Radial longitudinal deficiency (RLD) includes bone, musculotendinous and neurovascular abnormalities of multifactorial aetiology of the radial side of the upper extremity. Treatment includes improving the length of the limb, the appearance and functioning of the hand. The aim of this study was to present our experience in a series of patients attended over the past 15 years and to describe the clinical and radiological results.
MethodologyA retrospective study of patients with RLD between 2000 and 2016. Variables were analysed and age associations were identified at the time of surgery, sex, laterality, type of deformity according to the modified Bayne–Klug classification, surgical technique, physis damage, associated diseases, functional and radiological results.
Results47 cases of 65 met the inclusion criteria. The average age of surgery was 19 months, 61% female. According to classification 60% were type IV, type III in 19%, type 0 in 17% and type I in 4%. The intervention was centralization 72.3%, radialization 8.5% and one case of lengthening. Ulna osteotomy was performed in 55.3%. There was damage to the physis in 31%. The postoperative radiological position was neutral in 48.9%.
ConclusionsIn patients with centralization at 1year, good clinical and radiological correction were observed, however this was lost over time. The management of soft tissues prior to centralization is believed to give better results. The use of intramedullary nail from the ulna to the carpus could be associated with damage to the distal ulna.
La deficiencia radial longitudinal comprende anormalidades óseas, musculotendinosas y neurovasculares de etiología multifactorial del lado radial de la extremidad superior. El tratamiento incluye mejorar la longitud, la apariencia y el funcionamiento de la mano. El objetivo del trabajo es mostrar la experiencia en una serie de pacientes atendidos en los últimos 15 años y describir resultados clínicos y radiológicos.
MetodologíaEstudio retrospectivo de pacientes con deficiencia radial longitudinal entre 2000 a 2016. Se analizaron variables y se identificaron asociaciones de edad al momento de cirugía, sexo, lateralidad, grado de la deformidad según la clasificación Bayne-Klug modificada, técnica quirúrgica realizada, daño de la fisis, enfermedades asociadas, resultados funcionales y radiológicos.
ResultadosCuarenta y siete casos de 65 cumplían con criterios de inclusión. La edad promedio de la cirugía fue de 19 meses, 61% de sexo femenino. Según la clasificación el tipo IV fue el 60%, el tipo III el 19%, el tipo 0 el 17% y tipo I el 4%. La intervención practicada fue la centralización en el 72,3%, la radialización en el 8,5% y hubo un caso de alargamiento. Se realizó osteotomía de cúbito en el 55,3%. Hubo daño de la fisis en el 31%. La posición radiológica postoperatoria fue neutra en el 48,9%.
ConclusionesEn pacientes con centralización a un año se observa una buena corrección clínica y radiológica, sin embargo esta se va perdiendo con el tiempo. El tratamiento de los tejidos blandos previo a la centralización se cree que permite obtener mejores resultados. El uso de clavo intramedular del cúbito al carpo podría estar asociado con daño de fisis del cúbito distal.
Congenital malformations of the upper limbs are the most common congenital abnormalities after congenital heart malformations.1 They include radial longitudinal deficiency or radial club hand, which covers a spectrum of bone, muscle-tendon and neurovascular abnormalities in the radial edge of the upper limb, which may be absent or abnormally developed. They amount to from a quarter to a third of all upper limb deficiencies, with an incidence that varies from 1 in 5000 to 1 in 100,000 live births in different studies; their prevalence has been reported to be higher in boys, at a ratio of 3:2, and they are bilateral in 38–58% of cases.2–5
There is no exact knowledge of the molecular mechanisms which lead to radial longitudinal deficiencies; environmental, genetic or epigenetic alterations that interfere with the development of the arm in week 4–5 of embryogenesis would be involved in the development of the malformation.1–5
Although radial longitudinal deficiencies may be bilateral, they tend to be asymmetrical and in up to 67% of cases they may be associated with other musculoskeletal or systemic abnormalities: these often include congenital scoliosis, humeral hypoplasia, proximal radiocubital synostosis, congenital luxation of the radial head and rigidity of the fingers.6–8
The syndromes which are often associated with the condition are trisomy 18, trisomy 13, mosaic trisomy 16, Holt Oram syndrome, VACTERL association, thrombocytopenia-absence of radius syndrome, Fanconi anaemia, Rapadilino syndrome and Cornelia de Lange syndrome.3
It has also been linked to exposure to drugs during pregnancy, chiefly antiepileptics such as valproic acid and other related drugs, including thalidomide, Phenobarbital and aminopterin.4,9
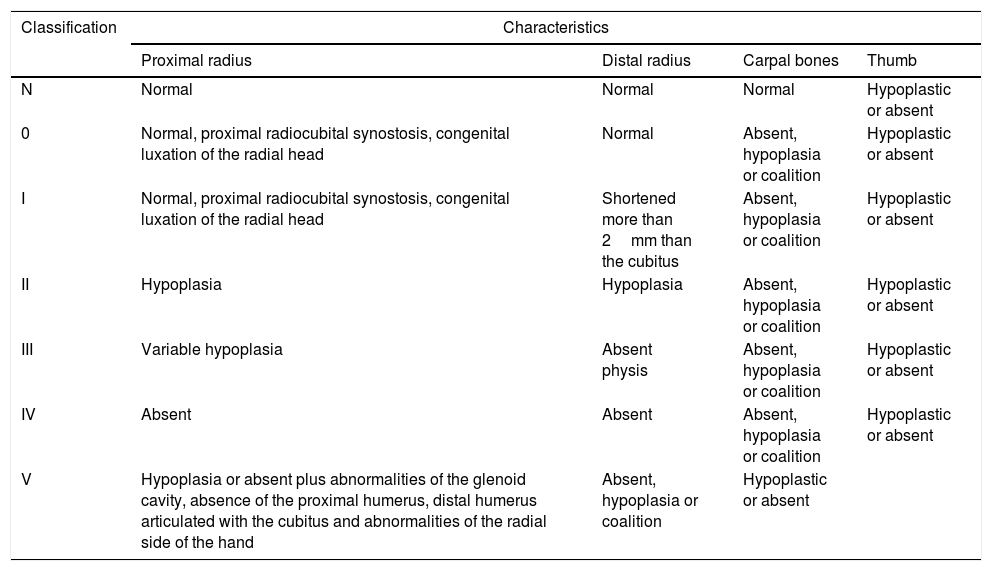
Bayne and Klug10 classified the condition in 4 types (Table 1); James et al. complemented the said classification with type 0, that includes carpal radial bone deficiencies with a normal radial length, and type N that includes isolated abnormalities of the thumb. They showed that thumb hypoplasia or absence and isolated abnormalities of the carpal bone are a mild to moderate form radial longitudinal deficiencies, and that the said abnormalities are always present in the most complicated forms.7
Modified Bayne and Klug classification.
| Classification | Characteristics | |||
|---|---|---|---|---|
| Proximal radius | Distal radius | Carpal bones | Thumb | |
| N | Normal | Normal | Normal | Hypoplastic or absent |
| 0 | Normal, proximal radiocubital synostosis, congenital luxation of the radial head | Normal | Absent, hypoplasia or coalition | Hypoplastic or absent |
| I | Normal, proximal radiocubital synostosis, congenital luxation of the radial head | Shortened more than 2mm than the cubitus | Absent, hypoplasia or coalition | Hypoplastic or absent |
| II | Hypoplasia | Hypoplasia | Absent, hypoplasia or coalition | Hypoplastic or absent |
| III | Variable hypoplasia | Absent physis | Absent, hypoplasia or coalition | Hypoplastic or absent |
| IV | Absent | Absent | Absent, hypoplasia or coalition | Hypoplastic or absent |
| V | Hypoplasia or absent plus abnormalities of the glenoid cavity, absence of the proximal humerus, distal humerus articulated with the cubitus and abnormalities of the radial side of the hand | Absent, hypoplasia or coalition | Hypoplastic or absent | |
Goldfarb et al. include type V, which covers proximal abnormalities of the upper limb such as abnormalities of the glenoid cavity, the absence of the proximal humerus, a distal humerus articulated with the cubitus and abnormalities of the radial side of the hand.11,12
Surgical treatment depends on the degree of involvement, and it varies from not intervening to surgical techniques such as lengthening the radius or centralisation.
Not all of type 0 and N cases require surgical treatment; surgical measures mainly aim to improve thumb function, while interventions at the level of the radius are indicated when there is clearly an angle greater than 20° with impossibility of active extension to the neutral position. This may be achieved by freeing soft tissues and using myotendon transfers, as is the case in type I, although distraction lengthening by external fixation may be considered in the latter type and in type II.8
The most commonly used and popular procedures for types III and IV are centralisation or radialisation in association with tendon transfers.9 The concept of centralisation was suggested by Sayre in 1893; this concept is still valid, with the partial resection of the lunate bone and part of the epiphysis of the cubitus, without affecting the physis.13 The correction is held by a Kirschner nail that passes through the 3rd metacarpal.14 The potential deforming forces have to be balanced by tendon transfers and correction of the angle of the cubitus if it is angled through the osteotomy.4,9
In radialisation, as described by Buck-Gramcko,15 the cubitus is placed radial to the carpal bone rather than in a central position, without the need to resect carpal bones. There is over-correction with cubital deviation. In this case carpi ulnaris extensor tendon transfer is very important, and it is generally found to be of good thickness; it is cut or moved distally up to the diaphysis of the 5th metacarpal bone. The radial extensor tendons, which are almost always hypoplastic and thinner, are transferred towards the cubital side.16
Other surgical options include cubitocarpal arthrodesis and transfer of the second metacarpophalangeal joint.15,17,18 This last technique is more recent and may be more demanding and with a high rate of complications, although it has given better results in terms of a lower recurrence rate, which is the main complication of centralisation.
This work describes the experience of the main author in a series of patients with radial longitudinal deficiency or club hand seen in the last 16 years, describing their clinical and radiological results.
Material and methodThis is a retrospective study of patients diagnosed radial longitudinal deficiency or radial club hand and treated by the main author in the last 16 years, from 2000 to 2016. The inclusion criteria were an age of from 0 to 5 years old, a confirmed diagnosis of radial longitudinal deficiency and a follow-up lasting for at least one year. The variables analysed included: age at the time of surgery, sex, laterality, degree of deformity according to the Bayne and Klug classification and modifications with the O and N types by James et al., and type V by Manske-Goldfarb, surgical technique used, damage to the physis, associated diseases and functional and radiological results.7,8
Data were tabulated for statistical analysis using SPSS 22 software, frequency analysis was performed for all of the records, qualitative variables were shown in absolute and relative frequencies and scale variables were shown as averages and standard deviations. The Chi-squared test was used to compare categorical variables. The results obtained using the physical appearance scale and wrist orientation shown by radiography were compared with the surgical technique used. Differences between the groups were evaluated according to age, sex and the presence of associated diseases. Associated complications were described, together with postoperative ranges of mobility one year after surgery.
The clinical assessment used the position of the hand respecting the forearm according to its cubital or radial deviation as the reference, and the position in flexion or extension respecting the neutral position of 0°, where:
- •
Very good: neutral position 0±5°.
- •
Good: variation greater than 5–10° from the neutral position.
- •
Acceptable: variation greater than 10–20°.
- •
Poor: variation greater than 20–30°.
- •
Very poor: variation greater than 30°.
Parents’ degree of satisfaction with the aesthetic and functional results was evaluated on a scale of from 1 to 5, where 1 corresponded to a very poor result and 5 to a very good result.
Radiological assessment used the angle between the hand and forearm, classified as follows:
- •
Cubital: less than −20°.
- •
Neutral: −20° to 20°.
- •
Radial: 20–30°.
- •
Very radial: greater than 30°.
This study was performed according to the ethical norms based on the Helsinki Declaration, and it was approved by the ethics committee of the University where the study was based. The authors have no conflict of interests to declare in this study, and there were no sources of financing. Likewise, the children's parents’ oral and written consent was obtained for the publication of photographs and data.Results
47 of the 65 cases treated by the author fulfilled the inclusion criteria, of which 11 corresponded to patients with involvement of both limbs, giving a total of 36 patients; of these, 30.5%, almost one third of the total, were patients with bilateral involvement. The patients who only had thumb hypoplasia, type N, were not included in this study and were covered in a previous publication.19
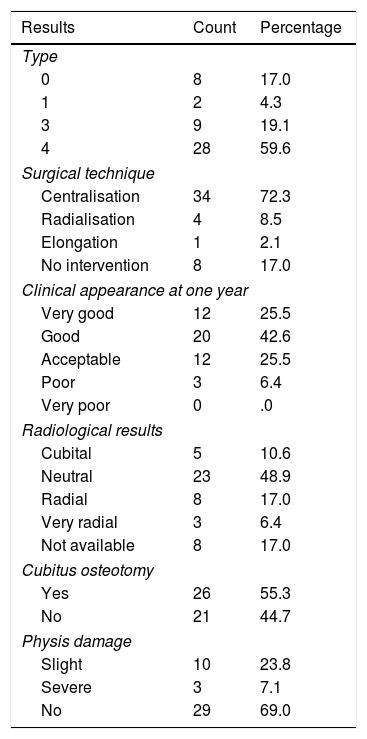
The average age at the time of surgery was 19 months, ranging from 0 to 56 months, although there were more operations at the age of 12 months; a higher prevalence of the female sex was observed, at 61% of cases. For all of the cases the distribution according to Bayne's classification was type IV in 60% of cases, type III in 19% and type 0 in 17%, and finally type I in 4% (Table 2).
Demographic factors in the patients with radial longitudinal deficiency.
| Results | Count | Percentage |
|---|---|---|
| Type | ||
| 0 | 8 | 17.0 |
| 1 | 2 | 4.3 |
| 3 | 9 | 19.1 |
| 4 | 28 | 59.6 |
| Surgical technique | ||
| Centralisation | 34 | 72.3 |
| Radialisation | 4 | 8.5 |
| Elongation | 1 | 2.1 |
| No intervention | 8 | 17.0 |
| Clinical appearance at one year | ||
| Very good | 12 | 25.5 |
| Good | 20 | 42.6 |
| Acceptable | 12 | 25.5 |
| Poor | 3 | 6.4 |
| Very poor | 0 | .0 |
| Radiological results | ||
| Cubital | 5 | 10.6 |
| Neutral | 23 | 48.9 |
| Radial | 8 | 17.0 |
| Very radial | 3 | 6.4 |
| Not available | 8 | 17.0 |
| Cubitus osteotomy | ||
| Yes | 26 | 55.3 |
| No | 21 | 44.7 |
| Physis damage | ||
| Slight | 10 | 23.8 |
| Severe | 3 | 7.1 |
| No | 29 | 69.0 |
There was a predominance of the right side in those patients with unilateral involvement, with 64% of cases, and the results were similar in terms of sex and Bayne's classification, with 60% female sex, while according to the classification, 60% were type IV, 20% were type III and the remaining 20% were types 0 and I.
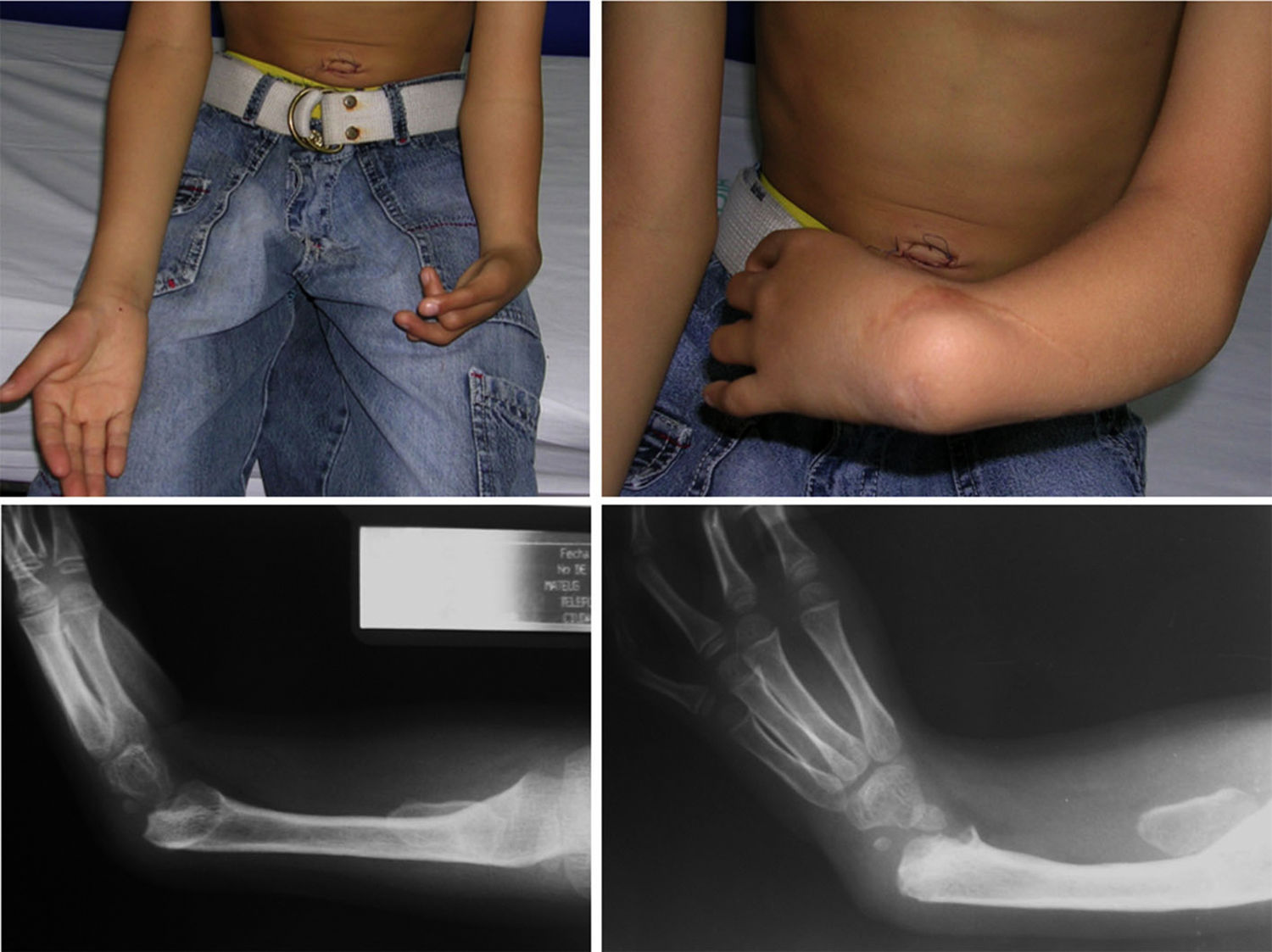
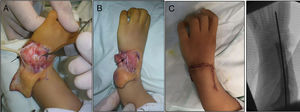
The female sex also predominated among the patients with bilateral involvement, at 63%, and type IV also predominated in 59% of cases, followed by type III at 31%, while the remaining 10% were types 0 and I. 72% of the patients in this group had the same condition in both limbs, while 19% of cases varied between types III and IV, and only one case had one grade 0 limb while the other was grade IV (Figs. 1 and 2).
11% of the patients, a total of 4, had an association with VACTERL, and of these 3 had bilateral involvement; nevertheless, other malformations were identified in individual cases of club foot and pectum excavatum without any direct relationship being established between these variables.
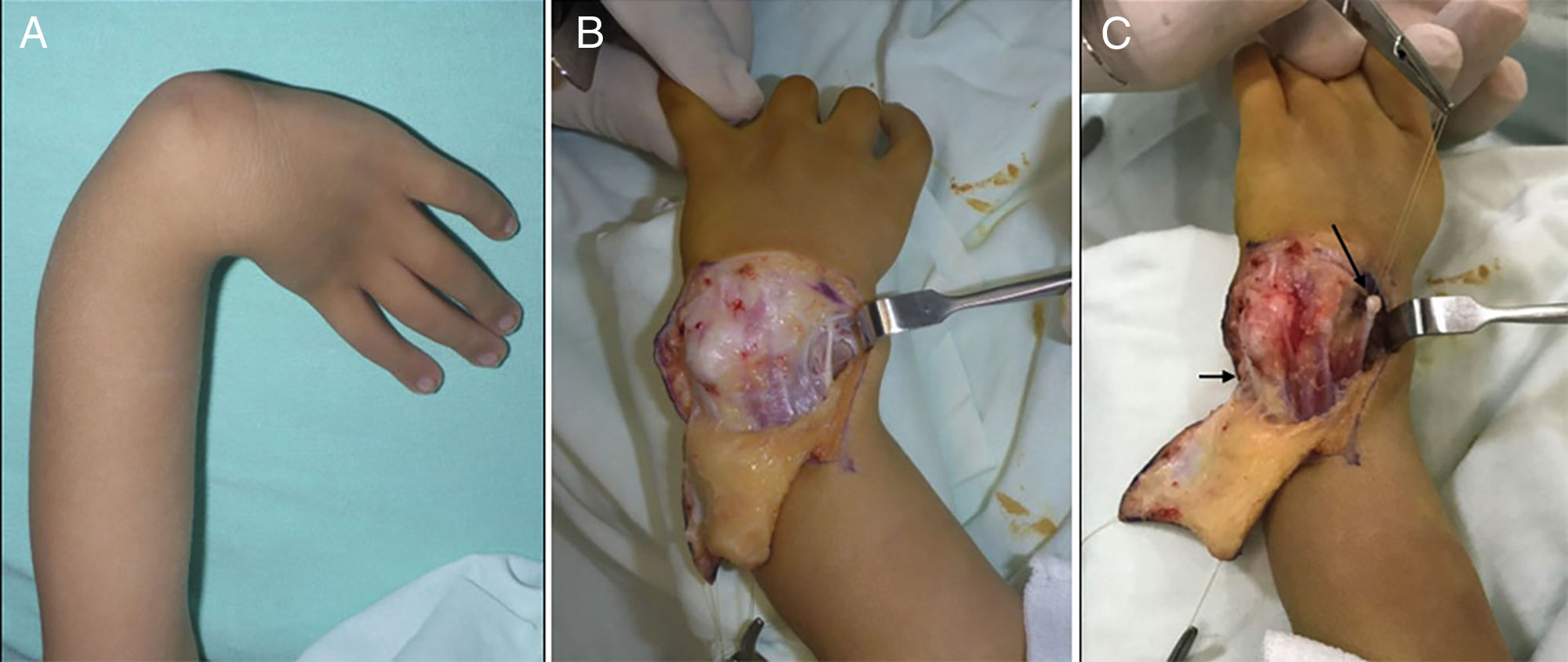
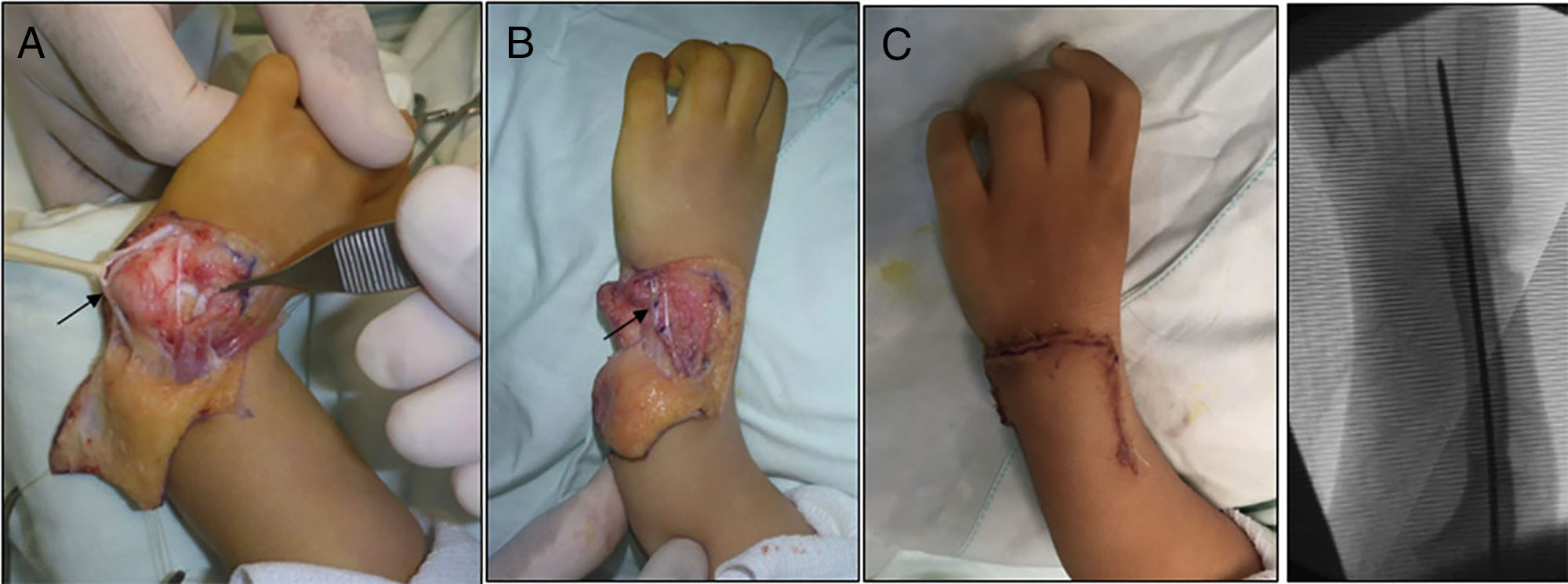
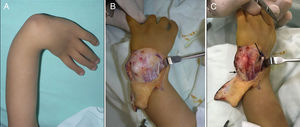
The most widely used surgical techniques were centralisation and radialisation, at 72.3% and 8.5% respectively. Although there were other more complex cases (types III and IV), for type I cases techniques such as an elongation splint was used in one case. Type 0 cases were not operated at wrist level, although 3 of them had grade IIIA and V thumb hypoplasia, so that they were treated surgically later (Figs. 3–7).
(A) Opening the carpal joint and preparing the centralisation of the carpus in the distal end of the cubitus, showing the carpi ulnaris (CU) with a black arrow. (B) The carpus capsuloligamentary tissues have been sutured, the CU has been shortened and the radial extensor has been transferred to the CU. (C) Final immediate clinical and radiological result.
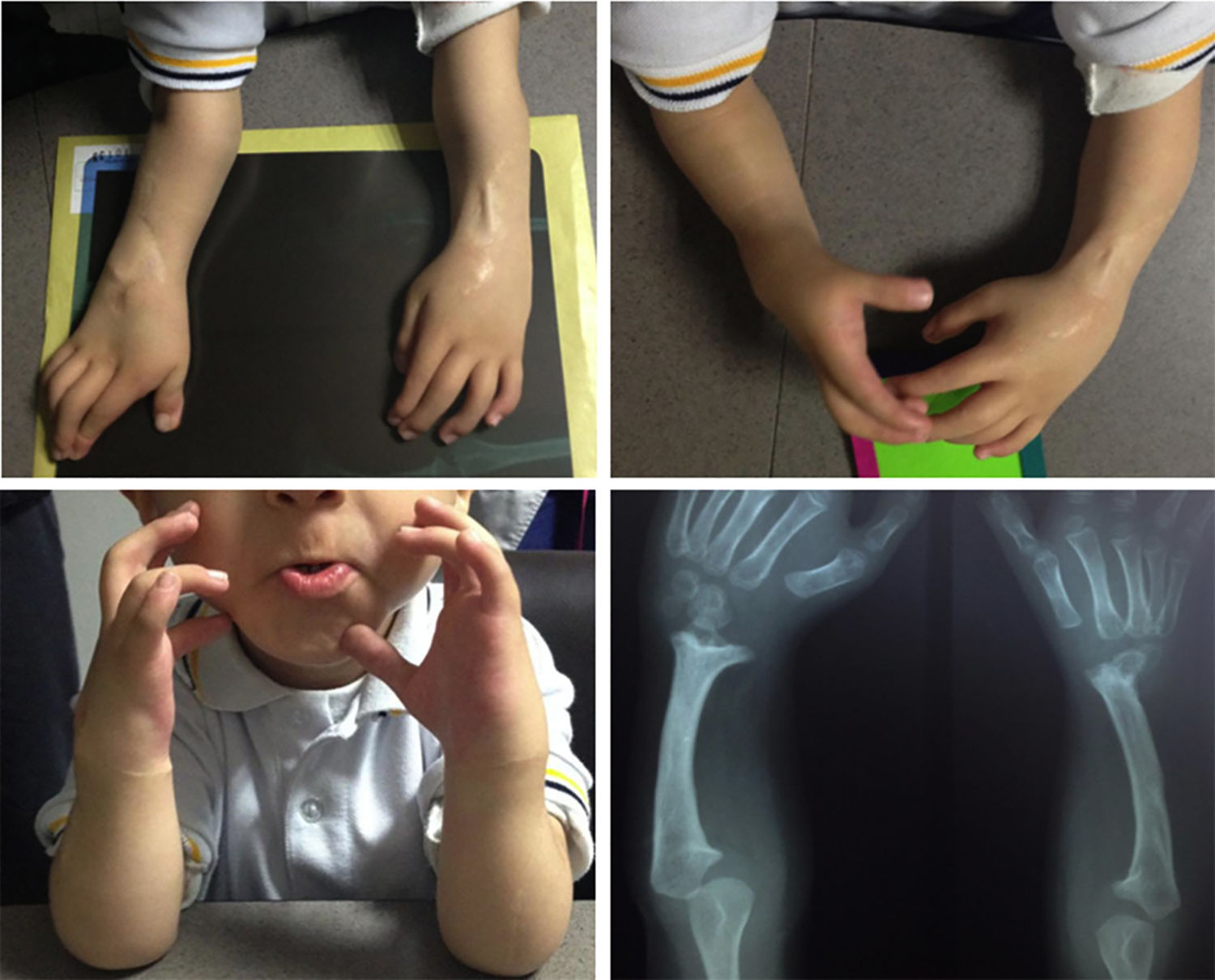
Patient shown in Fig. 3, operated with radialisation of the right hand and centralisation of the left hand. Three years after the operation. Good correction.
In 55.3% of cases osteotomy of the cubitus was necessary to correct the deformity, and of these cases 80% corresponded to a type IV radial longitudinal deficiency.
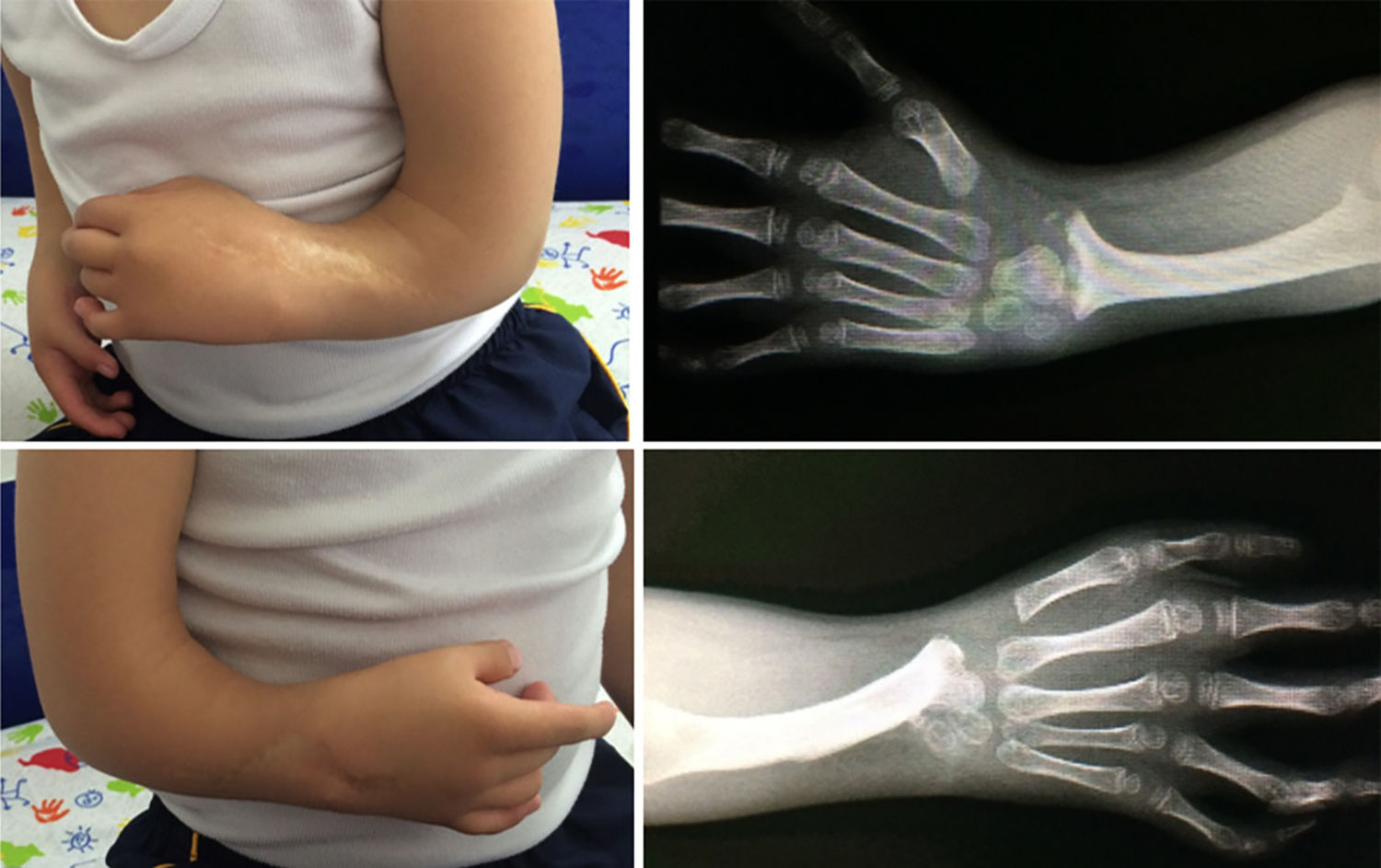
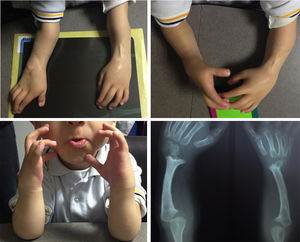
There was damage to the physis in 31% of cases, in the majority of which the damage was slight; in severe cases the appearance was worse after one year in comparison with cases where damage was slight or absent (P=.023) (Figs. 8 and 9).
Patient shown in Fig. 6; 6 years after the operation the correction achieved initially has been lost, with palmar and radial deviation of the hand. Radiologically a major alteration of the radium physis is visible.
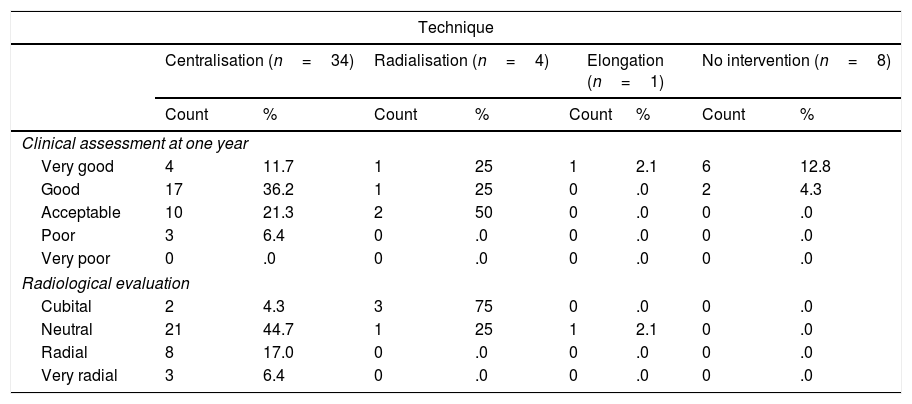
Appearance after one year in patients subjected to centralisation was good in 36.2% of cases, very good in 11.7% and acceptable or negative in 27.7% of cases; 18 patients were assessed after more than 2 years and in one third of them the appearance was found to have deteriorated (Table 3).
Appearance at one year and radiological evaluation according to the technique used in patients with radial longitudinal deficiency.
| Technique | ||||||||
|---|---|---|---|---|---|---|---|---|
| Centralisation (n=34) | Radialisation (n=4) | Elongation (n=1) | No intervention (n=8) | |||||
| Count | % | Count | % | Count | % | Count | % | |
| Clinical assessment at one year | ||||||||
| Very good | 4 | 11.7 | 1 | 25 | 1 | 2.1 | 6 | 12.8 |
| Good | 17 | 36.2 | 1 | 25 | 0 | .0 | 2 | 4.3 |
| Acceptable | 10 | 21.3 | 2 | 50 | 0 | .0 | 0 | .0 |
| Poor | 3 | 6.4 | 0 | .0 | 0 | .0 | 0 | .0 |
| Very poor | 0 | .0 | 0 | .0 | 0 | .0 | 0 | .0 |
| Radiological evaluation | ||||||||
| Cubital | 2 | 4.3 | 3 | 75 | 0 | .0 | 0 | .0 |
| Neutral | 21 | 44.7 | 1 | 25 | 1 | 2.1 | 0 | .0 |
| Radial | 8 | 17.0 | 0 | .0 | 0 | .0 | 0 | .0 |
| Very radial | 3 | 6.4 | 0 | .0 | 0 | .0 | 0 | .0 |
The degree of satisfaction was satisfactory, at 4 or 5 in 46.8% and 19.1% of cases, respectively. It was acceptable in 25.5% and unsatisfactory, at 1 or 2, in 6.38% and 2.12% of cases, respectively.
For all of the techniques the postoperative radiological appearance was neutral in 48.9% of cases, cubital in 10.6% and radial in 17%. In the cases of radialisation the radiological appearance showed cubital deviation in 75% of cases, one of which had a very poor outcome due to extreme cubital deviation, while one case has a very good result with a neutral position, and the only cases operated with an elongation splint was also neutral (Table 3).
Regarding the range of mobility (excluding the patients who were not operated), which runs from the maximum degree of flexion to the maximum degree of extension, the average was found to stand at 20.65°. The maximum flexion was 40°, and the point of maximum extension was also 40°, with a standard deviation of 13.96°.
DiscussionRadial club hand falls within the spectrum of radial deficiencies. It was first described in 1733 by Petit,4 and it takes the form of radial hypoplasia with shortening of the forearm and radial deviation of the wrist in the shape of a golf club. It is one of the most complicated and rarest forms of radial deficiency, and it is also a greater surgical challenge.
The symptoms depend on the degree of abnormality of the radial components of the upper limb, especially the length of the radius. This is evaluated in the wrist according to the position of the radial physis, which should be located more distal to the cubitus physis (ulnar variance of from 2.3 to 2.8mm).7,10,20
Types 0 and N are the most common varieties, which together make up 52% of radial longitudinal deficiencies, followed by type 4, with 27%, and type 1 with 15%. Type 0 and type 1 are the ones most often associated with proximal radiocubital synostosis and congenital luxation of the radius head, at 11% and 44%, respectively.7,12
Treatment aims to correct the radial angle and the flexed position of the carpus (palm and radial subluxation), optimising the length of the limb to improve the appearance and functioning of the hand, followed by reconstruction of the hypoplastic thumb when required.6
This study reviewed 39 cases operated due to radial longitudinal deficiency, 34 were operated using centralisation, and of these 91% had a clinical result that was either acceptable or very good, while 49% had a neutral or cubital radiological result after one year of follow-up. All of the cases operated using radialisation were found to give a clinical result that was either acceptable or better and radiologically neutral or cubital. However, these findings correspond to a group of only 4 patients, so that it is not possible to generate significant conclusions in comparison with other techniques. A statistically significant correlation was identified between the use of cubital osteotomy and an intramedullary nail with damage to the physis, and the majority of lesions were slight; when damage to the physis was severe with closure of the same, deformity was found to increase over time. The use of an intramedullary nail in the cubitus, its thickness and time, is a situation that should be taken into account.
The average age at the time of surgery was 1 year and 7 months; however, ideally the treatment should be started earlier with the use of serial castings or splints, with the aim of improving the length of the soft tissues before definitive surgery at around one year old.6,7 We had 3 cases in which the results were unfavourable, and their appearance after one year was poor.
In a series of cases of 10 patients with radial longitudinal deficiency, from 1990 to 2000,21 12 centralisations were performed using serial splints from the age of 6 months old; centralisation was maintained using Kirschner nails, achieving statistically significant correction of the radial deviation at the end of the follow-up of 79.5° at an average of 19.5°. Although it was not possible to implement functionality scales in our study, no statistically significant correlations were found in terms of the range of movement obtained between these functional measurements and the techniques used, so that more studies are required into the functional benefits of the different techniques.
In another series, 23 patients were subjected to a previous programme of elongation of the soft tissues, although in one case this was insufficient and a circular splint had to be used. Cubital osteotomy was performed in patients with a hand-forearm angle greater than 30°. The results showed significant differences between the pre- and postoperative angle after a follow-up period of 17 months.22
In spite of the good results found with distraction to improve the soft tissues prior to centralisation, Manske et al.8 reported the comparative results of only performing centralisation vs. doing so with previous distraction of the soft tissues using a circular splint; they found that centralisation with or without distraction of the soft tissues terminated in an improved wrist alignment, and that distraction facilitates centralisation. However, they did not show better results for radial deviation, recurrence of the deformity or volar subluxation in comparison with the cases without treatment of the soft tissues.
Goldfarb et al.10 studied the effect of treating the soft tissues prior to centralisation with a circular splint in 6 patients, with a follow-up period of 17 months. They found a marked improvement in alignment, which passed from 72 radial degrees to 8 cubital degrees, and they also obtained good early radiological and clinical results.8,10
It was very difficult to analyse the previous treatment of soft tissues with our patients, as the type of patient and their social conditions strongly hindered previous treatment with splints or casts to improve the soft tissues. In the few patients in which this treatment was possible, we believe it made it possible to reduce the suffering of the flaps of skin used in surgery.
In the cases that we have followed up during more than 5 years, we found that in spite of good initial correction this was gradually lost, and although radiologically the cubitus may be seen inside the carpus, it is angled.
Level of evidenceLevel of evidence III.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Vergara-Amador E, López Rincón L, Herrera Rodríguez S. Deficiencia radial longitudinal. Análisis de resultados clínicos y radiológicos. Rev Esp Cir Ortop Traumatol. 2019;63:217–226.