To determine the risk factors influencing in-hospital mortality and/or increased hospital stay in patients older than 65 years with proximal femur fracture.
MethodsRetrospective study of patients aged over 65 years operated on for hip fracture between January 2015 and December 2017. Medical, psychological, functional and analytical comorbidities present at admission as well as treatment, complications and analytical follow-up during admission and functional status and residence at discharge are studied for a total of 54 variables. A bivariate analysis was performed using a composite endpoint between in-hospital mortality and the increase of more than 10 days of hospital stay.
Results360 patients were included with a mean age of 84 years. 75% were women and 53.5% suffered a pertrochanteric fracture. The mean number of comorbidities per patient was 2.7 (0–7), the most frequent being hypertension, dementia and diabetes. In-hospital mortality was 3.6% (n: 13) and mean hospital stay was 8.4 days (1–35), with 16.4% exceeding 10 days. The presence of medical complications (P < .001), hemoglobin level at admission (P < .001), arterial hypertension (P = .012), obesity (P = .018) and parkinson (P = .034) were related to the occurrence of the studied cut-off point.
ConclusionArterial hypertension, obesity, Parkinson’s disease, hemoglobin level at admission and occurrence of medical complications are variables that increased the risk of in-hospital mortality and/or a hospital stay above 10 days in patients older than 65 years with proximal femoral fracture.
Determinar los factores de riesgo que influyen en la mortalidad intrahospitalaria y/o el incremento de la estancia hospitalaria en pacientes mayores de 65 años con fractura del fémur proximal.
Material y métodosEstudio retrospectivo de pacientes de edad superior a 65 años intervenidos por fractura de cadera entre Enero de 2015 y Diciembre de 2017. Se estudian comorbilidades médicas, psicológicas, funcionales y analíticas presentes al ingreso así como tratamiento, complicaciones y seguimiento analítico durante el ingreso y estado funcional y residencia al alta para una total de 54 variables. Se realiza un análisis bivariante mediante un punto de corte o endpoint compuesto entre mortalidad intrahospitalaria y el incremento de más de 10 días de estancia hospitalaria.
Resultados360 pacientes fueron incluidos con edad media de 84 años. El 75% eran mujeres y el 53,5% sufrió una fractura pertrocantérea. La media de comorbilidades por paciente fue 2,7 (0–7) siendo las más frecuentes la hipertensión arterial, demencia y diabetes. La mortalidad intrahospitalaria fue del 3,6% (n: 13) y la estancia hospitalaria media fue de 8,4 días (1–35), estando el 16,4% por encima de los 10 días. La presencia de complicaciones médicas (P < .001), nivel de hemoglobina al ingreso (P < .001), hipertensión arterial (P = .012), obesidad (P = .018) y parkinson (P = .034) se relacionaron con la aparición del punto de corte estudiado.
ConclusiónLa hipertensión arterial, obesidad, parkinson, el nivel de hemoglobina al ingreso y aparición de complicaciones médicas son variables que aumentaron el riesgo de la mortalidad intrahospitalaria y/o una estancia hospitalaria por encima de los 10 días en pacientes mayores de 65 años con fractura proximal del fémur.
Hip fractures are considered as the highest complication in terms of morbimortality and financial healthcare burden after osteoporosis in the geriatric population.1 It has a huge impact on the health systems worldwide, with 300,000 cases occurring per year in the United States2 and approximately 36,000 cases per year in Spain.3 It has been estimated that in the year 2050 six million cases per year will occur worldwide.4
Patient profile is fragile, and has reduced functional and cognitive capacity. This, together with a hip fracture predisposes them to suffering from major adverse effects during their hospital stay and often leads to a prolonged hospital stay and an increased risk of mortality. Nikkel et al.5 also related the increase in hospital stay with mortality in the first month following discharge.
Several medical, demographic and psychosocial factors have been linked to the increase in hospital stay.6–11
Intrahospital mortality of a patient with a hip fracture ranges between 4.5% and 11.4%6,7 and there are also multiple, varied factors related to this.12–14
No broad concordance between risk factors for prolonged stay and intrahospital mortality exists. As a result, studying the common factors may help to identify clearly those patients with a higher risk of suffering these adverse effects in the hospital environment.
The aim of this study was to determine the risk factors associated with intrahospital mortality and/or the increase in hospital stay above 10 days in patients over 65 years of age who had been operated on for proximal femur fracture.
Material and methodsStudy designRetrospective analytical study conducted between January 2015 and December 2017 in a University Hospital which serves a population of 216,610 inhabitants.
Patient selectionInclusion criteria of the study patients were patients who were hospitalised with a diagnosis of proximal femur fracture, who were operated on for this reason and were aged over 65. Exclusion criteria were conservative treatment, pathological fracture, polytrauma, lateral hip fracture and a history of previous hip fractures.
Data collectionData for the study was collected previously, with prior consent to documentation and clinical admission, from the data on the Abucassis, Mizar and Orion Clinical platforms, and hospital medical records obtained from operating theatre files. All data obtained were recorded on a database designed for this study.
Evaluation and follow-upAfter their arrival at the emergency services, the admission of the patient was performed by the Orthopaedic and Trauma Surgery (OTS) unit, registering the patients and collecting their personal data and history.
During their stay, follow-up was performed by the internal medicine services, together with the OTS, with the latter in charge of data collection such as complications, treatment and adverse effects occurring during stay, together with the distribution and collection of questionnaires to patients, and family members and the hospital discharge variables.
All patients were assessed by the anaesthesiology unit. Preoperative antibiotic prophylaxis was performed with cefazolin and vancomycin in the case of allergies and the antithrombotic prophylaxis was the same for all patients. The type of treatment was decided according to type of fracture and OTS unit criteria.
Definition of collected variablesThe variables studied prior to the fracture were age (lower or equal to 84 years, between 85 and 89 years, or over 90 years), sex (male or female), type of hip fracture (intracapsular: subcapital fracture or extracapsular: pertrochanteric and subtrochanteric fractures) side (right or left),place or residence of the patient (own home or old people’s home), day of admission (from Monday to Sunday), presence (yes/no) of anticoagulant, antiplatelet (type) treatment and previous treatment for osteoporosis, presence or not of medical comorbidities (hypertension, atrial fibrillation, chronic obstructive pulmonary disease [COPD], cerebral vascular disuse, coronaryopathy, kidney failure, a history of neoplasms, hypothyroidism, obesity, Parkinson’s disease, dementia, heart failure, rheumatic disease, total number of comorbidities, psychiatric comorbidities,(background of anxiety, depression, obsessive convulsive disorder, schizophrenia or bipolar disorder), haemoglobin on admission (serums levels in g/dL), serum creatinine levels (mg/dL), sodium (mmol/l), potassium (mmol/l), leukocytes (10e9/l), lymphocytes (%), platelets (10e9/l), albumin (g/dL), Charlson index,15 classification of the American Society of Anesthesiology (ASA).16 The Katz function indexes were collected, together with ability to walk (Palmer), Womac scales, Merle and physical and mental SF12, and minimental test (0–10) on the functional and cognitive status of the patient prior to the fracture, with data supplied by the patient or family members.17–21
During hospital stay several variables were collected: days of delay to surgery (infection, mobilisation of osteosynthesis or prosthesis, peri-implant fracture), medical complications (infections not relating to surgical site, acute myocardial infarction (AMI), vascular disease of the brain (S), days of hospital (total days and whether days were under or equal to 10 or more than 10), postoperative haemoglobin levels, presence of preoperative and postoperative blood transfusion and hospital death. Destination at discharge was assessed
Statistical analysisComorbidities were coded as dichotomous variables, with the presence or absence of them. Quantitative variables were presented as means and standard deviation and qualitative as percentages.
For analysis of the appearance of adverse effects of the study an endpoint was fixed in the form of the variable composed by the presence of intrahospital mortality and/or hospital stay above 10 days.
Bivariate analysis was made between the explanatory variables and the presence of the endpoint variable. For qualitative variables the X2 test was used and for continuous variables the Student’s t-test was used or the parametric Mann-Whitney U test
For data study and analysis P < .05 was considered a significant value.
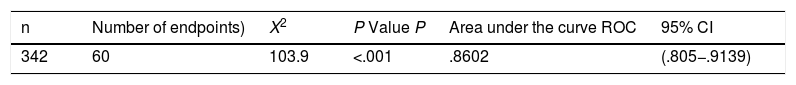
To estimate the magnitudes of the endpoint associations with explanatory variables, a logistic regression multivariate model was adjusted, estimating the odds ratio (OR) of association, together with confidence intervals of the corresponding 95%. (95%CI) The selection process of variables took place in backward steps to obtain an optimal model, based on the Akainke Information Criterium (AIC). Possible variables of confusion were taken into consideration. Goodness-of-fit indicators were estimated such as the X2 value and predictive indicators such as the area under the (ROC), as well as its 95% CIi for the endpoint variable.
The statistical programme SPSS v.25 and the R programme v.3.5.1. were used.
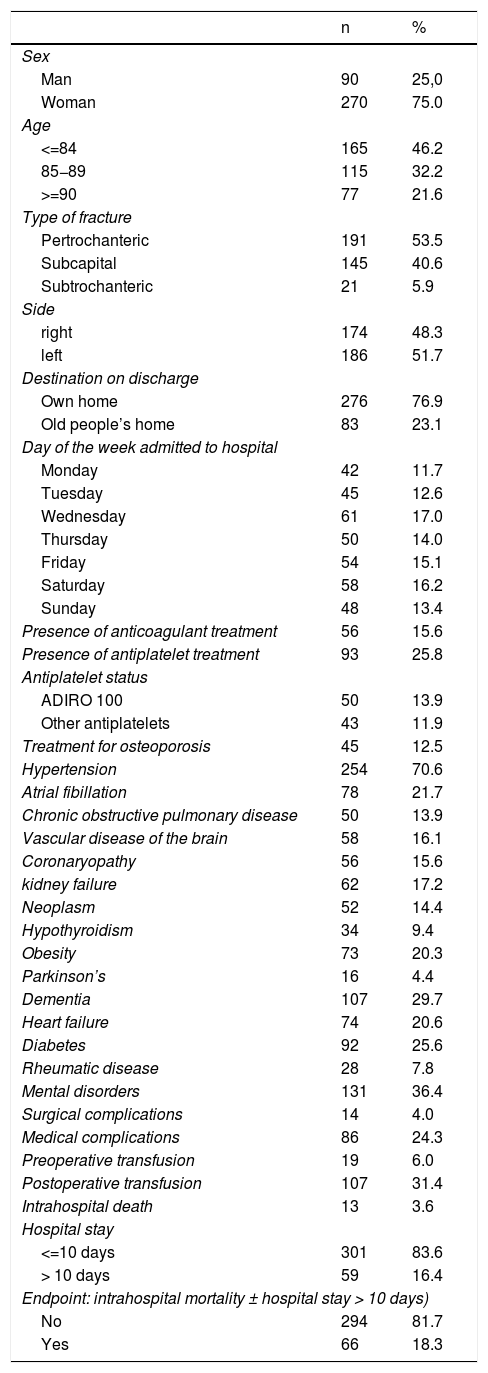
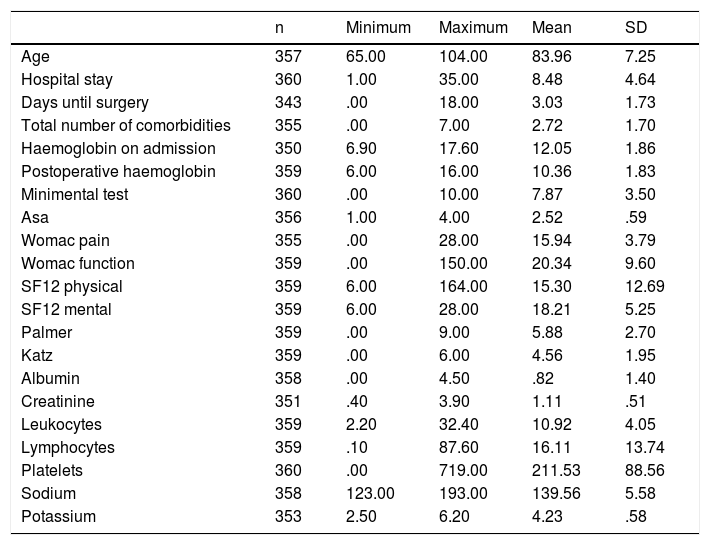
ResultsDuring the study period, 360 patients were included as they met with the inclusion criteria. Most of the patients were women (75%) and suffered from a pertrochanteric fracture (53%). Mean age was 84 years (65–104). The most common comorbidities were hypertension (70.6%), dementia (29.7%) and diabetes (25.6%). The patients had a mean of 2.7 (0–7) concomitant diseases when suffering from the hip fracture (Tables 1 and 2).
Sample characteristics – qualitative Variables.
| n | % | |
|---|---|---|
| Sex | ||
| Man | 90 | 25,0 |
| Woman | 270 | 75.0 |
| Age | ||
| <=84 | 165 | 46.2 |
| 85−89 | 115 | 32.2 |
| >=90 | 77 | 21.6 |
| Type of fracture | ||
| Pertrochanteric | 191 | 53.5 |
| Subcapital | 145 | 40.6 |
| Subtrochanteric | 21 | 5.9 |
| Side | ||
| right | 174 | 48.3 |
| left | 186 | 51.7 |
| Destination on discharge | ||
| Own home | 276 | 76.9 |
| Old people’s home | 83 | 23.1 |
| Day of the week admitted to hospital | ||
| Monday | 42 | 11.7 |
| Tuesday | 45 | 12.6 |
| Wednesday | 61 | 17.0 |
| Thursday | 50 | 14.0 |
| Friday | 54 | 15.1 |
| Saturday | 58 | 16.2 |
| Sunday | 48 | 13.4 |
| Presence of anticoagulant treatment | 56 | 15.6 |
| Presence of antiplatelet treatment | 93 | 25.8 |
| Antiplatelet status | ||
| ADIRO 100 | 50 | 13.9 |
| Other antiplatelets | 43 | 11.9 |
| Treatment for osteoporosis | 45 | 12.5 |
| Hypertension | 254 | 70.6 |
| Atrial fibillation | 78 | 21.7 |
| Chronic obstructive pulmonary disease | 50 | 13.9 |
| Vascular disease of the brain | 58 | 16.1 |
| Coronaryopathy | 56 | 15.6 |
| kidney failure | 62 | 17.2 |
| Neoplasm | 52 | 14.4 |
| Hypothyroidism | 34 | 9.4 |
| Obesity | 73 | 20.3 |
| Parkinson’s | 16 | 4.4 |
| Dementia | 107 | 29.7 |
| Heart failure | 74 | 20.6 |
| Diabetes | 92 | 25.6 |
| Rheumatic disease | 28 | 7.8 |
| Mental disorders | 131 | 36.4 |
| Surgical complications | 14 | 4.0 |
| Medical complications | 86 | 24.3 |
| Preoperative transfusion | 19 | 6.0 |
| Postoperative transfusion | 107 | 31.4 |
| Intrahospital death | 13 | 3.6 |
| Hospital stay | ||
| <=10 days | 301 | 83.6 |
| > 10 days | 59 | 16.4 |
| Endpoint: intrahospital mortality ± hospital stay > 10 days) | ||
| No | 294 | 81.7 |
| Yes | 66 | 18.3 |
General simple characteristics – continuous quantitative variables.
| n | Minimum | Maximum | Mean | SD | |
|---|---|---|---|---|---|
| Age | 357 | 65.00 | 104.00 | 83.96 | 7.25 |
| Hospital stay | 360 | 1.00 | 35.00 | 8.48 | 4.64 |
| Days until surgery | 343 | .00 | 18.00 | 3.03 | 1.73 |
| Total number of comorbidities | 355 | .00 | 7.00 | 2.72 | 1.70 |
| Haemoglobin on admission | 350 | 6.90 | 17.60 | 12.05 | 1.86 |
| Postoperative haemoglobin | 359 | 6.00 | 16.00 | 10.36 | 1.83 |
| Minimental test | 360 | .00 | 10.00 | 7.87 | 3.50 |
| Asa | 356 | 1.00 | 4.00 | 2.52 | .59 |
| Womac pain | 355 | .00 | 28.00 | 15.94 | 3.79 |
| Womac function | 359 | .00 | 150.00 | 20.34 | 9.60 |
| SF12 physical | 359 | 6.00 | 164.00 | 15.30 | 12.69 |
| SF12 mental | 359 | 6.00 | 28.00 | 18.21 | 5.25 |
| Palmer | 359 | .00 | 9.00 | 5.88 | 2.70 |
| Katz | 359 | .00 | 6.00 | 4.56 | 1.95 |
| Albumin | 358 | .00 | 4.50 | .82 | 1.40 |
| Creatinine | 351 | .40 | 3.90 | 1.11 | .51 |
| Leukocytes | 359 | 2.20 | 32.40 | 10.92 | 4.05 |
| Lymphocytes | 359 | .10 | 87.60 | 16.11 | 13.74 |
| Platelets | 360 | .00 | 719.00 | 211.53 | 88.56 |
| Sodium | 358 | 123.00 | 193.00 | 139.56 | 5.58 |
| Potassium | 353 | 2.50 | 6.20 | 4.23 | .58 |
Thirteen patients died in the hospital. The intrahospital mortality rate in the patients studied was 3.6%.
The mean hospital stay in the series was 8.4 days (1–35) with 16.4%of the patients having a longer than 10-day hospital stay.
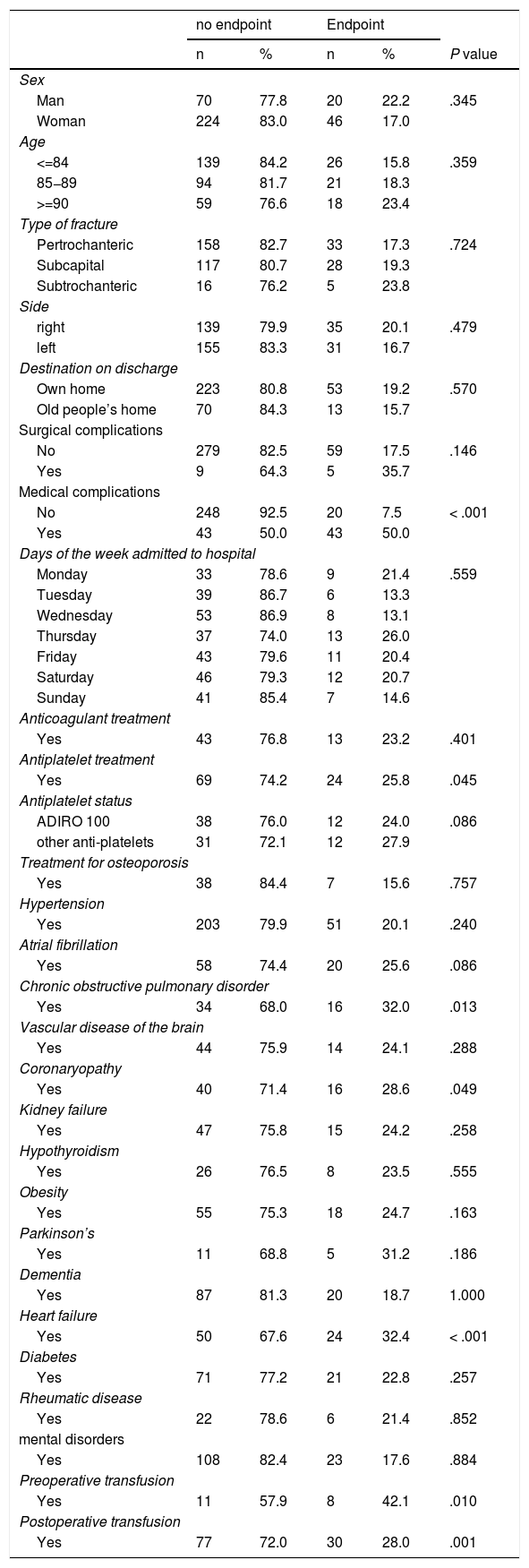
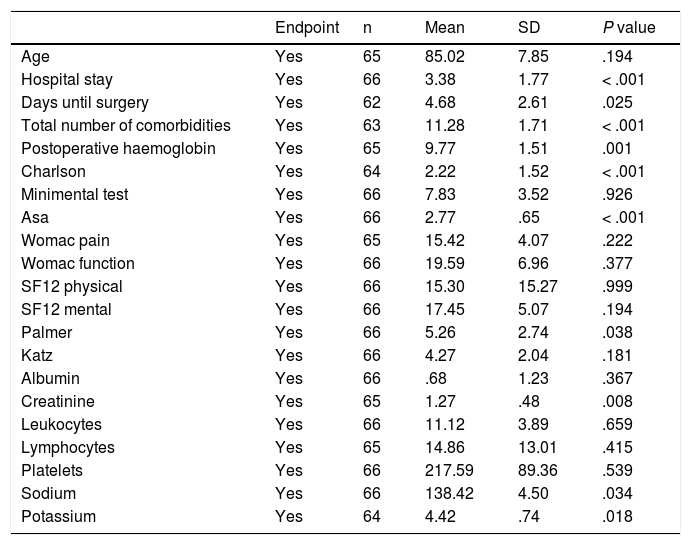
Tables 3 and 4 show the associations of the composite endpoint variable with the qualitative and quantitative variables respectively. The endpoint of the two variables studied was significantly associated with: presence of medical complications (P < .001), presence of antiplatelet process (P = .045), coronaryopathy (P = .049), COPD (P = .13), heart failure (P < .001), higher delay to surgery (P = .025), lower levels of haemoglobin on admission (P < .001) and postoperative period (P = .001), preoperative blood transfusion (P = .01), and postoperative blood transfusion (P = .001), higher number of comorbidities (P = .001), reduced sodium levels (P = .034) and creatinine (P = .008) and high levels of potassium on admission (P = .018), increased Charlson’s index (P < .001), higher ASA classification ASA (P < .001) and lower Palmer index value (P = .038).
Relationship with endpoint comprising intrahospital mortality and/or hospital stay prolonged >10 days. Qualitative variables.
| no endpoint | Endpoint | ||||
|---|---|---|---|---|---|
| n | % | n | % | P value | |
| Sex | |||||
| Man | 70 | 77.8 | 20 | 22.2 | .345 |
| Woman | 224 | 83.0 | 46 | 17.0 | |
| Age | |||||
| <=84 | 139 | 84.2 | 26 | 15.8 | .359 |
| 85−89 | 94 | 81.7 | 21 | 18.3 | |
| >=90 | 59 | 76.6 | 18 | 23.4 | |
| Type of fracture | |||||
| Pertrochanteric | 158 | 82.7 | 33 | 17.3 | .724 |
| Subcapital | 117 | 80.7 | 28 | 19.3 | |
| Subtrochanteric | 16 | 76.2 | 5 | 23.8 | |
| Side | |||||
| right | 139 | 79.9 | 35 | 20.1 | .479 |
| left | 155 | 83.3 | 31 | 16.7 | |
| Destination on discharge | |||||
| Own home | 223 | 80.8 | 53 | 19.2 | .570 |
| Old people’s home | 70 | 84.3 | 13 | 15.7 | |
| Surgical complications | |||||
| No | 279 | 82.5 | 59 | 17.5 | .146 |
| Yes | 9 | 64.3 | 5 | 35.7 | |
| Medical complications | |||||
| No | 248 | 92.5 | 20 | 7.5 | < .001 |
| Yes | 43 | 50.0 | 43 | 50.0 | |
| Days of the week admitted to hospital | |||||
| Monday | 33 | 78.6 | 9 | 21.4 | .559 |
| Tuesday | 39 | 86.7 | 6 | 13.3 | |
| Wednesday | 53 | 86.9 | 8 | 13.1 | |
| Thursday | 37 | 74.0 | 13 | 26.0 | |
| Friday | 43 | 79.6 | 11 | 20.4 | |
| Saturday | 46 | 79.3 | 12 | 20.7 | |
| Sunday | 41 | 85.4 | 7 | 14.6 | |
| Anticoagulant treatment | |||||
| Yes | 43 | 76.8 | 13 | 23.2 | .401 |
| Antiplatelet treatment | |||||
| Yes | 69 | 74.2 | 24 | 25.8 | .045 |
| Antiplatelet status | |||||
| ADIRO 100 | 38 | 76.0 | 12 | 24.0 | .086 |
| other anti-platelets | 31 | 72.1 | 12 | 27.9 | |
| Treatment for osteoporosis | |||||
| Yes | 38 | 84.4 | 7 | 15.6 | .757 |
| Hypertension | |||||
| Yes | 203 | 79.9 | 51 | 20.1 | .240 |
| Atrial fibrillation | |||||
| Yes | 58 | 74.4 | 20 | 25.6 | .086 |
| Chronic obstructive pulmonary disorder | |||||
| Yes | 34 | 68.0 | 16 | 32.0 | .013 |
| Vascular disease of the brain | |||||
| Yes | 44 | 75.9 | 14 | 24.1 | .288 |
| Coronaryopathy | |||||
| Yes | 40 | 71.4 | 16 | 28.6 | .049 |
| Kidney failure | |||||
| Yes | 47 | 75.8 | 15 | 24.2 | .258 |
| Hypothyroidism | |||||
| Yes | 26 | 76.5 | 8 | 23.5 | .555 |
| Obesity | |||||
| Yes | 55 | 75.3 | 18 | 24.7 | .163 |
| Parkinson’s | |||||
| Yes | 11 | 68.8 | 5 | 31.2 | .186 |
| Dementia | |||||
| Yes | 87 | 81.3 | 20 | 18.7 | 1.000 |
| Heart failure | |||||
| Yes | 50 | 67.6 | 24 | 32.4 | < .001 |
| Diabetes | |||||
| Yes | 71 | 77.2 | 21 | 22.8 | .257 |
| Rheumatic disease | |||||
| Yes | 22 | 78.6 | 6 | 21.4 | .852 |
| mental disorders | |||||
| Yes | 108 | 82.4 | 23 | 17.6 | .884 |
| Preoperative transfusion | |||||
| Yes | 11 | 57.9 | 8 | 42.1 | .010 |
| Postoperative transfusion | |||||
| Yes | 77 | 72.0 | 30 | 28.0 | .001 |
Relationship with endpoint comprising intrahospital mortality and/or hospital stay prolonged >10 days. Quantitative variables.
| Endpoint | n | Mean | SD | P value | |
|---|---|---|---|---|---|
| Age | Yes | 65 | 85.02 | 7.85 | .194 |
| Hospital stay | Yes | 66 | 3.38 | 1.77 | < .001 |
| Days until surgery | Yes | 62 | 4.68 | 2.61 | .025 |
| Total number of comorbidities | Yes | 63 | 11.28 | 1.71 | < .001 |
| Postoperative haemoglobin | Yes | 65 | 9.77 | 1.51 | .001 |
| Charlson | Yes | 64 | 2.22 | 1.52 | < .001 |
| Minimental test | Yes | 66 | 7.83 | 3.52 | .926 |
| Asa | Yes | 66 | 2.77 | .65 | < .001 |
| Womac pain | Yes | 65 | 15.42 | 4.07 | .222 |
| Womac function | Yes | 66 | 19.59 | 6.96 | .377 |
| SF12 physical | Yes | 66 | 15.30 | 15.27 | .999 |
| SF12 mental | Yes | 66 | 17.45 | 5.07 | .194 |
| Palmer | Yes | 66 | 5.26 | 2.74 | .038 |
| Katz | Yes | 66 | 4.27 | 2.04 | .181 |
| Albumin | Yes | 66 | .68 | 1.23 | .367 |
| Creatinine | Yes | 65 | 1.27 | .48 | .008 |
| Leukocytes | Yes | 66 | 11.12 | 3.89 | .659 |
| Lymphocytes | Yes | 65 | 14.86 | 13.01 | .415 |
| Platelets | Yes | 66 | 217.59 | 89.36 | .539 |
| Sodium | Yes | 66 | 138.42 | 4.50 | .034 |
| Potassium | Yes | 64 | 4.42 | .74 | .018 |
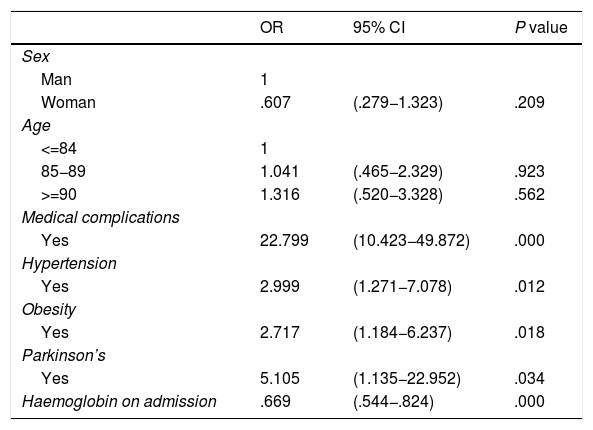
Multivariate analysis showed that the appearance of medical complications (P < .001), haemoglobin levels on admission (P < .001), high blood pressure (P = .012), obesity (P = .018) and Parkinson’s (P = .034) were related to the appearance of the composite endpoint by intrahospital mortality and prolonged hospital stay >10 days variables. Sex, age and haemoglobin levels on admission act as variables of confusion adjustment (Tables 5 and 6).
Logistic regression multivariate model.
| OR | 95% CI | P value | |
|---|---|---|---|
| Sex | |||
| Man | 1 | ||
| Woman | .607 | (.279−1.323) | .209 |
| Age | |||
| <=84 | 1 | ||
| 85−89 | 1.041 | (.465−2.329) | .923 |
| >=90 | 1.316 | (.520−3.328) | .562 |
| Medical complications | |||
| Yes | 22.799 | (10.423−49.872) | .000 |
| Hypertension | |||
| Yes | 2.999 | (1.271−7.078) | .012 |
| Obesity | |||
| Yes | 2.717 | (1.184−6.237) | .018 |
| Parkinson’s | |||
| Yes | 5.105 | (1.135−22.952) | .034 |
| Haemoglobin on admission | .669 | (.544−.824) | .000 |
Nikkel et al.5 related the increase in hospital stay with mortality in the first month after discharge, observing an increase in risk of 32% in patients whose stay was longer than 10 days compared with the group whose stay was from one to five days. The risk increased by 103% when it was over 14 days stay, which proved there were two related adverse effects and determined their combined study.
In our study it was shown that the medical complications during hospital admission, the haemoglobin levels on admission, high blood pressure, obesity and Parkinson’s are factors which increase the risk of intrahospital mortality and/or hospital stay above 10 days in patients over 65 years of age who have been operated on for a hip fracture. The other variables analysed did not show any significant relationship in the multivariate analysis.
In our study, intrahospital mortality was 3.6% and mean stay was 8.4 days, which did not differ from the published series,22 although it is true that this latter factor would vary according to the geographical regions studied, with European countries existing where the mean hospital stay would vary between five and 15 days.23–24 Similarly, in Spain the mean stay varied between autonomous communities from 7.2 to 18.6 days.3
Given the variety of risk factors relating to the adverse effects studied, clinical, surgical, analytical, demographic, functional and psychosocial factors were analysed for a total of 54 variables. The ASA classification, female sex, delay to surgery and day of admission have demonstrated a relationship with prolonged stay.8–11 In our study none of them was related to the endpoint of the variables studied. Just like in the Lott et al. Study, age as an isolated factor was not related in our study with an increase in days of stay or intrahospital mortality.2 On analysing the haemoglobin variable we found that its level on admission was related to a prolonged hospital stay and/or intrahospital mortality. However, we found no statistically significant relationship in the multivariate model in its postoperative values. Thus our results differed from the study by Willems et al.6 in that we found there was a relationship between prolonged hospital stay and postoperative haemoglobin levels, being more similar than to that of Choi et al.7 where this relationship was not shown.
In our study we observed that the appearance of medical complications is closely connected to prolonged stay or intrahospital death. This may also be related to the request for diagnostic tests and gradual treatment until the patient’s status has stabilised, as reflected in several studies.10
Richards et al.11 showed that the patients with low results in mental tests and reduced mobility would suffer from an increase in prolonged stay. Novoa et al.25 also related a reduced functional capacity in the Barthel index and age above 87 years, and an altered state of coagulation with INR > 1.5 with an increased in mortality at one year. In the light of these results, we analysed factors such as cognitive status, psychiatric disorder and functional questionnaires, as well as age and the presence of anticoagulant drugs but found no statistically significant relationship with the endpoint after multivariate analysis. Only the antiplatelet status of the patient and a low functional status measured in the Palmer questionnaire were related with these adverse effects in the univariate analysis.
Furthermore, being older than 90 years of age, being male, with heart failure, neoplasm, kidney failure, lung disasters, electrolytic changes, delay to surgery, a haemoglobin level ≤ 10 g/dL, a number of comorbidities ≥ 2, a Charlson index ≥ 2 and the presence of a rheumatic disease has been related to an increase in the risk of intrahospital mortality in some studies.12–14 However, other authors did not find any relationship between greater delay to surgery than two days and an increase in mortality.26 Regarding these variables, in our study there were only lower levels of haemoglobin on admission and the appearance of medical complications was related to the appearance of the studied adverse effects. The remainder did not establish any clear relationship.
With regard to serum and laboratory levels, Lizaur-Utrilla et al.27 appreciated that changes in sodium, albumin and parathormone levels were predictors of early mortality prior to 30 days in the elderly patient with a hip fracture. In our study initially the same was appreciated as in the before-mentioned study, that changes in serum sodium, and creatinine and potassium increased the risk of intrahospital mortality and prolonged stay, but we were finally unable to find any significance in the multivariate analysis.
The factors which our study related to the endpoint clearly show the patients with a greater risk of suffering from intrahospital mortality or an increase in hospital stay. This is why it is essential to identify and act on them. Haemoglobin levels on admission is a variable which we can act on and manage through early transfusion. Medical factors are foreseeable in many patients and are therefore avoidable, especially those on which we can directly act. High blood pressure, obesity and Parkinson’s are non changeable factors on admission but like with the others, knowing the risk they provoke can also help to establish an intensive multidisciplinary follow-up in patients of these characteristics.
With regard to future prospects, the literature contains some promising results, despite the low sample size. They support actions such as shared care using multidisciplinary care protocols, which may reduce the hospital stay and mortality of this type of patients.24,28 As such, it is highly important to clarify which are the factors with the greatest impact on intrahospital mortality and prolonged stays so as to detect high risk patients during admission and prevent adverse effects with optimization of the baseline status and reduction of medical complications.
ConclusionMedical complications, haemoglobin level on admission, hypertension, obesity and Parkinson’s are variables which increase the risk of intrahospital mortality and/or a prolonged hospital stay over 10 days in patients over 65 years of age with proximal fracture of the femur.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Salvador Marín J, Ferrández Martínez FJ, Fuster Such C, Seguí Ripoll JM, Orozco Beltrán D, Carratalá Munuera MC, et al. Factores de riesgo para el ingreso prolongado y mortalidad intrahospitalaria en la fractura del fémur proximal en pacientes mayores de 65 años. Rev Esp Cir Ortop Traumatol. 2021;65:322–330.