Fractures of the distal third of the tibia are mostly the consequence of high-energy trauma with significant soft tissue involvement, being more frequent in men.
These types of fractures differ from the tibial pilon joint fracture in their mechanism of injury, management and prognosis.
The objective of the present study was to analyse and compare the results obtained in the treatment of fractures of the distal third of the tibia without joint extension using a locked plate and intramedullary nail.
Material and methodsWe carried out a retrospective study with patients diagnosed of “distal third tibia fracture” segment 43A according to the classification proposed by the “Trauma Orthopedic Association” who were intervened between January 2015 and May 2019 were included. We obtained 24 patients intervened with a nail intramedullary and 29 using a blocked plate.
ResultsThe study included 53 patients, 36 men and 17 women with a mean age of 51 years (range: 15–77 years). The mean follow-up time was 6 months (3–30 months). No significant differences were found in the time to fracture healing, although the beginning with load walking was earlier in the nail group.
DiscussionCurrently there is no consensus on the therapeutic management of distal tibia fractures without joint extension.
ConclusionsAfter analyzing the results, we consider that both intramedullary nail osteosynthesis and a locked plate are valid options in the treatment of fractures of the distal third of the tibia.
Las fracturas del tercio distal de tibia son, en su mayoría, consecuencia de un traumatismo de alta energía con importante afectación de partes blandas siendo mas frecuentes en varones.
Este tipo de fracturas se diferencian de la fractura articular de pilón tibial en su mecanismo de lesión, manejo y pronóstico.
El objetivo del presente estudio fue analizar y comparar los resultados obtenidos en el tratamiento de las fracturas de tercio distal de tibia sin extensión articular mediante placa bloqueada y clavo intramedular.
Material y métodosRealizamos un estudio retrospectivo en el que se incluyeron todos los pacientes con diagnostico «fractura de tercio distal de tibia» segmento 43A, según la clasificación propuesta por la Trauma Orthopedic Association, intervenidos entre enero del 2015 y mayo del 2019. Obtuvimos 24 pacientes intervenidos mediante clavo intramedular y 29 mediante placa bloqueada.
ResultadosLa muestra incluyó 53 pacientes (36 varones y 17 mujeres) con una media de edad de 51 años (rango: 15–77 años). El tiempo de seguimiento medio fue de seis meses (3–30 meses). No se hallaron diferencias significativas en el tiempo de consolidación de la fractura, aunque el inicio de la deambulación con carga fue mas temprano en el grupo clavo.
DiscusiónEn la actualidad no existe consenso acerca del manejo terapeútico de las fracturas distales de tibia sin extensión articular.
ConclusionesDados los resultados obtenidos consideramos que tanto la osteosíntesis con clavo intramedular como con placa bloqueada son opciones válidas en el tratamiento de las fracturas del tercio distal de tibia.
Fractures of the distal third of the tibia are mostly the result of high-energy trauma with significant soft tissue involvement and are more common in males in the second decade of life.1
This type of fracture differs from the articular tibial pylon fracture in its mechanism of injury, management and prognosis.2
The treatment of fractures is difficult to manage, due on the one hand to their anatomical arrangement, since the antero-medial aspect of the tibia is subcutaneous,3 devoid of protective muscle tissue, and the fracture can often perforate the skin and become an open fracture. On the other hand, the distal third of the tibia is poorly vascularised.2,4 The outer third of the cortex is supplied by the periosteum while the inner two thirds are supplied by the nutritional artery. This artery, which is dependent on the posterior tibial artery, when it enters the bone distal to the soleus muscle line, divides into three branches: two ascending and a single descending branch. Injury to this single descending branch means that the vascularisation of the distal third of the tibia will be from the periostal system, a circumstance that may hinder fracture healing.
In addition to the delicate anatomy, the complex biomechanics of the distal third of the tibia must be taken into account, conditioned by the discrepancy in diameter between the diaphyseal and metaphyseal segments, as well as the remaining size of the distal fragment.
Both factors make fracture reduction and stable fixation difficult and condition them.5
The main definitive surgical treatment options for this type of fracture are intramedullary nailing and locked plates. Each technique is associated with potential complications. In intramedullary nailing we found higher rates of malalignment,6 delayed healing7,8 and anterior knee pain.9,10
For its part, plate osteosynthesis is associated with a higher incidence of soft tissue complications, such as surgical wound infection and implant protrusion.1–15
For all of the above reasons, the management of fractures of the distal third of the tibia continues to be a controversial issue.
The aim of the present study was to analyse and compare the results obtained in the treatment of fractures of the distal third of the tibia without joint extension using a locked plate and an intramedullary nail.
Material and methodsWe conducted a retrospective study in which we included all patients with a diagnosis of “fracture of the distal third of the tibia”, according to the classification proposed by the Orthopaedic Trauma Association (OTA),2 affecting segment 43A, this being the tibial segment between 4 and 11cm from the tibio-astragal joint. Patients underwent surgery between January 2015 and May 2019.
Exclusion criteria were: tibial involvement with proximal or distal joint extension, open grade III fractures according to the Gustilo-Anderson classification,2 vascular injury compromising limb survival, pathological fractures and patients with associated severe traumatic brain injury (TBI).
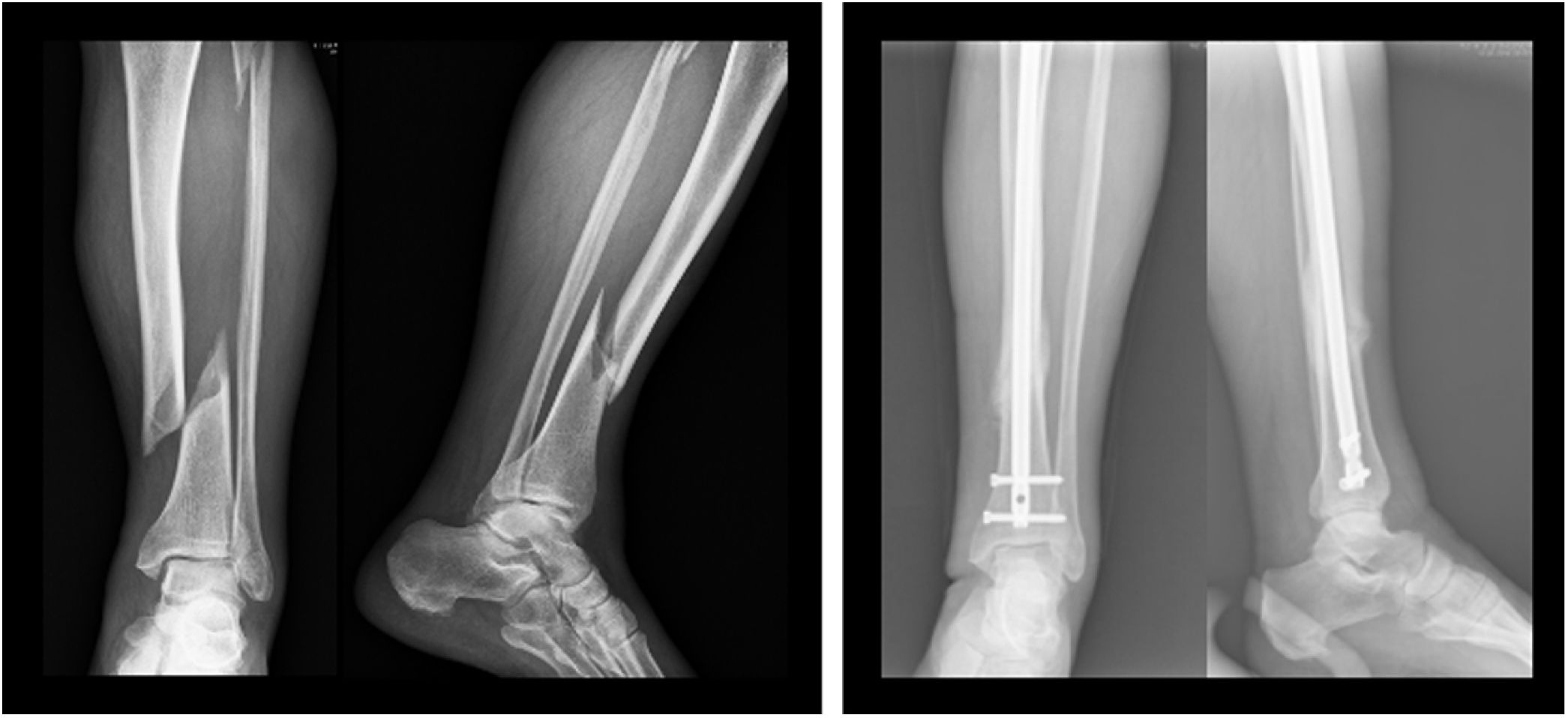
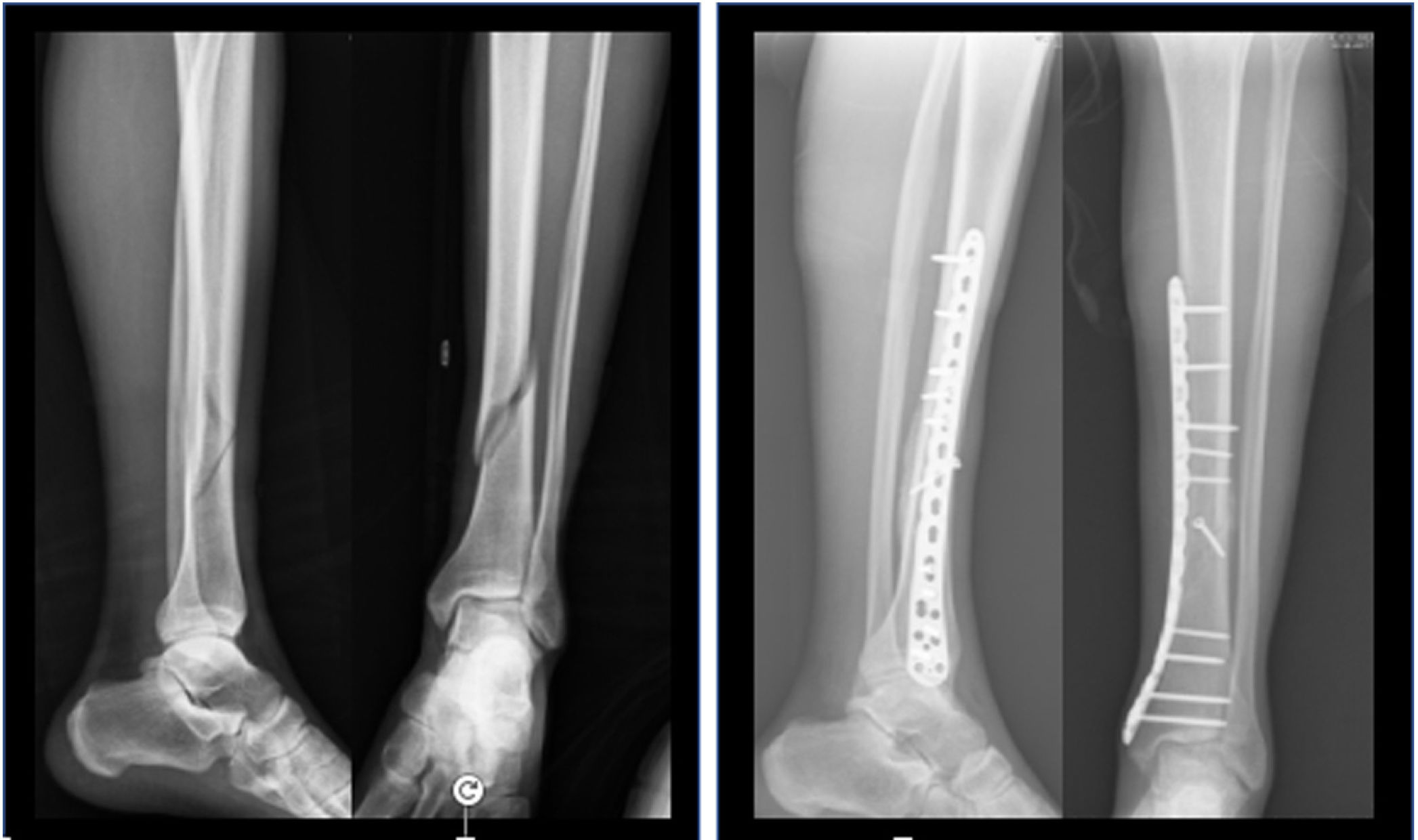
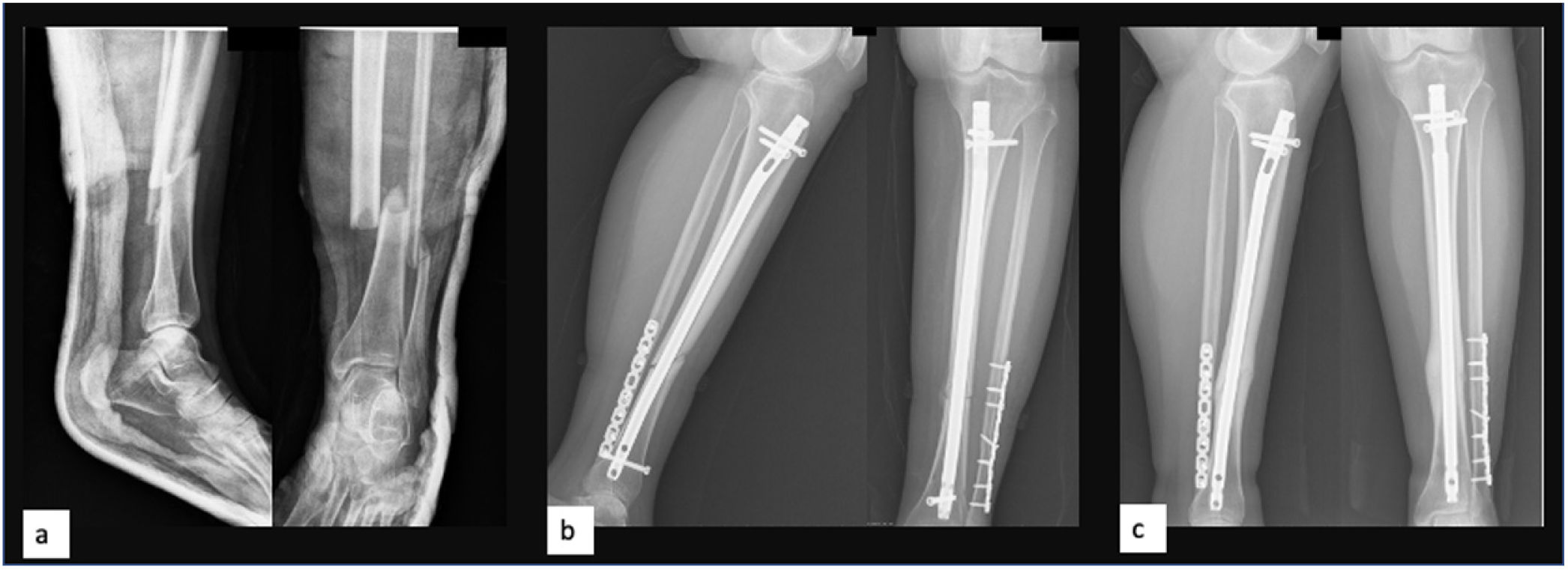
Twenty-four patients (45.3%) underwent intramedullary nailing (Fig. 1) and 29 patients (54.7%) opted for locked plate osteosynthesis (Fig. 2). The choice of osteosynthesis method was at the discretion of the surgeon responsible for the patient.
The intramedullary nail model used was the T2 (Stryker), which has the option of up to three proximal locks and three distal locks (two in the sagittal plane and one in the axial plane). In all cases, the medullary canal was reamed 1.5mm above the diameter of the definitive nail. The approaches used for implantation were, at the surgeon's choice, medial parapatellar, transpatellar and suprapatellar.
In those cases in which it was decided to synthesise the fracture by means of a plate, anatomical, low-profile titanium Low Compression Plate (LCP) with locking distal screws and fixed angle (Synthes) were used. A medial approach was used in all cases.
The associated fibula fracture was synthesised at the surgeon's discretion.
Among the epidemiological variables we collected age, sex, body mass index and consumption of toxic substances: tobacco and alcohol (more than 20cl/day). In the personal history, we checked whether the patient suffered from diabetes or had another peripheral vascular disease, as well as whether he/she was taking antiplatelet, anticoagulant or corticoid drugs.
For the determination of the anaesthetic risk we used the classification of the American Society of Anesthesiologists (ASA).
In criteria related to the fracture, we considered whether the causative trauma was high or low energy, whether the fracture was simple (43A1) or complex (43A2 and 43A3), open or closed, soft tissue involvement according to the Gustillo-Anderson classification and in the case of fibula involvement, the segment affected (proximal third, middle third or lower third).
The initial management of all patients was immobilisation by means of a posterior plaster splint, except in one case where the use of an external fixator was chosen.
In patients with grade I-II open fractures, antibiotic prophylaxis consisting of 2g of cefazolin and 240mg of gentamicin was administered on arrival at the ED, followed by debridement of the wound, abundant washing with physiological saline at low pressure and direct closure as long as there was no soft tissue tension.
After surgery, patients were followed up both clinically and radiologically at 2–3 weeks intervals until the fracture had healed.
With regard to clinical outcomes, the time to onset of weight-bearing ambulation, final active joint balance, and the presence of limping or pain were assessed using the visual analogue scale (VAS) on ambulation. The incidence of pre- and post-surgical complications was also obtained.
Radiological follow-up of the patients was carried out by means of simple radiography in two projections, anteroposterior and strict profile, considering the fracture as consolidated when the presence of a bone bridge was observed in three of the four corticals visible in both projections.
“Delayed healing” was considered as such when it exceeded 12 weeks post-surgery and “pseudo oseteoarthritis” when it exceeded 6 months.
For radiological assessment of tibial alignment, special loading radiographs were used at 12–14 weeks post-surgery, with varus/valgus deformity greater than 5° or antecurvatum/recurvatum deformity greater than 10° being determined as poor reduction.
For the description of continuous variables, measures of dispersion and centralisation were used; with respect to the distribution of categorical variables, frequency tables were used. In the case of the need to compare categorical variables, Pearson's χ2 test was used, and in the case of continuous variables, the Student's t-test was used when normality could be accepted and the Mann–Whitney U test in the opposite case. Two-tailed tests were used with a significance level of 5%. Statistical analysis was performed using R statistical software v.3.6.3.
ResultsThe sample included a total of 53 patients, 36 males and 17 females with a mean age of 51 years (range: 15–77 years). The median follow-up time was 6 months (3–30 months) and there was no loss to follow-up.
Eighty per cent of the fractures were closed (n: 46) and 54% were low energy (n: 29).
Using the OTA classification as a reference, of the 53 fractures included, 36 were classified as 43A1, i.e., they had a simple fracture trace while the remaining 17 were classified as complex, 43A2 and 43A3.
After analysing the epidemiological variables and personal medical history of both groups, it was determined that they were comparable with each other (Table 1).
Epidemiological variables and personal history according to treatment group.
| Variables | Total | Locked plate | Intramedullary nail | p value<0.05 |
|---|---|---|---|---|
| N°. | 53 | 29 (55%) | 24 (45%) | |
| Age | ||||
| Sex | 0.287 | |||
| Male | 36 (67.90%) | 22 (75.86%) | 14 (58.33%) | |
| Female | 17 (32.10%) | 7 (24.14%) | 10 (41.67%) | |
| ASA | 0.965 | |||
| I | 20 (37.70%) | 11 (37.93%) | 9 (37.50%) | |
| II | 28 (52.80%) | 15 (51.72%) | 13 (54.17%) | |
| III | 5 (9.40%) | 3 (10.34%) | 2 (8.33%) | |
| Smoker | 0.694 | |||
| Yes | 13 (24.50%) | 6 (20.69%) | 7 (29.17%) | |
| No | 40 (75.50%) | 23 (79.31%) | 17 (70.83%) | |
| Corticoids | 0.389 | |||
| Yes | 2 (3.80%) | 0 (.00%) | 2 (8.33%) | |
| No | 51 (96.20%) | 29 (100%) | 22 (91.67%) | |
| Alcohol | 1 | |||
| Yes | 26 (49.10%) | 14 (48.28%) | 12 (50.00%) | |
| No | 27 (50.90%) | 15 (51.72%) | 12 (50.00%) | |
| Diabetes | 0.533 | |||
| Yes ID | 1 (1.90%) | 0 (.00%) | 1 (4.17%) | |
| No | 50 (94.30%) | 28 (96. 55%) | 22 (91.67%) | |
| Yes NID | 2 (3.80%) | 1 (3.45%) | 1 (4.17%) | |
| Drugs | 1 | |||
| Antiaggregants | 4 (7.50%) | 2 (6.90%) | 2 (8.33%) | |
| No | 49 (92.50%) | 27 (93.10%) | 22 (91.67%) | |
| Energy | 0.838 | |||
| High | 24 (45.30%) | 14 (48.28%) | 10 (41.67%) | |
| Low | 29 (54.70%) | 15 (51.72%) | 14 (58.33%) | |
| Gustilo | 0.2 | |||
| Closed | 46 (86.80%) | 23 (79.31%) | 23 (95.83%) | |
| Open type I | 6 (11.30%) | 5 (17.24%) | 1 (4.17%) | |
| Open type II | 1 (1.90%) | 1 (3.45%) | 0 (.00%) | |
| OTA 43.A classification | 0.024 | |||
| 1 | 36 (67.90%) | 19 (65.52%) | 17 (70.83%) | |
| 2 | 4 (7.50%) | 0 (.00%) | 4 (16.67%) | |
| 3 | 13 (24.50%) | 10 (34.48%) | 3 (12.50%) | |
ASA: American Society of Anaesthesiologists; ID: insulin dependent; NID: not insulin dependent; OTA: Trauma Orthopedic Association.
The mean time to fracture healing was 10.3 weeks (range: 8–14 weeks) in the nail group and 11.4 weeks (range: 10–14 weeks) in the plate group, without finding statistically significant differences (Table 2).
This table contains the main outcomes.
| Variables | Total | Locked plate | Intramedullary nail | p value<0.05 |
|---|---|---|---|---|
| N°. | 53 | 29 | 24 | |
| Healing time (weeks) | 0.157 | |||
| Mean (SD) | 10.96 (2.59) | 11.48 (2.38) | 10.35 (2.74) | |
| Median (IQR) | 10 (9.00–14.00) | 10 (10.00–14.00) | 10 (8.00–14.00) | |
| Consolidation | 1 | |||
| No | 3 (5.70%) | 2 (6.9%) | 1 (4.17%) | |
| Yes | 50 (94.30%) | 27 (93.10%) | 23 (95.83%) | |
| Deambulation | <0.001 | |||
| 3–4 weeks | 12 (22.60%) | 0 (.00%) | 12 (50.00%) | |
| 5–6 weeks | 16 (30.20%) | 11 (37.93%) | 5 (20.83%) | |
| 7–8 weeks | 20 (37.70%) | 13 (44.83%) | 7 (29.17%) | |
| >8 weeks | 5 (9.40%) | 5 (17.24%) | 0 (.00%) | |
| Reduction | 0.171 | |||
| Anatomical | 35 (66%) | 22 (75.86%) | 13 (54.17%) | |
| Aligned | 18 (34%) | 7 (24.14%) | 11 (45.83%) | |
| Poor alignment | 0.459 | |||
| No | 46 (86.80%) | 25 (86.21%) | 21 (87.50%) | |
| Yes | 7 (13.20%) | 4 (13.79%) | 3 (12.50%) | |
| Pain | 0.003 | |||
| No | 29 (54.70%) | 10 (34.48%) | 19 (79.17%) | |
| Yes | 24 (45.30%) | 19 (65.52%) | 5 (20.83%) | |
| Implant removal | 0.294 | |||
| No | 37 (69.80%) | 18 (62.07%) | 19 (79.17%) | |
| Yes | 16 (30.20%) | 11 (37.93%) | 5 (20.83%) | |
In terms of delayed fracture healing, 12 patients (49%) in the plate group (6 by minimally invasive surgery “MIPO” and 6 by open surgery) suffered delayed fracture healing compared to 7 patients (29%) in those treated by intramedullary nailing (p>0.05). Two cases in the plate group (6.8%) developed pseudarthrosis compared to one (4.1%) with nailing (p>0.05).
The onset of weight-bearing ambulation was earlier in the nail group (3rd–4th week) compared to the plate group (5th week) and these differences were significant (p<.05).
When we compare the unloading time of each group with the rate of consolidation, we see that there is no direct relationship, i.e. the patients who load before the nail group, do not therefore achieve fracture consolidation before the plate group (p>.05).
In relation to the misalignments of the extremity, four patients in the plate group (13%) and three in the nail group (12.5%), consolidated with more than 5 angulations, with valgus deformity being more frequent (p>0.05). No relationship was found to exist between malalignment and the pain variable.
With regard to complications (excluding the pain variable), we found no significant differences between the two groups.
Four patients (13.7%) treated with plaque had complications: two suffered from reflex sympathetic syndrome, requiring specific treatment by the rehabilitation service and the pain unit. The third patient suffered from traumatic neuropathy of the posterior tibial nerve and hallux extensor, together with hypoaesthesia of the first intermetatarsal space. On a sensory level the patient has recovered completely, however, the posterior tibial paresis has not recovered and he suffers loss of the plantar arch which he corrects by orthosis. We consider that this complication is due to the trauma that caused the fracture and the soft tissue contusion and not to the surgical act.
The fourth case is a medial wound closure defect with no signs of infection that healed by secondary intention.
In the nail group three patients (12.5%) developed complications: one patient with a high energy fracture developed a subacute compartment syndrome of the posterior compartment with sequelae of claw toe and two patients lost active extension of the hallux and suffered paresthesia of the first intermetatarsal space. At 3 months both had fully regained mobility and sensibility without the need for treatment.
Specifically analysing the pain variable, we found that in the plate group 19 patients (65%) reported discomfort at the medial level over the implant, while in the nail group only 4 patients (16.6%) reported knee pain at 6 months follow-up, having used the transtendinous approach in 3 of the 4 cases (p<0.05).
In the plaque group, implant removal was performed in 11 patients, the remaining 8 declined surgery and opted for conservative analgesic treatment.
In the nail group, of the four patients who reported anterior knee pain, in one case there was a spontaneous resolution of the symptoms without specific treatment 6 months after surgery.
Two other patients continue with pain, one patient after failure of conservative treatment is awaiting arthroscopy to help identify the cause of pain and its management and the other patient is being treated by infiltration of the patellar tendon with platelet-rich plasma with a clear improvement of the symptoms.
The fourth patient reported pain on exploratory manoeuvres of the patellofemoral joint and was checked arthroscopically, confirming arthrosis of the patellofemoral joint. In this case the approach used was paratendinous.
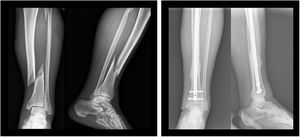
With regard to the removal of material, in the nail group this was carried out in five patients, three had discomfort on the proximal screws as they protruded into the skin, in the fourth patient the distal screws were removed in order to dynamise the system, thus favouring consolidation (Fig. 3), and the fifth patient requested the removal of the entire system, intramedullary nail and distal and proximal locking screws, without any clinical symptoms.
DiscussionThere is currently no consensus on the therapeutic management of distal tibial fractures without joint extensión.16–18
The distal tibia is a complex anatomical segment, with poor vascularisation and a poor overlying antero-medial aspect. As shown in their study by Yut et al.,19 the main factor for delayed or non-union of the fracture is insufficient blood supply due to injury to the soft tissues surrounding the fracture.
In our study the rate of pseudoarthrosis is 6.8% in the plate group and 4.1% in the nail group (p>0.05). These results are in agreement with those published by Vallier et al.8 in their prospective randomised study, where they found no significant differences between patients treated with nail versus locked plate. However, they did find a relationship between the rate of pseudarthrosis and the fact that the fractures were open (p<0.05).
In the meta-analysis published by Ekman et al.,20 they observed that the early onset of loading in patients treated with an intramedullary nail compared to those treated with a plate is common in the studies analysed. This is due to the fact that the intramedullary nail withstands axial loading better, a pattern which also occurs in our study, although not statistically significant, but marking a trend.
Regarding the correct alignment of the fracture and its influence on the functional outcome, previous studies have demonstrated its importance. In the study by Puno et al.21 where they evaluated 28 fractures in 27 patients with a follow-up of 8.2 years, analysis showed that the greater the degree of ankle joint angulation, the worse the clinical outcomes.
In our study we observed no significant differences in the degree of fracture alignment in both treatment groups. This differs from the study published by Wani et al.,22 where they show that rotational malalignment is significantly higher in patients treated with intramedullary nailing.
Several studies have been published with options to increase the stability of the distal fragment in intramedullary nail treatment to avoid possible malalignment. Moongilpatti et al.23 performed a prospective study on 20 patients with metaphyseal fractures of the distal third of the tibia treated by intramedullary nailing with static distal locking and supplemented by locking screws adjacent to the nail. They suggest that this conformation helps to maintain proper reduction of the distal fragment providing greater stability to distal metaphyseal fractures. This could extend the indication for intramedullary nailing to the detriment of the plate. Very similar results have been published by Shahulhameed et al.23 using Poller screws.
With regard to complications (excluding the pain variable), in our series we found an incidence of 13.7% in patients treated with a locked plate and 12.5% in those treated with a nail. These results are comparable to those published by Kasper et al.12 in their study of 24 patients (12 cases in the plate group vs. 12 in the nail group), with an incidence of 16% in patients treated with a plate (2 cases, a superficial infection and paralysis of the hallux extensor leading to claw toe deformity), while in their nail group the percentage of complications rises to almost 35%, much higher than ours.
Among the complications, it should be noted that no superficial or deep infection was recorded. This result differs from the results published by Vallier et al.8 who report an infection rate of 5.8%, with all patients requiring surgical debridement and intravenous antibiotherapy. In this study, the presence of infection is significantly related to the presence of open fractures, ruling out surgical time as a determining factor for the development of infection.
Regarding anterior knee pain, this is one of the most frequent complications associated with the treatment of tibia fractures using an intramedullary nail.
Numerous factors have been described as contributing to this pain, such as damage to the articular surface, injury to the infrapatellar branch of the saphenous nerve or Hoffa's fat, nail prominence, an anatomically narrow tibial plateau or injury to the intermeniscal ligament.24 The incidence described in the literature varies from 31% to 86% depending on the series.9,25,26
In our group of 24 patients treated with an intramedullary nail, an infrapatellar (IF) approach was used in 18 cases (9 transtendinous and 9 paratendinous) and in 6 cases a suprapatellar (SP) approach. After more than 6 months of follow-up, four patients reported pain. An IF approach was used in all cases, with three cases being transtendinous and one paratendinous. No patient who underwent the suprapatellar technique reported anterior knee pain (p<0.05).
Lu et al.27 have already published in their study how the group that underwent the SP approach had a better pain score using the visual analogue scale as a measure compared to the patients who underwent the IF approach. Results observed in the multicentre study by MacDonald et al.28 show that pain in the immediate postoperative period is lower in patients who underwent surgery using the SP approach.
While it is true that there are contradictory studies published in the literature on this subject, in their retrospective study Ozcan et al.29 found no significant differences in anterior knee pain or joint function when comparing the three main approaches, transtendinous, paratendinous and suprapatellar.
The reoperation rate in the plate group was 45%, the main reason being the pain patients reported at the metaphyseal–diaphyseal transition over the plate. Lau et al.30 report in their study that half of the patients they have treated with MIPO plate have had the material removed due to skin discomfort. They justify this fact on the basis of the thin skin overlying the tibia, the deficient conformation of the plate and its prominent thickness.
While in the nail group the rate of a second surgery is slightly lower at 29%.
Our study has a number of limitations as it is a retrospective study and did not take into account the associated fibula fracture as a variable or whether it required surgical treatment.
ConclusionGiven the clinical-radiological results obtained, we consider that both intramedullary nail osteosynthesis and locked plate osteosynthesis are valid options in the treatment of fractures of the distal third of the tibia, with no difference in healing between the two techniques, and with earlier deambulation with weight bearing in the nail group. With regard to complications, pain was the most frequent in both groups, leading to the extraction of the material in a significant number of cases.
Despite this, the latest meta-analyses carried out based on published articles conclude that it is necessary to carry out prospective randomised clinical trials to better define the results of the different types of treatment in extra-articular fractures of the distal third of the tibia.31
Level of evidenceLevel of evidence IV.
Conflict of interestsThe authors have no conflict of interests to declare.
Protection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.