Fractures of the proximal humerus constitute 10% of all fractures, with an incidence that continues to grow and could treble in the next three decades.1,2 In elderly patients, they constitute the third group in frequency, exceeded only by hip fractures and distal fractures of the radius. Despite classical teachings,3 recent epidemiological studies suggest that displaced fractures are more frequent than was traditionally thought.4 Non-displaced or minimally displaced fractures can be treated conservatively with good functional results.3 The remainder would be candidates for surgical treatment. Out of this total of proximal humerus fractures, both those treated conservatively and those undergoing surgery, only a small minority develop malunion or pseudoarthrosis, with malunion being more frequent.4 These complications are difficult to treat and constitute a surgical challenge with a high rate of complications. For this reason, it is important to identify fractures with the greatest risk as early as possible and to carry out clinical and radiological follow-up.
Pseudoarthrosis of the proximal humerusEpidemiology and classificationPseudoarthrosis of the proximal humerus is an infrequent complication associated with pain and a major functional limitation of the shoulder. Court-Brown et al.4 recently found an incidence of 1.1% in a revision of 1027 fractures monitored prospectively. It is more frequent in displaced fractures of the metaphysis in two parts and in some in three or four parts5 (Fig. 1). A greater incidence has been described following surgical treatment although it might be related to the greater complexity of the fractures in which this indication is chosen.4
Numerous factors have been related to the absence of consolidation in the proximal humerus. First of all, factors depending on the fracture itself. Among these, the most important are the initial displacement and metaphyseal comminution.4 The interposition of soft tissue such as deltoid fibres, the biceps tendon or the rotator cuff, as well as synovial fluid at the fracture focus, may also prevent consolidation.3 The second group of factors depends on the specific patient. Numerous authors have related age, the presence of comorbidities, the use of corticosteroids or smoking with the onset of complications. Finally, there are some that depend on the technique, such as excessive traction caused by hanging plaster casts, deficient osteosynthesis or early rehabilitation.5
Checchia et al.6 have put forward a classification for pseudoarthroses of the proximal humerus. Group 1 includes high two-part fractures such as those of the anatomical neck with a very small fragment of the head. It is possible to appreciate cavitation of the proximal fragment due to the speedy resorption of spongy bone. Neer proposed that this phenomenon was due to communication between the fracture and the synovial fluid.3 Group 2 is low two-part fractures with a larger proximal fragment. It includes pseudoarthroses occurring between the minor tuberosity and the insertion of the pectoralis major and fractures in three parts where the tuberosities have consolidated with a displacement of less than 5mm. Group 3 involves complex pseudoarthroses secondary to fractures in three or four parts, with division of the head or a displacement of more than 5mm in the tuberosities. Finally, group 4 contains pseudoarthroses with missing bone fragments or those secondary to high-energy trauma, open fractures or post-traumatic osteomyelitis.
In their classification of sequelae of fractures in the proximal humerus, Boileau et al.7 also highlight the importance of the state of the tuberosities and the size and quality of the cephalic fragment. The sequelae of fractures in the proximal humerus are divided into 4 groups with the aim of predicting what the results of their treatment will be. The first group includes the result of fractures impacted in varus or valgus, where there is cephalic collapse or necrosis, but with consolidated tuberosities. The second group comprises inveterate glenohumeral luxations or fractures with luxation. Group 3 is formed by pseudoarthroses of the metaphysis with displacement of the tuberosities and group 4 by sequelae of fractures in 4 parts with malunion of the tuberosities. Groups 1 and 2 would be intracapsular sequelae in which it is not necessary to perform osteotomy of the trochiter and they usually have predictably satisfactory results. Groups 3 and 4, on the other hand, would be extracapsular sequelae, with displacement of the tuberosities; these usually require osteotomy of the trochiter for their reconstruction and entail unpredictable and unsatisfactory results.
Pre-operative diagnosis and assessmentThe diagnosis of pseudoarthrosis must be made as soon as possible, even within the first 6 weeks. Following a fracture, patients generally experience an improvement over 3 months and an absence of progression between 3 and 6 months, con limitation in the flexion and abduction, variable pain and a delay in the recovery of the basic activities of daily living.4
Minimally symptomatic patients with low functional demands can be given a conservative treatment. However, consolidation should not be expected to occur at a late stage and patients must be aware that in some cases they will continue to feel pain and functional impotence with a reduction in the anterior elevation and rotations during the long-term follow-up.8,9
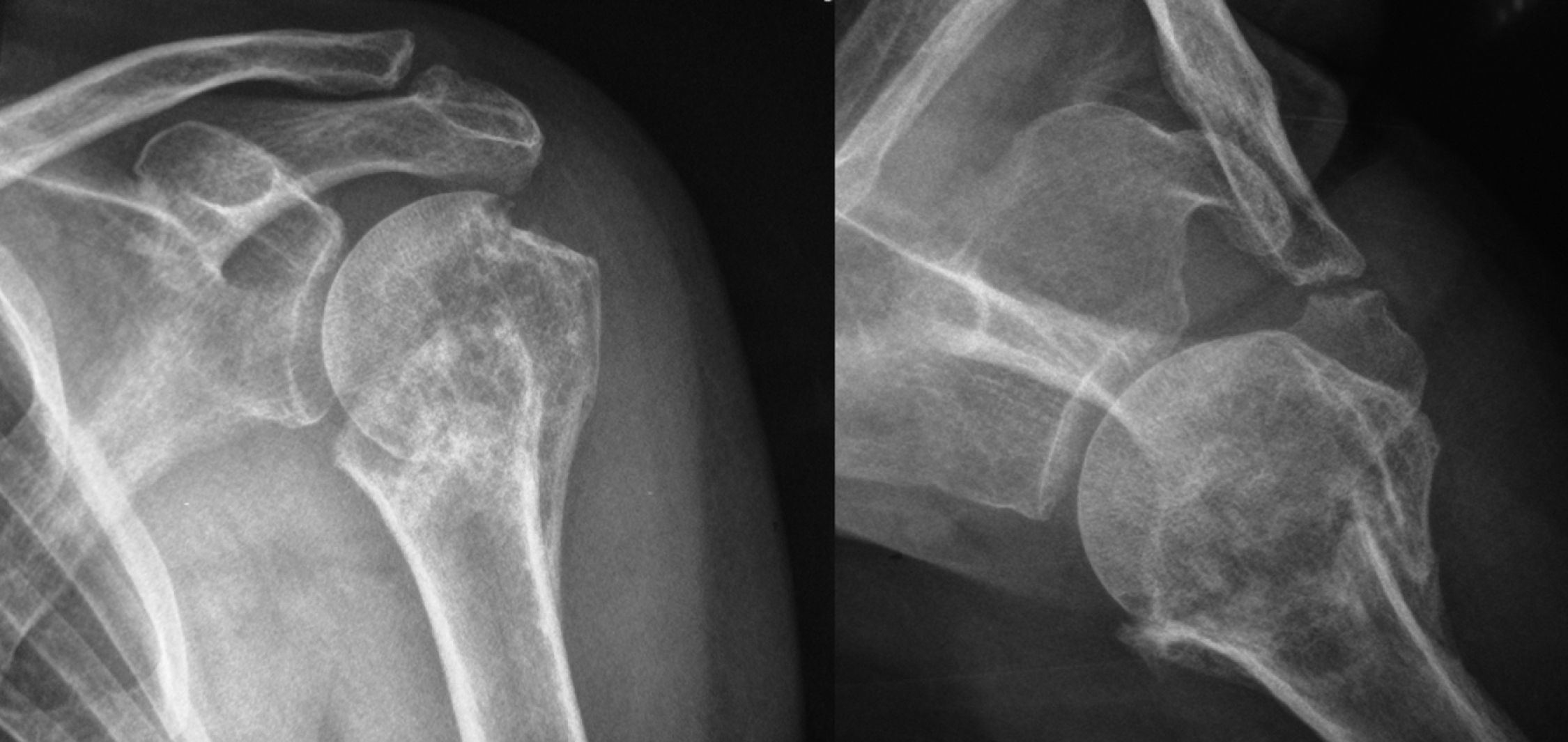
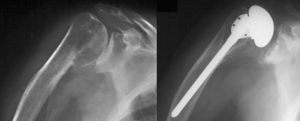
Where surgical treatment is considered, it is necessary to carry out a complete pre-operative study of the characteristics of the patient and of the fracture. It is recommendable to perform an exhaustive neurological examination, verifying the functionality of the deltoid. The radiological study must include at least one anteroposterior projection in the scapular plane and a true axillary projection (Fig. 2). The following must be evaluated: the status of the cephalic fragment, the bone deficit at the focus of the pseudoarthrosis, the presence or otherwise of necrosis in the head of the humerus and the integrity of the joint cartilage. The use of computed tomography (CT) might be particularly useful for the evaluation of the fractures with division of the head and to quantify the displacement of the tuberosities.
(A) Anteroposterior X-ray of the left shoulder in the scapular plane raising suspicions of absence of consolidation following fracture of the proximal humerus in 3 parts. (B) True axillary X-ray of the left shoulder showing pseudoarthrosis at the level of the metaphysis and partial consolidation of the trochiter.
Open reduction and osteosynthesis is recommended in young patients with good bone quality and complete joint surface.8 In order to favour consolidation, it is possible to use bone graft or a range of biomaterials.5 When pseudoarthrosis occurs in elderly patients, there is also normally poor bone quality, resorption and cavitation of the proximal fragment. In such cases, it is difficult to achieve consolidation and osteosynthesis may pose problems due the scant amount of remaining bone. For all these reasons, the most suitable option is the replacement of the head of the humerus. Arthroplasty is also the option of choice in cases where there has been a prior failure in the treatment of a pseudoarthrosis and bone quality has deteriorated so much that osteosynthesis offers little guarantee.8
There are scant references in the scientific literature to the results of surgical treatment for pseudoarthroses in the proximal humerus. The first series from the 1990s published less than hopeful results with a relative improvement at the expense of a reduction in pain rather than functional recovery.10–12 Duralde et al.11 obtained a clinically satisfactory consolidation in only half of the cases in their series, which included 20 patients. Of the 10 cases treated with open reduction and osteosynthesis, 9 required re-intervention due to a lack of consolidation, discomfort with the osteosynthesis material or stiffness. Furthermore, Healy et al.9, in their 25-case series treated with 4 different methods, and obtained only 52% satisfactory results. In all cases, they used the tension band mechanism that enables reconstruction of the rotator cuff and neutralization of the forces exerted. The worst results were obtained with intramedullary nail and the best when they combined the use of a T plate with bone graft and tension band.
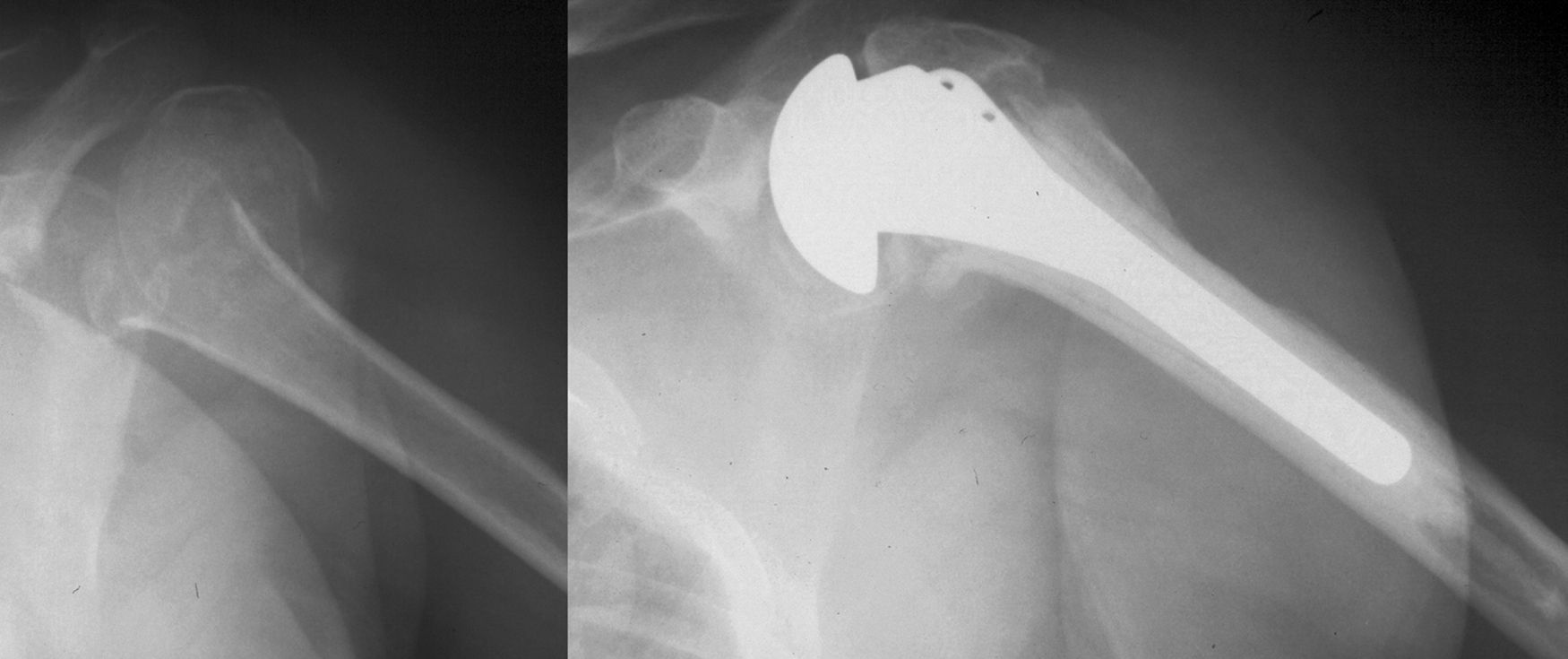
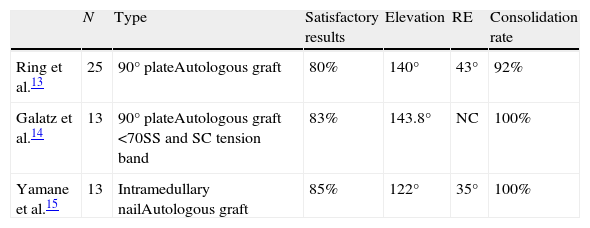
New osteosynthesis techniques and improvements in implant design have enabled better results with the reconstructive options in the treatment of symptomatic pseudoarthroses of the proximal humerus13–15 (Table 1). The most commonly used osteosynthesis options are 90° plates and the new intramedullary nails. The use of bone graft has been systematized, with the graft of choice being autologous iliac crest although some authors advise against it in patients over 70 years of age.15 The new blocked plates associated with iliac crest autografts would probably be the option of choice today.5
Arthroplasty as treatment for pseudoarthrosis of the proximal humerusArthroplasty would be indicated in elderly patients with poor bone quality,8,16 and also in cases where there has been large-scale resorption and cavitation in the cephalic fragment or in synovial pseudoarthroses. Evaluation of the glenoid is essential to assess the need for a hemi-arthroplasty or a total shoulder prosthesis. The placement of a prosthesis in such a setting is technically difficult. Dissection must be meticulous, particularly if it is a re-intervention, due to the considerable anatomical distortion and retraction of soft tissue. In order to access the joint, it is preferable to effect disinsertion of the subscapular muscle and keep the trochin adjacent to the medial calcar and the trochiter.2 If the tuberosities are not attached, it is possible to access the articulation without the need for arthrotomy. Any prior osteosynthesis material is extracted. Once the pseudoarthrosis focus has been identified, it is debrided, eliminating any fibrous or soft tissue that might be interposed. The head of the humerus is extracted using osteotomy with an oscillating saw. Reaming of the channel and insertion of the stem may be difficult due to translation of the fragments and a poor position of the tuberosities. Nonetheless, osteotomy of the trochiter must be avoided whenever possible (Fig. 3). The humeral stem must be inserted through the portion of remaining annular bone containing the two tuberosities. Chips of spongy bone are obtained from the head of the humerus and are inserted between the diaphysis and the calcar. If there is any erosion of the medial calcar, the fragment remaining is shaped like a letter “C” instead of being a ring. In such cases, the use of large cortical-spongy graft from the head itself is recommended, to be placed in the medial region using the technique described by Lin et al.17 If the stem is cemented and all prior osteosynthesis material has been extracted, care must be taken to ensure no cement escapes through the orifices of the diaphysis. Once the stem is in place, in those cases where it has been necessary to perform osteotomy of the trochiter, this is rebuilt according to the acute fracture technique using non-absorbable sutures. The tuberosities are sutured to each other and with the diaphysis and then the subscapular muscle is re-anchored to the smaller tuberosity. The post-operative period comprises immobilization in a sling for 6 weeks during which time gentle passive exercises may be performed. Active mobilization is only allowed after there are radiological indications of consolidation, generally from 6 weeks on.4
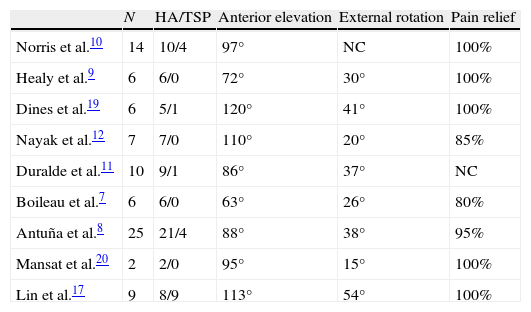
The results of arthroplasties in this context are summarized in Table 2.7–12,17,19,20 The mean values for active elevation and external rotation are 93° (range: 63–120) and 32° (range: 15–54), respectively. Although the improvement in pain is constant in practically all the series, achieving an elevation of the shoulder above horizontal is not to be expected. The outcomes are always less than those obtained with arthroplasties in the treatment of primary arthrosis.8
Results of treating pseudoarthrosis of the proximal humerus with arthroplasty.
| N | HA/TSP | Anterior elevation | External rotation | Pain relief | |
| Norris et al.10 | 14 | 10/4 | 97° | NC | 100% |
| Healy et al.9 | 6 | 6/0 | 72° | 30° | 100% |
| Dines et al.19 | 6 | 5/1 | 120° | 41° | 100% |
| Nayak et al.12 | 7 | 7/0 | 110° | 20° | 85% |
| Duralde et al.11 | 10 | 9/1 | 86° | 37° | NC |
| Boileau et al.7 | 6 | 6/0 | 63° | 26° | 80% |
| Antuña et al.8 | 25 | 21/4 | 88° | 38° | 95% |
| Mansat et al.20 | 2 | 2/0 | 95° | 15° | 100% |
| Lin et al.17 | 9 | 8/9 | 113° | 54° | 100% |
Reverse prostheses have been used with relative success in the treatment of cuff arthropathy and in fracture sequelae.21 Their role in the treatment of pseudoarthroses in the proximal humerus has not yet been clearly elucidated, although it seems a reasonable option in elderly patients with sequelae of fractures in which there is no functioning cuff or discontinuity in the trochiter. Resection arthroplasty has been used in the past but it no longer seems to be a resource worth considering as it has a right rate of complications with the risk of inferior instability and neuritis due to traction of the brachial plexus.
Most of the complications arising after the implantation of an anatomical prosthesis as treatment for pseudoarthrosis stem from the osteotomy of the trochiter. Antuña et al.8 reported that 10 of the 24 patients in which this technique was used presented complications related to osteotomy, such as malunion, pseudoarthrosis or resorption of the trochiter. When this occurred, 100% of the cases obtained unsatisfactory results. Other possible complications are: infection, nerve lesion or persistence of the pseudoarthrosis. When osteosynthesis is performed, the most frequent complications are: discomfort from the osteosynthesis material and the incorrect position of the tuberosities.11 In the case of hemi-arthroplasty, another reason for surgical failure is the appearance of glenoid erosion, whereas the most frequent in total arthroplasties is loosening or anterior or proximal subluxation.8
Malunions of the proximal humerusConsolidation in an incorrect position following a fracture of the proximal humerus may appear after orthopaedic treatment or as a complication of open reduction and osteosynthesis. Malunions habitually present clinically with significant functional limitation of the shoulder, with a variable degree of pain.22 Although this situation may be accepted by elderly patients with scant functional demand, this is not the case with young, active patients.
One of the most frequent limiting scenarios is varus consolidation following fracture of the humeral metaphysis, manifested as a major reduction in anterior elevation and abduction.23 As a consequence of the improper position of the trochiter, the subacromial space is compromised and it bumps into the coracoacromial arch. The approximation of the origin and insertion of the supraspinous ligament diminishes its lever arm thus affecting shoulder function. In addition, the sliding surface between the head of the humerus and the glenoid is diminished.
Classification of malunions in the proximal humerusBeredjiklian et al. classified malunions of the proximal humerus into three groups.24 The first comprises malunions with incorrect position of the tuberosities. The second group is made up of the malunions in which there is incongruence in the articular surface and the third group is those with malposition of the articular fragments. The authors highlight the importance of soft tissue in the pathophysiology of stiffness and functional limitation in the sequelae of proximal humerus fractures.
Malunions in young patients with congruence of the glenohumeral articulation may potentially be treated with osteotomies allowing re-orientation of bone fragments. Nonetheless, in those with glenohumeral incongruence due to an intra-articular step, necrosis of the head or degenerative changes secondary to the fracture, we must consider the indication of an arthroplasty. Elderly patients with scant functional demands are also candidates for arthroplasty.
Evaluation of patients with malunion of the proximal humerusThe dominant symptom in these patients is functional limitation with variable pain. In the physical examination it is important to distinguish between the range of active and passive mobility. The loss of passive mobility may indicate glenohumeral arthrosis with or without capsular stiffness. The presence of a pseudoparalytic shoulder may lead to suspicion of trochiter malunion. The radiological study to be performed must include true anteroposterior and axillary projections. In cases where humeral osteotomy is planned, an X-ray may be taken of the contralateral shoulder to calculate the cervico-diaphyseal angle. In complex cases, CT with three-dimensional reconstruction may be useful.
Treatment options for malunions of the proximal humerusThere are few references in the literature about the treatment of proximal humerus malunions. From a treatment perspective, they could be divided into two groups according to Beredjiklian's classification24: those with malunion of the tuberosities and, on the other hand, those included in groups 2 and 3.
Malunions of the tuberositiesMalunions of tuberosities constitute an entity in its own right. Arthroscopy is a useful tool in these cases to evaluate the displacement of the tuberosities, the status of soft tissue and the joint surface. Furthermore, it allows identification and treatment of intra-articular contractures and subacromial or subcoracoid compromise. Treatment by means of osteotomy of the tuberosities has provided poor outcomes.24 However, new arthroscopic techniques have achieved good functional results. In cases of malunion of the trochin with blockage of rotations arthroscopic debridement and remodelling of the bone block.25 In malunions of the greater tuberosity with a displacement of less than 15mm, it is possible to perform an acromyoplasty, thus diminishing the subacromial compromise.24 In those cases where this is not sufficient, it may be associated with a tuberoplasty in accordance with the technique described by Calvo et al.26
Corrective osteotomiesIn cases where there is defective consolidation of the proximal humerus without involvement of the joint surface, one option is to correct the deformity by means of osteotomy. This technique would be recommendable in young patients where there are no clinical or radiological signs of degenerative changes in the glenohumeral articulation. However, it should be avoided in cases of irreparable breakage of the rotator cuff, angular deformity in multiple planes and in the presence of a nerve lesion or active infection. The surgical technique for varus consolidation of a fracture in the metaphysis was described by Benegas et al.23 as having good outcomes in their series of 5 cases. It consists in a closure osteotomy attempting to reproduce the contralateral cervico-diaphyseal angle. Consolidation was achieved in 100% of cases after 6 weeks and it was necessary to remove the plate in 2 of the 5 cases. All patients presented absence of pain and increase in anterior elevation at the end of the follow-up.
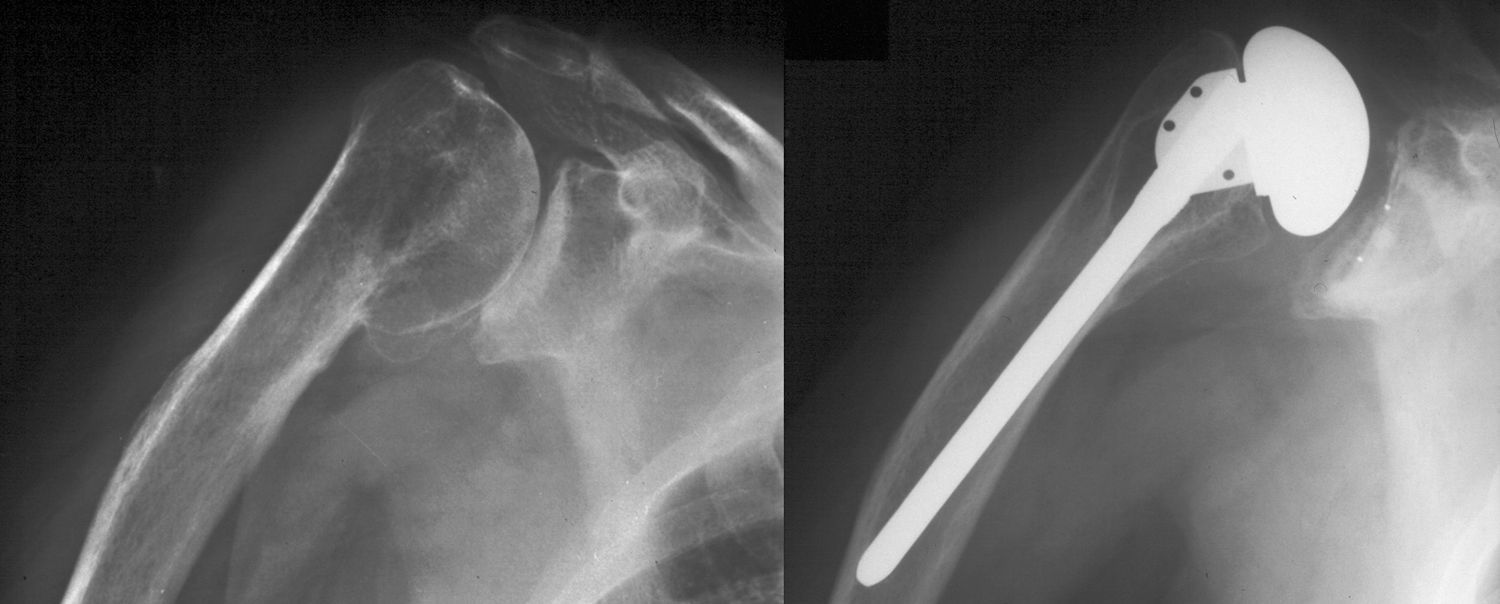
Arthroplasties for malunions of the proximal humerusIn elderly patients with significant involvement of the joint surface, the technique of choice is joint replacement. It normally involves stiff shoulders with subacromial, subdeltoid and subcoracoid adherences. It is frequent to see necrosis in the head of the humerus, ruptures of the rotator cuff and atrophy of the deltoid and subscapular muscles.20 As with surgery of the pseudoarthrosis, the most delicate step is the preparation of the medullary channel of the humerus for insertion of the stem. Osteotomy of the trochiter is to be avoided whenever possible, as this might constrain a poor outcome.7,18,20,22,24 In such cases, there is an option to use short stems or tailor-made implants with curvatures adapted to the deformed anatomy. It is interesting to know that small varus or valgus deviations when implanting the stem are permissible and are not associated with greater rates of loosening2 (Fig. 4). In the highly infrequent event of osteotomy of the trochiter being essential, it must be performed biplanarly leaving enough remaining bone in the cuff to be able to suture it to the diaphysis. After placement of the prosthesis, both tuberosities are fixed to the implant and to the diaphysis with large non-absorbable sutures. It is possible to use autologous bone graft from the head of the humerus or the iliac crest to facilitate consolidation.
(A) Anteroposterior X-ray of the right shoulder in the scapular projection. Malunion of the proximal humerus with the cepahlic fragment consolidated in varus position. (B) Treatment with a total shoulder arthroplasty. A slight placement of the humeral stem into varus position was carried out, in order to avoid performing a lesser tuberosity osteotomy.
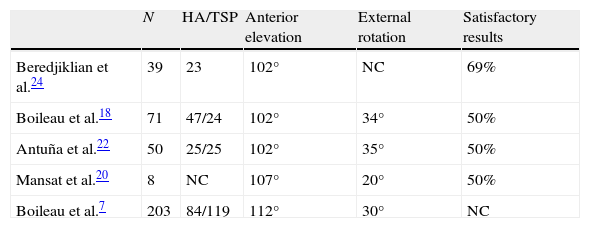
The results of arthroplasty in the sequelae of fractures are inferior to those in patients with primary glenohumeral arthrosis or under treatment for acute fractures in three or four parts.27–30Table 3 shows the published outcomes on the use of arthroplasty as treatment for a malunion of the proximal humerus.18,22 Generally speaking, a reduction in pain is achieved in most cases whereas the functional results are variable, with only a discreet improvement being observed. Several factors seem to constrain the poor functional results, including: age, duration of the symptoms,20 lack of integrity in the cuff with a coracohumeral distance of less than 8mm,20 the performance of trochiter osteotomy,18,20,22 hemi-arthroplasty versus total shoulder prosthesis19 and the duration and intensity of rehabilitation.29
Mansat et al. obtained 64% of satisfactory outcomes in their series of 28 patients with sequelae of proximal humerus fractures treated by arthroplasty.20 The mean active elevation was 107° and 85% of the total reported absence or a minimal presence of pain. Similarly, Boileau et al. published 42% of good or excellent results in 71 arthroplasties, with complication rates of 27%.18 Most of these complications were related to osteotomy of the trochiter. Of all the patients in whom it was performed, none achieved active elevation in excess of 90°. These poor outcomes would be constrained by the devascularization of the tuberosity, which would lead to pseudoarthrosis, malunion or resorption, as also reported by Antuña et al.22 Other possible complications would be intra-operative fractures, nerve lesions, deep infections, heterotopic ossifications, proximal migration and loosening of the implant.
Reverse prostheses might be indicated as a salvage option in older patients with poor bone quality.31,32 Pape et al. have published good results with the use of superficialization prostheses in malunions of the proximal humerus.33 In their series of 28 patients they obtained the best results in sequelae of valgus impacted fractures, with a better final score in Constant's test, better flexion, better abduction and greater patient satisfaction. The overall results were an improvement in the score of 23.2 points on the Constant scale pre-operatively to 55.1 points post-operatively with a mean follow-up of 24 months. Only one case of symptomatic glenoid erosion was detected in this series.
ConclusionThe treatment of the sequelae in fractures of the proximal humerus is probably one of the most difficult challenges for surgeons of the shoulder. They are invariably associated with variable degrees of involvement of the soft tissues, predominantly stiffness due to excessive scarring and shortening of the capsule-ligament structures.
Surgery preserving the proximal humerus is reserved for those cases in which the joint is preserved and the quality of the bone stock is acceptable. When the joint is damaged and poor bone quality prevents proper osteosynthesis or major cavitation in the head of the humerus, then the most recommendable option is a replacement articulation. When the trochiter is conserved and in a good position, good results can be expected from the anatomical prosthesis. In the event of pseudoarthrosis of the trochiter, the most reasonable option is probably a reverse prosthesis. In either case, it is crucial for the patient to understand what should be expected and to be prepared to collaborate in post-operative rehabilitation.
Level of evidenceLevel of evidence V.
Protection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Valencia M, et al. Pseudoartrosis y maluniones de húmero proximal. Rev Esp Cir Ortop Traumatol. 2011;55(5):405–12.