (mm) | 4.3 (3.6) | 5.3 (4.7) | 4.4 (4.9) | 46 (4.3) | .1 |
| Abductor lever arm22 (mm) | 58.9 (2.3) | 57.8 (2.2) | 57.4 (3.3) | 58.2 (2.7) | <.001 |
| Height of greater trochanter22 (mm) | −0.1 (2.5) | −1.1 (3.9) | 0.1 (5.3) | −0.3 (3.9) | .03 |
| [0,1-6] | |||||
| [0,1-6]Position of femoral component, n (%) | |||||
| Anteroposterior radiography | <.001 | ||||
| Neutral position | 182 (93.3) | 95 (78.5) | 114 (91.9) | 391 (88.9) | |
| Position in varus | 13 (6.7) | 26 (21.5) | 10 (8.1) | 49 (11.1) | |
| Lateral radiography | .004 | ||||
| Neutral position | 188 (96.4) | 107 (88.4) | 120 (96.8) | 415 (94.3) | |
| Non-neutral position | 7 (3.6) | 14 (11.6) | 4 (3.2) | 25 (5.7) | |
The total number of hips is 440, as the patient who died in the first 6h after surgery is not included.
SD: Standard Deviation.
The increase in life expectancy correlates with an increase in the demand for primary THP. In our country, one third of the patients operated for THP are over the age of 75 years, a decisive variable for the frequency of this surgical procedure.26 The greater risk of complications due to higher associated preoperative comorbidity, the increase in the indication for cementless THP, in spite of the lack of evidence for this, and problems in follow-up over time to analyse the results are factors which hinder clinical studies in this population.4,6,9 In our study we find that implanting cemented as well as cementless THP are procedures with acceptable risks, although certain differences should be taken into account.
The number of medical complications was similar in both of the groups which were compared. Although there are different comorbidity indexes, the ASA system was used in this study, which facilitates the classification of risk.12 In this series only ASA type II and III patients were accepted for surgery. Ondeck et al. state that the ASA system is more useful to predict the appearance of adverse effects in octogenarians than more complex systems such as the modified Charlson Comorbidity Index and the modified Frailty Index.27 Although the patients in the cemented THP group have an older average age, were hospitalised for longer and had more comorbidities, the total number of medical complications was similar. The development of modern recover protocols may have contributed to the fall in the incidence of adverse events in these patients.4 It is more important to evaluate preoperative anaemia in octogenarian patients because it occurs more often and they have a higher risk of transfusion than younger pacientes.3 The overall requirement for erythrocyte concentrate transfusions amounted to 25%; nevertheless, although in our hospital we currently use multimode protocols to save blood, including the use of tranexamic acid, this was not normal practise during the period of the study because of the great variability and controversy existing in this type of population.28
It should be underlined that the incidence of complications associated with intra- and postoperative periprosthetic fractures was higher in the groups of patients with uncemented THP, in spite of the higher frequency of Dorr femoral C type in the cemented group. This finding was also detected in studies of national registers.6,29 Similarly, in the United States, where uncemented THPs are used more widely than in Europe, the same findings have recently been observed.30 The results of some biomechanical studies have confirmed that osteoporotic bones are more fragile and susceptible to fractures than bones with a higher bone density, and the protective effect of cement has been observed in terms of the load which is necessary to cause failure.31 Luxation was similar in the different groups, although a more widespread use of large diameter femoral heads or double mobility cups may have contributed to a lower rate of this complication.32,33 Although the clinical results were better in group 3, the above-mentioned preoperative differences, the surgical approach and the higher number of trochanter fractures in group 2 may affect these findings.34 Regarding the radiological analysis, we found better data in the group OF patients with a cemented THP in terms of the position of the components. The choice of implant was based on the preferences of the surgeon and their everyday clinical routine, and this may influence the results depending on their experience and surgical technique.6 Likewise, we have not compared the quality of cementation, as 2 different types of fixation were used, and we only included major defects in technique.
The accumulated incidence of revision of one or both components due to any cause, considering death as a competing risk factor, was less in the cemented group. However, given the number of available hips, there were no significant differences here. Kaplan-Meier survival analysis overestimates values when mortality is high, due to the involvement of this factor as a competing risk. In our study survival analysis respecting the probability of undergoing revision surgery or loosening was carried out by analysing accumulated incidence and taking this factor into account, as Lampropoulou-Adamidou et al. recommend.9 In studies with fewer patients than those undertaken using national registries, possible competing risk factors become more important.8 Some studies of registries therefore find a higher risk of revision surgery for uncemented THP in elderly pacientes.29 Although uncemented fixation is often optimum in patients with osteoporotic bones,35 it is important to know both techniques so that risks can be reduced.6,30
This study is neither prospective nor randomised, so that preoperative differences between the groups may have influenced its results. This is a general series in a tertiary hospital, and surgical technique may vary between different surgeons. This may explain some of the differences between groups. These results reflect our experience, which perhaps cannot be extrapolated to other cemented and cementless designs or to other surgeons. The exclusion of patients with severe or tumoral bone disease may also have influenced the results. The chief limitation of these studies on the results of THP in patients within this population is the short follow-up due to their advanced age, giving rise to a large number of hips that are lost due to causes unconnected with surgery. The strengths of this study are its comparative sample, including radiological analysis, of more than 400 cemented and uncemented THP in octogenarian patients, the evaluation of associated comorbidities and the survival analysis with evaluation of mortality as a competing risk factor.
ConclusionsAn appropriate selection of octogenarian patients who will be operated for THP and evaluating their comorbidities will lead to an acceptable number of complications and reasonable duration of hospitalisation. Surgeons must inform patients and their families of the increased risk of morbimortality before the operation. Although the results in our study were generally good with both types of fixation, there was no periprosthetic femoral fracture in the cemented group, in spite of the fact that the bones of more patients in this group were osteoporotic than was the case in the uncemented group.
Level of evidenceLevel of evidence IV.
FinancingThis research received no specific support from public, commercial or not-for-profit bodies.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: García Rey E, Cruz Pardos A, Ortega Chamarro J. Mortalidad como factor de riesgo de competencia en el análisis de supervivencia de los resultados del tipo de fijación de la prótesis total de cadera en pacientes octogenarios. Rev Esp Cir Ortop Traumatol. 2021;65:99–107.