Prosthetic infections are a potentially devastating complication, especially in elderly patients. Antibiotic-loaded bone cement has been used both as a treatment and prophylaxis in prosthetic infection, and its use is not well documented in the prophylaxis of infection in patients who have suffered a hip fracture.
MaterialA retrospective descriptive was performed. The data were obtained from all the patients who underwent hip hemiarthroplasty due to a subcapital fracture between 2011 and 2017 (N=241). An epidemiological study of the patients studied was carried out. We analysed the incidence of periprosthetic infection in the groups treated with cement without antibiotic and antibiotic-loaded bone cement, as well as the protective effect of the antibiotic-loaded bone cement. At the same time, a pilot cost analysis study was carried out.
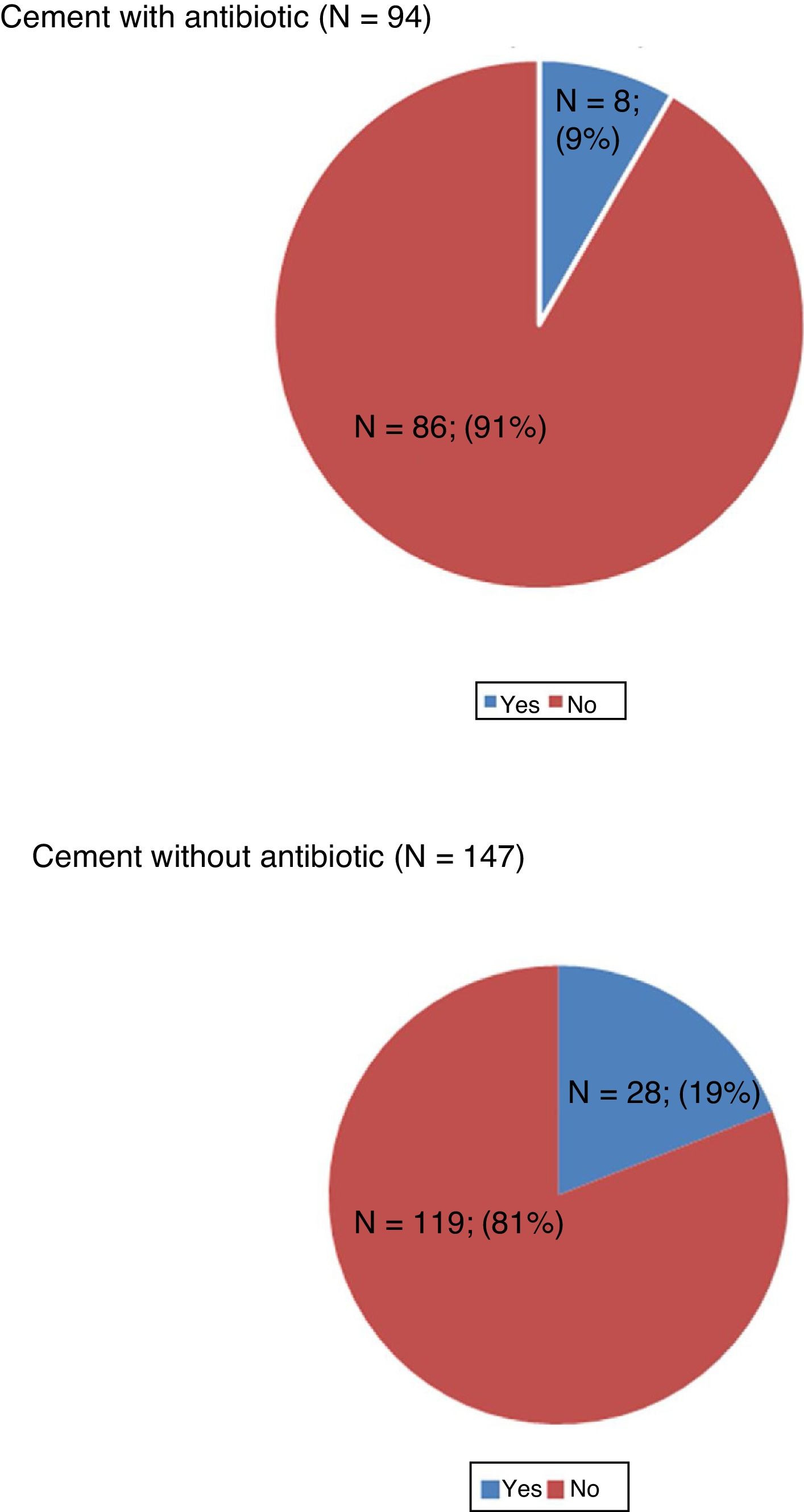
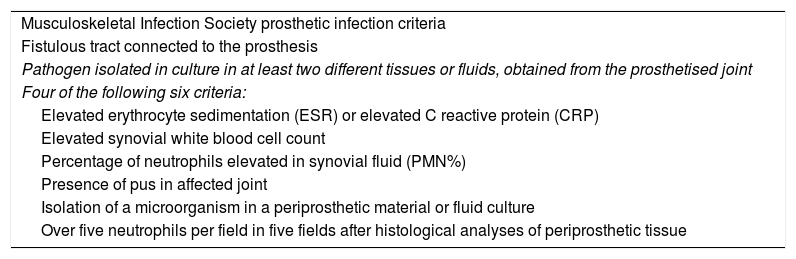
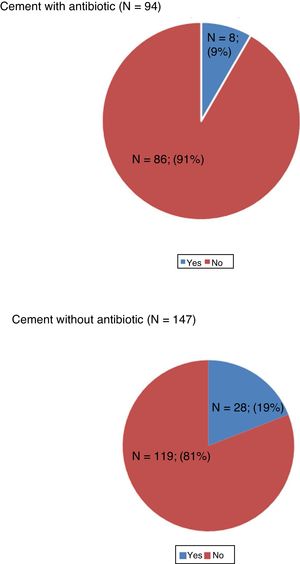
ResultsIn the group that received antibiotic-loaded bone cement (n=94) there were 8 infections (8%), while in the group with cement without antibiotic (n=147) there were 28 infections (19%). The odds ratio (OR) was calculated, showing a 55.3% reduction in the risk of developing late infection in the group that received cement with antibiotic (95% CI: 6.2–78.7 %) (P=.0025). The use of antibiotic-loaded bone cement led to significant cost savings per patient.
ConclusionsThe use of antibiotic-loaded bone cement is a protective factor in the development of late infection after hip hemiarthroplasty surgery in elderly patients with hip fracture.
Las infecciones protésicas son una complicación potencialmente devastadora, más aún en pacientes ancianos. Los cementos con antibiótico han sido usados tanto como tratamiento como profilaxis en la infección protésica, no encontrándose bien documentado su uso en la profilaxis de la infección en la cirugía hemiartroplastia en pacientes que han sufrido una fractura de cadera.
MaterialEstudio descriptivo retrospectivo donde se obtuvieron datos de todos los pacientes intervenidos mediante hemiartroplastia de cadera por fractura subcapital entre los años 2011 y 2017 (N=241). Se realizó un estudio epidemiológico de los pacientes estudiados. Se analizó la incidencia de infección periprotésica en los grupos tratados con cemento sin antibiótico y con antibiótico, así como el efecto protector del mismo. A su vez se realizó análisis de costes piloto.
ResultadosEn el grupo que recibió cemento con antibiótico (n=94) se produjeron 8 infecciones (8%), mientras que en el grupo con cemento sin antibiótico (n=147) se produjeron 28 infecciones (19%). Se realizó el cálculo de odds ratio (OR) observándose un 55.3% de disminución de riesgo de desarrollar infección tardía en el grupo que recibió cemento con antibiótico (IC 95%: 6,2–78,7%) (P=0,0025). El uso de cemento con antibiótico conllevó un importante ahorro de costes por paciente.
ConclusionesEl uso de cementos con antibiótico resulta un factor protector en el desarrollo de infección tardía en hemiartroplastia de cadera en pacientes ancianos con fractura de cadera.
Prosthetic infections are a rare but potentially devastating complication. The rate of infection after a primary hip arthroplasty is between 1% and 2%,1 but is much more daunting when we refer to elderly patients with hip fractures, where rates rise to between 1.7% and 7.3%.2 This involves high socioeconomic costs3 and raised morbimortality.2
Antibiotic-loaded bone cements have been used both as a treatment and as prophylaxis in prosthetic infection. Whilst their use has been well studied in elective primary arthoplasty,4–6 it has not been well documented in the prophylaxis of infection in partial prosthesis implantation in patients with a hip fracture.
The use of acrylic cements in orthopaedia dates back to the decade of the 1950’s when Sir John Charnley became interested in them, but it was not until 1969 when investigation into their use as a vector for the release of antibiotic drugs in situ was started by Buccholz and Engelbrecht.7
The interest in creating cements enriched with antibiotics is due to the difficulty in achieving effective levels of antibiotics in bone tissue, because the pro-inflammatory conditions reduce blood flow and impede drug access, although there is no real anatomical barrier.8 Furthermore, the bacteria in contact with the implants create adhesive barriers, biofilms, which prevent the penetration of the antibiotic and minimize its effect.7 Antibiotic-loaded bone cements are of great value for the release of effective doses directly into the required area over a prolonged period, which according to some studies is limited to the first 2 years.9 This maximizes the concentrations of the antibiotic drug in the joint and minimises systemic exposure.7
The high rates of prosthetic infection after hemiarthroplasty detected in our centre have led us to contemplate other strategies in infection prophylaxis. We decided to analyse the impact the introduction of antibiotic-loaded bone cement has had in our population, with the hypothesis that its use, combined with systemic prophylaxis would result in a protective factor.
Our main objective was to compare the rate of infection in patients with a hip fracture and who had been operated on for a hemiarthroplasty with antibiotic-loaded bone cement compared to those in whom no antibiotic-loaded bone cement had been used. Our secondary objective was to analyse the different variables which could have had an impact on the development of infection, to undertake a population analysis and a pilot cost study.
Material and methodsA retrospective descriptive study was conducted in the Universitario Central de la Defensa Gómez Ulla of Madrid (Spain). Data was obtained from all of the patients who underwent hip hemiarthroplasty due to a subcapital fracture between 2011 and 2017 from their medical file (written or digital in the Balmis ®, electronic clinical history programme, Hewlett Packard Española, SL). Inclusion criteria considered any intracapsular fracture of the femur operated on with cemented arthroplasty (bipolar or monopolar). Exclusion criteria included pathological fractures and patients who died during the first 30 days following intervention.
All operations were performed by the same medical team and used the same surgical approach route (direct lateral or Hardinge). Preoperative parenteral prophylaxis was performed with 2g of cefazolin one hour prior to the operation or 1g of vancomycin if there was a contraindication or allergy to cephalosporins. Three doses were administered after surgery of 1g every 8h for cefazolin or 2 doses of 1g of vancomycin every 12h.
The implanted prosthesis was a SAMO Multifit ® with a monopolar Ellitica ® head or bipolar SBA ® (SAMO biomedical, Italy) head in all patients. The cement used was CEMEX ® (TECRAS SPA, Italy), an antibiotic-free cement with high viscosity mixed and applied with a cement gun and mixture without a vacuum system up until June 2013. From that date onwards and until the end of the study (December 2017) the Palacos® R+G (Heraeus Medical GmbH, Germany) cement was used, with gentamycin (.5g) of high viscosity, mixed using a vacuum system and applied with a pressure cement gun.
Data was collected retrospectively on age, sex, type of intracapsular hip fracture according to the Garden scale, injurious mechanism (low/high energy), form of transfer to emergency services (walking, taken by family members in a private vehicle, taken by ambulance from home or by ambulance for another healthcare centre).
The presence or absence of previous risk factors for the development of infection was assessed (inflammatory arthopathies, immunosuppressant status, diabetes mellitus type 1, previous joint infection, malnutrition, malignant tumours o haemophilia).
The physical status of the patients was assessed using the American Society of Anesthesiologists physical status scale (ASA), ambulation ability was assessed using the Functional Ambulation Category Score (FAC) and degree of dependence for everyday life activities by the Modified Barthel Functional Index.
The development of acute or late infection in both groups (cemented with or without antibiotics) was assessed and mean time until infection was diagnosed.
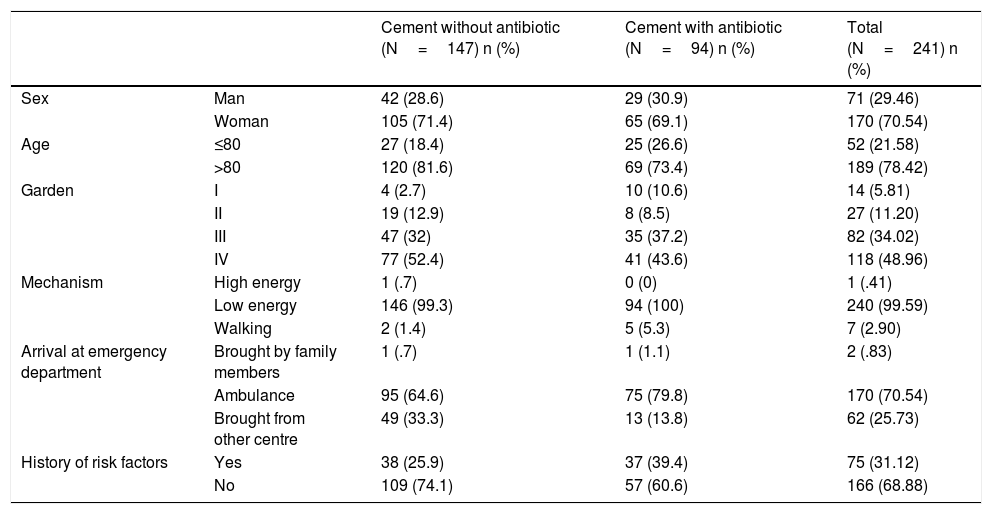
Diagnosis of infection was approached according to the criteria reflected in the 21st anual meeting of the Musculoskeletal Infection Society in 2011 (Table 1).
Musculoskeletal Infection Society prosthetic infection criteria.
| Musculoskeletal Infection Society prosthetic infection criteria |
| Fistulous tract connected to the prosthesis |
| Pathogen isolated in culture in at least two different tissues or fluids, obtained from the prosthetised joint |
| Four of the following six criteria: |
| Elevated erythrocyte sedimentation (ESR) or elevated C reactive protein (CRP) |
| Elevated synovial white blood cell count |
| Percentage of neutrophils elevated in synovial fluid (PMN%) |
| Presence of pus in affected joint |
| Isolation of a microorganism in a periprosthetic material or fluid culture |
| Over five neutrophils per field in five fields after histological analyses of periprosthetic tissue |
Data were collected in a Microsoft Excel ® table anonymously and analysed with the SPSS ® version 15 statistical package (SPSS Inc., Chicago, IL, U.S.A.).
A pilot cost/benefit study was also conducted, comparing the cost of the products, surgical interventions and length of stay in the hospital according to the standard DRG (diagnosis related groups) coding, established by Order DEF/2277/2014, of 28th November, published in the Official State Bulletin (BOE-A-2014-942) which established the public prices for provision of healthcare services and activities in the Ministry of Defence area. The price offered included:
- a)
Routine or special diagnostic and therapeutic tests, which the patient was required to have prior to the procedure they were to be submitted to, including, when necessary, the preoperative study.
- b)
The costs derived from possible complications which could present over the whole healthcare process, both in the preoperative phase and in the actual surgical and postoperative intervention.
- c)
The necessary surgical reinterventions required by the patient, provided they are always related to the process leading to admission, resulting from poor surgical practice and taking place within a period not superior to 2 months, counted from the day after hospital discharge.
- d)
Medical treatment if required during the process, or blood and blood products.
- e)
Healing treatments.
- f)
Food, including parenteral and enteral nutrition.
- g)
Assistance by a specialised medical team; nurses and auxiliary healthcare staff.
- h)
The use of an operating theatre and anaesthesia costs.
- i)
The necessary expendable material and pre and postoperative controls, including those of the outpatient regime.
- j)
Costs of days in the hospital in a shared room or a private room, when due to the special circumstances of the patient this becomes necessary.
- k)
Any necessary intensive care unit stays in hospital.
- l)
Revision check-ups that are necessary after hospital discharge, with at least one consultation for each procedure.
During the study period of 2191 days (January 2011–January 2017) a sample of 241 patients was obtained, 94 of whom received antibiotic-loaded bone cement and 147 who did not.
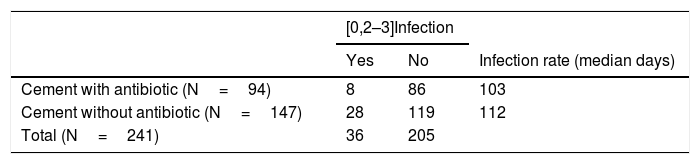
Population clinical data (age, sex, type of fracture according to Garden classification, fracture mechanisms, method of hospital transfer and the presence of risk factors for the development of infection) are described in Table 2.
Clinical data.
| Cement without antibiotic (N=147) n (%) | Cement with antibiotic (N=94) n (%) | Total (N=241) n (%) | ||
|---|---|---|---|---|
| Sex | Man | 42 (28.6) | 29 (30.9) | 71 (29.46) |
| Woman | 105 (71.4) | 65 (69.1) | 170 (70.54) | |
| Age | ≤80 | 27 (18.4) | 25 (26.6) | 52 (21.58) |
| >80 | 120 (81.6) | 69 (73.4) | 189 (78.42) | |
| Garden | I | 4 (2.7) | 10 (10.6) | 14 (5.81) |
| II | 19 (12.9) | 8 (8.5) | 27 (11.20) | |
| III | 47 (32) | 35 (37.2) | 82 (34.02) | |
| IV | 77 (52.4) | 41 (43.6) | 118 (48.96) | |
| Mechanism | High energy | 1 (.7) | 0 (0) | 1 (.41) |
| Low energy | 146 (99.3) | 94 (100) | 240 (99.59) | |
| Walking | 2 (1.4) | 5 (5.3) | 7 (2.90) | |
| Arrival at emergency department | Brought by family members | 1 (.7) | 1 (1.1) | 2 (.83) |
| Ambulance | 95 (64.6) | 75 (79.8) | 170 (70.54) | |
| Brought from other centre | 49 (33.3) | 13 (13.8) | 62 (25.73) | |
| History of risk factors | Yes | 38 (25.9) | 37 (39.4) | 75 (31.12) |
| No | 109 (74.1) | 57 (60.6) | 166 (68.88) |
In the group which received cement without antibiotic only 38 patients (25.9%) presented with a history of medical risk for the development of infection (inflammatory arthropathies, immunosuppressant status, diabetes mellitus type 1, previous joint infection, malignant tumours or haemophilia). In the group which received antibiotic-loaded bone cement this percentage of patients was 39.4% (n=37). We also assessed the use of oral anticoagulants (acenocumarol): this was used in 18 (7.4%); 10 (6.8%) in the group of cement without antibiotic and 8 (8.5%) in the group with antibiotic-loaded bone cement.
The predominant ASA in both groups was 3 (patient with severe but not incapacitating systemic disease) in 127 patients (52.9%).
Regarding the functional state of patients, in both groups a FAC dependence of 4 predominated (independent walking on flat ground, but no stairs), median and mode=4 for both groups and a dependence on the Barthel scale with a median of 70 points in both groups (moderate dependence), cement without antibiotic mode=60; cement with antibiotic mode=80. Mean ages were very similar in both groups: around 85 years of age.
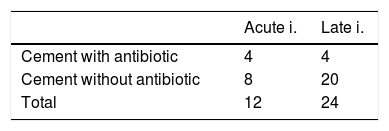
In the group which received antibiotic-loaded bone cement (n=94) there were 8 infections (8%) of which 4 were acute (under 3 months) and 4 late (>3 months). In the group with cement without antibiotic (n=147) there were 28 infections (19%) of which 8 were acute and 20 late (Tables 3 and 4, Fig. 1). Between the 2 groups there were 14.9% of acute and late infections (n=36).
The odds ratio (OR) was calculated showing a 55.3% reduction in the risk of developing late infection in the group who received cement with antibiotic (95% IC: 6.2–78.7%) compared to those who did not receive cement with antibiotic (p=.0025).
The process of a partial prosthesis of the hip costs approximately 12,665€, and when there are complications there would be added costs of 11,540.45 € (approximately 24,205 € per patient in the case of acute infection or of 35,746 € in the case of late infection due to the longer hospital stay and number of operations). Bearing in mind that the PALACOS® R+G cement has an added cost of approximately 20€ per unit compared to CEMEX® cement without antibiotic, the group treated with antibiotic-loaded bone cement cost a mean of 14,127.54 € per patient whilst the group with cement without antibiotic cost a mean of 17,632.81 € per patient. These costs are approximate, and are in keeping with the DRG of our centre.
DiscussionImplant contamination most often occurs from direct spread during surgery, direct spread through skin defects or from haematogenous spread. The most common isolated germ is Staphylococcus aureus.
In their study Stefánsdóttir et al.10 reviewed deep infections in primary knee arthroplasty through the national Swedish register between 1986 and 2000, and found that in acute, subacute and late infections coagulate negative staphylococcus were the most prevalent (35.1%) and double as common as S. aureus (18.4%), which was the predominant pathogen in blood-borne infections. This microbiological pattern changed considerably during the study period (p=.019): the proportion of infections caused by S. aureus fell from 46.3% in 1986–1990 to 27.6% between 1996 and 2000.
The use of antibiotic-loaded bone cements has been well studied in primary arthroplasty.11 Engesaeter et al. performed an analysis of 22,170 primary hip arthroplasties through the Norwegian register between 1987 and 2001 and compared systemic antibiotic prophylaxis combined with the use of antibiotic-loaded bone cement to antibiotic prophylaxis alone in different administration guidelines. The best results were obtained in the group which received intravenous prophylaxis and also cement with antibiotic: systemic prophylaxis alone had 1.4 times more revision surgery (p=.001), 1.3 times more revision surgery for aseptic loosening (p=.02) and 1.8 times more rates of infection (p=.01).7 Furthermore, Jiranek et al.12 carried out an in-depth analysis of the current state of use of antibiotic-loaded bone cements in primary arthroplasty and recommended its prophylactic use against infection only in patients who had a high risk of infection: i.e. those patients with associated factors such as inflammatory arthropathies (rheumatoid arthritis, lupus), immunosuppressant status, diabetes mellitus type 1, prior joint infection, malnutrition, malignant tumours or haemophilia.
The use of antibiotic-loaded bone cements in hemiarthroplasty cases after a fracture is not well documented in scientific literature. The main use of hemiarthroplasty of the hip is restricted as the treatment of choice in intracapsular fractures in elderly patients. We should consider that the prototype patient is not the same as in an elective prosthesis. These are elderly patients with many comorbidities, which drastically reduce their life expectancy13 and increase their possibilities of suffering from a prosthetic infection up to 4 times more than in an elective arthroplasty,14,15 but who also have presented with a traumatic event which in itself affects their survival enormously.16 Mortality after a hip hemiarthroplasty is around 10–40% in the first year, often linked to an infection.17 Infection rates after the implantation of a partial hip prosthesis are between 1.7% and 7.3%.2 In our study, this figure was much higher: between acute and late infections the rate was 14.9%. We believe that this rate, higher than that identified by other studies, could be due to the old age of the population treated by our hospital (78.42% of our sample were over 80 years of age). Also, if we refer to the definition of a fragile elderly person, our patients met with many of the criteria included in this group (advanced age, moderate dependence measured by the Barthel scale, changes to mobility and balanced measured through the FAC scale, medical/comorbidity status measured through the ASA scale).18
The use of cemented implants may slightly increase time in surgery and bleeding, although it is not of clinical significance since there is no increase in morbimortality,19 but it seems clear that the use of cement reduce pain and improves the patient’s mobility after surgery, without a significant increase in complications.20,21
In a bibliographic review of 37 articles obtained from the data bases of MedLine, PubMed and Cochrane, Noailles et al. Identified the risk factors for the development of a surgical infection after hemiarthroplasty and possible methods of prevention and they recommended the use of antibiotic-loaded bone cement.2 The comorbidity of the patient (obesity, liver disease, advanced age), the intraoperative conditions (inexperienced surgeons, prolonged time of surgery or cementless implants) and postoperative management (prolonged hospitalisation, haematoma, prolonged use of drainage or repeated use of vesicle catheters) were identified as the risk factors in the development of surgical infection. Recently, Crego et al.22 demonstrated that functional ASA classification and advanced age are independent factors in obtaining poorer results since they increase complications and mortality after surgery in elderly patients with hip fractures.
Sanz-Ruiz et al.,23 in a comparative study with 2518 patients operated on for total or partial prosthesis of the hip and of the knee, analysed the relative risk reduction of a prosthetic infection when using antibiotic-loaded bone cement vs. cement without antibiotic and specifically 72.6% in the case of the hip arthroplasty (partial or total) (p=.019). Subsequently, in cost calculation, the use of antibiotic-loaded bone cement resulted in a saving of 1123.846 € (992 € per patient), as the rate of infections dropped.
In our study a 55.3% drop in the risk of developing late infection was observed in the group which received antibiotic-loaded bone cement (95% CI: 6.2–78.7%) compared to those who had not received antibiotic-loaded bone cement (p=.0025). The group treated with antibiotic-loaded bone cement cost a mean of 14,127.54 € per patient, whilst the group with cement without antibiotic cost a mean of 17,632.81 € per patient.
Some of the possible problems which could present with the use of antibiotic-loaded bone cements according to its detractors would be the development of bacterial resistance,24 because of the exposure of subinhibitory concentrations of antibiotics prolonged over time.25 A source of concern is also whether the mechanical properties of the cement26 may be affected. With regards to the toxicity or allergies from use, these have very rarely been reported in publications and isolated reports have referred to hypersensitivity.27,28 In our study we did not find any adverse effects or allergies to the use of antibiotic-loaded bone cement.
Recently, Sprowson et al.29 conducted a quasi-randomised study to compare the effectiveness of cements with dual synergistic action antibiotics (1g clindamycin+1g de gentamicin) vs. plain (.5g de gentamicin) in patients with intracapsular hip fracture: the result was a reduction in the rate of surgical infection without any increase in complications. However, further studies are necessary to determine optimum doses of antibiotics and their effect on the mechanical characteristics of the cement.
It is striking that, despite being in favour of the use of antibiotic-loaded bone cement for the prevention of infections the Food and Drug Administration has only approved its use in second time reimplantation in a replacement prosthesis which had been previously infected.12,30 We should also take into account the epidemiological peculiarities and the different costs of marketing antibiotic-loaded bone cements in other countries such as the United States, in what Sanz-Ruiz describes as “the transatlantic paradox” where results cannot be extrapolated.23
Our study has several imitations which should be mentioned. On the one hand, the fact it is retrospective in nature and the low sample number of patients. Also there is an imbalance between the group who received cement without antibiotic (n=147) vs. those with antibiotic (n=94) and the fact that the antibiotic came from two different manufacturers.
ConclusionsThe strength of our study resides in the demonstration of the use of antibiotic-loaded bone cement as a protective factor in the development of late surgical infection: it is one of the few studies that takes into account the peculiarities of the population with hip fracture and also encompasses an epidemiological study of the patients who were hospitalised as a result.
Although our cost study was a pilot study and is not definitive, it is highly illustrative of the major benefit obtained with a simple cost increase of scarcely 20€ per patient.
Given the well-known high costs and devastating repercussions of a prosthetic infection, the research team would recommend the use of antibiotic-loaded bone cement as prophylaxis in primary prosthetic surgery in patients with intracapsular hip fracture.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Aedo-Martín D, Crego-Vita D, García-Cañas R, Espigares-Correa A, Sánchez-Pérez C, Areta-Jiménez FJ. Infección periprótesica en pacientes ancianos tratados mediante hemiartroplastia de cadera tras fractura intracapsular. ¿Debemos usar cementación con antibiótico? Rev Esp Cir Ortop Traumatol. 2020;64:28–34.