At least 10% of ankle fractures involve the posterior malleolus of the tibia, which has been related to poorer long-term prognosis. Our aim was to analyse the clinical and functional outcomes of ankle fractures involving the posterior edge, treated surgically without direct reduction of the third malleolus.
Material and methodsWe performed a retrospective study of 45 patients aged under 60, who we classified into three groups in terms of the percentage of joint involvement of the posterior fragment (<10%, 10%–25% and >25%) assessing the functional outcomes using the visual analogue pain scale (VAS), the AOFAS scale (American Orthopedic Foot and Ankle Society) of the ankle and hindfoot and the global health questionnaire SF-36; we also analysed the degree of osteoarthritis with weight-bearing radiography, at least one year following the injury.
ResultsThe mean VAS pain score of the sample was 1.1 (0–5) at rest and 3 (0–8) on exercise; 88.4±10.1 on the AOFAS scale, and 68.5±19.3 points on the SF-36. Up to 18% of the patients developed radiographically significant osteoarthritis in the short and medium term (between 12 and 73months, with a mean of 33months). Of the patients, 55.6% had involvement of between 19% and 25% of the joint surface. We found that a larger posterior fragment size related to a greater degree of early-onset osteoarthritis (p<0.03) and poorer AOFAS scores (p<0.01).
ConclusionAnkle fractures involving the posterior malleolus seem to contribute to the development of early-onset osteoarthritis with functional limitation in young adults.
Al menos el 10% de las fracturas de tobillo presentan afectación del maléolo posterior de la tibia, lo cual se ha relacionado con peor pronóstico a largo plazo. Nuestro objetivo ha sido analizar los resultados clínico-funcionales de las fracturas de tobillo con afectación del canto posterior, tratadas de forma quirúrgica sin reducción directa del tercer maléolo.
Material y métodosRealizamos un estudio retrospectivo sobre 45 pacientes menores de 60años que hemos clasificado en tres grupos atendiendo al porcentaje de afectación articular del fragmento posterior (<10%, 10-25% y >25%), valorando los resultados funcionales mediante la escala visual analógica del dolor (EVA), la escala American Orthopaedic Foot and Ankle Society (AOFAS) de tobillo y retropié, y el cuestionario de salud global SF-36; también hemos analizado el grado de artrosis con radiografía en carga, al menos un año tras la lesión.
ResultadosLa puntuación media del dolor EVA de la muestra fue de 1,1 (0-5) en reposo y de 3 (0-8) en ejercicio; en la escala AOFAS fue de 88,4±10,1 y en la de SF-36, de 68,5±19,3 puntos. Hasta el 18% de los pacientes desarrollaron artrosis radiográficamente significativa a corto y a medio plazo (entre 12 y 73meses, con una media de 33meses). El 55,6% presentaban una afectación entre el 10 y el 25% de la superficie articular. Comprobamos que un mayor tamaño del fragmento posterior se relacionaba con mayor grado de artrosis precoz (p<0,03) y peores puntuaciones en la escala AOFAS (p<0,01).
ConclusiónLas fracturas de tobillo con afectación del maléolo posterior parecen contribuir al desarrollo de artrosis precoz con limitación funcional en adultos jóvenes.
Ankle fractures have an incidence of 187/100,000 inhabitants every year and are among the most common injuries in orthopaedic and trauma consultations. Between 7% and 44% involve the posterior or third malleolus.1 The presence of a posterior or Volkmann's fragment has been associated with poor functional outcomes and the onset of osteoarthritis in the long term2,3; size is a factor to be considered in the surgical treatment of these injuries.2–4 Based on clinical and biomechanical studies, surgical fixation of the posterior malleolus has traditionally been indicated when more than 25% of the joint surface is involved on lateral ankle X-ray, complementing synthesis of the medial and lateral malleoli2,3,5,6; traditionally osteosynthesis was performed with anterior-posterior cannulated screws, after indirect reduction.7 In recent years this approach to these injuries has changed thanks to computed tomography (CT) imaging, which enables more detailed study of the joint,8,9 since not only the size, but also joint surface reduction, the restoration of the fibular incisor and syndesmosis stability are determining factors in the outcome of these fractures.10–12 There are authors, therefore, that recommend posterior approaches for reduction and direct synthesis of Volkmann's fragment.13
The aim of this paper was to analyse clinical/functional outcomes and progression to osteoarthritis in fractures with posterior malleolus involvement treated according to conventional criteria of osteosynthesis, with indirect reduction of the posterior malleolus.
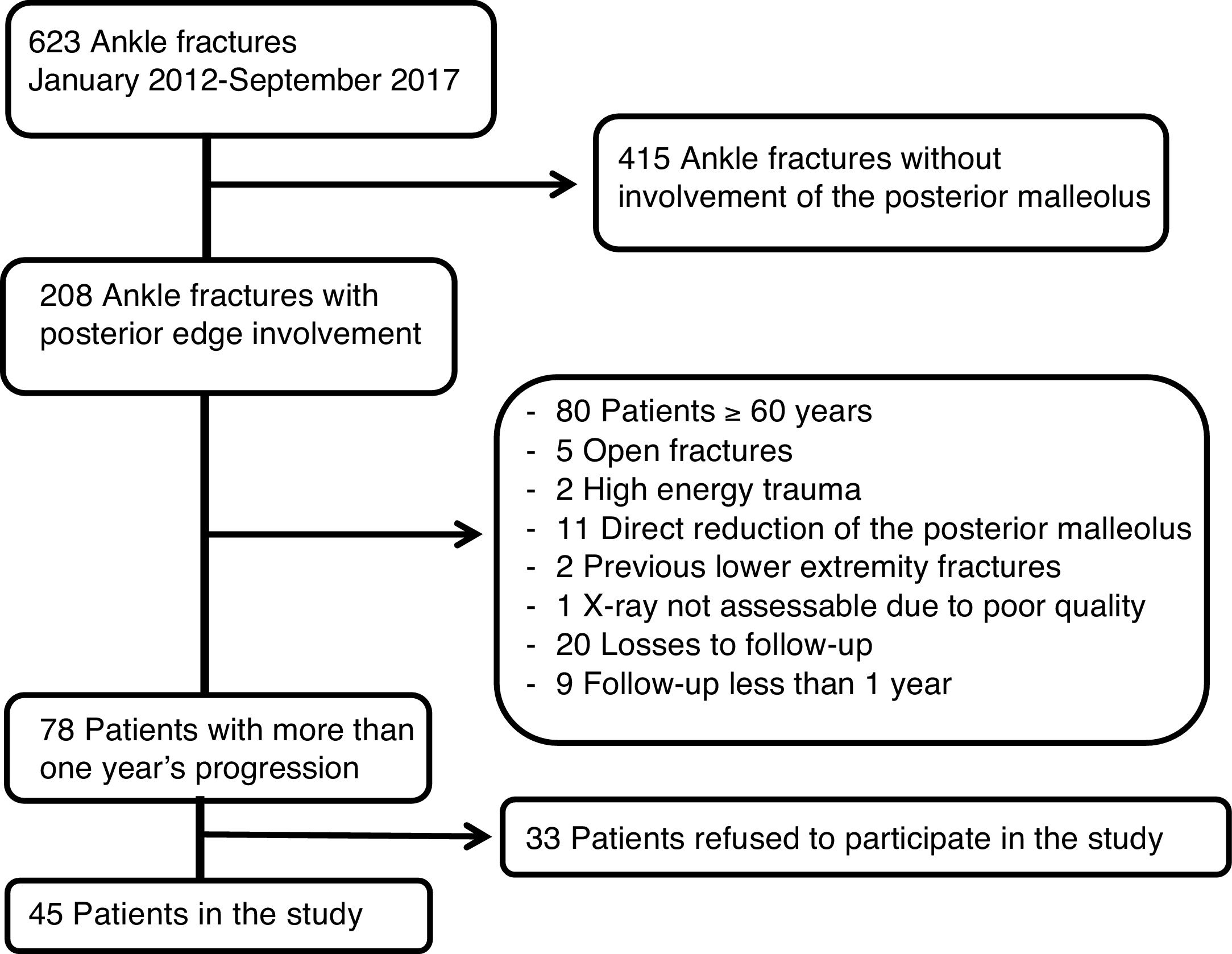
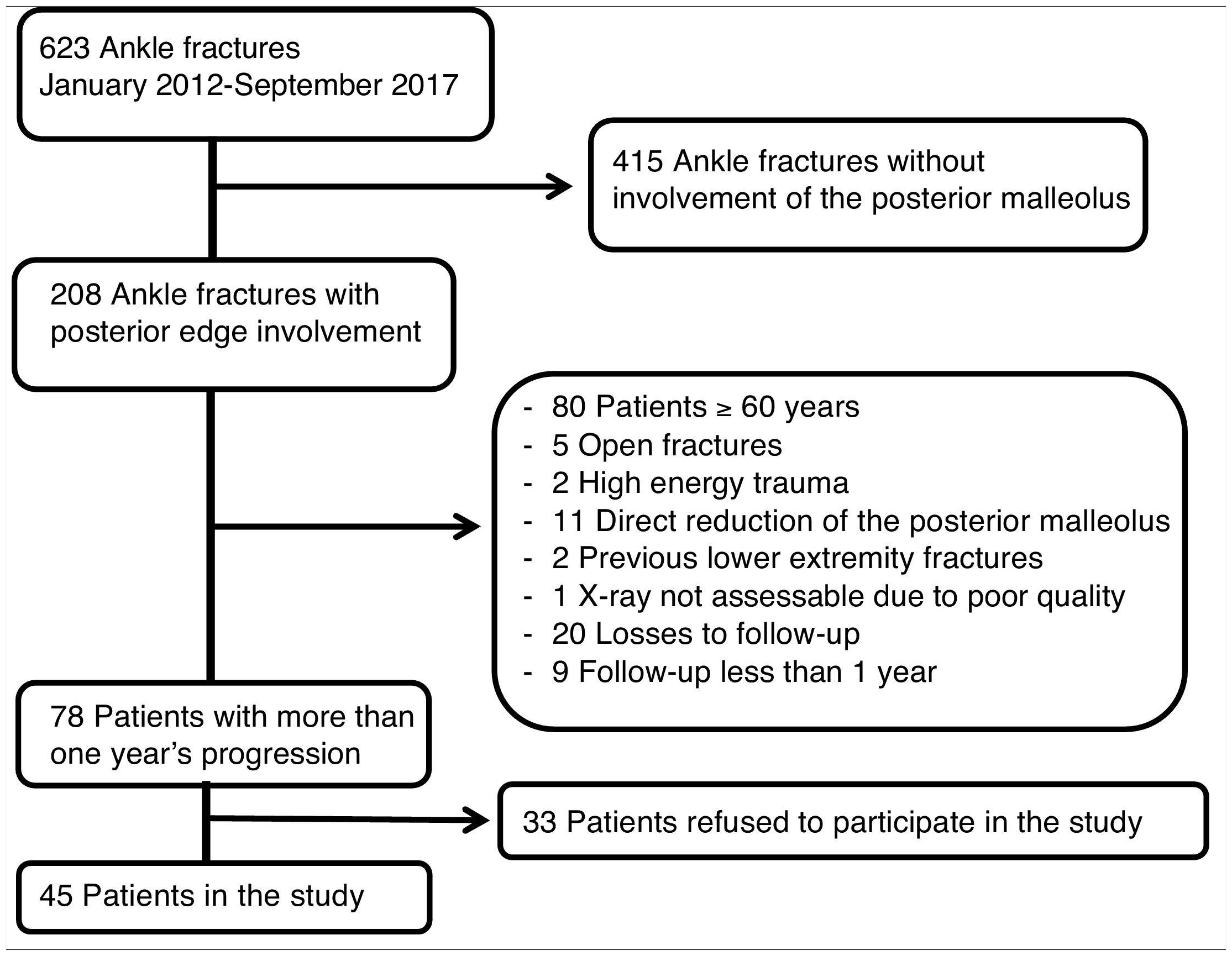
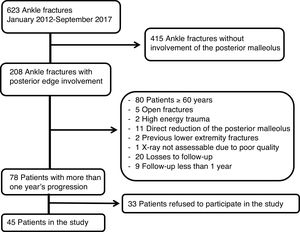
Material and methodsCollection of patientsUsing the computerised surgical registry, we collected 623 patients over the age of 18 years with ankle fractures operated in our centre from January 2012 to September 2017, and selected those with posterior malleolus involvement by reviewing radiographic images of the fracture, obtaining a total of 208 patients with ankle fractures involving the posterior edge. We excluded from this sample all patients over the age of 60 and open fractures or fractures produced by high energy mechanisms and fractures that were treated with direct reduction and osteosynthesis of the posterior malleolus by posterior approach. All patients with a follow-up period of less than one year were ruled out. A total of 78 patients met the criteria and we contacted them by telephone to include them in our study with weight-bearing X-rays and functional assessment using validated questionnaires. Eventually, 45 patients (44.6%) agreed to take part in the study, and the definitive sample comprised 22 males and 23 females, with a mean age of 41±11.2 years (Table 1).
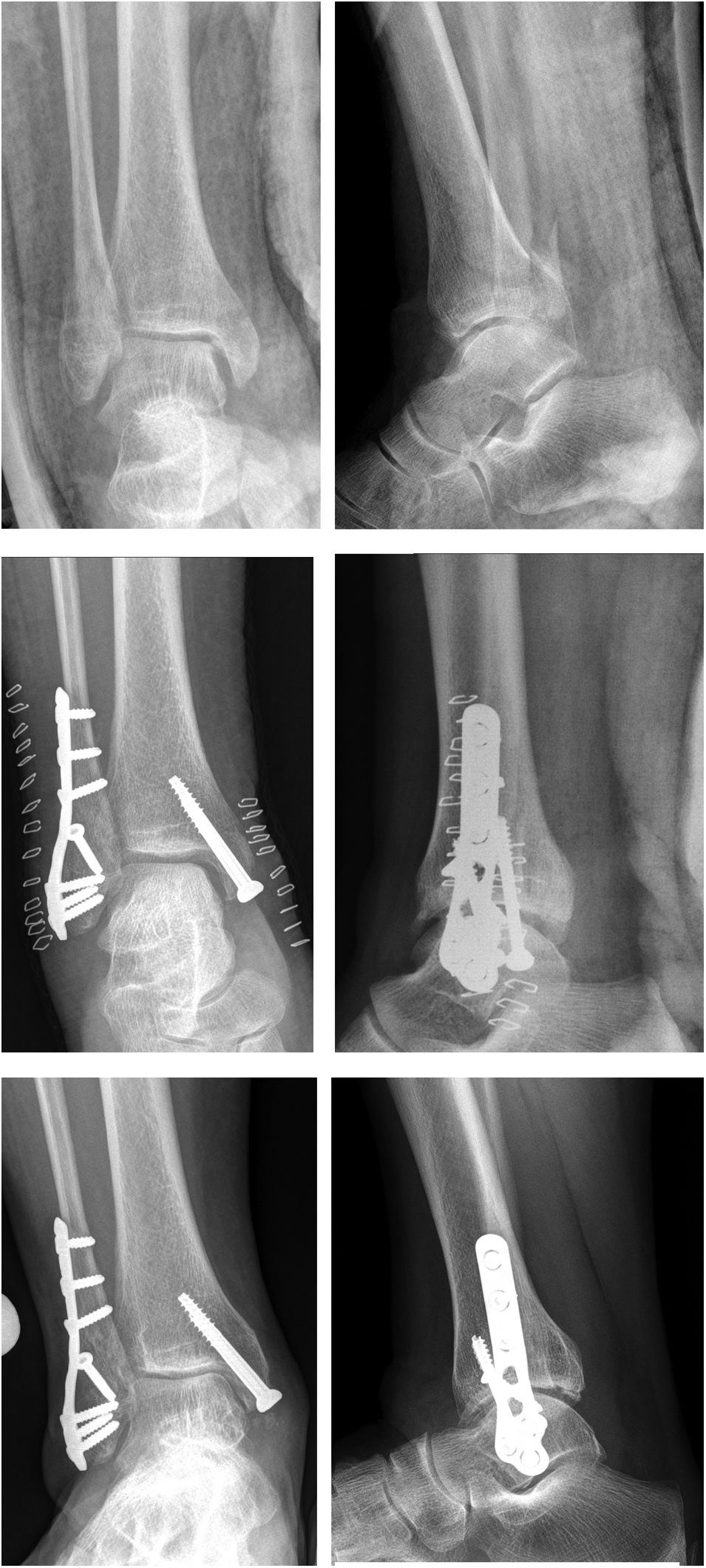
Study variablesThe initial X-rays of all the patients were reviewed, determining the type of fracture according to the Lauge-Hansen classification, and the size of the posterior malleolus was measured in millimetres. The patients were divided into three categories according to the percentage of involvement of the joint surface of the tibia: involvement <10% (group A), between 10% and 25% (group B) and >25% (group C) (Fig. 1). Joint reduction after osteosynthesis was checked in all the patients, measuring the medial clear space and the tibiofibular overlap, assuming an adequate reduction when these were less than 5mm and greater than 10mm respectively.14
After a mean follow-up period of 33 months (12–73 months) after the fracture, all the patients were reassessed in the trauma clinic, where scores of the VAS scales at rest and during exercise were taken (from 0 no pain, to 10 the worst pain imaginable) of the American Orthopaedic Foot and Ankle Society (AOFAS) for the ankle and hindfoot (0–100) and of SF-36 as a general health questionnaire. Weight-bearing X-rays were also taken (AP and lateral) to determine the degree of tibioastragaline osteoarthritis; these were all assessed by the same surgeon using the osteoarthritis classifications of Takakura15 and Van Dijk16,17 (Fig. 2).
Statistical analysisSPSS (IBM®) was used to analyse the data, studying the sample as a whole and comparing the three groups with each other according to joint involvement. We used Pearson's correlation tests for the quantitative variables, the chi-square test for qualitative variables and the ANOVA variance analysis, results with a p<0.05 were considered significant.
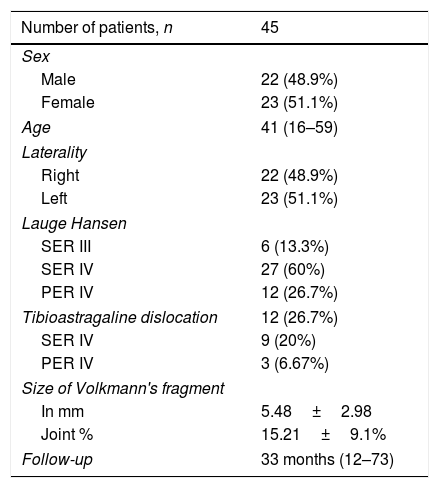
ResultsThe final sample comprised 45 patients, with a mean age of 41 years and a balanced distribution of both sex and laterality. Based on Lauge Hansen's ankle fracture classification, we observed that the majority (60% of the patients) had an SER IV type fracture; the rest were SER III and PER IV fractures; in addition, 12 of the patients (26.7%) had a tibioastragaline dislocation as well at the time of diagnosis (Fig. 3). The 45 patients in the series had adequate reduction of the ankle joint and syndesmosis after osteosynthesis. The mean size of the posterior Volkmann's fragment measured on the initial X-ray was 5.4mm, with average joint surface involvement of 15.21% without taking into account the degree of displacement of the fragments (Table 2).
Descriptive study of data.
| Number of patients, n | 45 |
|---|---|
| Sex | |
| Male | 22 (48.9%) |
| Female | 23 (51.1%) |
| Age | 41 (16–59) |
| Laterality | |
| Right | 22 (48.9%) |
| Left | 23 (51.1%) |
| Lauge Hansen | |
| SER III | 6 (13.3%) |
| SER IV | 27 (60%) |
| PER IV | 12 (26.7%) |
| Tibioastragaline dislocation | 12 (26.7%) |
| SER IV | 9 (20%) |
| PER IV | 3 (6.67%) |
| Size of Volkmann's fragment | |
| In mm | 5.48±2.98 |
| Joint % | 15.21±9.1% |
| Follow-up | 33 months (12–73) |
We classified the patients into three groups according to joint involvement, and we found that in more than half (55.56%) between 10% and 25% of the joint surface was compromised (group B); 26.67% showed less than 10% involvement (group A), and the remaining 17.78% were included within group C, with more than 25% of the joint surface compromised. Only two of our patients underwent CT scans to assess the fracture, and in both cases we found 50% underestimation of the posterior fragment. The ankle fractures of all of the patients were operated, and no case underwent direct reduction using a posterior approach to the ankle. In 4 of the 8 patients that comprised group C, osteosynthesis of the posterior malleolus was performed with a percutaneous cannulated screw in an anteroposterior direction. We checked that all the cases met the post-surgical joint reduction criteria, with a clear medial space of less than 4mm and a tibiofibular overlap of more than 5mm.14
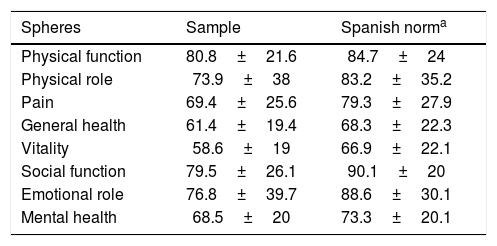
At the time of the clinical assessment, using the VAS scale (0–10) to assess pain at rest, 86.7% of the patients had mild pain (0–3), and 13.3% reported moderate pain (3–7). During exercise, up to 13.3% of the patients reported severe pain (7–10), 26.7% moderate pain and 60% mild pain. The mean AOFAS score was 88.4±10.1. We found that up to 82.22% of the patients had good or excellent outcomes (>80 points) at the time of assessment; 11.11% had fair outcomes, and only 6.67% poor outcomes (<69 points) (Fig. 3). In the assessment of the patients’ overall health status using the SF-36 questionnaire we found a mean score of 68.49±19.3, with a score in each of the spheres that was lower than expected according to the mean age of our patients18 (Table 3).
SF-36 score.
| Spheres | Sample | Spanish norma |
|---|---|---|
| Physical function | 80.8±21.6 | 84.7±24 |
| Physical role | 73.9±38 | 83.2±35.2 |
| Pain | 69.4±25.6 | 79.3±27.9 |
| General health | 61.4±19.4 | 68.3±22.3 |
| Vitality | 58.6±19 | 66.9±22.1 |
| Social function | 79.5±26.1 | 90.1±20 |
| Emotional role | 76.8±39.7 | 88.6±30.1 |
| Mental health | 68.5±20 | 73.3±20.1 |
a Note that, in our patient sample, all the scores were below the mean of the healthy Spanish population of the same age group (Vilagut et al.).18
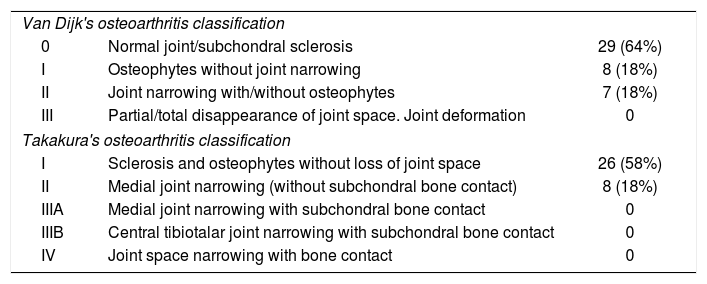
Progression to osteoarthritis was assessed using the Takakura and Van Dijk classifications, and we found that up to 18% of our patients had osteoarthritis with reduced joint space (Takakura type II). In no case did we observe a degree of osteoarthritis equal to or greater than a III in the Takakura or Van Dijk classification (Table 4).
Osteoarthritis seen at the end of follow-up.
| Van Dijk's osteoarthritis classification | ||
| 0 | Normal joint/subchondral sclerosis | 29 (64%) |
| I | Osteophytes without joint narrowing | 8 (18%) |
| II | Joint narrowing with/without osteophytes | 7 (18%) |
| III | Partial/total disappearance of joint space. Joint deformation | 0 |
| Takakura's osteoarthritis classification | ||
| I | Sclerosis and osteophytes without loss of joint space | 26 (58%) |
| II | Medial joint narrowing (without subchondral bone contact) | 8 (18%) |
| IIIA | Medial joint narrowing with subchondral bone contact | 0 |
| IIIB | Central tibiotalar joint narrowing with subchondral bone contact | 0 |
| IV | Joint space narrowing with bone contact | 0 |
Distribution of the sample according to the degree of osteoarthritis identified on the weight-bearing X-ray at the end of follow-up.
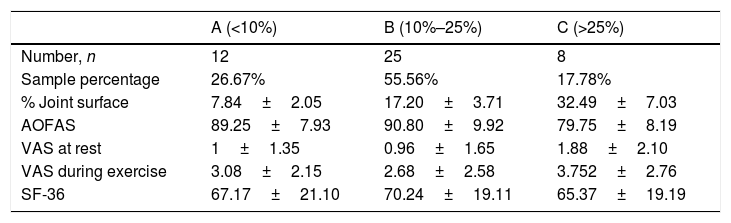
In the results of the different study groups according to the percentage of joint affected, it can be seen that the group with joint involvement of more than 25% scored 10 points less on the AOFAS functional assessment scale than the other two groups, this being the main difference we found between them (Table 5).
Distribution by group according to size.
| A (<10%) | B (10%–25%) | C (>25%) | |
|---|---|---|---|
| Number, n | 12 | 25 | 8 |
| Sample percentage | 26.67% | 55.56% | 17.78% |
| % Joint surface | 7.84±2.05 | 17.20±3.71 | 32.49±7.03 |
| AOFAS | 89.25±7.93 | 90.80±9.92 | 79.75±8.19 |
| VAS at rest | 1±1.35 | 0.96±1.65 | 1.88±2.10 |
| VAS during exercise | 3.08±2.15 | 2.68±2.58 | 3.752±2.76 |
| SF-36 | 67.17±21.10 | 70.24±19.11 | 65.37±19.19 |
Group A with joint involvement of less than 10%. Group B with joint involvement of between 10% and 25%. Group C with involvement of more than 25%.
We performed an analysis to find a relationship between the percentage of joint involvement and the functional results measured by the AOFAS. We observed that there was an inverse correlation, the functional results were poorer the larger the size of the posterior fragment (p=0.04). If we take into account the results on the AOFAS scale of each of the three groups under study and compare them with each other, we find significantly poorer AOFAS scores (p=0.01) in group C (involvement of more than 25% of joint surface (Table 5). Patients with greater joint involvement were not associated with poorer results on the SF-36 general health questionnaires. Neither did we find significant differences comparing pain on the VAS scale at rest and during exercise between the patients in the three groups (p=0.39 and p=0.57, respectively).
If we attempt to relate tibioastragaline osteoarthritis with the joint surface affected by the fracture of the posterior edge, we can see that there is a relationship between the percentage of joint involvement with the development of osteoarthritis according to Takakura's classification, the more advanced the degree of osteoarthritis the greater the joint involvement (p=0.034). However, when we compared the three groups with each other we found no statistically significant differences in the development of tibioastragaline osteoarthritis, as this occurs even in patient with less than 10% joint involvement.
On the other hand, as we would expect, the greater the degree of osteoarthritis (Takakura), the poorer the AOFAS score (ANOVA; F=3.97; p=0.027).
We found no complications after the surgical intervention or during follow-up among the patients in our series.
DiscussionA history of trauma is an important risk factor for the development of osteoarthritis, and ankle fracture is one of its main causes in young patients.19 The final painful stage can take 20 years to develop after ankle trauma.20 In our case we observed that 18% of our patients had a type II osteoarthritis according to Takakura's classification (and type II Van Dijk) short to medium term (between 12 and 73 months, with a mean of 33 months) following the trauma, which is also accompanied by poor functional results on the AOFAS assessment scale Takakura type II, the scores being significantly worse in the patients with a higher degree of osteoarthritis on X-rays. On the other hand we observed more cases of osteoarthritis the longer the follow-up time following the trauma, contrary to the data published by Drijfhout van Hooff et al.,21 who found no differences in the incidence of osteoarthritis comparing means and long follow-up periods.
With the data collected in this study, greater arthritic involvement of the tibioastragaline joint is demonstrated the larger the fractured posterior fragment, although we did not find significant differences if we compared the three groups with each other, as this occurs even in patients with joint involvement of less than 10%. This result may be due to the small sample size, especially in the patients of group C. But it also has another interpretation since, although size is a factor to be taken into account, we must give importance to all fractures with a posterior fragment, no matter how small it may appear on X-rays, because as we have been able to verify in our sample, progression towards osteoarthritis is possible with any percentage of joint involvement. In the paper published by Drijfhout van Hooff et al. a higher incidence of osteoarthritis was found with fractures of the posterior edge with involvement greater than 5% of the joint surface.21 However, for other authors there is no such relationship between the size of the posterior fragment and the development of osteoarthritis,2,6,22 with the persistence of step-off or residual joint incongruence after the treatment being greater risk factors than the specific size of the fractured fragment, although the results are not entirely conclusive.6,21,22
General health status was measured using the validated Spanish version of the SF-36, which assesses 8 spheres, both physical and mental, that evaluate an individual's state of health, and in our case the items that refer to physical activity and pain are the most relevant. Obremskey et al.23 published an improvement in all the items between 6 and 10 months following Weber B and C ankle fractures treated surgically, comparing the outcomes to those of the healthy population in a maximum of 20 months; their study, with a sample of 20 patients, did not include trimalleolar ankle fractures. In our case, with a mean follow-up of 33 months, we found an average score lower than that of the Spanish norm in all spheres, this difference being more marked in those of physical activity and pain. As with the VAS pain scale, we found no statistically significant relationship between the size of the posterior malleolus and general health status measured by the SF-36; this could be because this is a subjective scale that assesses the patient's own perception of his or her health and therefore could be influenced by many other factors that are independent of his or her ankle injury, such as their mental status or other concomitant medical conditions. For our sample of patients, we excluded the oldest (all subjects over the age of 60 were excluded) and therefore these are young adults, in whom no great comorbidities would be expected.
With a mean score on the AOFAS scale of 88.4±10.1 points, this sample is two points below the mean for patients of the same age.24 Our data show that 82.22% of the patients achieved good excellent functional outcomes regardless of the size of the fractured posterior fragment, and are similar to previous published studies with medium and long-term follow-up of trimalleaolar ankle fractures,21,25 although there are contradictory results regarding the influence of the size of the posterior edge on functional outcomes. Drijfhout van Hoof et al. found no relationship between the AOFAS score and the size of the posterior malleolus when comparing patients with more than 25% involvement versus patients with smaller fractures,21 as in the paper published by Xu et al.22 on 102 trimalleolar ankle fractures; in our case we found an inverse linear relationship between the size of the posterior fragment and the AOFAS score with significantly poorer results in group C, with involvement of more than 25% of the joint surface; results similar to those published by the Spanish team of Mingo et al.,25 who also found worse outcomes in patients with more than 25% involvement of the joint surface. Some authors have tried to relate the residual joint step-off after ankle osteosynthesis with the onset of osteoarthritis, without conclusive results, although this has been related to poorer functional outcomes measured by the AOFAS scale.21,22 In our study we did not take this variable into account due to the difficulty of obtaining reliable measurement on X-ray.
None of the studies published to date have demonstrated a relationship between the size of the posterior malleolus and the level of pain at rest and during exercise,21,22 and ours is no exception, although we observed a slight tendency to poorer VAS results at rest the greater the percentage of joint surface involved in the fracture (Pearson's correlation index=0.3; p=0.06), which is to be expected, given the higher incidence of osteoarthritis among these patients.
Biomechanical studies have emphasised the importance of osseoligamentous stability of both medial and lateral malleolus and syndesmosis, these being determining factors in the development of tibioastragaline instability after a trimalleolar ankle fracture.5,12,26 The importance of the posterior malleolus lies in its relationship with the PITFL, stabiliser of syndesmosis,11 and therefore requires an anatomical reduction and stable fixation in the treatment of these fractures.5,12,26,27 All the patients in this series showed adequate reduction of the ankle joint after osteosynthesis (medial clear space and reduced tibiofibular overlap measured on standard ankle X-rays and obeying joint reduction criteria).14 This leads us to believe that reduction of the posterior fragment may not be appropriate despite maintaining radiographic parameters within normal ranges. The indications for fixation of the posterior malleolus are not yet clear; the classical osteosynthesis criteria for all fragments greater than 25% of the joint surface have been called into question in recent years, due to the contribution, among others, of studies such as those of Bartoníček and Haraguchi.9,10 The most recent reviews conclude that, for appropriate management of these fractures, the size of the fragment obtained by X-ray measurement does not determine surgical indication.28,29 Appropriate reduction of the posterior fragment preventing residual joint step-off is important, direct reduction and internal reduction by posterior approach being superior radiologically and functionally to anteroposterior percutaneous synthesis28; it is also important to achieve stable synthesis of both the medial and lateral malleolus, as they are essential for maintaining ankle stability, which may contribute to the development of post-traumatic osteoarthritis.29
The first limitation of our study is that it is retrospective with a limited number of patients, and that not all the patients recruited agreed to participate in the study, with the biases that this implies. On the other hand, to estimate the size of the malleolus fragment, lateral X-rays of the ankle taken after the trauma were used, as in studies with similar characteristics.6,22,25 However, this system is imprecise, since the fracture line is not perpendicular to the incidence of the X-ray beam, which causes measurement errors, especially of the larger fragments.30 To prevent underestimating the size, the measurement should be made with projections in 20° ER, and in recent years the use of CT has been defended to study and classify these fractures preoperatively. CT allows measurement of the actual size and assessment of the morphology of the fragment and guides the surgical treatment of these fractures with posterior approaches for reduction and direct fixation of the posterior malleolus when necessary.8,9 In our series only two patients underwent CT image testing, and in both cases the size was clearly undersized on the X-ray, going from 4mm to 8.5mm on one, and from 10mm to 16mm in the second X-ray, which is an example of the error made in estimating the actual size of the posterior malleolus fracture through evaluating lateral X-rays. Another important limitation is the assessment of joint reduction solely considering the medial clear space and tibiofibular overlap; this method gives us an idea of the reduction and stability of the syndesmosis, but it is not sufficient to assess reduction of the posterior fragment and joint surface congruence. Standard lateral X-ray of the ankle allows an approximate assessment of posterior fragment reduction; however, we found an important limitation in this regard due to the overlap of fibular osteosynthesis material, which limited this assessment in a considerable number of patients. Postoperative CT control would enable more precise assessment of joint surface regularity, but in our study control CT was not used in any of our patients.
Despite the limitations listed, this is a homogeneous sample in terms of selection of patients and characteristics of the injury, since it targeted patients who did not require a direct approach to the posterior malleolus due to the characteristics of the injury, in the judgement of the surgeon; thus all the fractures that were most likely to progress to osteoarthritis were excluded, altering the results of the study.
With this study we found that, although we obtained acceptable reductions in terms of syndesmosis stability in all our patients, the early onset of osteoarthritis can be observed in a not inconsiderable number of them, which makes us suspect the importance of the size of the posterior malleolus fracture in the functional outcome of these patients. However, more long-term prospective studies are required for an appropriate understanding of the functional impact of posterior malleolus injuries in patients with ankle fracture. Following the latest recommendations for the treatment of posterior malleolus fractures,9,10,28 we are changing the management of these patients in our centre, expanding the preoperative study with CT imaging tests and performing direct reduction with a posterior approach to improve their functional outcomes.
ConclusionsAnkle fractures involving the posterior malleolus are the cause of early osteoarthritis, with functional limitation, despite appropriate restoration of the tibiofibular mortise following the classical criteria of syndesmosis reduction. Furthermore, a larger posterior fragment is related to a greater degree of osteoarthritis and poorer functional outcomes (p<0.05) in the short term.
Level of evidenceLevel of evidence IV: retrospective case series.
FundingThis research study received no specific grants from public sector agencies, the commercial sector or not-for-profit organisations.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Abarquero-Diezhandino A, Luengo-Alonso G, Alonso-Tejero D, Sánchez-Morata EJ, Olaya-Gonzalez C, Vilá y Rico J. Estudio de la relación de la fractura del maléolo posterior y el desarrollo de artrosis. Rev Esp Cir Ortop Traumatol. 2020;64:41–49.