To see if, in elderly patients with traumatic thoracolumbar fracture, standing X-rays with orthoses 24–48h after admission can predict vertebral collapse after consolidation.
Material and methodsProspective cohort study endorsed by the Clinical Research Ethics Committee. Inclusion criteria: age >65 years, acute thoracolumbar junction fracture due to fall, hospital admission, treatment with orthesis. Exclusion criteria: various levels, suspected malignancy, non-immediate fracture or atraumatic. Variables: Farcy index (F), regional kyphosis (C: Cobb from cranial to caudal to broken vertebra) – both measured at admission (F0 and C0), at 24–48h in standing position with orthesis (F1 and C1) and 3 months, without brace (F2 and C2), collapse (increase from F0 to F1 —F0F1— and from F1 to F2 —F1F2—; as well as from C0 to C1 —C0C1— and from C1 to C2 —C1C2—), age and gender. Statistical analysis: R package.
ResultsSeries of 40 patients, with a mean age of 75 years (66–87). Nine men and 31 women. Neither gender nor age were correlated with any variable. Six required surgery at follow-up. There were no differences in F1, C1, F0F1 or C0C1 between the six patients who required surgery and the other 34. Subsequently, data analysis was performed only for those patients who did not require surgery.
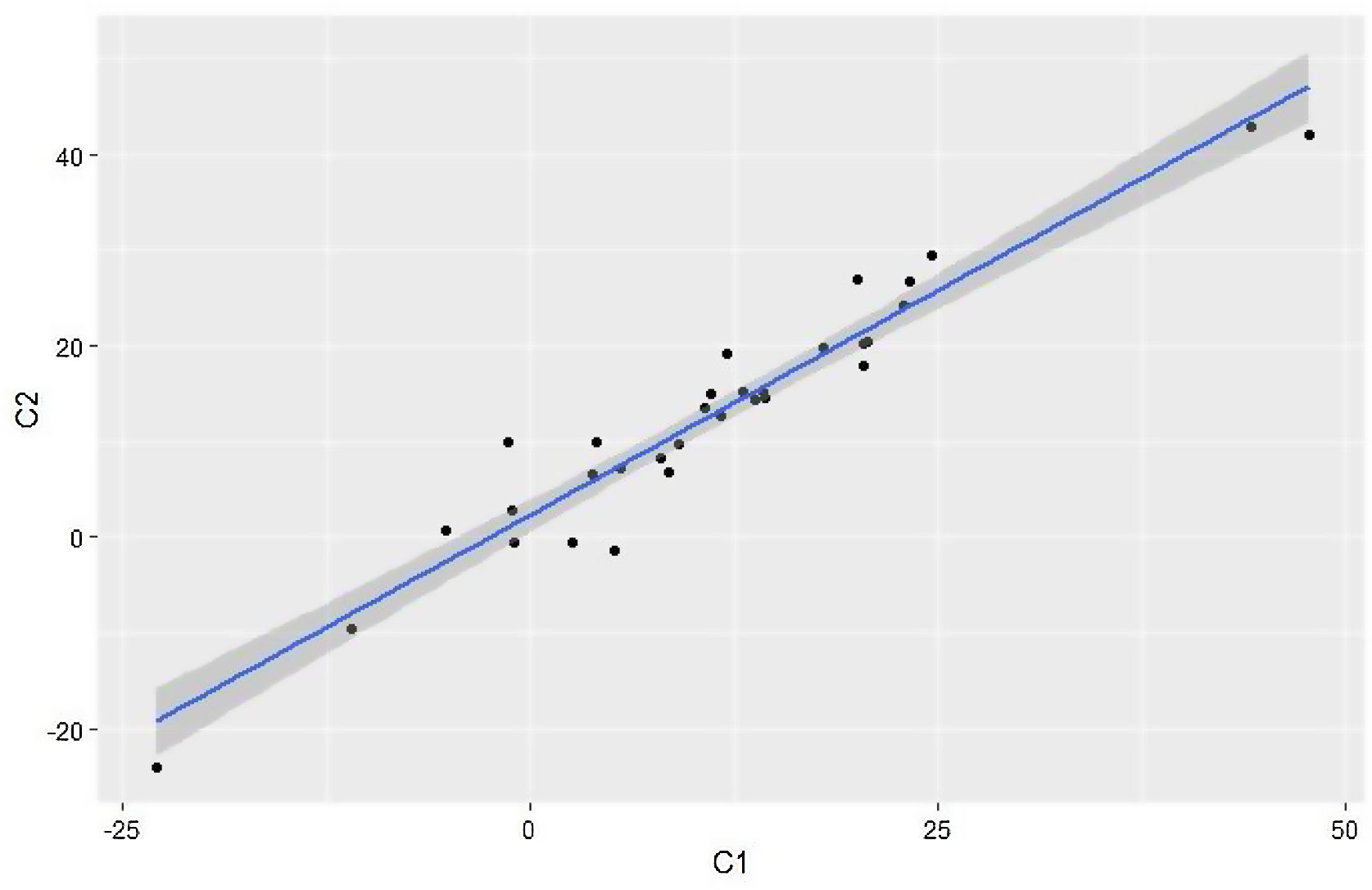
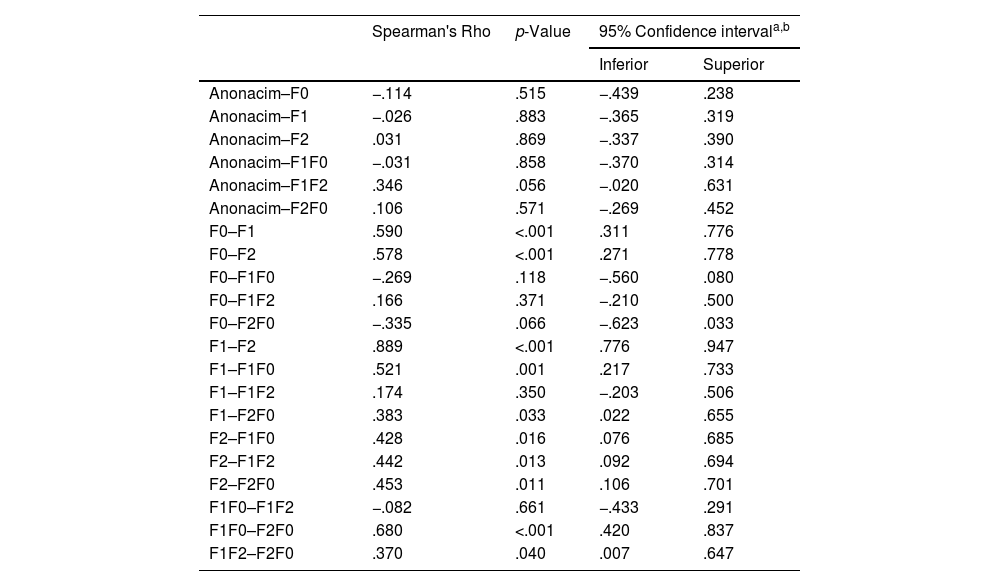
The values obtained in the Farcy index were 8°+7° (F0), 12°+7° (F1) and 15°+8° (F2) and in kyphosis (three vertebrae, Cobb) they were: C0=8°+13°; C1=11.5°+14° and C2=13°+13°. There was a correlation of F2 with F0 and F1 (p<.001), with F0F1 (p=.038) and F1F2 (p=.007). The most powerful was with F1 (Rho Spearman=.889, 95% CI=.776–.947), with a linear regression line: F2=2.61288+F1×1.01237 (R2=.79). C2 was correlated with C0 and C1 (p<.001), especially with C1 (Rho Spearman=.952, 95% CI=.899–.977). Linear regression: C2=2.23371+C1×0.93758 (R2=.927).
ConclusionsImmediate standing collapse predicts alignment at consolidation (3 months). It is therefore advisable to perform that radiography in the follow-up protocol.
Ver si, en pacientes añosos con fractura toracolumbar traumática, las radiografías en bipedestación con ortesis a las 24-48h del ingreso permiten predecir el colapso vertebral tras la consolidación.
Material y métodosEstudio prospectivo de 40 pacientes consecutivos con fractura-estallido de charnela toracolumbar (T11-L2), mayores de 65años. Avalado por el Comité de Ética de Investigación Clínica (CEIC). Criterios de inclusión: edad >65años, fractura aguda por caída, ingreso hospitalario, tratamiento con corsé. Criterios de exclusión: afectación multinivel, sospecha de malignidad, fractura subaguda o sin caída. Variables: índice de Farcy (F), cifosis regional (C: Cobb de vértebra craneal a la caudal a la rota), ambos medidos al ingreso (F0 y C0), a las 24-48h en bipedestación con corsé (F1 y C1) y a los 3meses, sin corsé (F2 y C2), colapso (incremento de F0 a F1 [F0F1] y de F1 a F2 [F1F2]; así como de C0 a C1 [C0C1] y de C1 a C2 [C1C2]), edad y género. Análisis estadístico: paquete R.
ResultadosSerie de 40 pacientes, con una edad media de 75años (66-87). Nueve varones y 31 mujeres. Ni el género ni la edad se correlacionaron con ninguna variable. Seis requirieron cirugía en el seguimiento. No hubo diferencias en F1, C1, F0F1 ni C0C1 entre los 5 pacientes que requirieron cirugía y los otros 34. Posteriormente se realizó el análisis de los datos solo de aquellos pacientes que no precisaron cirugía.
Los valores obtenidos en el índice de Farcy fueron de 8±7° (F0), de 12±7° (F1) y de 15±8° (F2) y en la cifosis (3 vértebras, Cobb) fueron: C0=8±13°; C1=11,5±14° y C2=13±13°. Hubo correlación de F2 con F0 y F1 (p<0,001), con F0F1 (p=0,038) y con F1F2 (p=0,007). La más poderosa fue con F1 (Rho Spearman: 0,889; IC95%: 0,776-0,947), con una recta de regresión lineal: F2=2,61288 +F1 ×1,01237 (R2=0,79). C2 se correlacionó con C0 y C1 (p<0,001), sobre todo con C1 (Rho de Spearman: 0,952; IC95%: 0,899-0,977). Regresión lineal: C2=2,23371 +C1 ×0,93758 (R2=0,927).
ConclusionesLa radiografía en bipedestación inmediata (F1, C1, F0F1 y C0C1) predice el colapso a la consolidación (3meses) en los pacientes de más de 65años de edad con una fractura-estallido toracolumbar por caída que se tratan conservadoramente. Se aconseja, por tanto, realizar dicha radiografía en el protocolo de seguimiento.
Thoracolumbar fractures are the most frequent fractures of the spine. The thoracolumbar hinge is the transition zone between the thoracic spine, which is rigid and in kyphosis, and the lumbar spine, which is more mobile and in lordosis, causing it to bear a significant concentration of loads. It is the region in which the greatest number of fractures occur due to biomechanical stress.1
Although there is extensive research, the management of thoracolumbar fractures remains controversial.2 Most fractures are stable and amenable to conservative treatment. Various classification systems have been published over time in an attempt to guide treatment. Holdsworth in the 1960s, taking up Nicol's 1949 concept, describes dividing the spinal column into 2 zones for the transmission of loads, an anterior column and a posterior column; a concept developed by Denis3 in 1983, introducing the concept of the medial column, giving special importance to the involvement of the medial column in order to classify a fracture as unstable. This is easily explained, since the posterior wall maintained prevents the collapse of the vertebral body and, furthermore, avoids the projection of bone material into the spinal canal. White and Panjabi4 established varying degrees of instability: mechanical, neurological and combined instability. Mechanical instability, defined as the loss of the spine's ability to bear physiological loads without pain, can result in progressive post-traumatic kyphosis, which can have serious long-term sequelae. The Magerl (AO)5 classification, introduced in 1994, is an alphanumeric system in which fractures are classified by their mechanism of production and morphological pattern. It has the ability to establish a grading of injuries that correlates with an increased risk of neurological damage or failure of conservative treatment. In 2004, Vaccaro et al.6 developed a new grading system, The Thoraco-lumbar Injury and Severity Score (TLICSS), based on fracture morphology, integrity of the posterior ligamentous complex and neurological status. It is focused on clinical practice so that once the total score has been obtained, treatment is oriented towards conservative or surgical management of the injuries.
In the absence of consensus, in 2013, the AOSpine7 classification was published by an international group of experts, with the contribution of Magerl et al. and TLICS. They consider criteria such as the morphological description of the fracture and the neurological state of the patient and, in addition, add modifying criteria specific to each patient that are relevant to the choice of surgical treatment.
When a vertebral fracture is suspected, the definitive diagnosis is mainly established with plain radiology, which allows the characteristics of the fracture to be visualised and a series of radiological stability criteria to be assessed: local kyphosis, degree of comminution of the vertebra, involvement of the posterior ligamentous complex, etc.
Although there is consensus on the definition of instability and the radiological criteria describing mechanical instability, the debate remains open regarding the indication for treatment, as there are no follow-up studies that allow us to identify prognostic factors for the evolution of a thoracolumbar burst fracture.
While there is little literature on this topic, Mehta et al.8 published a study in 2004 that aimed to compare the initial supine and subsequent seated or standing radiographs (without orthosis) in patients diagnosed with a vertebral fracture of the thoracolumbar hinge without neurological deficit to determine the increase in deformity and to see if the outcome influenced the treatment plan. The changes observed on seated/standing radiographs resulted in a change in the therapeutic orientation for 25% of the patients participating in the study, ultimately requiring surgical intervention.
In an investigation carried out by one of the co-authors of this study,9 whose main objective was to analyse the prognostic value of immediate lateral radiography performed in standing with TLSO in patients with thoracolumbar burst fracture, the percentage of patients requiring surgical intervention was 8%. With regard to the association between kyphosis and post-traumatic residual pain, several studies have been carried out in which no correlation was found between pain and radiographic deformity.10–13
In contrast, Koller et al. reported that increased kyphosis in the thoracolumbar hinge is strongly associated with a low VAS-Spine-Score.14 Koller et al. also studied the evolution of spino-pelvic parameters after vertebral fractures of the thoracolumbar hinge and concluded that patients with the ability to compensate for post-traumatic kyphosis at the expense of lumbar lordosis had better clinical outcomes. It has also been observed that as the Farcy index increased so did the likelihood of lumbosacral pain, of which a considerable percentage of patients had lumbo-sacral pain with facet characteristics at L5–S1, possibly related to mechanical overload due to immobilisation up to L5.
Based on what has been presented above, this research aims to find out whether, in patients diagnosed with thoracolumbar burst fracture, the performance of total spine X-rays, anteroposterior and lateral projections, in standing position after the placement of an orthosis in the days following the trauma, can predict the final collapse of the fracture and the sagittal profile of the patient in the long term, both clinically and radiologically, and thus provide a tool for deciding the definitive treatment of the fracture.
Material and methodsThe study carried out is a prospective study, in which patients over 65 years of age with thoracolumbar hinge burst fractures treated at the Hospital Clínico Universitario de Santiago de Compostela were included. Endorsed by the Clinical Research Ethics Committee (CEIC) of Santiago de Compostela.
Baseline patient data were collected between March 2018 and January 2021.
All patients included were diagnosed with fractures requiring non-surgical management and treated with a rigid thoracolumbosacral orthosis.
Therapeutic failure would be considered if the control X-ray performed in the standing position with the brace (at the immediate moment, during the initial admission) showed significant collapse and/or the appearance of significant local mechanical pain, thus establishing the indication for surgery.
The main hypothesis of the study is that the X-ray performed in the ED on admission and the X-ray performed while standing with the brace (at 24/48h) in this type of patient described above, allow prediction of the final situation after consolidation.
Inclusion criteria:
- -
Patients over the age of 65 years.
- -
Acute trauma thoracolumbar hinge burse fracture, subsidiary of conservative treatment according to kyphosis criteria and without neutrological symptoms.
Exclusion criteria:
- -
Pathological fractures.
- -
Fractures at various levels.
- -
Non-acute fractures.
- -
Patients who do not meet the criteria described in the previous point.
- -
Patients who do not wish to participate in the study.
Demographic data including age and gender were also collected.
The level of the fracture was taken into account and the parameters to be measured which were the main object of the study were the regional kyphosis (C) and the Farcy angle (F).
For these measurements, AP and lateral radiographs were taken at the time of initial care in the supine decubitus position, radiographs immediately after the orthosis was fitted, radiographs at 3 months (the latter two are full spine radiographs in standing position, barefoot and the first with a brace) and at one year of follow-up. The measurements were performed in the SECTRA image visualisation programme and using the programme's own measurement tools.
As the distribution was non-normal, non-parametric tests were used for statistical analysis. Correlation studies of the data (using Spearman's Rho) and linear regression were carried out using the R statistical package.
ResultsSeries of 40 consecutive patients with acute thoracolumbar hinge burst fracture (T11–L2) due to a fall, who were admitted and in whom there was an initial indication for orthopaedic management. Of these, 4 required surgery after standing X-ray (3 braces and one fusion), all of them due to pain, sometimes accompanied by collapse to kyphosis >25. The mean age of the series was 75 years (range: 66–87), all of them above the age considered to be at osteoporotic risk. Thirty-one patients were female and 9 were male. Neither gender nor age correlated with any variable.
The mean regional kyphosis at admission (C0) with supine radiography was 8°±13° and the Farcy index (F0) was 8°±7°.
At the first radiograph with standing orthosis, the regional kyphosis (C1) was 11.5°±14° and the Farcy index (F1) was 12°±7°.
At the 3-month follow-up radiograph the mean regional kyphosis (C2) and Farcy's angle (F2) were 13°±13°, and 15°±8°, respectively.
The mean regional kyphosis at admission (C0) with supine radiography was 8°±13°, and the Farcy angle (F0) was 8°±7°.
After the first radiograph with standing orthosis the mean regional kyphosis (C1) was 11.5°±14°, and the mean Farcy angle (F1) was 12°±7°.
At the 3-month follow-up radiograph the mean regional kyphosis (C2) and Farcy angle (F2) were 13°±13° and 15°±8°, respectively.
Of the 40 patients recruited, data from six were excluded from the final analysis because they had a surgical indication due to the clinical evolution of the fracture during the first 3 months. This change in therapeutic orientation accounted for 16% of the cases, the surgical indication in all of them being local mechanical pain, with no significant variations in fracture collapse. There were no significant differences in the Farcy index in immediate standing (F1) or in their immediate collapse (F0F1) between the six patients who required surgery and the other 34, nor between the local kyphosis at 3 Cobb vertebrae in immediate standing (C1) or their immediate collapse (C0C1). Subsequently, only those patients who did not require surgery were studied.
C0C1 and F0F1 are described as the increase in regional kyphosis and Farcy's index, respectively in the transition from supine to standing and C1C2 and F1F2 as the increase in collapse comparing the first standing X-ray and the one taken at 3 months for the parameters described.
Based on these assumptions, analysis using Speaman's Rho showed that there was correlation of F2 with F0 and F1 (p<.001), with F0F1 (p=.038) and F1F2 (p=.007). The most powerful association of F2 was with F1 (Rho Spearman: .889; 95% CI: .776–.947), with a linear regression line: F2=2.61288+F1×1.01237 (R2=.79). This means that the Farcy index in immediate standing (F1) explains 79% of the Farcy value at 3 months (F2).
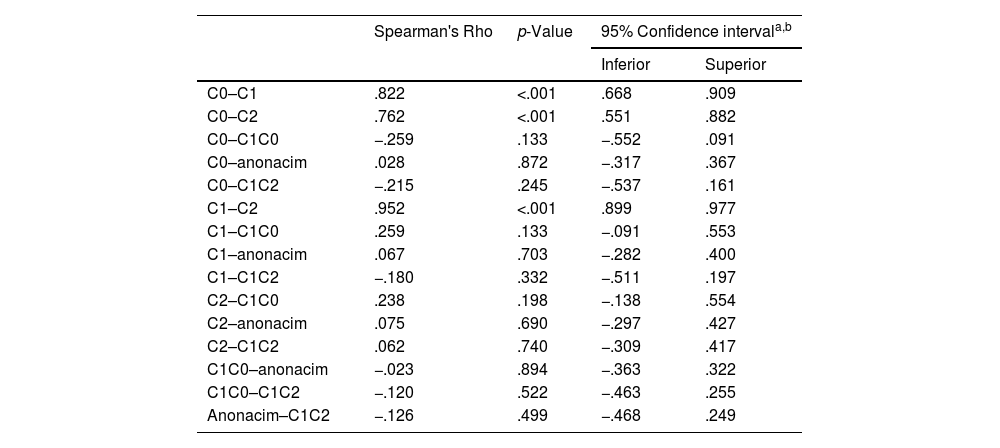
In regional kyphosis (3 vertebrae, Cobb angle), initial kyphosis (C0) correlated with immediate kyphosis on the first standing X-ray (C1) with a coefficient of .822 (95% CI .668–.909), this correlation being statistically significant (p<.001). Similarly, initial kyphosis correlated with kyphosis at 3 months (C2) with a coefficient of .762 (95% CI: .551–.882), this correlation being statistically significant (p<.001). In the study of regional kyphosis the strongest correlation was between kyphosis immediately at standing (C1) and kyphosis 3 months after injury (C2) with a coefficient of .952 (95% CI: .899–.977) with this correlation being statistically significant (p<.001); that is, C1 explains 92.7% of C2 (Table 1).
Spearman's Rho confidence intervals for regional kyphosis (C).
| Spearman's Rho | p-Value | 95% Confidence intervala,b | ||
|---|---|---|---|---|
| Inferior | Superior | |||
| C0–C1 | .822 | <.001 | .668 | .909 |
| C0–C2 | .762 | <.001 | .551 | .882 |
| C0–C1C0 | −.259 | .133 | −.552 | .091 |
| C0–anonacim | .028 | .872 | −.317 | .367 |
| C0–C1C2 | −.215 | .245 | −.537 | .161 |
| C1–C2 | .952 | <.001 | .899 | .977 |
| C1–C1C0 | .259 | .133 | −.091 | .553 |
| C1–anonacim | .067 | .703 | −.282 | .400 |
| C1–C1C2 | −.180 | .332 | −.511 | .197 |
| C2–C1C0 | .238 | .198 | −.138 | .554 |
| C2–anonacim | .075 | .690 | −.297 | .427 |
| C2–C1C2 | .062 | .740 | −.309 | .417 |
| C1C0–anonacim | −.023 | .894 | −.363 | .322 |
| C1C0–C1C2 | −.120 | .522 | −.463 | .255 |
| Anonacim–C1C2 | −.126 | .499 | −.468 | .249 |
C0: regional kyphosis measured on the initial ED X-ray; C1: regional kyphosis measured on the X-ray immediately after lifting the patient with the brace in place; C2: regional kyphosis measured on the X-ray 3 months after injury.
As for the Farcy index study, there was also a significant correlation between the difference in collapse between F1F0 (patient's transition from decubitus to standing) and collapse between baseline and 3 months (F2F0) at 68% (95% CI: .420–.837). In this analysis, we find, again, that the highest degree of correlation again appears with the measurement immediately after standing (F1) and the measurement 3 months after the injury (F2) with .889 (95% CI: .776–.947), this correlation being statistically significant (Table 2).
Confidence intervals of Spearman's Rho for Farcy angle (F).
| Spearman's Rho | p-Value | 95% Confidence intervala,b | ||
|---|---|---|---|---|
| Inferior | Superior | |||
| Anonacim–F0 | −.114 | .515 | −.439 | .238 |
| Anonacim–F1 | −.026 | .883 | −.365 | .319 |
| Anonacim–F2 | .031 | .869 | −.337 | .390 |
| Anonacim–F1F0 | −.031 | .858 | −.370 | .314 |
| Anonacim–F1F2 | .346 | .056 | −.020 | .631 |
| Anonacim–F2F0 | .106 | .571 | −.269 | .452 |
| F0–F1 | .590 | <.001 | .311 | .776 |
| F0–F2 | .578 | <.001 | .271 | .778 |
| F0–F1F0 | −.269 | .118 | −.560 | .080 |
| F0–F1F2 | .166 | .371 | −.210 | .500 |
| F0–F2F0 | −.335 | .066 | −.623 | .033 |
| F1–F2 | .889 | <.001 | .776 | .947 |
| F1–F1F0 | .521 | .001 | .217 | .733 |
| F1–F1F2 | .174 | .350 | −.203 | .506 |
| F1–F2F0 | .383 | .033 | .022 | .655 |
| F2–F1F0 | .428 | .016 | .076 | .685 |
| F2–F1F2 | .442 | .013 | .092 | .694 |
| F2–F2F0 | .453 | .011 | .106 | .701 |
| F1F0–F1F2 | −.082 | .661 | −.433 | .291 |
| F1F0–F2F0 | .680 | <.001 | .420 | .837 |
| F1F2–F2F0 | .370 | .040 | .007 | .647 |
F0: Farcy angle measured on the initial emergency department X-ray; F1: Farcy angle measured on the X-ray immediately after lifting the patient with the brace in place; F2: Farcy angle measured on the X-ray 3 months after injury.
To recapitulate, the linear regression studies allowed us to calculate the final values of C2 and F2 based on the data from the admission radiographs (F1 and C1), obtaining the following regression lines:
Regarding the Farcy index, applying the above function, we found that F1 would explain the value of F2 by 79%, and that the collapse F0F1 is also significantly related to the value of F2 (p=.037), but in this case, this collapse only explains 12% of the value of F2.
But the greatest predictive capacity was shown by the regional kyphosis variable, since knowing the initial kyphosis (C1) it is possible to predict what the final result will be on consolidation of the vertebral body (C2) with an R2=.027; that is, C1 explains 93% of C2 (Fig. 1).
Of the patients who had satisfactory immediate standing X-ray and clinical tolerance, none required surgical intervention at follow-up, with revisions at 1 and 3 months.
Regarding the data collected with respect to the one-year follow-up radiographic measurements, the one-year follow-up measurements, which will report on spinal accommodation after the fracture-stroke event, still need to be completed, but that will be contained in another paper.
DiscussionFractures of the spine are common fractures in osteoporotic patients and in those over 65 years of age.
The transitional regions or hinges of the spine are areas in which the changes of curves in the sagittal axis cause them to have special aspects.
In this study we have included patients with mechanically stable vertebral burst fractures affecting the thoracolumbar transition zone, which require conservative treatment.
Rudol and Gummerson1 (2014) spoke of the lack of consensus in both classifications and types of treatment for these fractures, and reviewed anatomical and biomechanical concepts that help the surgeon to make decisions.
It has been discussed on various occasions whether this type of fracture requires surgical treatment or whether it can be treated conservatively.
In 2004, Mehta et al.8 studied the influence of loading (by standing radiography) on the increase in fracture deformity, and concluded that there is a significant increase that may alter the treatment strategy.
In a publication by one of the co-authors of this study,9 it is observed that immediate radiography, in a standing position and with a brace, has prognostic value in terms of pain and the need for surgical intervention in patients with this type of fracture.
We consider that the most decisive moment for establishing conservative treatment as the most appropriate option in this type of fracture is when an axial load is placed on the vertebral body. This is the moment when collapse can increase significantly (as well as local mechanical pain) and, when this occurs, a surgical indication could be established.
This is one of the reasons why this study stresses the importance of the total spine X-ray in two projections in standing position, taken immediately after the patient is fitted with the rigid thoracolumbosacral orthosis.
Once this X-ray has been performed, as the results of this study show, by measuring and knowing the initial collapse of the vertebral body, we will be able to predict, by more than 93%, what the final degree of collapse of the vertebral body will be on consolidation of the fractures.
There is no established protocol in the follow-up of conservatively treated fractures in terms of which imaging tests to use and when to perform them.
The results yield data that allow immediate radiography to be related to radiography at consolidation, which may lead to a change in the follow-up protocol.
A few years ago, one of the authors presented a paper9 in which such radiological control was introduced in immediate standing, but the series covered a wide age group and not always in the range of probable osteoporosis and in a retrospective review; for this reason, a weakness of the study was its extrapolation to patients with osteoporosis. This is why the present study was designed, prospectively recruiting a cohort of patients with a structured follow-up protocol, including only thoracolumbar transverse fractures (T11 to L2) in patients with a minimum age of 65 years and with a fracture secondary to a fall, to imply a greater injurious energy and differentiate them from patients with osteoporotic vertebral wedging due to stress, which we consider to be a different nosological entity.
In our experience, the follow-up of stable fractures with conservative treatment with orthosis is usually carried out with check-ups in consultation and monthly standing X-rays during the first 3 months to ensure that there are no new collapses and to ascertain the clinical condition of the patients.
The results of this study are interesting and could change the follow-up protocol carried out. One idea to consider would be to establish a protocol that includes an X-ray immediately after standing upright, since, knowing the collapse in this X-ray, we can predict the final collapse of the fractures and thus postpone the next imaging test to 3 months.
During this study there were 6 patients who required vertebral reinforcement or fixation techniques not because of increased kyphosis or instability criteria, but because of clinical criteria marked by the pain of the patients; as this is a not insignificant percentage (15.7%) it is very important to know the clinical state of the patients during the follow-up, even if imaging tests are not carried out every month.
Bearing this in mind, this opens the door to the possibility that, during these first 3 months of follow-up, before a new X-ray is taken, patients could be followed up by telephone in order to know the clinical evolution of the patient and thus identify if there are any warning signs that require medical and/or surgical attention prior to the X-ray at 3 months.
This last aspect is interesting as it can be applied to times such as the pandemic situation we are currently experiencing and avoid some hospital visits in elderly patients who usually have certain comorbidities associated with them.
All this is possible because, by means of a mathematical procedure, we are able to predict the collapse to consolidation of the fractures based on the initial collapse of the fractures, since they are significantly related, and thus help to establish a follow-up protocol.
Of the patients who had satisfactory immediate standing X-rays and clinical tolerance, none required surgical intervention at follow-up, with revisions at 1 and 3 months. Collapse, according to the regression lines, was 3 on average beyond the immediate standing X-ray, so that exhaustive radiological follow-up does not appear to be necessary in these patients if the immediate standing X-ray is satisfactory.
Finally, it should be added that, although the results at one year cannot yet be shown because not all patients have reached the follow-up time at the present time, it seems that the results are very promising and that the collapse at one year of follow-up also correlates with that observed in the immediate standing X-ray.
Conclusions- 1.
The final collapse is conditioned between 79% (Farcy) and 93% (local kyphosis to 3 vertebrae) by the values of the immediate standing X-ray and we are able to mathematically calculate the final values according to the values at the time of admission.
- 2.
It is recommended to perform an immediate standing X-ray to be able to determine the final result of thoracolumbar hinge burst fractures under conservative treatment and to help establish a follow-up protocol.
The authors have no conflict of interests to declare.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.