Peripheral trauma is a very frequent cause of consultation in paediatric emergency departments but few studies have been published describing the characteristics of these patients.
Material and methodsWe performed a retrospective descriptive study by reviewing computerised emergency department forms during January and February 2020.
ObjectiveTo describe the characteristics of traumatic injuries in our area and to detect possible areas for improvement.
ResultsA total of 714 peripheral trauma cases were attended, which represents 9.5% of the total consultations. A total of 52.7% were schoolchildren (6–11 years). The most frequent locations were the ankle (27.5%) and fingers (17.2%). Fracture was detected in 6.7% of cases. Radiographs were requested in 78.6% of the patients, with pathological findings in 9.6% of them. Half of the X-rays were requested due to ankle or finger trauma. Referral to traumatology was made in 16.4% of patients, mainly for elbow and knee trauma, and the most commonly used treatment was general measures (49%) and bandaging (29.4%).
ConclusionsPeripheral trauma is very common and, in general, banal. A large number of X-rays are requested with a very low yield, so it seems necessary to establish new protocols to reduce the number of requests. Improving training in elbow and knee trauma could improve paediatricians’ autonomy in dealing with these more complex injuries.
Los traumatismos periféricos son una causa muy frecuente de consulta en las urgencias pediátricas, pero apenas se han publicado estudios que describan las características de estos pacientes.
Material y métodosSe realiza un estudio descriptivo retrospectivo mediante revisión de formularios informatizados de urgencias pediátricas durante los meses de enero y febrero de 2020.
ObjetivoConocer las características de la patología traumática pediátrica de nuestra área y detectar posibles puntos de mejora.
ResultadosSe atendieron 714 traumatismos periféricos, lo que supone 9,5% de las consultas totales. De los pacientes presentados, 52,7% fueron escolares (seis a 11 años). Las localizaciones más frecuentes fueron el tobillo (27,5%) y los dedos de la mano (17,2%). Se detectó fractura en 6,7% de los casos. En 78,6% de los pacientes se solicitó radiografía, siendo patológica 9,6% de las mismas. La mitad de las radiografías se solicitaron por traumatismo en el tobillo o dedos de la mano. Se realizó interconsulta a traumatología en 16,4% de los pacientes, sobre todo en traumatismos de codo y rodilla, y el tratamiento más empleado fueron las medidas generales (49%) y el vendaje (29,4%).
ConclusionesLos traumatismos periféricos son muy habituales y, en general, banales. Se solicita un gran número de radiografías con una rentabilidad muy baja, por lo que parece necesario establecer nuevos protocolos que permitan reducir el número de peticiones. Mejorar la formación respecto a los traumatismos de codo y rodilla podría mejorar la autonomía de los pediatras respecto a este tipo de lesiones, más complejas.
Trauma injury accounts for a high percentage of consultations in paediatric emergency departments (PED), comprising between 20% and 30% of all visits.1–6 This percentage increases by age group, up to 50% of consultations in the case of adolescents.2 Furthermore, it seems that this percentage has been increasing in recent years,1 which may be due to guardians increasingly preferring to consult hospitals rather than other healthcare centres.5
It is well known that unintentional trauma injuries are a public health problem, representing one of the main causes of morbidity and mortality in the paediatric population and, hence, not insignificant health expenditure.1 However, most trauma cases assessed in the PED are diagnosed as contusions or sprains, and are considered minor injuries that do not require any major intervention and can be discharged with analgesia and relative rest. Only 20% of cases are diagnosed as major injuries, and fracture is the most common diagnosis (up to 70% of cases).6,7 Fortunately, life-threatening injuries are very rare.6
Despite the high incidence of minor trauma injuries, there are few descriptive studies on the subject and very little scientific evidence on the management of these injuries in children.8 There could be several reasons for this in our setting. There is a lack of homogeneity in the care of these patients in our country. While purely paediatric pathologies are generally treated by paediatric specialists, up to 50% of minor trauma injuries are treated in the first instance by other specialists such as family and community medicine, trauma, or even paediatric surgery specialists.8 This heterogeneity is centre-dependent and influences the establishment of consensus and updated protocols.
This is compounded by the lack of training during the MIR stage. In a recent study on this subject, up to 73% of Spanish paediatricians consulted reported not having received sufficient training in trauma pathology during their residency.8
The aim of this study is therefore to determine the characteristics of the trauma injuries treated in our population and thus be able to detect potential areas for improvement.
Material and methodsA descriptive, retrospective study was conducted in our centre, an intermediate complexity hospital on the outskirts of Madrid that covers a population of approximately 47,000 children, attending 40,000 patients in the paediatric emergency department during 2022.
We have advanced paediatric triage in our centre, the nursing staff being responsible for ordering, according to protocol, complementary tests such as X-rays, even before the patient is assessed by a doctor. The paediatrician provides the initial care of all paediatric trauma patients, and the trauma specialist acts as consultant. If urgent surgical intervention is required, the patient is transferred to a higher-level centre.
For this study we reviewed the electronic emergency forms completed using the Selene computer programme for patients aged 0–15 years seen for trauma injury in the PED between 1 January and 6 March 2020.
All peripheral injuries were included, excluding head, facial, trunk, and polytrauma injuries from the study. Data were collected on demographic variables, location of the trauma, diagnosis, radiography, treatment, consultation with traumatology, or need for transfer to another centre. The data were computer processed with Microsoft Excel 2019 and analysed using the IBM SPSS Statistics 23 (Armonk, New York, USA) statistical package in its Windows version.
The statistical analysis consisted of calculating relative frequencies and the corresponding measures of trend and dispersion according to the characteristics of the variable. The X2 or Fisher's test was used to determine the association between variables, considering a significance level of .05.
This study was conducted with the approval of our centre's research committee, in compliance with the regulations governing access, protection, and confidentiality of patient data. Given that the electronic forms are anonymised, this was considered an exemption situation, and informed consent was not sought.
ResultsOver the two-month study period, a total of 7535 patients were seen in our centre's PED. The reason for consultation was peripheral trauma in 714 cases (9.5).
The median age was 10 years with an interquartile range of 5. Analysing by age group, 52.7% of the patients seen were schoolchildren and 30.3% were adolescents. In terms of sex, we found a male/female prevalence ratio in relation to the reference population of 1.27 (95% CI 1.085–1.456, p=.002). This statistically significant difference is maintained when analysed by age group.
Table 1 shows the overall results and Table 2 shows the results by age group and sex.
Characteristics of patients treated for peripheral trauma in the PED.
| Variables | n | %a |
|---|---|---|
| Total patients | 714 | 100% |
| Clavicle | 3 | .4% |
| Shoulder | 8 | 1.1% |
| Arm | 7 | 1% |
| Elbow | 51 | 7.1% |
| Forearm | 5 | .7% |
| Wrist | 82 | 11.5% |
| Hand | 29 | 4.1% |
| Fingers | 123 | 17.2% |
| Hip | 18 | 2.5% |
| Thigh | 10 | 1.4% |
| Knee | 92 | 12.9% |
| Leg | 30 | 4.2% |
| Ankle | 196 | 27.5% |
| Foot | 31 | 4.3% |
| Toes | 23 | 3.2% |
| Diagnosis | ||
| Contusion | 335 | 46.9% |
| Sprain | 194 | 27.2% |
| Fracture | 49 | 6.9% |
| Skin injury | 34 | 4.8% |
| Painful pronation | 15 | 2.1% |
| Free fluid in the joint | 6 | .8% |
| Osteochondrosis | 3 | .4% |
| Other | 78 | 10.9% |
| Sex | ||
| Male | 408 | 57.1% |
| Female | 306 | 42.9% |
| Age | ||
| Infants | 29 | 4.1% |
| Preschool children | 92 | 12.9% |
| School children | 376 | 52.7% |
| Adolescents | 217 | 30.3% |
| X-rays ordered | 561 | 78.6% |
| Treatment provided | ||
| General measures | 350 | 49% |
| Bandaging | 210 | 29.4% |
| Splinting | 54 | 7.6% |
| Buddy taping | 50 | 7% |
| Sutures | 20 | 2.8% |
| Closed reduction | 7 | 1% |
| Biological glueing | 2 | .3% |
| Other | 6 | .8% |
| Cross-consultation with traumatology | 117 | 16.4% |
| Transfer to another centre | 5 | .7% |
| Repeat consultation in the first week | 15 | 2.1% |
Characteristics of the patients seen by age group and sex.
| Age group | ||||||||
|---|---|---|---|---|---|---|---|---|
| Infant(0–2 years)29 (4.1%) | Preschool(3–5 years)92 (12.9%) | School(6–11 years)376 (52.7%) | Adolescent(12–15 years)217 (30.3%) | |||||
| Male18(62.1%)* | Female11(37.9%)* | Male51(55.4%)* | Female41(44.6%)* | Male209(55.6%)* | Female167(44.4%)* | Male129(59.7%)* | Female87(40.3%)* | |
| Site | ||||||||
| Clavicle | – | – | 1 (.3%) | 2 (.9%) | ||||
| – | – | – | – | 1 | .5% | – | 2 (2.3%) | |
| Shoulder | – | 1 (1.1%) | 5 (1.3%) | 2 (.9%) | ||||
| – | – | 1 (2%) | – | 4 (1.9%) | 1 (.6%) | 1 (.8%) | 1 (1.1%) | |
| Arm | 2 (6.9%) | – | 1 (.3%) | 4 (1.9%) | ||||
| 1 (5.6%) | 1 (9.1%) | – | – | 1 (.5%) | – | 4 (3.1%) | – | |
| Elbow | 6 (20.7%) | 11 (12%) | 22 (5.9%) | 12 (5.6%) | ||||
| 2 (11.1%) | 4 (36.4%) | 3 (5.9%) | 8(19.5%) | 9 (4.3%) | 13 (7.8%) | 6 (4.7%) | 6 (6.9%) | |
| Forearm | – | 1 (1.1%) | 4 (1.1%) | – | ||||
| – | – | – | 1 (2.4%) | 3 (1.4%) | 1 (.6%) | – | – | |
| Wrist | 1 (3.4%) | 5 (5.4%) | 54 (14.4%) | 22 (10.2%) | ||||
| – | 1 (5.6%) | 3 (5.9%) | 2 (4.9%) | 28 (13.4%) | 26 (15.6%) | 13 (10.1%) | 9 (10.3%) | |
| Hand | – | 3 (3.3%) | 13 (3.5%) | 12 (5.6%) | ||||
| – | – | 3 (5.9%) | – | 8 (3.8%) | 5 (3%) | 7 (5.4%) | 5 (5.7%) | |
| Fingers | 5 (17.2%) | 20 (21.7%) | 67 (17.8%) | 31 (14.4%) | ||||
| 2 (11.1%) | 3 (27.3%) | 10 (19.6%) | 10 (24.4%) | 39 (18.7%) | 28 (16.8%) | 17 (13.2%) | 14 (16.1%) | |
| Hip | 2 (6.9%) | 10 (10.9%) | 6 (1.6%) | – | ||||
| 1 (5.6%) | 1 (9.1%) | 6 (11.8%) | 4 (9.8%) | 3 (1.4%) | 3 (1.8%) | – | – | |
| Thigh | – | 3 (3.3%) | 4 (1.1%) | 3 (1.4%) | ||||
| – | – | 2 (3.9%) | 1 (2.4%) | 3 (1.4%) | 1 (.6%) | 2 (1.6%) | 1 (1.1%) | |
| Knee | 2 (6.9%) | 10 (10.9%) | 44 (11.7%) | 36 (16.7%) | ||||
| 2 (11.1%) | – | 8 (15.7%) | 2 (4.9%) | 27 (12.9%) | 17 (10.2%) | 20 (15.5%) | 16 (18.4%) | |
| Leg | 4 (13.8%) | 6 (6.5%) | 15 (4%) | 5 (2.3%) | ||||
| 4 (22.2%) | – | 4 (7.8%) | 2 (4.9%) | 11 (5.3%) | 4 (2.4%) | 4 (3.1%) | 1 (1.1%) | |
| Ankle | 2 (6.9%) | 11 (12%) | 109 (29%) | 74 (34.4%) | ||||
| 2 (11.1%) | – | 4 (7.8%) | 7 (17.1%) | 53 (25.4%) | 56 (33.5%) | 45 (34.9%) | 29 (33.3%) | |
| Foot | 2 (6.9%) | 8 (8.7%) | 17 (4.5%) | 4 (1.9%) | ||||
| 2 (11.1%) | – | 5 (9.8%) | 3 (7.3%) | 11 (5.3%) | 6 (3.6%) | 3 (2.3%) | 1 (1.1%) | |
| Toes | – | 3 (3.3%) | 11 (2.9%) | 9 (4.2%) | ||||
| – | – | 2 (3.9%) | 1 (2.4%) | 7 (3.3%) | 4 (2.4%) | 7 (5.4%) | 2 (2.3%) | |
| Diagnosis | ||||||||
| Contusion | 13 (44.8%) | 35 (38%) | 189 (50.3%) | 98 (45.4%) | ||||
| 10 (55.6%) | 3 (27.3%)* | 22 (43.1%) | 13 (31.7%)* | 105 (50.2%) | 84 (50.3%)* | 64 (49.6%) | 34 (39.1%)* | |
| Sprain | 1 (3.4%)* | 11 (12%)* | 108 (28.7%)* | 74 (34.3%)* | ||||
| 1 (5.6%)* | – | 4 (7.8%)* | 7 (17.1%)* | 50 (23.9%)* | 58 (34.7%)* | 41 (31.8%)* | 33 (37.9%)* | |
| Fracture | 3 (10.3%) | 10 (10.9%) | 23 (6.1%) | 12 (5.6%) | ||||
| 1 (5.6%) | 2 (18.2%) | 6 (11.8%) | 4 (9.8%) | 17 (8.1%) | 6 (3.6%) | 8 (6.2%) | 4 (4.6%) | |
| Other | 10 (34.5%) | 23 (25%) | 56 (14.9%) | 12 (5.6%) | ||||
| 6 (33.3%) | 6 (54.5%) | 19 (37.3%) | 17 (41.5%) | 37 (17.7%) | 19 (11.4%) | 16 (12.4%) | 16 (18.4%) | |
| X-rays performed | ||||||||
| 13 (44.8%)* | 60 (65.2%)* | 304 (80.9%)* | 183 (84.7%)* | |||||
| 9 (50%)* | 4 (36.4%)* | 34 (66.7%)* | 26 (63.4%)* | 167 (79.9%)* | 137 (82%)* | 112 (86.8%)* | 71 (81.6%)* | |
The most common sites of trauma were ankle (27.5%), fingers (17.2%), knee (12.9%), wrist (11.5%), and elbow (7.1%). Contusion was the most common diagnosis (46.9%), followed by sprain (27.3%).
Fracture was detected in 6.7% of cases. The diagnosis of fracture was considered after assessment by the trauma specialist, except in two cases in which it was made directly by the paediatrician. Both cases were diagnosed as low-risk fractures of the phalanges of the hands and were discharged without cross-consultation with the trauma department. Of the patients diagnosed with fracture and evaluated by traumatology, up to 89.36% of the cases (42/47) had been previously diagnosed by the paediatrician. In the remaining five patients, in whom the paediatrician did not detect a fracture, a diagnosis of grade I epiphysiolysis (one of the fibula and two of the radius) was made by traumatology in 60% (3/5). Another patient was diagnosed with “tuft” fracture of the distal phalanx of the hand (1/5), and another with clavicle fracture (1/5).
The fractures detected were located in the upper limbs in 81.6% of patients (40/49). Fracture of the wrist was the most common at 44.9% (22/49). Fig. 1 shows the data in relation to the diagnosis by site and Table 3 shows the types of fracture found.
X-rays were taken in 78.6% of the patients, 9.6% of which were pathological (49/513). Almost half of the X-rays were ordered for trauma to the ankle (29.4%) or fingers (16.5%). Fig. 2 lists the X-rays performed by site.
If we analyse the X-rays ordered by age group, we can see an increase in the number of those ordered as age increases, going from 44.8% in the infant group (13/29) to 84.7% in the adolescent group (183/216); this difference is statistically significant. In contrast, the proportion of fractures diagnosed decreases slightly with increasing age, from 10.3% (3/29) to 5.6% (12/216), as can be seen in Fig. 3; this difference is not statistically significant.
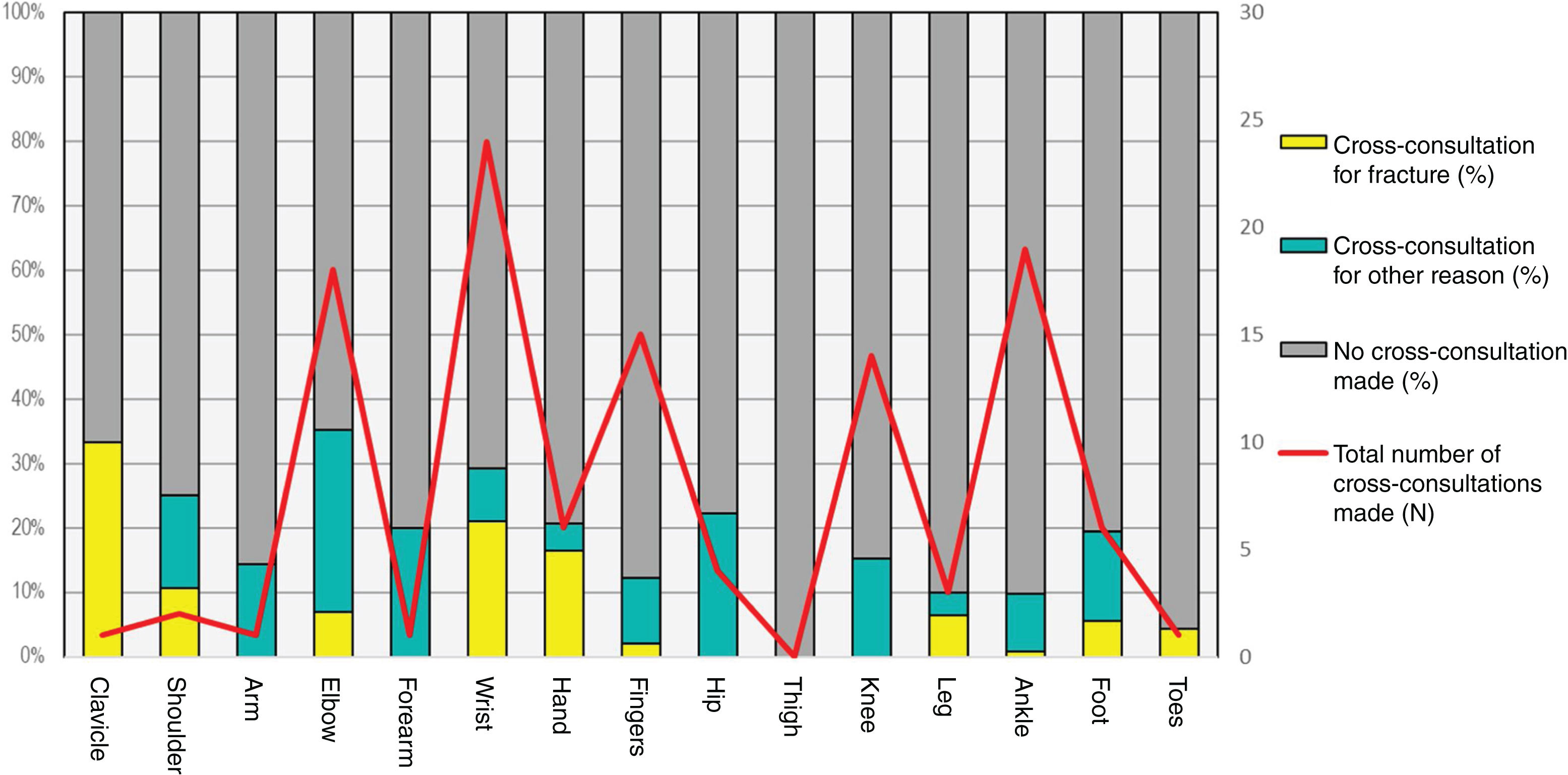
Cross-consultation with traumatology was requested in 16.4% of cases, and the most common reasons were ankle trauma (16.2%) and elbow trauma (15.4%). If we analyse by site, elbow trauma is proportionally the most frequently seen, at 35.3% of cross-consultations (18/51), followed by wrist trauma at 29.3% (24/82). In practically all cases of fracture (85.7%), assessment by traumatology was requested. If we consider only those patients who were not diagnosed with fracture, the percentage of cases for which traumatology was consulted dropped to 11.3%, the most common sites being the elbow (28.3%, 13/46) and the knee (15.2%, 14/92). Fig. 4 lists cross-consultations by site.
Overall, general measures were the most common treatment used, namely anti-inflammatory drugs, local cold, and relative rest (49%), followed by bandaging (29.4%). Closed reduction was performed in 14.3% of the fractures (7/49) and .7% (5/714) of the cases were transferred to the referral hospital for different reasons.
Of the patients, 2.1% (15/714) returned to the PED for the same trauma in the first week after the initial diagnosis. Of the cases, 46.7% (7/15) had previously been diagnosed with ankle sprain; this new consultation did not result in a change in diagnosis. Of the patients who consulted again, 33.33% (5/15) had a change in treatment: in one patient with an ankle sprain treated with a bandage, the bandage was removed due to toe oedema, in another patient diagnosed with a knee contusion treated with general measures a knee brace was indicated, and in the remaining three patients, two of whom were diagnosed with a radius fracture and the other with an ankle sprain, a change of splint was made due to complications with the splint (chafing or toe oedema).
A secondary analysis of the most common pathology was performed. In the case of ankle trauma, X-rays were ordered in 85.2% of cases, the most common diagnosis being sprain (85.7%), followed by contusion (10%). The proportion of sprains increased with age, from 3.4% in infants to 34.4% in adolescents (p=.001). In the school children group the proportion of females who were diagnosed with sprain was higher than expected (p=.021), with no differences in the other age groups. Fracture was found in 1% of cases. The most common treatment was bandaging (60.7%), followed by general measures (26%), and splinting (8.7%).
Radiography was ordered in 89.4% of cases of finger trauma, the most common diagnosis being contusion (74.8%). Fracture was found in 4.1% of cases. The most common treatment was general measures (39.8%) and buddy taping (34.1%).
DiscussionPeripheral trauma is one of the main reasons for consultation in our PED. Because we only analysed the months of January and February, months with a high demand for care, the proportion could be even higher in other periods of the year.
The proportion of males seen for this reason is higher than that of females, regardless of age; schoolchildren being the age group making the highest number of consultations, followed by adolescents.
The ankle is the most frequent site, followed by the fingers, and the two together account for almost half of the visits for peripheral trauma.
Most cases assessed in the PED are considered minor injuries, in line with previously published evidence.6 However, we found a very low incidence of major injuries, lower than that reported in other articles.6 This may be because most previous studies include other types of trauma such as head injuries and polytrauma, not only peripheral trauma. Another reason is the greater tendency on the part of guardians to consult hospital PEDs for trivial injuries.
A higher proportion of sprains is observed at older ages compared to other diagnoses, which has been previously reported in the literature. It is curious, however, that the proportion of sprains in the female population within the group of school children is higher than expected compared to the male population.
Despite the benign nature of most of the trauma injuries assessed, X-rays are ordered in almost all cases. Less than 10% of them are pathological, which indicates that it is likely that this imaging test was not really necessary in some patients. This situation is even more striking if we consider the analysis by site. Only 1% of the ankle X-rays were pathological and only 4% in the case of the fingers. We can also see that as age increases, the number of X-rays ordered increases without an increase in the severity of the injuries sustained. It is interesting, therefore, to consider implementing measures that help detect patients at high risk of fracture, such as the Ottawa criteria for the ankle or knee, thus reducing, as far as possible, the number of X-rays ordered. The advantages of these measures are well known, as they not only reduce the radiation emitted, but also considerably reduce waiting times in the emergency department and healthcare costs.
The main reason for requesting an assessment by traumatology is the presence of a fracture. If we disregard this condition, there was cross-consultation in only 11% of cases, although in the case of elbow and knee trauma this increased to 28.3% and 15.3%, respectively. These differences indicate the difficulty of approaching this type of injury. We cannot confirm in this study whether this is due to the complexity of these injuries or to a lack of confidence on the part of the paediatricians attending them. Therefore, it would be appropriate for further studies to assess whether the number of cross-consultations to traumatology can be reduced if training sessions and protocols are implemented and agreed between the two services.
General measures were the most common treatment, corresponding to the benign nature of the injuries. Compressive bandaging was used in approximately one third of patients, most commonly for ankle trauma. Splinting was used for fractures or moderate-severe sprains (8.7% of sprains). Fractures requiring closed reduction were rare and those requiring transfer to a tertiary hospital exceptional.
There were few patients who consulted again in the first week after the trauma, and this was generally due to persistence of symptoms. However, in up to 20% of patients, complications caused by the earlier immobilisation were the reason for repeat consultation in the PED.
The present study has limitations that would be expected of a retrospective study. It is difficult to assess the final outcome of the patients since only our centre's clinical histories were reviewed, and it is impossible to know whether they later visited another health centre. Potential errors in establishing the definitive diagnosis and their impact on the results obtained must also be considered.
ConclusionsPeripheral trauma is a very important reason for consulting our PED, half of these visits being for trauma to the ankle or fingers.
Males consult more than females for peripheral trauma, and this difference is maintained over all age groups.
There is a higher proportion of sprains with increasing age. In addition, females are diagnosed with sprains more frequently than males in the school children group.
X-rays are ordered in almost all peripheral trauma cases and are normal in most cases. It would be advisable to establish new protocols specifying clinical criteria to allow the selection of patients with a greater risk of fracture and thus reduce the number of X-rays ordered.
Cross-consultation with traumatology is more frequent for elbow and knee trauma, complex joints that require special management. The establishment of protocols and training sessions could increase the autonomy of paediatricians in this respect.
Level of evidenceLevel of evidence iv.
FundingNo funding was received for this study.
Conflict of interestsThe authors have no conflict of interests to declare.