Osteoporosis and fragility play a significant role in the treatment and planning of patients with deformity secondary to osteoporotic vertebral fracture (OVF). The resulting deformity can present significant challenges for its management, both from a medical and surgical perspective. The need for a specific classification for these deformities, including the potential for the development of artificial intelligence and machine learning in predictive analysis, is emerging as a key point in the coming years. Relevant aspects in preoperative optimisation and management of these patients are addressed. A classification with therapeutic guidance for the management of spinal deformity secondary to OVF is developed, emphasising the importance of personalised treatment. Flexibility and sagittal balance are considered key aspects. On the other hand, we recommend, especially with these fragile patients, management with minimally invasive techniques to promote rapid recovery and reduce the number of complications.
La osteoporosis y la fragilidad desempeñan un papel importante en el tratamiento y la planificación de los pacientes con una deformidad secundaria a la fractura vertebral osteoporótica. La deformidad resultante presenta desafíos significativos para su manejo, tanto desde el punto de vista médico como quirúrgico. La necesidad de una clasificación específica para estas deformidades, incluyendo para su desarrollo el potencial de la inteligencia artificial y el aprendizaje automático en el análisis predictivo, se perfilan como un punto clave en los próximos años. Se abordan aspectos relevantes en la optimización preoperatoria y en el manejo de estos pacientes. Se elabora una clasificación con orientación terapéutica para el manejo de la deformidad espinal secundaria a fractura vertebral osteoporótica, pero destacando la importancia del tratamiento personalizado. En ella consideramos la flexibilidad y el equilibrio sagital como aspectos clave. Por otro lado, recomendamos, en especial con estos pacientes frágiles, un manejo con técnicas mínimamente invasivas para promover una recuperación rápida y reducir el número de complicaciones.
To understand spinal deformity in the elderly patient, it is important to be aware of the underlying pathology, which is osteoporosis, and to understand the concept of frailty. Osteoporosis is a systemic and progressive metabolic bone disease characterised by a progressive decrease in bone mineral mass and an alteration of the microarchitecture of bone tissue in the form of a decrease in the number and thinning of trabeculae and loss of connectivity. It is a subclinical condition until the onset of fragility fractures, which are particularly frequent at the vertebral level.1
The concept of frailty has become popular in the geriatric population, closely related to sarcopenia and functional deterioration. Frailty is defined as a clinical state, associated with age, with a decline in physiological reserve and function in multiple organs and systems, which confers a decreased capacity to cope with chronic or acute stressors, and increased vulnerability to them.2
There is evidence that frailty predicts the onset of osteoporotic vertebral fractures in the elderly patient, irrespective of their chronological age. Both osteoporosis and frailty influence the origin of the vertebral fracture and its progression, and affect the success of treatment. It is very important to take both into account when deciding and planning treatment.
Deformity in the vertebral fragility fracture patientThe osteoporotic vertebral fracture (OVF) is the most common fragility fracture in the context of osteoporosis. For the most part they can be treated conservatively with good medium-term clinical results, and can even be subclinical or asymptomatic. However, in up to 30% of cases they significantly impact the patient's quality of life. The risk factors for the failure of conservative treatment described in the literature include location in the thoracolumbar hinge, involvement of the intermediate spine and posterior wall, and the degree of initial kyphosis.3,4 When these fractures are associated with a spinal deformity, they increase morbidity and mortality, cause chronic low back pain and have a negative impact on health-related quality of life (HRQoL).5,6
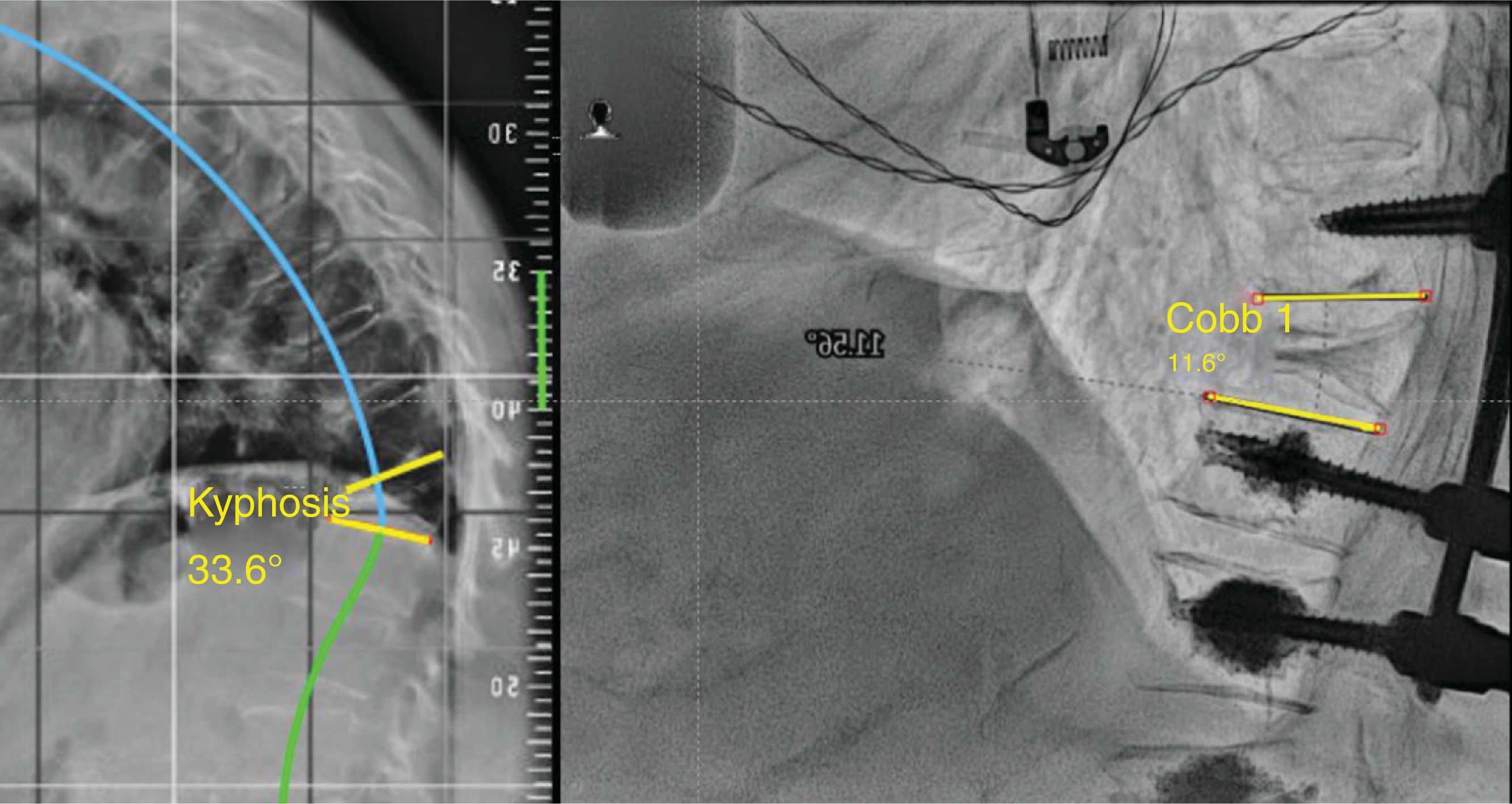
Following Schwab's Scoliosis Research Society (SRS) classification, we consider a spinal deformity to be a Cobb angle >30° in the coronal plane, kyphosis greater than 30°, or an anterior–posterior wall height ratio of less than 75%.7 Therefore, an OVF can cause deformity in the coronal plane and in the sagittal plane, which we have to consider when assessing these patients.
Global alignment is measured by a plumb line drawn from C7 on a lateral radiograph, sagittal vertical axis (SVA). A balanced sagittal balance has three characteristics: having an adequate head position to maintain horizontal gaze, the C7 plumb line falling centred over the sacrum and between the ankles with the knees extended, and all without consuming pelvic tilt reserve (pelvic tilt<20°). It has been shown that the radiological parameters defining sagittal balance (SVA, pelvic incidence [PT], sacral slope [SS], lumbar lordosis [LL]) are not static parameters, and these parameters evolve over time. A study by Lafage et al.8 on a multicentre cohort of 775 patients with adult deformity, analysed the spinopelvic parameters and correlated them with the Oswestry Disability Index (ODI) in order to establish an ideal alignment for each age. The study concluded that older patients had greater compensation, greater degenerative loss of lordosis, and were more pitched forward. The SVA for 35–45 years was 5.2 and the SVA at >75 years was 65.8mm.
In a recent study of a cohort of 249 patients with OVF (over 70 years) it was shown that 84% of patients were able to maintain SVA in normal ranges by recruiting compensatory mechanisms such as lumbar hyperlordosis, pelvic retroversion, hip extension, and knee flexion. Hence, we can state that OVF is not always the cause of sagittal imbalance. This same study concludes that there are two risk factors in patients with OVF for the onset of sagittal imbalance: thoracolumbar and lumbar location and the number of fractures at these levels have been associated with a greater impact on sagittal alignment and require closer follow-up and in some cases surgical treatment.9
Measures to reduce the onset of spinal deformities secondary to OVF: we could say that the best treatment for a patient with OVF is to prevent onset of deformity, firstly, with medical treatment for secondary prevention of new fractures.
Among other parameters described in the literature, it is worth highlighting SVA>50mm, a distance in cm from the C7 plumb line to the centre of the fractured vertebra (DSVA)>60mm, thoracolumbar location, Kümmell's disease, involvement of the anterior and posterior walls, and adjacent level fractures.10
If we identify these risk groups, we can monitor these patients more closely and offer more aggressive rheumatological management of osteoporosis and assess the option of early surgical treatment to avoid collapse of the body.
A multidisciplinary approach in these risk groups helps in the prevention of new OVFs and, consequently, a decrease in the incidence of deformity secondary to OVF. Hence, the individualised management of these patients is key.
Classification of spinal deformity associated with osteoporotic vertebral fracturesCurrently there is no classification of spinal deformities associated with OVF as an entity differentiated from adult deformity. A classification based on the aggressiveness of the surgical correction and the frailty of the patient would be fundamental. Fundamental data for decision making are those relating to the patient (comorbidities, Charlson Index, ASA), the deformity (regional kyphosis, compensatory mechanisms, rigid, or flexible deformity), and the neurological status of the patient. Obesity and sarcopenia would be other factors to be considered for classification.
To qualify this, we can distinguish patients with previous deformities (previous hyperkyphosis, scoliosis, etc.) that become decompensated and worsen due to OVF.
Deformities are usually classified as flexible or rigid depending on the reduction of kyphosis with decubitus. Osteotomies are necessary to make rigid deformities flexible for reduction. On the other hand, in flexible deformities, three-column osteotomies are not necessary, and fixations can be made in situ, even with percutaneous techniques with less surgical aggression to the patient.
Assessing the sagittal plane to check for sagittal imbalance also influences the decision on the levels to be instrumented. If there is a positive sagittal imbalance, it is usually necessary to perform long instrumentations up to the upper thoracic spine. If sagittal balance is normal, short instrumentations, i.e., one or two levels above and below the fracture may be sufficient.
There are many factors that influence the treatment decision for patients, and therefore an individualised decision with each patient is essential. Using linear regression models to detect factors that may influence the prognosis of these patients can be incomplete. In this particular aspect, the application of artificial intelligence with machine learning leads to advances in predictive analytics that can detect non-linear relationships extracted from the analysis of large amounts of data.11 This may be a line of development in the coming years to achieve a prognostic classification of deformity associated with OVF.
Treatment of spinal deformity secondary to osteoporotic vertebral fracturesOnce post-traumatic kyphotic deformity secondary to an OVF has been established, with a local deformity of >30° of kyphosis and anterior to posterior wall height ratio <75%, we are in a complex scenario, both for the patient (frail patient with associated comorbidities) and for the surgical treatment required (sometimes aggressive). Conservative treatment is indicated in those patients who are not suitable for surgery due to medical conditions and are unable to withstand surgery of these characteristics. Therefore, surgery to correct the deformity, although possible, is not always the best decision in these patients, and decisions must be made on a case-by-case basis. The indications for surgical treatment described in the literature are neurological involvement, progression of a deformity due to segmental instability with potential delayed neurological involvement, disabling pain despite third-step analgesic treatment, and severe kyphotic deformity that prevents going about a normal life.7,12–14
Several measures to consider to reduce complications in surgery in geriatric patients have been described: implementing enhanced recovery after surgery (ERAS) protocols,15 using minimally invasive techniques, implementing postoperative rehabilitation management protocols, adequate postoperative pain control, and psychological management.16 There is also talk of implementing treatment measures for osteoporosis prior to surgical treatment, but we believe that a patient with a deformity and severe pain should not wait to undergo osteoporotic treatment prior to surgery, but that surgery should be performed and the treatment undertaken by the rheumatology department in follow-up.
The characteristics of the deformity that influence the type of treatment include the location (thoracic, thoracolumbar, and lumbar hinge), the rigidity of the deformity (flexible, rigid), whether it is local/segmental or global, and whether there is neurological involvement.
Our fundamental concepts in the surgical treatment of this type of osteoporotic patient are:
- -
The use of adequate instrumentation with cemented screws to improve anchorage in the osteoporotic bone using as many anchors as necessary.17
- -
Avoid terminating instrumentation at the apex of the kyphosis.
- -
Base correction on release rather than instrumentation.
- -
Do all this with as little aggression as possible, using minimally invasive techniques.
The objectives of surgery in patients with deformity secondary to an OVF are:
- -
To stabilise the spine.
- -
To reduce kyphosis.
- -
To decompress the spinal canal when necessary.
- -
To avoid reinterventions in frail patients.
Based on the above, we recommend this guideline to assist in the decision-making process to treat this type of deformity secondary to insufficiency fractures (Fig. 1).
In the local deformity group (stage 1), this can be flexible (1A), if a reduction in angulation greater than 50% is observed in the decubitus position with respect to the X-ray (Fig. 2) in standing position, or rigid (1B), when no reduction is seen in the decubitus position (Fig. 3).13 Finally, this local deformity may be compensated (C) when the standing teleradiography shows the SVA to be within normal parameters, or non-compensated (NC), when the teleradiography shows an out-of-range SVA. It should be remembered that SVA varies with age, and we are not looking for as rigorous a correction in the elderly patient as in the young patient.8
In the global deformity group (stage 2), we observed patients whose deformity is reduced in the decubitus position (Fig. 4). This is partly due to the flexibility (2 A) of the intervertebral discs or the presence of Kummell's disease. However, we may find rigid global deformities (2 B) in patients with ankylosing spondylitis or diffuse hyperostosis. In turn, these patients may be compensated (C) or non-compensated (NC).
In the group with compensated flexible angular kyphosis (1 A C), if a stable curve is present, vertebroplasty (VP)/kyphoplasty (KP) can be performed to correct the flexible kyphosis and provide anterior stability. In the case of posterior wall involvement or pedicle fracture, resulting in instability, a short cemented instrumentation should be added to provide stability.7 If the flexible angular kyphosis is not compensated (1 A NC) and there is sagittal imbalance due to proximal thoracic hyperkyphosis, Ponte or facet flexion osteotomies may be necessary and long instrumentation up to the upper thoracic spine (T2–5) would be necessary to prevent pathology at the adjacent level (Fig. 5).
Illustration of a case with stage 1 A NC, in which, without the need to perform a three-column osteotomy, very good intraoperative reduction is observed and long percutaneous T4-L2 instrumentation and vertebroplasty of L3, L4, and L5 is performed due to fractures at that level. 1 A NC: deformity secondary to angular, flexible and non-compensated osteoporotic vertebral fracture.
In patients who present with a rigid angular kyphosis (1 B), if compensated, treatment could be conservative. This scenario is rare and usually occurs in the thoracic area.7 If it is located in the thoracolumbar hinge or at the lumbar level, surgery may be necessary (Fig. 6). Multiple surgical options have been described. There is the traditional open posterior approach with a pedicle subtraction osteotomy initially described by Heinig in 1985 with the ‘eggshell’ or decancellation technique,18 with the inherent risk of bleeding and neurological complications with the classic technique. The combined anterior and posterior approach has also been described to perform an anterior arthrodesis by corpectomy and placement of an intersomatic cage combined with a posterior approach.12 The advantages of this approach are direct decompression of the vertebral body fragments compressing the canal and solid reconstruction of the anterior spine. Good results have been published with this technique, but due to the osteoporotic nature of the fracture, and the frailty of the patient, combined approach surgery may prolong surgical time and increase the risk of bleeding and complications related to an anterior approach (lumbar, thoracolumbar, or thoracic). Implant subsidence in osteoporotic bone has also been reported. Suk et al. compared both approaches,19 and concluded that the posterior approach offers advantages over the combined approach, such as better correction of kyphosis and less surgical time and bleeding. Finally, recent studies have published promising results with a simplified decancellation osteotomy technique combined with minimally invasive instrumentation.20–22 This technique minimises bleeding and neurological complications, and improves postoperative pain control and functional recovery. In these cases where the patient is compensated, short posterior instrumentation (with two levels below the osteotomy and two to three levels above the osteotomy) can be performed with good results.
Illustration of a case with a stage 1 B C, showing that it compensates with a lumbar hyperlordosis mechanism (note a lumbar lordosis of 74° for a pelvic incidence of 54°). The patient was treated with a decancellation osteotomy and short instrumentation and normalisation of the lumbar hyperlordosis is observed on the 5-year postoperative control X-ray.
In the case of rigid angular kyphosis with thoracic hyperkyphosis and sagittal imbalance (1 B NC), the same treatment options as above can be discussed, but with the caveat that, to prevent problems at the proximal adjacent level, it is advisable to instrument up to the high thoracic level (T2–T5).
In the scenario of a global deformity (stage 2), such as a case with multiple OVFs resulting in global kyphosis, if flexible (stage 2A), conservative treatment may be reasonable. In the case of sagittal imbalance, due to failure of conservative mechanisms, it may be necessary to make a correction where, given that it is reducible, facet or Ponte osteotomies and a long arthrodesis can be performed to improve the sagittal profile and prevent pathology at the adjacent level.
Finally, in stage 2B, global deformity with non-reducible rigid kyphosis, three-column osteotomies will be necessary to correct post-traumatic kyphosis and adequately reduce the deformity to achieve a balanced spine, with fixation to the upper thoracic area and usually to the pelvis.
ComplicationsDeformity surgery secondary to OVF is not without complications. From a didactic point of view, we can classify them into four groups: general medical complications, infectious complications, early surgical complications (derived directly from the surgical act), and late surgical complications (as a consequence of poor postoperative progress). The percentage of patients with at least one complication after adult deformity surgery is 39%.23
General medical complications (13.7%): psychiatric complications (acute confusional syndrome), urinary or respiratory infection, side effects of prescribed medication or withdrawal syndrome due to discontinuation of previous regular medication, catheter infection, atelectasis, deep vein thrombosis, pulmonary thromboembolism, angina pectoris or acute myocardial infarction, digestive complications, blindness, and even death. In general, these complications are usually resolved with appropriate treatment and optimisation by the geriatrics department prior to deformity surgery. This is part of our standard practice in this type of patient.
Infectious complications (5.2%): acute post-operative infection (within the first three months post-surgery) or chronic post-operative infection (>3 months post-surgery). The severity of the complication ranges from wound staining with no general consequences to generalised sepsis requiring broad-spectrum intravenous (IV) antibiotherapy and emergency surgery.
Early surgical complications (7.5%): durotomy, early post-operative neurological deterioration due to compressive haematoma, implant malposition.
Late mechanical surgical complications (19.3%): proximal (Fig. 7) or distal adjacent level syndrome, pseudoarthrosis, instrumentation failure (pull-out) or implant breakage.
ConclusionSpinal deformity secondary to OVF is a complex pathology that can be managed surgically with good correction of the sagittal profile but is not complication-free. We recommend prior assessment by the geriatrics department to optimise the patient's general condition before surgery. We also recommend patient-tailored treatment, depending on the type of deformity (flexible/rigid), the location and the patient's sagittal balance, and minimally invasive techniques to promote rapid recovery and reduce post-operative complications.
Level of evidenceLevel of evidence iv.
FundingThe authors received no grants or external funding to support their research or prepare this manuscript. They did not receive payments or other benefits or a commitment or agreement to provide such benefits from a commercial entity. No commercial entity paid or directed, or agreed to pay or direct, any benefits to any research fund, foundation, educational institution, or other charitable or non-profit organisation with which the authors are affiliated or associated.
Conflict of interestThe authors declare that they have no conflict of interest.