The transpsoas approach, also known as extreme lateral interbody fusion (XLIF), to the lumbar spine is a novel minimally invasive technique with positive clinical outcomes and a low complication rate. There is a low risk of bleeding, due to this approach causing less soft tissue disruption than traditional spine surgery, but segmental arteries and great vessels can be damaged. Retroperitoneal haematoma is a major complication, with few cases reported. This is the first case reported in a Stand-alone XLIF and also the first case reported with haemorrhagic shock. Non-specific symptoms such tachycardia, hypotension, and anaemia are the most prevalent in this complication. With this case, our aim is to describe serious complications related to XLIF.
El abordaje lateral transpsoas a la columna lumbar es una técnica mínimamente invasiva cada vez más usada debido a sus buenos resultados y a su tasa de complicaciones baja. El sangrado de este tipo de cirugía es escaso ya que la disección de partes blandas es mínima comparada con la cirugía vertebral tradicional, pero las arterias segmentarias y los grandes vasos pueden ser lesionados. Hasta ahora, hay muy pocos casos descritos de haematoma retroperitoneal mediante este abordaje pero este es el primero en una fusión lumbar intersomática mediante abordaje lateral transpsoas (XLIF) sin instrumentación añadida y el primero con shock hemorrágico. Los síntomas del haematoma retroperitoneal son inespecíficos, siendo los más prevalentes la taquicardia, la hipotensión y la anaemia. Con este caso pretendemos mostrar que, a pesar de los buenos resultados de esta técnica, no está exenta de complicaciones graves.
Lumbar arthrodesis, which is often combined with direct or indirect decompression of the lumbar canal, is frequently used to treat degenerative processes of the lumbar column.
Although the posterolateral approach is still the most commonly used to perform vertebral fusion, the current tendency is to combine this with anterior (interbody) fusion to increase the stability of the arthrodesis.1
Many approaches have been described to perform anterior fusion, including posterior (PLIF), transforaminal (TLIF), anterior (ALIF) and now the lateral transpsoas approach (XLIF). This approach minimises the risk of vascular and neurological complications deriving from approaches such as the ALIF,2 while it also leads to minimal muscular damage. On the other hand, intraoperative neuromonitoring techniques have to be used to prevent lumbar plexus lesion.3
XLIF consists of the extralateral approach to the intervertebral disc from the oblique muscles of the abdominal wall, accessing the retroperitoneum and going through the psoas. This permits a considerable exposure of the intervertebral disc, together with broad discectomy and the positioning of a larger and more stable interbody box, while keeping both the annulus and the anterior longitudinal ligament, leading to a large area for fusion.4
The publications that were revised contain few descriptions of complications with this technique in comparison with the approaches described previously. As well as mobilisation of the implant and involvement of the lumbar plexus in approximately 8.6% of cases, other complications which are serious although they are less frequent have to be taken into account. In spite of the light bleeding which occurs in this approach, and which has also been described in other series, retroperitoneal haematoma is a serious complication that appears in this type of surgery. It has not been described beforehand in patients subjected to XLIF without subsequent additional instrumentation. Its lack of specific clinical symptoms may delay diagnosis. Our aim here is to describe complications of this type and to show how to avoid them to prevent complications and achieve surgery that is both satisfactory and safe.
Clinical caseA 65 year-old woman referred to our Spinal Column Unit due to chronic lumbar pain irradiating to the lower right limb (LRL). Relevant personal factors included moderate obesity, arterial hypertension and an aortic valve prosthesis implanted in 2012. The latter was complicated by a cardiac block during the postoperative phase. Due to this condition the patient was treated with Acenocumarol, which was withdrawn 7 days before surgery (the final dose of Enoxaparin was administered the day before surgery).
In physical examination, the patient presented lumbar pain irradiating to the LRL and occasionally to the LLL. Although there was no motor deficit the patient mentioned neurogenic claudication after walking 50m. Additionally, the Lasegue and Bragard manoeuvres were positive in the LRL. In spite of conservative treatment with morphine patches after evaluation by the Pain Unit, the patient did not undergo any clinical improvement of the pain.
X-ray study in 2 projections showed no signs of acute disease, although degenerative signs were observed ((Fig. 1A and B). Magnetic resonance imaging could not be used due to the valve implant. Lumbar computerised axial tomography showed L3–L4 and L4–L5 discopathy, as well as spondolytic and spondyloarthrotic alterations that led to canal stenosis, fundamentally in L4–L5 (Fig. 1C).
(A) Anteroposterior lumbosacral X-ray while standing. (B) The same, with a lateral projection. The arrow points to the visibly reduced L4–L5 space and the degenerative alterations such as the anterior osteophyte. (C) Image showing the presence of air in the L4–L5 space that makes manifest the disc degeneration in the said space and its reduction in height.
The decision was taken to perform a circumferential arthrodesis at the said levels. In the first surgical operation a single right XLIF was used to implant 2 interbody (XLIF) devices in L3–L4 and L4–L5, with the aim of bringing about an indirect decompression by increasing the height of the disc and the area of the foramen. Intraoperative neurophysiological monitoring was within normal limits and no complications were detected during surgery.
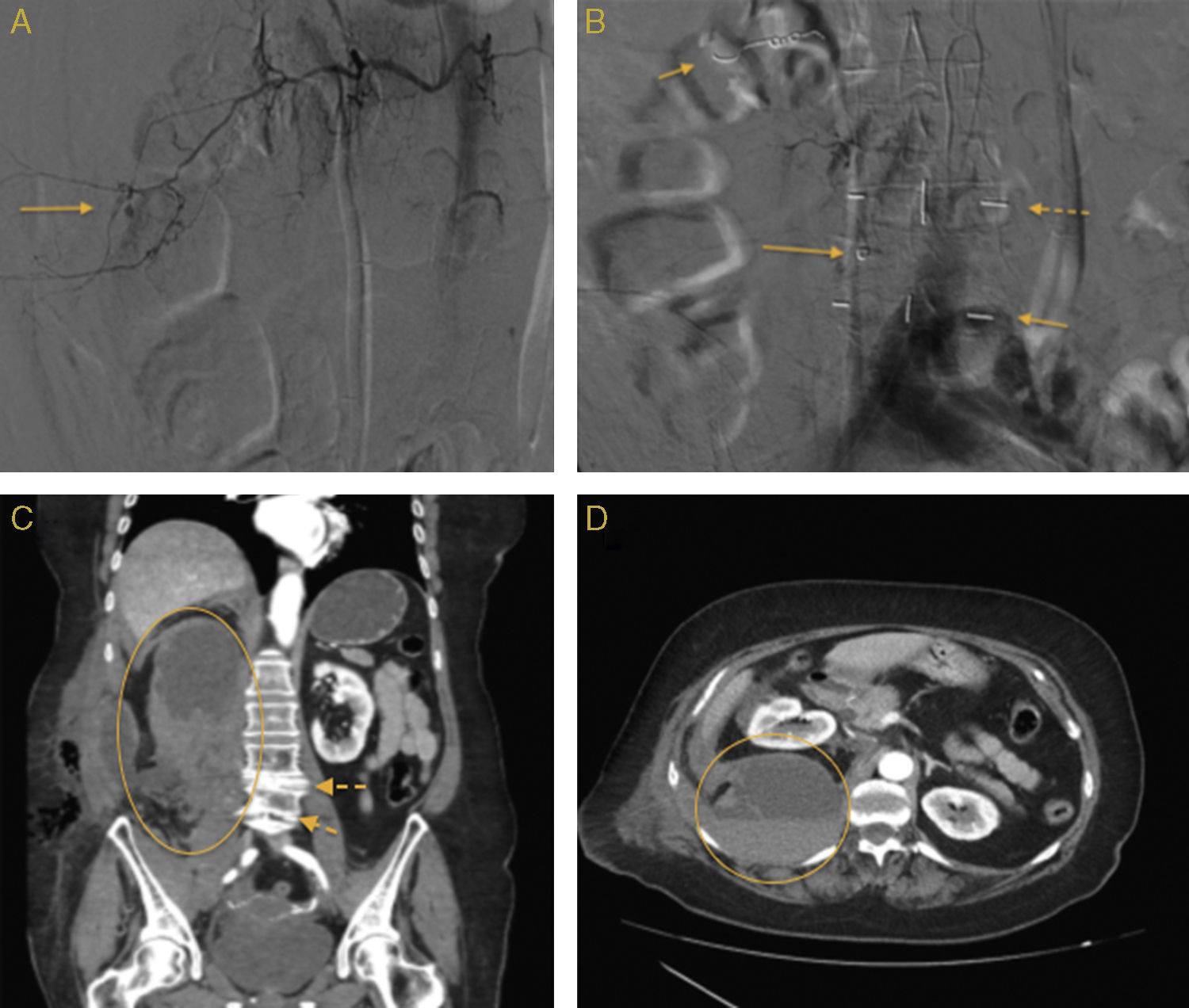
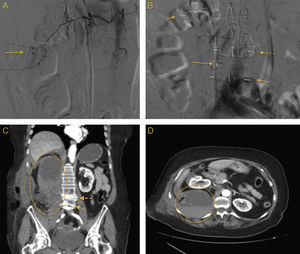
5 days after surgery the patient suddenly presented abdominal pain accompanied by vegetative cortex, with an arterial pressure of 90/50, 90lpm, sweating and anemization. Abdominal computerised axial tomography showed active retroperitoneal bleeding and a large retroperitoneal haematoma measuring 15cm×9cm×8cm that displaced the right kidney forwards (Fig. 2C and D). Abdominal aorta, pelvic and selective right L2, L3 and L4 lumbar artery arteriography subsequently showed active bleeding from a branch of the L2 segmentary artery (Fig. 2A). Its afference was selectively catheterised and it was embolised and blocked using spheres and coils. A pseudoaneurismatic image was also observed hanging from lumbar segment L4 at a paravertebral level that also occluded the pseudoaneurism distally. This branch was embolised with fibre coils, and it was occluded (Fig. 2B).
(A) Selective arteriograph image showing bleeding (arrowed) in the arterial branch hanging from the L2 segmentary artery. (B) The coils (continuous arrows) are visible following embolisation of the L2 segmentary arteries (top left arrow) and the L4 artery (lower continuous arrow). The dashed arrows show the XLIF radiomarkers in the L3–L4 spaces (top arrow) and in L4–L5 (bottom arrow). (C) Coronal plane CT scan showing the large retroperitoneal haematoma (yellow area) and both XLIF (dashed arrows). (D) Axial plane CT scan image showing the large haematoma (yellow circle) that displaces the kidney forwards.
Due to the anemization 3 red blood cell concentrates and one frozen fresh plasma concentrate were transfused.
The patient presented no neurological complications during her hospitalisation. It should be pointed out that following this complication the patient refused the second phase of surgery, which consisted of percutaneous fixing with pedicle screws. The patient was finally discharged after 10 days with no lumbar or radicular pain, progressing from a lumbar pain VAS score of 8 to 3, and a leg pain VAS score falling from 10 to 3.
DiscussionThe minimally invasive lateral approach is a relatively new technique for interbody fusion. It makes it possible to insert a large interbody implant into a part of the vertebra where the bone is stronger. It also minimises vascular risk as it requires a smaller dissection that avoids the need to manipulate and retract large vessels, which had given rise to serious vascular complications in the anterior approach.5 Nevertheless, the fact that the surgical field is smaller may increase the risk of a vascular lesion going unnoticed.
The complication rate with this type of surgery is hard to establish, due to differences in terms of its indications and the data recorded. However, the complication rate for XLIF stands at from 2% to 30.4%,6 described as lower in about 20% of cases and higher in about 8.6% of cases.7 The most common symptoms are postoperative discomfort in the thigh in from 1% to 60.1% of cases. This may be transitory, and it generally disappears a few weeks after the operation. In spite of this, loss of muscular strength may arise in up to 25% of the patients in some series, and this may sometimes last for up to 6 months.
Nevertheless, more serious complications have also been recorded. These include intestinal perforation, infection, nerve and motor lesions, pleural bleeding, haemodynamic instability, pulmonary embolism, ileotomy and durotomy (during the subsequent instrumentation).8
Longer series have been published such as that by Rodgers et al.9, which describe complications after 600 patients operated using XLIF with 741 levels implanted. These complications occurred in 6.2% of the patients. No infections, vascular or intraoperative intestinal lesions were recorded in this series, and 1.8% of patients were operated again.
Although the vascular complications rate described for the ALIF technique is higher than is the case for XLIF, one case of vascular lesion during XLIF surgery has been described.10 Nevertheless, hematomas of this type may be asymptomatic, and as no CT scan is performed they may go unnoticed.
In our experience, after 65 patients and 89 levels operated using XLIF we have had few complications. The infections rate is 0% and the rate of major complications per segment operated stands at 6.7%. Of these complications, there were 2 severe neurological lesions, classified as such as they caused a reduction of at least one point in the Medical Research Council (MRC) modified strength scale after the initial examination. These lesions were resolved in a period of 6 months.
We have not found any similar case in the literature we revised, so that we consider this complication to be exceptional. The surprising images as well as the absence of similar cases mean that this case has a high educational value for the prevention of complications in a new and increasingly used technique such as XLIF. We therefore wish to share our experience with other professionals working in the field of spinal disease, given that the early diagnosis of this complication may be essential to save the life of the patient. To prevent complications of this type we recommend the use of haemostatic agents and direct visual examination of the space before the wound is closed.
Lastly, we believe that in spite of this complication, XLIF is a safe and easily reproducible technique that achieves a high success rate when it is properly indicated. It also has the advantage of reducing the high rate of complications when traditional spinal surgery is used.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of persons and animalsThe authors declare that no experiments took place in human beings or in animals for this research.
Data confidentialityThe authors declare that no patient data appear in this paper.
Right to privacy and informed consentThe authors declare that no patient data appear in this paper.
We would like to thank doctors Manuel Noriega-Bastos and José Rey del Castillo for their collaboration.
Please cite this article as: Peiró-García A, Domínguez-Esteban I, Alía-Benítez J. Haematoma retroperitoneal tras fusión lumbar intersomática mediante abordaje lateral transpsoas (XLIF): revisión de literatura a propósito de un caso. Rev Esp Cir Ortop Traumatol. 2016;60:330–334.