To evaluate whether augmentation grafts using autologous fascia lata improve functional results for rotator cuff repairs and reduce the retear rate compared to those without augmentation.
Material and methodsThis is a prospective evaluation comprising 20 patients with a complete symptomatic rotator cuff tear. The operations were carried out from a superior approach performing a total cuff repair, for 10 patients we used a suture augmented with an autologous graft taken from their own fascia lata while unaugmented sutures were used for the other 10 patients. The follow-up period lasted for one year post-intervention. We measured variables for tear type, functionality and pain, both baseline and at 6 and 12-month follow ups. We evaluated retear incidence in each group as well as each group's pain and functionality response.
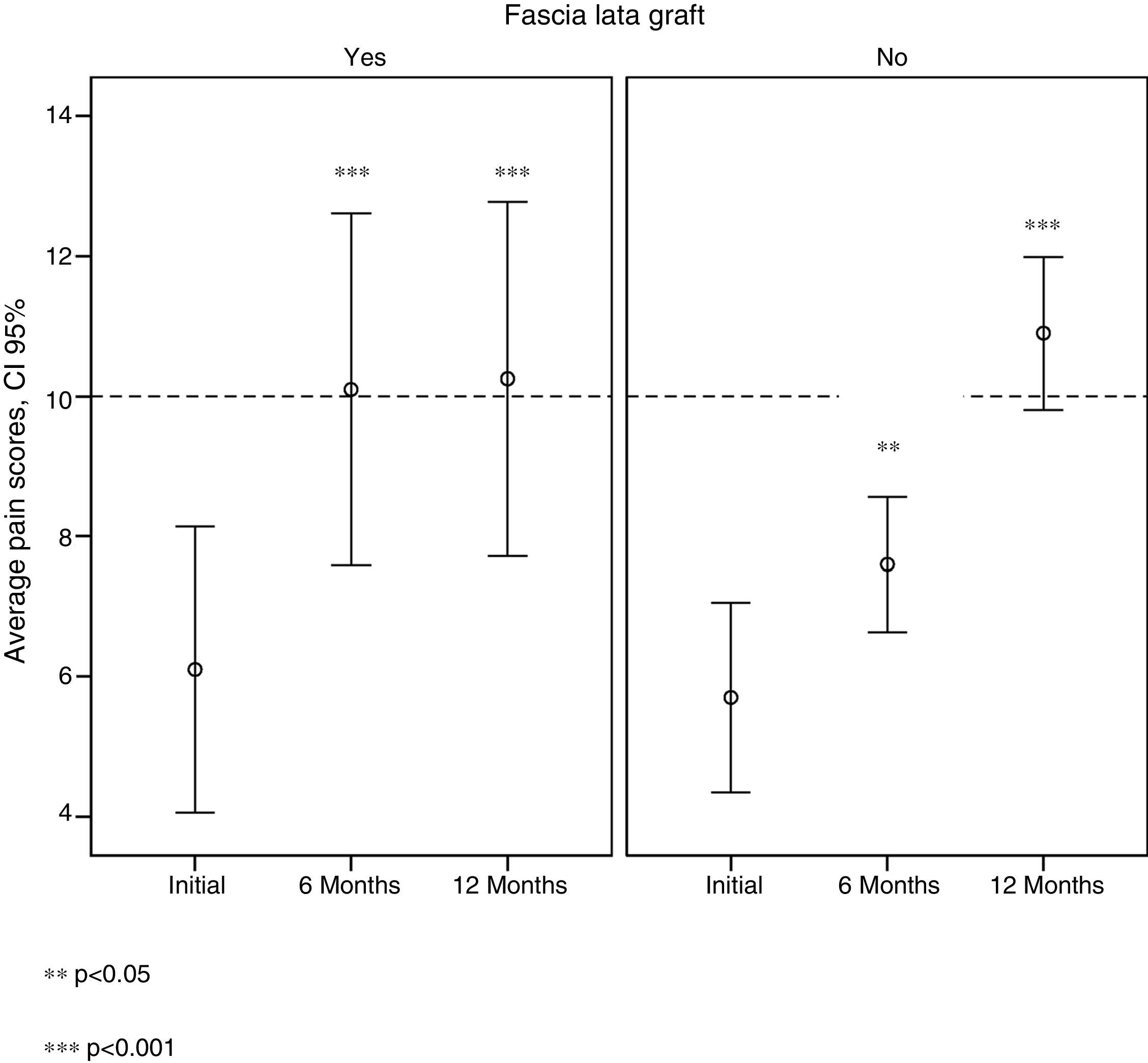
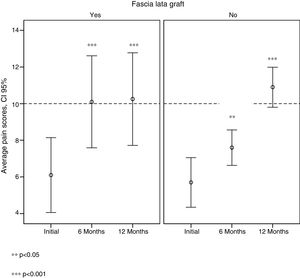
ResultsThe improved pain levels in the non-graft group evolved gradually over time. Conversely, in the group with the augmentation grafts, average Constant–Murley shoulder outcome scores at six months were already above 10 and were maintained at 12 months. One retear occurred in the graft group and 2 in the group without grafts, thus presenting no significant differences. There were no significant changes in pain and function values at the one year follow up in either group.
ConclusionOur preliminary results regarding rotator cuff augmentation surgery with autologous fascia lata showed a significant improvement in pain levels after 6 months compared to the patients with no augmentation, who required 12 months to reach the same values. After a year of follow up, there were no differences between the mean Constant and pain scores in either intervention group The number of retears in the non-graft group was greater than that in the group with grafts although the difference was not significant.
Evaluar si el injerto de refuerzo con fascia lata autógena mejora los resultados funcionales en las reparaciones del manguito rotador y si disminuye la tasa de rerroturas en comparación con las realizadas sin refuerzo.
Material y métodosEstudio prospectivo sobre una muestra piloto de 20 pacientes con una rotura completa sintomática del manguito de los rotadores. Los pacientes fueron intervenidos mediante un abordaje superior, realizándose una reparación completa sin tensión de la rotura mediante sutura reforzada con injerto autógeno procedente de fascia lata del propio paciente a 10 de ellos y sutura sin refuerzo a los otros 10. El tiempo de seguimiento fue de un año desde la intervención. Se han medido variables sobre la tipología de la lesión, la funcionalidad y el dolor mediante la escala de Constant-Murley, tanto basalmente como a los 6 y 12 meses de seguimiento. Se realizó un análisis descriptivo de todas las variables en ambos grupos de intervención y un análisis de normalidad. Se evaluó la incidencia de rerroturas al año en ambos grupos.
ResultadosHay una mejoría significativa de las puntuaciones medias de Constant-Murley y del dolor al año de seguimiento en ambos grupos de tratamiento respecto al inicio, pero sin cambios significativos entre los valores de dolor y función al año de seguimiento en ambos grupos de intervención. La mejoría del dolor en el grupo de no injertados se produce paulatinamente a lo largo del tiempo, mientras que en el grupo de injertados a los 6 meses ya se alcanzan valores medios por encima de 10 de la escala de Constant-Murley, que se mantienen hasta los 12 meses. Se produjo una rerrotura en el grupo con injerto y 2 en el grupo sin injerto, no apareciendo diferencias significativas.
ConclusiónNuestros resultados preliminares de la cirugía de refuerzo del maguito rotador con fascia lata autógena muestran una mejoría significativa del dolor a los 6 meses, que se mantiene en el tiempo respecto a los pacientes sin refuerzo quienes requirieron 12 meses para obtener los mismos valores y a pesar de no hallar diferencias significativas respecto a función ni cicatrización, los pacientes con refuerzo de fascia lata se benefician de una más rápida mejoría del dolor. El número de reroturas en el grupo sin injerto fue mayor que en el grupo con injerto, aunque la diferencia no fue significativa.
Lesions of the rotator cuff are one of the most common causes of shoulder pain and incapacity of the upper limbs. The incidence of this condition increases with age, and it affects more than 40% of individuals over the age of 60 years old.1–3 Although it consumes an important proportion of healthcare resources4 there is still debate about how it should be managed.3
In spite of current understanding of this disease and technical progress in the surgical treatment of it, there is a high rate of repeat tears, which is estimated to stand at from 20% to 90%.5–13 These repeat tears are associated with different parameters, most especially age at the time of surgery,9,14–16 tendon quality5 or the size of the initial lesion.5,17 The majority of repeat tears occur in the first 12 weeks after surgery, so that we keep some type of protection of the repair in place during this time.18 It must not be forgotten that the results of revision repairs of the cuff are inferior to those of the primary repair.19–22
This high failure rate associated with cuff repair has led surgeons to explore alternatives, as there is a need to introduce strategies that improve the repair, adding mechanical reinforcement as well as a biological improvement in the potential cure of the tendon. We are therefore able to observe that although surgical technique has advanced considerably in recent decades,23 there is now an increase in the number of papers expressing concern for the biological scarring applied in these lesions.
Theoretically the ideal implant to reinforce the rotator cuff should combine the characteristics of biological and synthetic implants. It would function as an inductive template to help tissue regeneration and be strong enough to protect the suture during the first weeks after surgery while tissue repair takes place.24
The use of allografts has been described as a cuff repair augmentation device by Neviaser et al.,25 Ito and Morioka,26 Moore et al.,27 Rotini et al.,28 Barber et al.,29 Bond et al.,30 Wong et al.31 and Gupta et al.32 They prove that allografts of this type may aid curing of the tendon.
Grafts made from the extracellular matrix have now been approved by the FDA and are commercialised as medical devices for the repair of the rotator cuff in human beings.
This is the first prospective study undertaken on reinforcing the primary suture of the rotator cuff with autologous fascia lata, although descriptions of other autologous grafts for augmentation have been found in the literature. These include studies by Scheibel et al.,33 with augmentation by autologous periostium, Sano et al.,34 who used the long part of the biceps to repair massive cuff lesions, or Bektaser et al.,35 who used the coracoacromial ligament. Nevertheless, to date the degree to which autologous grafts are successful has not been sufficiently proven, and nor are there prospective clinical studies that demonstrate the efficacy of autologous reinforcements in terms of a reduction in the repeat tear rate. However, there are laboratory studies which show that fascia lata has similar biochemical and structural characteristics to those of the human supraspinatus tendon and the canine infraspinatus tendon,36 with similar mechanical properties showing that this could be used as a means of augmentation.37
Given the lack of studies on autologous augmentation in the repair of human rotator cuff and the importance of seeking new methods that reduce the number of repeat tears, we designed this study to evaluate whether augmentation surgery with autologous fascia lata reduces the repeat tear rate in cuff repairs and improves functional results in comparison with unaugmented repairs.
Material and methodsA prospective clinical study was conducted of a pilot sample of 20 patients to evaluate the incidence of repeat years and the efficacy of surgery with fascia lata augmentation graft vs. surgery without augmentation.
The subjects included in the study were patients admitted to our hospital sequentially from January to November 2013 with complete symptomatic tear of the rotator cuff and who fulfilled the following inclusion criteria: complete symptomatic tear of the rotator cuff of one shoulder that involved the supraspinatus (SS) tendon completely, or the SS and infraspinatus (IS) tendons completely or the IS tendon completely or the SS tendon completely and the IS or subscapular tendon partially; aged from 40 to 70 years old at the time they first consulted; fatty degeneration of the SS and IS ≤50%, according to Goutallier's classification; muscular atrophy in stage 1 or 2 of Thomazeau's classification; complete and non-acute tears (non-traumatic >3 months symptoms); accepted taking part in the study by giving consent.
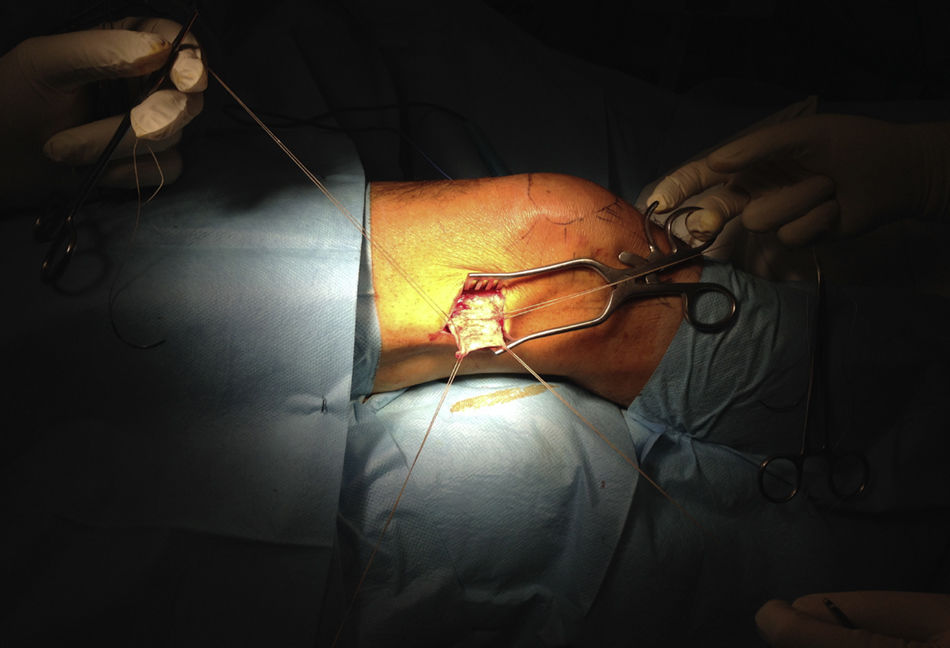
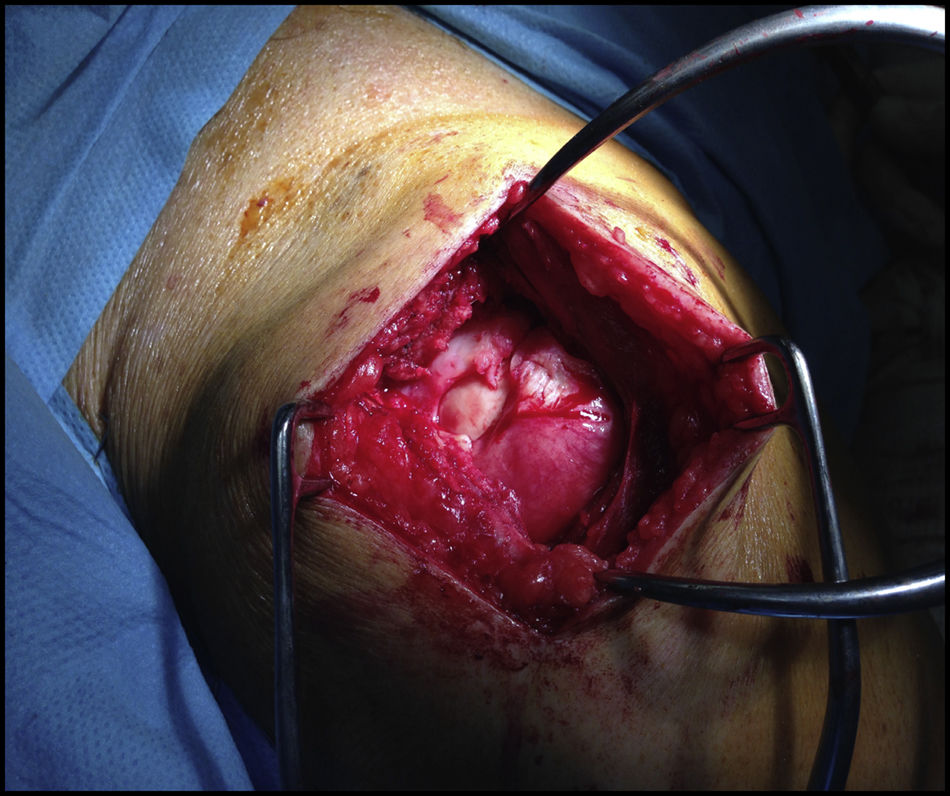
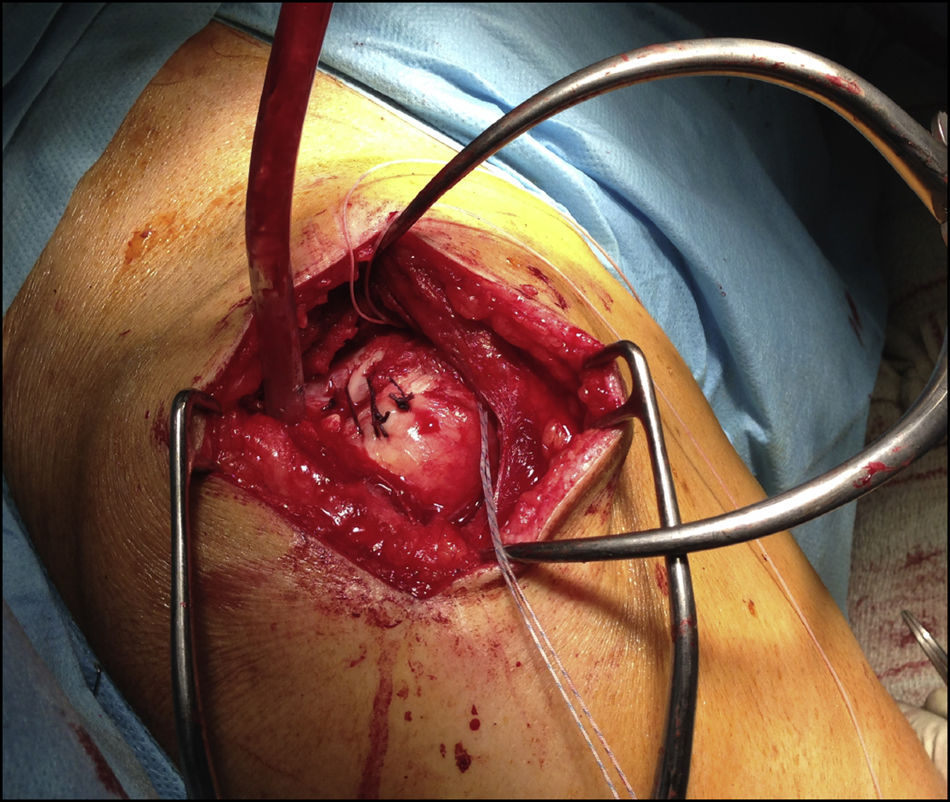
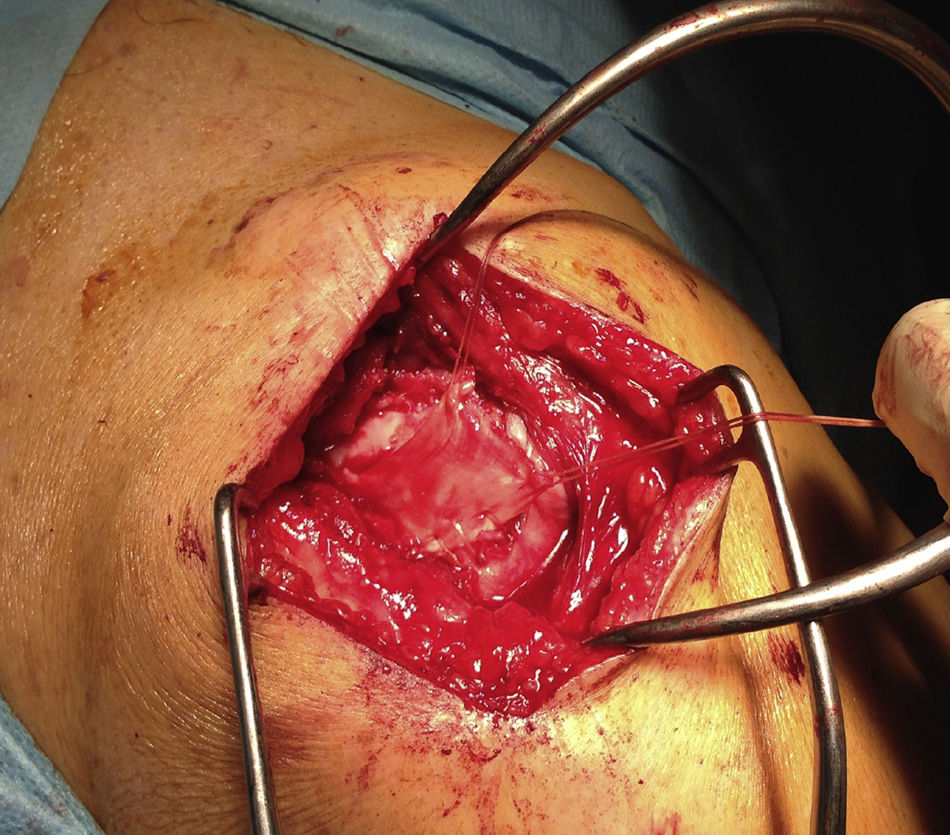
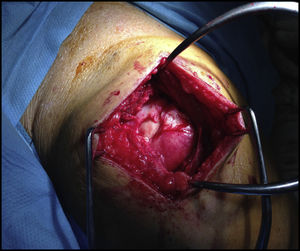
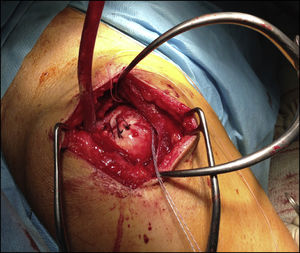
The patients were distributed in 2 groups according to the type of surgical procedure, which was performed by the same surgeon. In the first group of 10 patients surgery consisted of repair of the tear using a superior approach, with complete closure without tension, reinforced with an autologous graft of fascia lata taken from the patient (Figs. 1–4). In 10 other patients the suture was performed using the same technique without augmentation. The tendon was repaired using a suture with number 5 metal anchorages, without using a double row of suture in any case, after curettage of the bed with a K needle and without acromioplasty, except in one case where we found a type 3 acromion. We found 12 “U” shaped tears (6 in each group) and 8 “L” shaped tears (4 in each group). The fascia lata was taken from the distal zone approximately 15cm from the knee joint interline, and in the cases where it was used as augmentation, it was placed over the tendon repair and sutured with Vicryl® double zero thread. A one-year follow-up took place after the date of surgery.
Variables associated with the lesion were recorded at the start of the study: the initial number of torn tendons, the type of initial tear, initial retraction, initial fatty degeneration of the SS and IS, atrophy of the SS and IS. Pain and functionality of the affected shoulder were measured using the Constant–Murley test initially and at 6 and 12 months of follow-up. The response variable was the appearance of a repeat tear after one year (yes/no).
MR imaging was used to detect whether a repeat tear had occurred 12 months after the surgical procedure; this evaluation was performed by the same radiologist, differentiating between repeat tear at the level of the repair and/or at a different level of the tendon.
All of the subjects underwent the same rehabilitation program which was set by the protocol published by the GANCHO38 group. This is a personalised plan for shoulder problems and a modification of Rockwood Orthotherapy.
A descriptive analysis of all of the variables was undertaken using frequency tables for qualitative variables and statistical calculation for the quantitative variables, including the minimum, the maximum, the average value and standard deviation.
The chi-squared test was used to analyse the homogeneity of the qualitative explanative variables in both treatment groups. Student's t-test was used to compare the average values of the quantitative variables in both groups, after checking the normality of each group using the Kolmogorov–Smirnov test.
The chi-squared test was used to compare the incidence of repeat tears in each group after a one year follow-up. Dichotomised pain and functionality were evaluated in each treatment group using the chi-squared test. Pain and functionality were also analysed quantitatively in each treatment group using Student's t-test after checking normality.
The chi-squared test was used to evaluate the qualitative variables of the patients with repeat tears after one year. Mann–Whitney's U test was used for the quantitative variables.
Wilcoxon's test was used to compare the basal average scores after one year for pain and functionality.
Tests were accepted as statistically significant at 95% confidence level. The SPSS v.18 statistical package was used for analysis.
Ethical considerationsNational and international guidelines for biomedical research in human beings were followed during this study (the Ethical Code and the Helsinki Declaration). The legal regulations governing patient data confidentiality were also complied with (Organic Law 15/1999, of 13 December, on Personal Data Protection) according to the body for the control of compliance with the regulations of the Spanish Data Protection Agency.
Results10 patients in each study group were evaluated. There were 12 women and 8 men aged from 50 to 64 years old, with an average age of 58.5 years old.
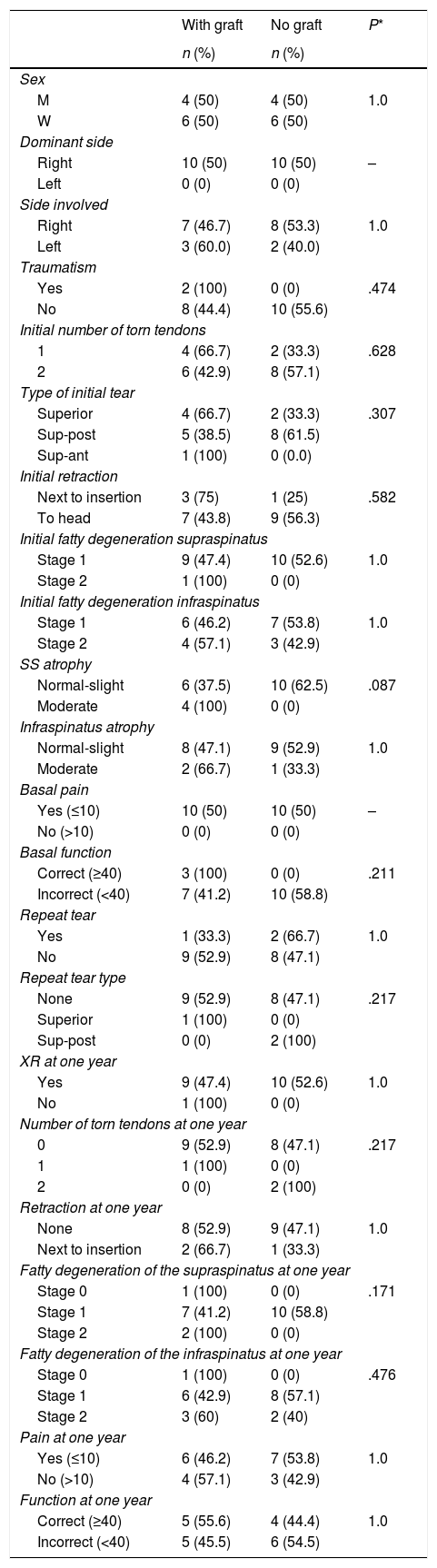
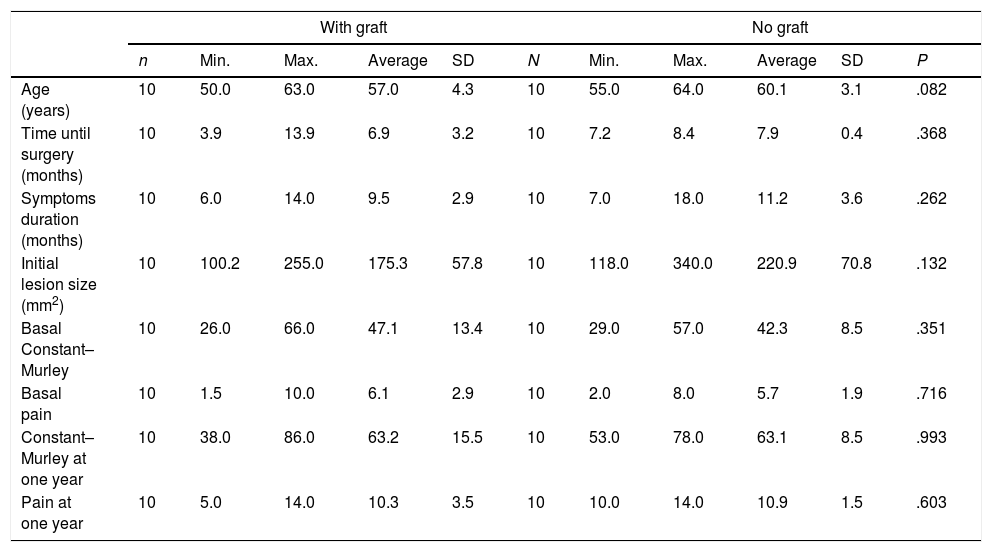
Both study groups are homogeneous in terms of age, sex, dominant and affected sides, trauma, initial number of tendons torn, type of initial tear, initial retraction, initial fatty degeneration of the SS and IS, atrophy of the SS a IS, time until surgery, the duration of symptoms, initial size of lesion, pain, functioning and basal Constant–Murley scores (Tables 1 and 2).
Number and percentage of patients with and without a fascia lata graft in each level of the explanative variables.
| With graft | No graft | P* | |
|---|---|---|---|
| n (%) | n (%) | ||
| Sex | |||
| M | 4 (50) | 4 (50) | 1.0 |
| W | 6 (50) | 6 (50) | |
| Dominant side | |||
| Right | 10 (50) | 10 (50) | – |
| Left | 0 (0) | 0 (0) | |
| Side involved | |||
| Right | 7 (46.7) | 8 (53.3) | 1.0 |
| Left | 3 (60.0) | 2 (40.0) | |
| Traumatism | |||
| Yes | 2 (100) | 0 (0) | .474 |
| No | 8 (44.4) | 10 (55.6) | |
| Initial number of torn tendons | |||
| 1 | 4 (66.7) | 2 (33.3) | .628 |
| 2 | 6 (42.9) | 8 (57.1) | |
| Type of initial tear | |||
| Superior | 4 (66.7) | 2 (33.3) | .307 |
| Sup-post | 5 (38.5) | 8 (61.5) | |
| Sup-ant | 1 (100) | 0 (0.0) | |
| Initial retraction | |||
| Next to insertion | 3 (75) | 1 (25) | .582 |
| To head | 7 (43.8) | 9 (56.3) | |
| Initial fatty degeneration supraspinatus | |||
| Stage 1 | 9 (47.4) | 10 (52.6) | 1.0 |
| Stage 2 | 1 (100) | 0 (0) | |
| Initial fatty degeneration infraspinatus | |||
| Stage 1 | 6 (46.2) | 7 (53.8) | 1.0 |
| Stage 2 | 4 (57.1) | 3 (42.9) | |
| SS atrophy | |||
| Normal-slight | 6 (37.5) | 10 (62.5) | .087 |
| Moderate | 4 (100) | 0 (0) | |
| Infraspinatus atrophy | |||
| Normal-slight | 8 (47.1) | 9 (52.9) | 1.0 |
| Moderate | 2 (66.7) | 1 (33.3) | |
| Basal pain | |||
| Yes (≤10) | 10 (50) | 10 (50) | – |
| No (>10) | 0 (0) | 0 (0) | |
| Basal function | |||
| Correct (≥40) | 3 (100) | 0 (0) | .211 |
| Incorrect (<40) | 7 (41.2) | 10 (58.8) | |
| Repeat tear | |||
| Yes | 1 (33.3) | 2 (66.7) | 1.0 |
| No | 9 (52.9) | 8 (47.1) | |
| Repeat tear type | |||
| None | 9 (52.9) | 8 (47.1) | .217 |
| Superior | 1 (100) | 0 (0) | |
| Sup-post | 0 (0) | 2 (100) | |
| XR at one year | |||
| Yes | 9 (47.4) | 10 (52.6) | 1.0 |
| No | 1 (100) | 0 (0) | |
| Number of torn tendons at one year | |||
| 0 | 9 (52.9) | 8 (47.1) | .217 |
| 1 | 1 (100) | 0 (0) | |
| 2 | 0 (0) | 2 (100) | |
| Retraction at one year | |||
| None | 8 (52.9) | 9 (47.1) | 1.0 |
| Next to insertion | 2 (66.7) | 1 (33.3) | |
| Fatty degeneration of the supraspinatus at one year | |||
| Stage 0 | 1 (100) | 0 (0) | .171 |
| Stage 1 | 7 (41.2) | 10 (58.8) | |
| Stage 2 | 2 (100) | 0 (0) | |
| Fatty degeneration of the infraspinatus at one year | |||
| Stage 0 | 1 (100) | 0 (0) | .476 |
| Stage 1 | 6 (42.9) | 8 (57.1) | |
| Stage 2 | 3 (60) | 2 (40) | |
| Pain at one year | |||
| Yes (≤10) | 6 (46.2) | 7 (53.8) | 1.0 |
| No (>10) | 4 (57.1) | 3 (42.9) | |
| Function at one year | |||
| Correct (≥40) | 5 (55.6) | 4 (44.4) | 1.0 |
| Incorrect (<40) | 5 (45.5) | 6 (54.5) | |
P estimated by the chi-squared test.
Inconclusive chi-squared test due to lack of data, results are a guideline.
95% significant tests are in bold print.
Number, minimum and maximum values, averages and standard deviations of the main variables in both groups.
| With graft | No graft | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Min. | Max. | Average | SD | N | Min. | Max. | Average | SD | P | |
| Age (years) | 10 | 50.0 | 63.0 | 57.0 | 4.3 | 10 | 55.0 | 64.0 | 60.1 | 3.1 | .082 |
| Time until surgery (months) | 10 | 3.9 | 13.9 | 6.9 | 3.2 | 10 | 7.2 | 8.4 | 7.9 | 0.4 | .368 |
| Symptoms duration (months) | 10 | 6.0 | 14.0 | 9.5 | 2.9 | 10 | 7.0 | 18.0 | 11.2 | 3.6 | .262 |
| Initial lesion size (mm2) | 10 | 100.2 | 255.0 | 175.3 | 57.8 | 10 | 118.0 | 340.0 | 220.9 | 70.8 | .132 |
| Basal Constant–Murley | 10 | 26.0 | 66.0 | 47.1 | 13.4 | 10 | 29.0 | 57.0 | 42.3 | 8.5 | .351 |
| Basal pain | 10 | 1.5 | 10.0 | 6.1 | 2.9 | 10 | 2.0 | 8.0 | 5.7 | 1.9 | .716 |
| Constant–Murley at one year | 10 | 38.0 | 86.0 | 63.2 | 15.5 | 10 | 53.0 | 78.0 | 63.1 | 8.5 | .993 |
| Pain at one year | 10 | 5.0 | 14.0 | 10.3 | 3.5 | 10 | 10.0 | 14.0 | 10.9 | 1.5 | .603 |
P estimated by Student's t-test for comparing the averages in each group: all of the variables are distributed as normal in each group (Kolmogorov–Smirnov test).
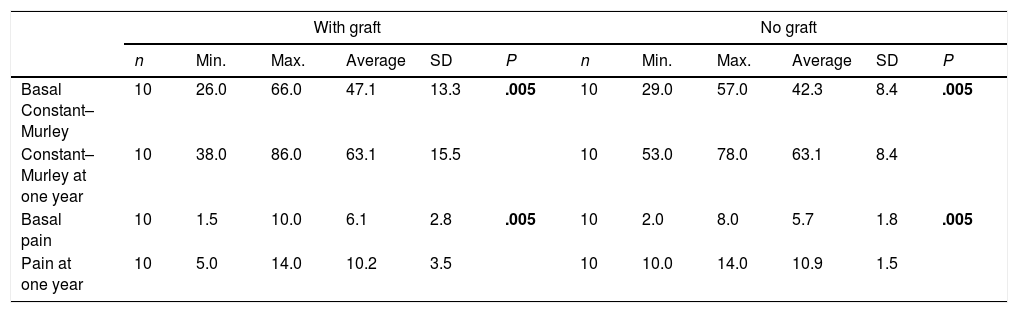
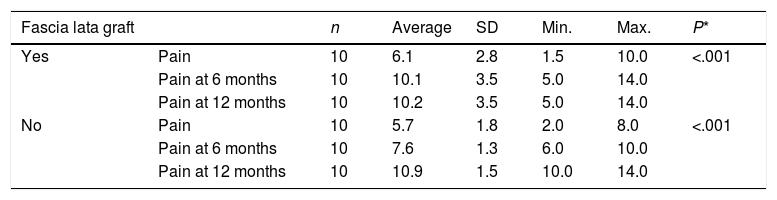
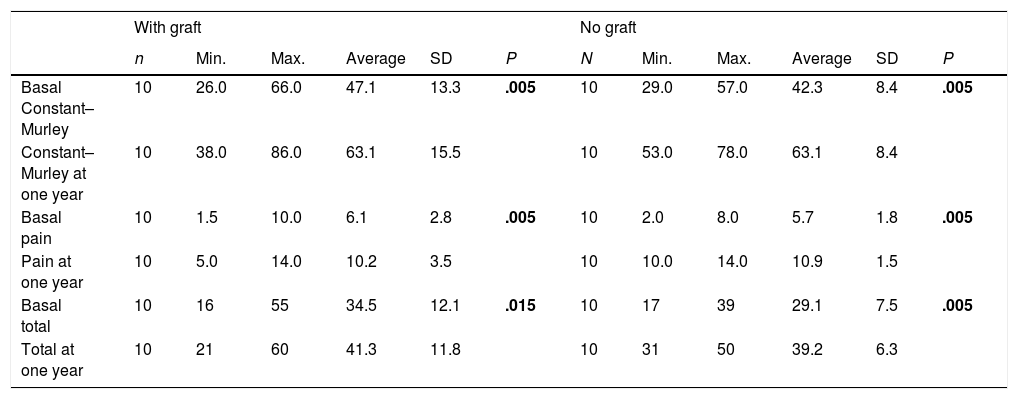
Respecting the clinical symptoms, we analysed the average Constant–Murley scores and basal pain levels at 6 months and 12 months. We found after both periods that a significant increase had occurred in both groups in comparison with their initial situation. There were no significant differences between both groups studied in terms of their average Constant–Murley scores and pain (Table 3).
Number, minimum and maximum values, averages and standard deviations of the basal Constant–Murley score and basal pain in both treatment groups and after one year.
| With graft | No graft | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Min. | Max. | Average | SD | P | n | Min. | Max. | Average | SD | P | |
| Basal Constant–Murley | 10 | 26.0 | 66.0 | 47.1 | 13.3 | .005 | 10 | 29.0 | 57.0 | 42.3 | 8.4 | .005 |
| Constant–Murley at one year | 10 | 38.0 | 86.0 | 63.1 | 15.5 | 10 | 53.0 | 78.0 | 63.1 | 8.4 | ||
| Basal pain | 10 | 1.5 | 10.0 | 6.1 | 2.8 | .005 | 10 | 2.0 | 8.0 | 5.7 | 1.8 | .005 |
| Pain at one year | 10 | 5.0 | 14.0 | 10.2 | 3.5 | 10 | 10.0 | 14.0 | 10.9 | 1.5 | ||
P estimated by Wilcoxon's test for the comparison of associated averages in each treatment group.
95% significant tests are in bold print.
In the graft group the improvement in pain at 6 months is highly significant (P<.001), reaching average values higher than 10. In the non-graft group we found an increase with values of P<.05, obtaining average values under 8 (Table 4). At 12 months both groups showed a highly significant increase in their pain scores (P<.001) in comparison with their initial scores (Table 4).
Pain scores at 6 and 12 months in both groups.
| Fascia lata graft | n | Average | SD | Min. | Max. | P* | |
|---|---|---|---|---|---|---|---|
| Yes | Pain | 10 | 6.1 | 2.8 | 1.5 | 10.0 | <.001 |
| Pain at 6 months | 10 | 10.1 | 3.5 | 5.0 | 14.0 | ||
| Pain at 12 months | 10 | 10.2 | 3.5 | 5.0 | 14.0 | ||
| No | Pain | 10 | 5.7 | 1.8 | 2.0 | 8.0 | <.001 |
| Pain at 6 months | 10 | 7.6 | 1.3 | 6.0 | 10.0 | ||
| Pain at 12 months | 10 | 10.9 | 1.5 | 10.0 | 14.0 |
Friedman's test, P<.001.
These results show that although at 12 months both groups have similar scores for pain, the non-graft group took longer to reach the values attained by the graft group after 6 months (Fig. 5).
If patient functioning in terms of mobility is evaluated (flexion+external rotation+internal rotation+abduction) together with everyday life activities in both groups, the graft group is found to have a better response (an average of 41.3) in comparison with the non-graft group (an average of 39.2) (Table 5).
Number, minimum and maximum values, averages and standard deviations of the basal Constant–Murley score, pain and total in both treatment groups and after one year.
| With graft | No graft | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Min. | Max. | Average | SD | P | N | Min. | Max. | Average | SD | P | |
| Basal Constant–Murley | 10 | 26.0 | 66.0 | 47.1 | 13.3 | .005 | 10 | 29.0 | 57.0 | 42.3 | 8.4 | .005 |
| Constant–Murley at one year | 10 | 38.0 | 86.0 | 63.1 | 15.5 | 10 | 53.0 | 78.0 | 63.1 | 8.4 | ||
| Basal pain | 10 | 1.5 | 10.0 | 6.1 | 2.8 | .005 | 10 | 2.0 | 8.0 | 5.7 | 1.8 | .005 |
| Pain at one year | 10 | 5.0 | 14.0 | 10.2 | 3.5 | 10 | 10.0 | 14.0 | 10.9 | 1.5 | ||
| Basal total | 10 | 16 | 55 | 34.5 | 12.1 | .015 | 10 | 17 | 39 | 29.1 | 7.5 | .005 |
| Total at one year | 10 | 21 | 60 | 41.3 | 11.8 | 10 | 31 | 50 | 39.2 | 6.3 | ||
P estimated by Wilcoxon's test for associated averages in each treatment group.
TOTAL: flexion+external rotation+internal rotation+abduction.
There was one repeat tear in the graft group and 2 in the non-graft group, although there were no significant differences. The proportion and type of repeat tear after one year were not significantly different in both groups (Table 1). There were no differences between the proportions of number of tendons torn, retraction, fatty degeneration of the SS and IS, pain and functioning after one year of follow-up in both groups (Table 1).
DiscussionIn this work the results show a functional improvement in the patients treated with autologous fascia lata augmentation after one year of follow-up, although there are no differences in comparison with the control group. In the graft group the improvement in pain after 6 months is highly significant (P<.001). There is a reduction in the rate of repeat tear in the group treated with an autologous fascia lata graft, without any significant differences between both groups in the proportion and type of repeat tears after one year of follow-up.
Although the structural strengthening of rotator cuff repair has been proven in vitro, the clinical evidence for a higher rate of scarring is limited. The majority of studies centre on synthetic grafts or allografts used in massive tears, while fewer cover autologous grafts and the augmentation of repairable tears.
In the best cases, chemically treated frozen fresh grafts, frozen fresh allografts or lyophilised allografts act as scaffolding that permits new growth of the host tissues. This is appealing as given that tendons have restricted spontaneous capacity for scarring, implanting scaffolding that stimulates their regeneration may be a very important aid in the scarring process.
Grafts deriving from the extracellular matrix, synthetic polymers or hybrid combinations of the same have now been approved by the FDA and commercialised as medical devices to aid rotator cuff repair in human beings. They are from the dermis, small intestine submucosa, fascia lata or pericardium, and they are processed and formed into patches to reinforce the cuff. Descriptions of them may be found in several publications.39–42,24 Although many grafts based on the extracellular matrix or synthetic polymers are available for the repair of the cuff in humans, some of them have yet to be fully proven to be effective in reducing the repeat tear rate in comparison with primary repair. Some experimental works on graft augmentation in animals and human cadavers show mechanical strength, a reduction in retraction and a possible reduction in repeat tears. Likewise, other publications show a reduction in pain, functional improvement and higher rates of satisfaction and cure in patients with graft augmented rotator cuff repair in comparison with their previous condition31,43–45 or with a control group.29
Nevertheless, little emphasis has been placed on the use of autologous grafts. This is surely due to their lower strength and swift re-absorption, although it must not be forgotten that implanting them creates a suitable environment for tissue repair. They create regenerative stimuli that support the curing process and may be strong enough to protect the suture during the first weeks after surgery while tissue repair takes place.24 Some laboratory studies show that fascia lata has similar biochemical and structural characteristics to human SS tendon and canine IS tendon,36 with similar mechanical properties that indicate it may be used as an augmentation medium.37
Several recent publications have shown improved repair results when augmentation grafts were used.30,44,46 Nevertheless, their efficacy in reducing the repeat tear rate in comparison with graft-reinforced suture has hardly been studied. Studies have taken place in cadavers and animals,47 or improvements are described in comparison with their previous condition.31 Few studies observe an improvement in the rate of cure in the group of patients given a graft in comparison with a control group in which repair took place without an augmentation graft.29
We found no prospective studies that evaluate the reduction in the repeat tear rate in rotator cuff repair patients who had received an autologous fascia lata implant. However, some experimental works in animals and human cadavers refer to mechanical strength, a reduction in retraction and the possible reduction in repeat tears. McCarron et al., in their study, stated that the said implants may reduce the failure rate of cuff repairs. Their biomechanical study observed that augmentation with fascia lata patches led to less gap formation that was the case with un-augmented repairs, with the possibility of eliminating 33% of primary suture failures and the subsequent clinical benefit this would bring. Our results are consistent with these findings, as after a one-year follow-up there were twice the number of repeat tears in the group without an autologous fascia implant after the primary suture as there were in the group that received the implant after the primary suture.
Native fascia lata has weaker biomechanical properties than fascia lata reinforced by means of tissue engineering. Autologous fascia lata is free of antigenicity problems, and in our study we found that it continues to give structural and biomechanical reinforcement that helps to reduce the repeat tear rate. Moreover, as the majority of retractions occur in the first 12 weeks after surgery,18 protecting or reinforcing the suture during this period may lead to a reduction in the number of repeat tears.
This is the first prospective study on augmenting the primary suture with autologous fascia lata in a group of patients with rotator cuff lesion, in comparison with a control group. Other autologous augmentation implants are described in the literature: Scheibel et al. published their results using autologous periostium, Sano et al. used the long part of the biceps to repair massive cuff lesions in 14 patients and Bektaser et al. used coracoacromial ligament as an augmentation in massive cuff lesions. We observed a functional improvement in the patients treated with an augmentation of autologous fascia lata after one year of follow-up, although there were no differences respecting the control group. Nevertheless, in the group with the implant the improvement in pain at 6 months is highly significant. If we evaluate patient mobility (flexion+external rotation+internal rotation+abduction) together with everyday life activities in both groups, the graft group is found to have a better response (with an average of 41.3) in comparison with the non-graft group (with an average of 39.2). We believe that the implant has a mechanical and biological effect that reduces the duration of subjective pain in comparison with non-augmented sutures, as the latter depend solely on repair of the existing cuff and its scarring. There is a reduction in the rate of repeat tears in the group treated with the augmentation of autologous fascia lata, and no significant differences were found in the proportion or type of repeat tears after a one-year follow-up in both groups studied.
Although other authors have used allografts, they took the form of augmentation devices for the repair of large and massive cuff tears when conventional repair was impossible: Neviaser et al.25 and Nasca48 used lyophilised cadaveric rotator cuff; Ito and Morioka26 used a double layer of lyophilised fascia lata to treat large and massive tears; Moore et al.27 repaired massive tears of the rotator cuff in 32 patients with different interposed allografts (quadriceps tendon, patella tendon or Achilles tendon) when it was not possible to obtain a tension-free repair. Human dermis matrix was used by Rotini et al.,28 Barber et al.,29 Bond et al.,30 Wong et al.31 and Gupta et al.,32 showing that this type of allograft may be an aid in curing the tendon.
Our sample is homogeneous in terms of the type of tear in both treatment classes and, unlike the majority of the above-mentioned publications, we did not operate on massive and/or irreparable tears, but rather all of the tears were repaired without tension in both treatment groups, with or without augmentation. We obtained a reduction in the repeat tear rate in the group treated with the augmentation of autologous fascia lata implant, without finding significant differences between both groups in the proportion or type of repeat tears after a follow-up of one year.
In 2014 Ciampi et al.49 published their results with 152 patients with massive posterosuperior cuff tear, comparing the results of open repair without augmentation as the control group with open repair and a patch with collagen augmentation, and a third group with a synthetic patch. The latter had the best results in terms of function, strength and the repeat year rate. Although it is not the ideal patch, the synthetic one gave successful results and reduced the repeat tear rate by somewhat more than 50% in comparison with the control group. This agrees with our results, as we found a 50% reduction in patients treated with fascia augmentation after their primary suture. The high rate of repeat tears in the collagen group may be explained by the rapid absorption of the same; in our biological implant the fascia lata has structural and biomechanical properties that are similar to those of the tendon. This similarity allows us to use it as an augmentation medium,37 and as it is autologous it offers the benefits of regenerative stimuli that support the curing process. This means that we would achieve a similar reduction in the repeat tear rate as is achieved with the synthetic patch used by this author, although with the benefits of the biological properties of an autologous graft.
Respecting the improvement in functional results, ours are similar to those found in previous publications. Although both types of treatment (a primary suture with and without augmentation) led to improvement after one year of follow-up,29 there were no differences between the average Constant–Murley scores and pain after one year between both groups.
In the implant group the improvement in pain at 6 months is highly significant. Our results show that although both groups attain similar values for pain at 12 months, the non-implant group took longer to reach values that the implant group had attained after 6 months’ evolution. This supports the idea that the autologous implant used confers mechanical reinforcement as well as a biological improvement in the curative potential of the tendon.
In the literature only Barber et al.50 present better clinical results following the biological augmentation of a primary standard rotator cuff repair, although their study was not randomised; the other studies29,51–53 that compare results between augmentation and conventional repairs do not find any significant differences in terms of improved clinical results between the groups treated with augmentation and the control group.
In 2016 Jiménez-Martín et al.54 published the results of cases treated by repeat suture and orthobiological augmentation with porcine intestinal submucosa, equine pericardium and porcine dermis. These were found to be acceptable in the suture of cuffs where results had been ineffective, and as an alternative to tendon transfers in massive tears.
Several publications have described reduction in pain, functional improvement, higher satisfaction and rates of cure in patients with cuff repair after augmentation with an implant in comparison with their previous condition31 or with a control group.29 In our study although an improvement was observed in comparison with the previous condition of patients, this was not the case in comparison with the control group.
The majority of augmentation studies centre on massive and/or irreparable lesions of the rotator cuff, while other studies centre on medium-sized or small lesions. This makes it harder to determine which procedure is the most effective for a specific type of lesion in terms of functional improvement. In our study both groups were homogeneous in terms of their initial tear, and all of them were repaired without tension. There were no differences between both treatment groups in pain or function after one year.
Although both groups were homogeneous in terms of the initial fatty degeneration of the SS and IS and in the initial atrophy of the same, we found that we were starting from a situation with more fatty infiltration of the IS in the group treated with the implant (4 in stage 2, as opposed to 3 in the non-implant group). We also started with a situation of 2 cases of moderate IS atrophy in the implant group, compared with one case in the non-implant group; in spite of this initial disadvantageous situation the repeat tear rate was lower in the implant group.
We found no complications in the donor zone in any of the patients treated with a graft, and none of them mentioned any discomfort during the postoperative period in comparison with the non-graft group.
Assignation to each group was not random, as this decision was taken by the surgeon. Nevertheless, analysis of the homogeneity of the groups shows there were no differences between them, so that they may be considered homogeneous and comparable.
In treatments of this type it is not possible to hide the method used from the patient; however, we suppose that the possible effect of patient knowledge on the incidence of repeat tears is practically zero.
Future works may check the hypothesis and results of our study with a larger sample and a longer follow-up over time.
ConclusionOur preliminary results of augmentation surgery of the rotator cuff with autologous fascia lata show a significant improvement in pain at 6 months in comparison with the patients without augmentation, and although there were no significant differences in terms of function or the risk of a repeat tear, the patients with the augmentation of fascia lata benefited from a swifter improvement in pain.
Level of evidenceLevel of evidence II.
Conflict of interestThe authors have no conflict of interest to declare.
Please cite this article as: Rosales-Varo AP, García-Espona MA, Roda-Murillo O. Resultados de la cirugía de refuerzo del manguito rotador con fascia lata autógena. Rev Esp Cir Ortop Traumatol. 2018;62:157–167.