Bone-preserving implants in primary total hip arthroplasty have become an increasingly popular treatment choice, especially short stems. Currently there are many models with morphological and biodynamic differences, among which stand out the neck-retaining systems, but there are not many studies with a long-term follow-up of these systems. The objective of this study is to retrospectively analyse the results of the Collum Femoris Preserving (CFP) short neck-retaining stem system with a minimum follow-up of 10 years.
Material and methodsBetween 2001 and 2010, 175 prostheses with a CFP stem were performed in 157 patients in our hospital. All patients were operated on by a single surgeon. The mean age at the time of surgery was 56.47 years (range 22–77).
Results175 prostheses have been evaluated with a minimum follow-up of 10 years and a mean of 13.89 years (range 10–19), with 16 cases having been lost. During the follow-up there were 8 polyethylene replacements, 2 cup replacements due to loosening, 2 osteosynthesis due to fracture without loosening, and 5 stem replacements: 1 due to chronic infection, 2 due to fracture and 2 due to aseptic loosening.
ConclusionsAs far as we know, this is the first follow-up work on a short stem implanted in our country with a minimum of 10 years of follow-up. The replacement of this stem due to aseptic loosening has been 2/159 and, therefore, survival for this reason is 98.75% at 10 years.
Las técnicas de preservación ósea en prótesis totales de cadera primarias han experimentado un gran auge en los últimos años, especialmente los vástagos cortos. Actualmente existen muchos modelos con diferencias morfológicas y biodinámicas, entre los cuales destacan los sistemas con preservación del cuello femoral, pero no existen muchos trabajos con un seguimiento a largo plazo de estos sistemas. El objetivo de este trabajo es analizar retrospectivamente el resultado del sistema de vástago corto con preservación de cuello femoral (collum femoris preserving [CFP]) con un seguimiento mínimo de 10años.
Material y métodosEntre los años 2001 y 2010 se realizaron 175 prótesis con vástago CFP en 157 pacientes en nuestro hospital. Todos los pacientes fueron intervenidos por un único cirujano. La edad media en el momento de la cirugía fue de 56,47años (rango 22-77).
ResultadosSe han evaluado 175 prótesis con un seguimiento mínimo de 10años y una media de 13,89años (rango 10-19), habiéndose perdido 16 casos. Durante el seguimiento ha habido 8 recambios de polietileno, 2 de cótilo por aflojamiento, 2 osteosíntesis por fractura sin aflojamiento y 5 recambios de vástago: uno por infección crónica, 2 por fractura y 2 por aflojamiento aséptico.
ConclusionesHasta donde sabemos, es el primer trabajo de seguimiento de un vástago corto implantado en nuestro país con un mínimo de 10años de evolución. Los recambios de este vástago por aflojamiento aséptico han sido 2/159 y, por tanto, la supervivencia por este motivo es del 98,75% a los 10años.
The total hip prosthesis (THP) is a surgical resource that is widely used throughout the world, and which has proven over the years to be a highly cost-effective procedure, offering a notable improvement in the quality of life of the patients who undergo surgery.
Since the early work of Charnley,1–4 who conducted evolutionary studies of the patients in whom he implanted his prosthesis, countless recent studies have appeared with different models and designs, fixation systems, friction torques, materials, etc. always trying to improve the survival of these implants.
The great challenge has always been to extend the life of these implants and to facilitate their replacement when necessary, preserving the greatest possible amount of bone remnant. On the other hand, prostheses are increasingly being implanted in younger patients, with greater functional demand and in whom it is more necessary to preserve the bone. In this sense, preservation techniques have appeared, among which the use of short stems stands out, enjoying great popularity in recent years.5–8
There are currently many models with notable differences in their design and biomechanical behaviour, among which systems with preservation of the femoral neck stand out. Studies showing their short- and medium-term results have been appearing in the literature over the last decade.9–21 Unfortunately, there are few studies in the literature with long-term follow-up of these systems.22–24
The aim of this study was to retrospectively analyse the result of the Collum Femoris Preserving (CFP) system as a short stem system of femoral neck preservation in a single centre cohort of patients who underwent surgery in our hospital, by a single surgeon with a minimum case follow-up of 10 years.
Material and methodsStudy designA retrospective, single-centre clinical study (Hospital Universitario Sant Rafael, Barcelona) was performed according to the Declaration of Helsinki of the World Medical Association to assess the survival of this stem, establishing as end point the situation of replacement due to aseptic loosening. From October 2001 to December 2010, a total of 175 consecutive primary THPs were performed by a single surgeon in our Department with the CFP stem (Waldemar Link, Hamburg, Germany) and followed up for a minimum of 10 years until December 2020. The cohort (175 THP in 157 patients) included 48 women and 109 men. Of the operated hips, 91 were left and 84 right; 18 patients underwent THP bilaterally. The mean age at the time of surgery was 56.47 years (range 22–77 years). Osteoarthritis of the hip was the most common preoperative diagnosis. Exclusion criteria for stem implantation included patients with hip dysplasia with anatomical deformities of the femoral head or femoral neck of any aetiology, femoral neck fractures and hips with a history of septic disease. All cases were reviewed in clinical consultation or by telephone call or through the Shared Clinical History of Catalonia (HCCC for its initials in Spanish).
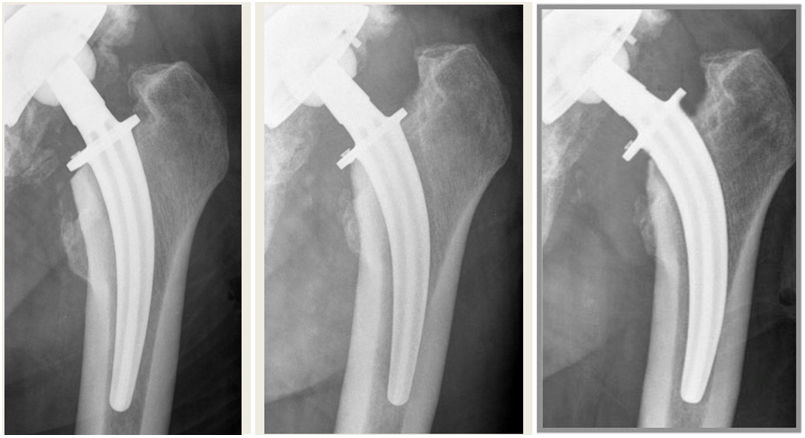
Prosthetic modelCFP stems are short femoral neck preservation stems because the osteotomy of the femoral neck is performed at the level of the isthmus, thus preserving more than 50% of the neck. On the other hand, the bone marrow is prepared using cancellous bone compressors instead of a rasp. They are made of an alloy known as Tilastan® (TiAl6V4) and promote osseointegration with a thick microporous surface coated with hydroxyapatite (thickness of 20m in the proximal 2/3). The short distal part is only a guide to improve insertion into the femoral medullary canal and does not show osseointegration (Fig. 1). It is an anatomical stem and there is a left and a right version with 6° anatomical anteversion with 5 sizes and 2 curvatures (A and B) to improve the fit in the femoral neck. Two different acetabular systems were used: the TOP (Trabeculae-Oriented Pattern) (Waldemar Link, Hamburg, Germany) with a polyethylene insert and the Betacup (Waldemar Link, Hamburg, Germany) with a ceramic insert (Biolox delta, Ceramtec AG, Plochingen, Germany) for young patients from 2007 onwards. Ceramic heads (Biolox forte, Ceramtec, AG, Plochingen, Germany) of 28mm were used in TOP cups and ceramic heads (Biolox delta, Ceramtec AG, Plochingen, Germany) of 36mm (32mm in smaller cups) were used in Betacups with a diameter of more than 50mm. Curve A was implanted in 142 hips and curve B in 33. Stem size was extra-small in 32 cases, small in 63, medium in 61, large in 16 and extra-large in 3.
Surgical procedureAll procedures were performed by an experienced orthopaedic surgeon, with the patients in lateral position and using a standard posterior approach. Anaesthesia was general or regional. The final stem size was decided intraoperatively with the help of proper preoperative planning to choose the type of curvature. The method used for the final decision was to check the torsional stability achieved with the bone compressor within the femoral medullary canal: in cases where rotation was observed, a larger size was checked until no or minimal rotation was observed. To prevent deep vein thrombosis, enoxaparin was administered for 30 days postoperatively according to the guidelines of the Spanish Society of Orthopaedic Surgery. NSAID prophylaxis was not administered to prevent heterotopic ossification. Patients were able to stand upright 24h after surgery and partial weight bearing with two crutches was allowed for 3 weeks progressing to full weight bearing with one crutch for 1–3 weeks.
ResultsA total of 175 prostheses were studied with a minimum follow-up of 10 years and a mean follow-up of 13.89 years (range 10–19), with a total of 16 losses. The total number of losses was distributed as follows: 5 patients had died of non-procedural causes during the first 10 postoperative years and the remaining 11 patients were lost to follow-up (patients who had moved residence and others who could not be contacted). There were no dislocations of the prosthetic hips during the study period. Two patients had acetabular aseptic loosening requiring acetabular replacement. The polyethylene had to be replaced on its own in 6 patients due to progressive wear of the polyethylene as confirmed by radiological evolutionary study. Two intraoperative femoral fractures were observed that did not require additional treatment: one periprosthetic fracture of the diaphysis and one metaphyseal fracture. A chronic Staphylococcus aureus infection was also observed that was treated with a 2-stage prosthesis replacement and 2 post-traumatic periprosthetic fractures at 3 and 102 days, treated with femoral revision in one case and osteosynthesis in the other. Finally, 2 aseptic femoral loosening were identified and treated by revision and replacement (Figs. 2 and 3).
The CFP system was first clinically tested in 1997 (Orthopaedic Clinic, University of Genoa, Italy).25 Studies more than 15 years ago have already shown that femoral neck preservation hip replacement restores natural hip displacement and balances the tension of the medial musculature and pelvitrochanteric muscles, and the patient's bone reacts around the components whilst preserving their mineral contents.25,26
Concern about preserving the femoral neck to improve clinical outcomes after THP is nothing new. In 1995 Whiteside et al.27 initiated a study on the pretext that loosening of the femoral component in THP usually results from inadequate resistance to torsional loading. They determined the effect of different levels of femoral neck resection on the torsional strength of adult human cadaver femurs, publishing as results increased torsional strength with greater preservation of the femoral neck: retaining the entire femoral neck was more effective in reducing micromotion at low loads, while retaining the mid-diaphyseal area of the femoral neck was more effective in controlling micromotion at higher torsional loads. A resection below the mid-diaphysis of the neck significantly decreases the torsional load responsiveness of the proximal femur.
Along these lines, 6 years later Kim et al.28 performed a cadaveric study comparing a conventional femoral stem and a new, much shorter and more anatomical proximal insertion femoral stem. They published results that the new metaphyseal socket stem with no contact with the distal cortex provided immediate postoperative stability, reduced flexion stiffness with tapering of the stem, reduced stress shielding with no contact between the stem and distal cortex, reduced bone resorption and reduced thigh pain. This study was conducted in the context of previous work by Jasty et al.,29 who demonstrated in a canine model that in a proximal-only overlay stem that achieves immediate proximal stability, the distal portion of the stem has no biomechanical contribution.
Against this research backdrop, in the 1990s, the introduction of short stems with femoral neck preservation in selected patients gradually began, with the first CFP prosthesis implanted in our case in October 2001. Initially we reserved this model for young patients requiring a THP. Over the years of experience in its implantation and with several years of follow-up of the implanted prostheses, the age of the patients in whom we implanted this type of model has been increasing. We have also increased the average age of indication of this prosthesis with the increase in the quality of life of the population, as well as the life expectancy of our society.
This opening in the age range of patients has been due to the promising results obtained in our sample when the components were placed normally positioned according to the surgical technique: we have only observed 2 cases of aseptic loosening of the stem, and these were due to excessive undersizing of the stem, which caused subsequent loosening and varisation of the stem. There were no prosthetic dislocations. Only 3 patients reported mild thigh pain and 2 reported significant trochanteric pain that resolved spontaneously. The radiological findings are quite similar to the results reported by the designer of this system,25,26 with some differences: calcar resorptions were found due to oversized stems and in one case without apparent cause (we suspect a subacute infection with a low virulence bacterium).
In our series, heterotopic ossifications were much less frequent (7.9%) than in Pipino's series (44%).25,26 This difference may be due to the approach: Pipino used the Watson-Jones approach and found ossifications in the greater trochanter near the insertion of the gluteus minimus and vastus lateralis muscle, whereas in our case a posterior approach was always used and some grade I heterotopic ossifications were observed near the acetabular rim.
We believe that a minimal undersizing but with good stem alignment will provide a good medium and long-term result, whereas an oversized stem may cause metaphyseal fractures or neck resorption due to distal fixation, as also described by Pipino and Pons et al.25,30
In terms of limitations, the main limitation of this study is the small cohort of patients, mainly due to the inclusion of patients who were recipients of a cementless stem (our philosophy is that in patients over 75 years of age we practically always opt for a cemented stem, especially in the case of female patients) and to the fact that in the beginning we looked for very selected patients to improve the learning curve. This makes our sample considerably smaller than that of the study with the largest number of patients, by Wacha et al. who included 144 patients over 80 years of age.24 Other important limitations are the classic limitations of retrospective studies, as is the case in our review.
The main objective of the study was to evaluate clinical outcomes and analyse survival after femoral neck-sparing THP implantation using the CFP model with minimal long follow-up. We observed that the CFP system has provided excellent results to date with a survival of 98.75% at 10 years of minimum follow-up if we exclusively evaluate replacements due to aseptic loosening, being a very valid option for primary THP implantation if the aim is to preserve as much bone as possible. To our knowledge, this is the first study published in our country to evaluate the survival of a short stem with a minimum follow-up of 10 years.
It has not been the aim of this study to compare the different short stem options on the market with each other, with good results published in the short and medium term for both the stem placed in our case9–12 and in other existing options.13–21 Our interest lies in observing this large group of published studies with the low volume of published studies with a long follow-up.22–24 In this sense, a greater number of long-term studies of both this CFP model and others that preserve the femoral neck are required to determine the best options not only in young patients who require a THP but also in elderly patients, as another alternative in the range of possibilities for implanting a primary THP.
Finally, we would like to point out that since 2019 we have been conducting an international multicentre study to assess the behaviour and initial results of the evolution of the CFP system to CFP II, a system with the same philosophy but with changes in its design that we believe may improve its biomechanical behaviour.
ConclusionsTo our knowledge, this is the first follow-up study of a short stem implanted in our country with a minimum of 10 years of evolution. The number of replacements of this stem due to aseptic loosening was 2/159 and, therefore, the survival rate for this reason is 98.75% at 10 years.
Level of evidenceLevel of evidence IV.
FundingThis study did not receive any specific funding from the public sector, the commercial sector or not for profit entities.
Conflict of interestsThe authors have no conflict of interests to declare.