Although conservative treatment of calcific tendinopathy has a high success rate, arthroscopic excision of the calcific deposit is occasionally necessary. Controversy exists as to whether the remaining rotator cuff defect can be left in situ or should be repaired to achieve better functional outcomes. This study aimed to compare the results of debridement versus debridement combined with suturing in arthroscopic surgery for calcific tendinopathy.
MethodologyMEDLINE, EMBASE, Cochrane Library, and Web of Science were searched from inception to February 2023 for articles on arthroscopic treatment of calcific tendinopathy. Functional outcomes (VAS, ASES, UCLA, and Constant) and the number of complications were analyzed. The effect size was calculated using Cohen's d-index.
ResultsTwenty-one studies were included, including a total of 1172 patients aged between 44.7 and 55 years. The mean follow-up time was 24.7 months. The combined ES estimates for the total score of the VAS, ASES, UCLA, and Constant scales were very strong (>1.0) for both debridement and combined debridement with suture. The ES estimates for the number of total complications were 1.75 (95% CI: 0.08–3.43, I2=0%) for debridement and 9.07 (95% CI: −0.03 to 18.17, I2=50.4%) for combined debridement with suture.
ConclusionsBoth arthroscopic procedures improve the total score significantly on the EVA, ASES, UCLA, and Constant scales. However, a higher proportion of complications was observed in the group that performed suturing. In this regard, we must consider whether it is really necessary to repair all partial tears after the calcified deposits removal.
Aunque el tratamiento conservador de la tendinopatía calcificante tiene una alta tasa de éxito, ocasionalmente es necesario realizar exéresis artroscópica del depósito cálcico. Existe controversia en si el defecto que queda en el manguito rotador puede dejarse in situ o debe repararse para conseguir mejores resultados funcionales. El objetivo de este estudio fue comparar los resultados del desbridamiento frente al desbridamiento combinado con sutura en la cirugía artroscópica de la tendinopatía calcificante.
MetodologíaSe realizó una búsqueda en MEDLINE, EMBASE, Cochrane Library y Web of Science desde el inicio hasta febrero de 2023 de artículos sobre tratamiento artroscópico de tendinopatía calcificante. Se analizaron los resultados funcionales (EVA, ASES, UCLA y Constant), y el número de complicaciones. El tamaño del efecto se calculó mediante el índice d de Cohen.
ResultadosSe incluyeron 21 estudios, incluyendo un total de 1.172 pacientes con edades comprendidas entre 44,7 y 55 años. El tiempo medio de seguimiento fue de 24,7 meses. Las estimaciones del ES combinado para la puntuación total de las escalas EVA, ASES, UCLA y Constant resultaron muy fuertes (>1,0) tanto para el desbridamiento como para el desbridamiento combinado con sutura. Las estimaciones del ES para el número de complicaciones totales fueron de 1,75 (IC del 95%: 0,08-3,43; I2=0%) para el desbridamiento y 9,07 (IC del 95%: −0,03-18,17; I2=50,4%) para el desbridamiento combinado con sutura.
ConclusionesAmbos procedimientos artroscópicos mejoran la puntuación total de forma significativa en las escalas EVA, ASES, UCLA y Constant. Sin embargo, se observó una mayor proporción de complicaciones en el grupo que realizaba sutura. En este sentido debemos plantearnos si es realmente necesario reparar todas las roturas parciales tras la eliminación de los depósitos calcificados.
Calcific tendinopathy (CT) is a common cause of painful shoulder.1 Its incidence varies between 2.7% and 22% and it usually occurs in women aged 30–60 years.2,3 The supraspinatus tendon is the most frequently affected (80%).4 Although the aetiopathogenesis of CT is still unclear,5 the main theories are chronic degeneration, ischaemia, incorrect differentiation of tendon stem cells into bone cells, tendon hypoxia, and hormonal changes.2,4
Conservative treatment is the gold standard, and very good outcomes have been shown in most patients with CT.3,5,6 This treatment includes non-steroidal anti-inflammatory drugs, physiotherapy, subacromial infiltrations, extracorporeal shock wave therapy, ultrasound-guided puncture, or ultrasound-guided needling and lavage (barbotage) of the calcium deposit.3,5,6 However, if conservative treatment fails after 6 months, arthroscopic removal of the calcium deposit is recommended.7,8
Minor or major damage to the rotator cuff tendon may occur after removal of the calcific deposit, depending on the size and shape of the deposit.1 In this regard, the question remains whether the defect remaining in the rotator cuff after debridement and excision of the calcific deposit can be left in situ or should be repaired to achieve better functional results. We hypothesize that additional rotator cuff repair could improve functional outcomes. The main functional and quality of life scales used to assess outcomes after shoulder surgery are: (a) VAS pain scale9 (range, 0–10) [10=worst pain]; (b) ASES (American Shoulder and Elbow Surgeons) scale10 (range, 0–100) [100=best score]; (c) UCLA scale11 (range, 0–35) [35=best shoulder function]; and (d) Constant scale12,13 (range 0–100) [100=least disability].
The aim of this systematic review and meta-analysis is to (a) analyse the functional results after arthroscopic CT surgery, using the VAS, ASES, UCLA, and Constant scales, (b) compare the results of debridement versus debridement combined with suturing in arthroscopic surgery for CT, and (c) establish whether there are differences between the number of complications of both surgical processes.
Following the PICO structure,14,15 a tool used in quantitative systematic reviews to identify the different components of the clinical evidence, the objectives of the present study are as follows: population (patients diagnosed with calcific tendinopathy of the shoulder resistant to conservative treatment and treated surgically), intervention (debridement of calcific deposits plus rotator cuff repair), comparison (isolated debridement of calcific deposits without rotator cuff repair, and outcomes), functional outcomes (VAS, ASES, UCLA and Constant) and number of complications.
Material and methodsThis systematic review and meta-analysis were conducted in accordance with the PRISMA statement16 and guided by the Cochrane Handbook.17 The protocol for this systematic review and meta-analysis was registered beforehand with PROSPERO (registration number: CRD42023395066).
Search strategyThe following electronic databases were systematically searched to identify relevant articles: MEDLINE (via Pub-Med), EMBASE, Cochrane Library, and Web of Science. The search strategy included the following terms: ‘calcifying tendinitis’, ‘calcifying tendinopathy’, ‘calcified tendinitis’, ‘shoulder’, ‘rotator cuff’, ‘VAS’, ‘ASES’, ‘UCLA’, ‘Constant’. The search was conducted until 10 February 2023. The full MEDLINE search strategy is shown as supplementary material (Supplementary Table S1).
EligibilityStudies reporting on the effect of arthroscopic CT surgery involving debridement or debridement combined with suturing, as measured by the VAS, ASES, UCLA, and Constant scales, were included. Inclusion criteria were as follows: (a) patients over 18 years of age; (b) use of arthroscopic surgical techniques performing debridement or debridement with suturing; (c) outcome of scales and questionnaires, including pre- and post-surgery period; (d) outcome measurement using the VAS, ASES, UCLA, and Constant scales, reported as mean and standard deviation (SD); (e) randomised clinical trials, non-randomised experimental studies, and one-way pre–post studies (quasi-experimental study without control group with assessment of outcome variables before and after surgery); and (f) written in English or Spanish. Studies reporting data on shoulder pathologies other than CT or involving patients who had undergone revision surgery of CT were excluded.
Data extraction and risk of bias assessmentThe following data were extracted from each study: (1) author, (2) year of publication, (3) country of study, (4) number of participants by sex (in control and intervention groups), (5) mean age, (6) surgical procedures, (7) VAS, ASES, UCLA, and Constant scale and domains reported, (8) follow-up time (in months), and (9) number of complications. After masking out information on authors, affiliations, date, and source of each manuscript, two investigators (MG-M and DG-M) assessed the risk of bias of the included studies individually; discrepancies were resolved by consensus or by consulting a third investigator (LH-C).
We used the National Heart, Lung and Blood Institute (NIH) quality assessment tool for observational cohort and cross-sectional studies18 to assess the risk of bias of pre–post studies (quasi-experimental studies without control group with assessment of outcome variables before and after surgery). This tool consists of a checklist of twelve items, including selection bias, study design, confounders, blinding, data collection method, withdrawals, dropouts. Each of the criteria in these scales was assessed as: (Y, yes; N, no; NA, not applicable; NR, not reported; ND, not determining). Based on the affirmative responses obtained, the risk of bias of each study is classified as: (affirmative responses 75–100%=low risk of bias; 50–75%=moderate or fair risk of bias; <50%=high risk of bias) (Supplementary Table S2).
Statistical analysisSeparate analyses were performed for the effect of arthroscopic shoulder surgery on CT performing isolated debridement and debridement combined with suturing. Data from the VAS, ASES, UCLA, and Constant scales were used. Preoperative and postoperative values at least 6 months after surgery were considered for the analysis. The effect size (ES) for each outcome was calculated using Cohen's d-index.19 The pooled effect size estimates for the pre–post interventions (debridement and debridement combined with suturing) and their 95% CIs were estimated using a random-effects model based on the method of Der Simonian and Laird,20 where positive effect size values with higher scores are more in favour of the outcomes in the intervention group. Cohen's d values were interpreted as .2 (weak effect), .5 (moderate effect), .8 (strong effect), and >1.0 (very strong effect). This index was also used to compare the effects of the two interventions (debridement versus debridement combined with suturing) on the different scales analysed. Heterogeneity between studies was calculated using the I statistic21 considering values of 0–40%, 30–60%, 50–90%, and 75–100% as unimportant, moderate, important, and considerable, respectively.22 In addition, p-values were considered.
Some considerations should be highlighted: (a) only studies that provided complete data for pre- and post-intervention measurements were considered; (b) only studies that provided data for the scales analysed at least 6 months after the intervention were considered for statistical analysis; (c) if two measurements for the same domain were provided in the same study, they were pooled; (d) data from different cohorts were considered independent samples; and (e) data from the longest follow-up were considered when studies provided data for several follow-up periods.
We also pooled the total number of post-procedural complications for each type of surgery (debridement or debridement combined with suturing). Thus, the pooled estimate and 95% CI were estimated as an aggregate or mean proportion depending on the unit of the outcome analysed.
Sensitivity analyses were performed to quantify the influence of each study on the pooled effect size estimates, removing each study from the pooled estimates one-by-one. In addition, meta-regression analyses were performed to assess the influence of mean age, percentage of women, and follow-up time (in months) on the effect size of arthroscopic CT surgery on the VAS, ASES, UCLA, and Constant scales.
Publication bias was assessed using Egger's regression test.23,24 Statistical analyses were performed using Stata SE software, version 15 (StataCorp, College Station, TX, USA).
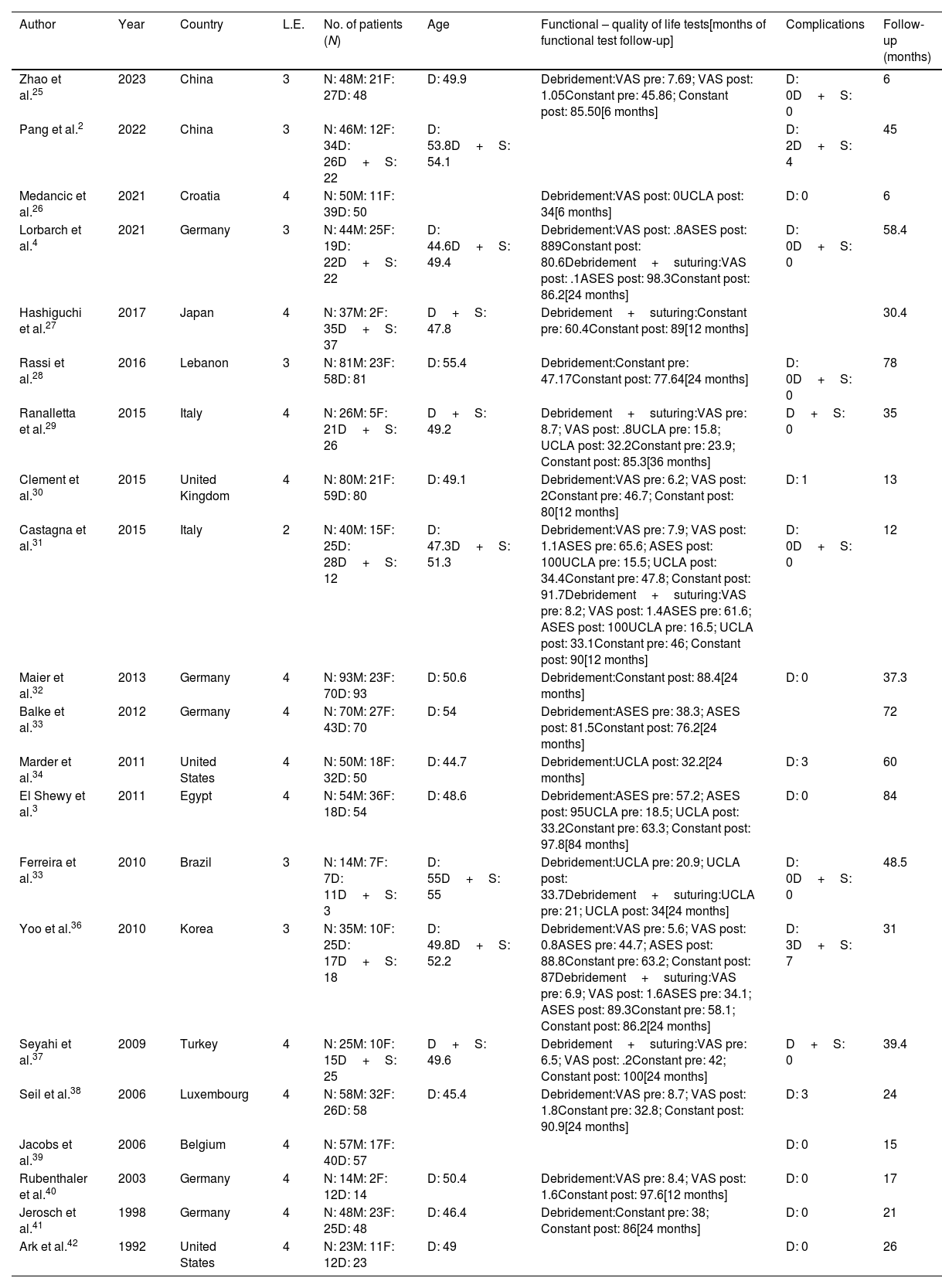
ResultsSystematic reviewThe literature search yielded a total of 1521 studies, of which 21 were included in this systematic review and meta-analysis (Supplementary Fig. S1). The baseline data of the included studies are summarised in Table 1. The studies were published between 1992 and 2023, and all were pre–post studies.2,25–42 The included studies were conducted in 14 countries (Belgium, Brazil, China, Croatia, Egypt, Germany, Italy, Japan, Lebanon, Luxembourg, South Korea, South Korea, Turkey, United Kingdom, and United States), and involved a total of 1172 patients aged between 44.7 and 55 years. The mean follow-up time was 24.7 months, and the median was 18 months.
Characteristics of the study sample.
| Author | Year | Country | L.E. | No. of patients (N) | Age | Functional – quality of life tests[months of functional test follow-up] | Complications | Follow-up (months) |
|---|---|---|---|---|---|---|---|---|
| Zhao et al.25 | 2023 | China | 3 | N: 48M: 21F: 27D: 48 | D: 49.9 | Debridement:VAS pre: 7.69; VAS post: 1.05Constant pre: 45.86; Constant post: 85.50[6 months] | D: 0D+S: 0 | 6 |
| Pang et al.2 | 2022 | China | 3 | N: 46M: 12F: 34D: 26D+S: 22 | D: 53.8D+S: 54.1 | D: 2D+S: 4 | 45 | |
| Medancic et al.26 | 2021 | Croatia | 4 | N: 50M: 11F: 39D: 50 | Debridement:VAS post: 0UCLA post: 34[6 months] | D: 0 | 6 | |
| Lorbarch et al.4 | 2021 | Germany | 3 | N: 44M: 25F: 19D: 22D+S: 22 | D: 44.6D+S: 49.4 | Debridement:VAS post: .8ASES post: 889Constant post: 80.6Debridement+suturing:VAS post: .1ASES post: 98.3Constant post: 86.2[24 months] | D: 0D+S: 0 | 58.4 |
| Hashiguchi et al.27 | 2017 | Japan | 4 | N: 37M: 2F: 35D+S: 37 | D+S: 47.8 | Debridement+suturing:Constant pre: 60.4Constant post: 89[12 months] | 30.4 | |
| Rassi et al.28 | 2016 | Lebanon | 3 | N: 81M: 23F: 58D: 81 | D: 55.4 | Debridement:Constant pre: 47.17Constant post: 77.64[24 months] | D: 0D+S: 0 | 78 |
| Ranalletta et al.29 | 2015 | Italy | 4 | N: 26M: 5F: 21D+S: 26 | D+S: 49.2 | Debridement+suturing:VAS pre: 8.7; VAS post: .8UCLA pre: 15.8; UCLA post: 32.2Constant pre: 23.9; Constant post: 85.3[36 months] | D+S: 0 | 35 |
| Clement et al.30 | 2015 | United Kingdom | 4 | N: 80M: 21F: 59D: 80 | D: 49.1 | Debridement:VAS pre: 6.2; VAS post: 2Constant pre: 46.7; Constant post: 80[12 months] | D: 1 | 13 |
| Castagna et al.31 | 2015 | Italy | 2 | N: 40M: 15F: 25D: 28D+S: 12 | D: 47.3D+S: 51.3 | Debridement:VAS pre: 7.9; VAS post: 1.1ASES pre: 65.6; ASES post: 100UCLA pre: 15.5; UCLA post: 34.4Constant pre: 47.8; Constant post: 91.7Debridement+suturing:VAS pre: 8.2; VAS post: 1.4ASES pre: 61.6; ASES post: 100UCLA pre: 16.5; UCLA post: 33.1Constant pre: 46; Constant post: 90[12 months] | D: 0D+S: 0 | 12 |
| Maier et al.32 | 2013 | Germany | 4 | N: 93M: 23F: 70D: 93 | D: 50.6 | Debridement:Constant post: 88.4[24 months] | D: 0 | 37.3 |
| Balke et al.33 | 2012 | Germany | 4 | N: 70M: 27F: 43D: 70 | D: 54 | Debridement:ASES pre: 38.3; ASES post: 81.5Constant post: 76.2[24 months] | 72 | |
| Marder et al.34 | 2011 | United States | 4 | N: 50M: 18F: 32D: 50 | D: 44.7 | Debridement:UCLA post: 32.2[24 months] | D: 3 | 60 |
| El Shewy et al.3 | 2011 | Egypt | 4 | N: 54M: 36F: 18D: 54 | D: 48.6 | Debridement:ASES pre: 57.2; ASES post: 95UCLA pre: 18.5; UCLA post: 33.2Constant pre: 63.3; Constant post: 97.8[84 months] | D: 0 | 84 |
| Ferreira et al.33 | 2010 | Brazil | 3 | N: 14M: 7F: 7D: 11D+S: 3 | D: 55D+S: 55 | Debridement:UCLA pre: 20.9; UCLA post: 33.7Debridement+suturing:UCLA pre: 21; UCLA post: 34[24 months] | D: 0D+S: 0 | 48.5 |
| Yoo et al.36 | 2010 | Korea | 3 | N: 35M: 10F: 25D: 17D+S: 18 | D: 49.8D+S: 52.2 | Debridement:VAS pre: 5.6; VAS post: 0.8ASES pre: 44.7; ASES post: 88.8Constant pre: 63.2; Constant post: 87Debridement+suturing:VAS pre: 6.9; VAS post: 1.6ASES pre: 34.1; ASES post: 89.3Constant pre: 58.1; Constant post: 86.2[24 months] | D: 3D+S: 7 | 31 |
| Seyahi et al.37 | 2009 | Turkey | 4 | N: 25M: 10F: 15D+S: 25 | D+S: 49.6 | Debridement+suturing:VAS pre: 6.5; VAS post: .2Constant pre: 42; Constant post: 100[24 months] | D+S: 0 | 39.4 |
| Seil et al.38 | 2006 | Luxembourg | 4 | N: 58M: 32F: 26D: 58 | D: 45.4 | Debridement:VAS pre: 8.7; VAS post: 1.8Constant pre: 32.8; Constant post: 90.9[24 months] | D: 3 | 24 |
| Jacobs et al.39 | 2006 | Belgium | 4 | N: 57M: 17F: 40D: 57 | D: 0 | 15 | ||
| Rubenthaler et al.40 | 2003 | Germany | 4 | N: 14M: 2F: 12D: 14 | D: 50.4 | Debridement:VAS pre: 8.4; VAS post: 1.6Constant post: 97.6[12 months] | D: 0 | 17 |
| Jerosch et al.41 | 1998 | Germany | 4 | N: 48M: 23F: 25D: 48 | D: 46.4 | Debridement:Constant pre: 38; Constant post: 86[24 months] | D: 0 | 21 |
| Ark et al.42 | 1992 | United States | 4 | N: 23M: 11F: 12D: 23 | D: 49 | D: 0 | 26 |
D: debridement; D+S: debridement+suturing; F: females; L.E.: level of evidence; M: males; pre: preoperative; post: postoperative.
According to the quality assessment tool for observational cohort and cross-sectional studies,18 all pre–post studies included in the meta-analysis were considered to be at fair or moderate risk of bias. When assessing the individual domains of this tool, all studies included information regarding the representativeness of the sample and the description of the intervention. However, all the studies were limited in terms of sample eligibility and blinding (Supplementary Table S2).
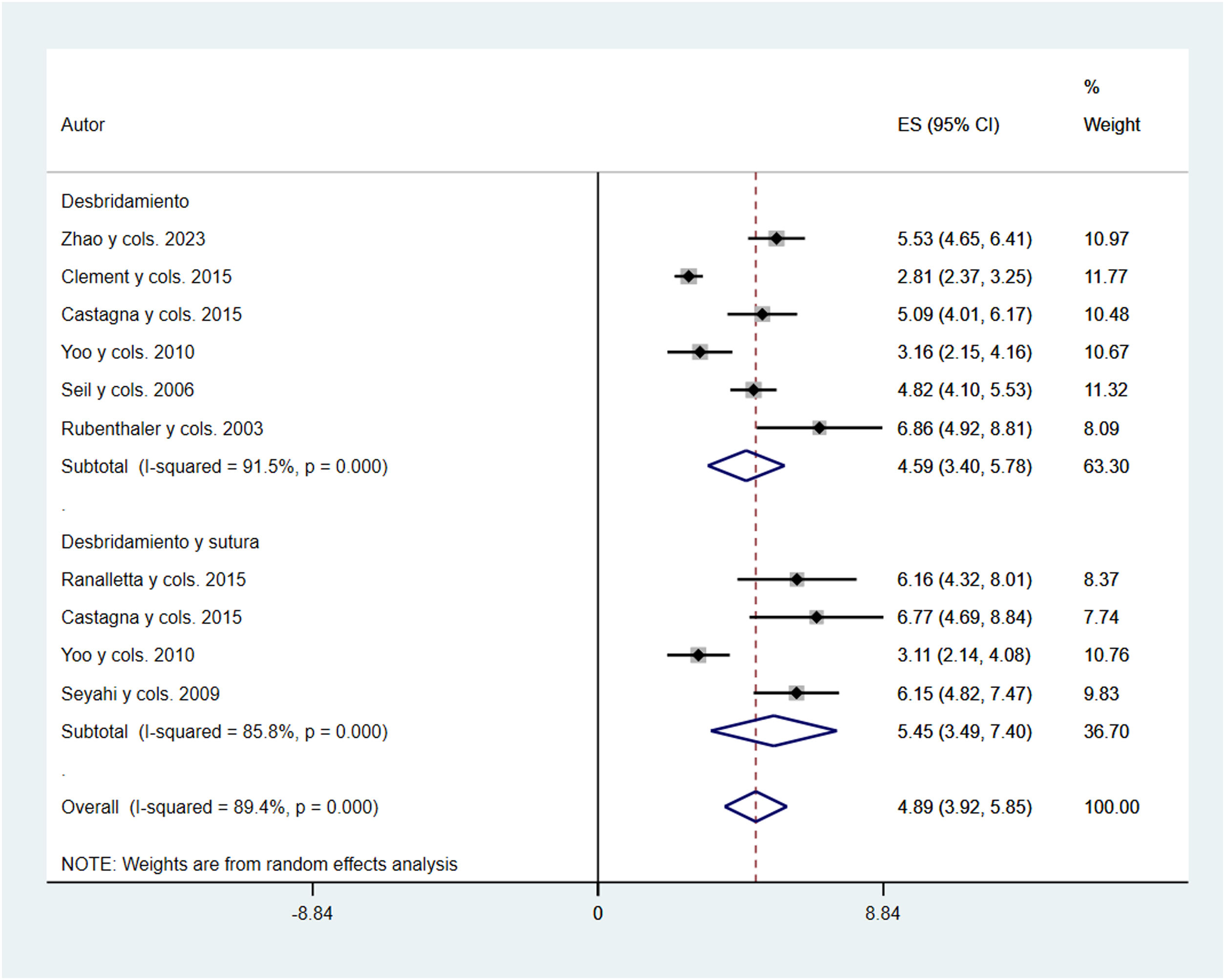
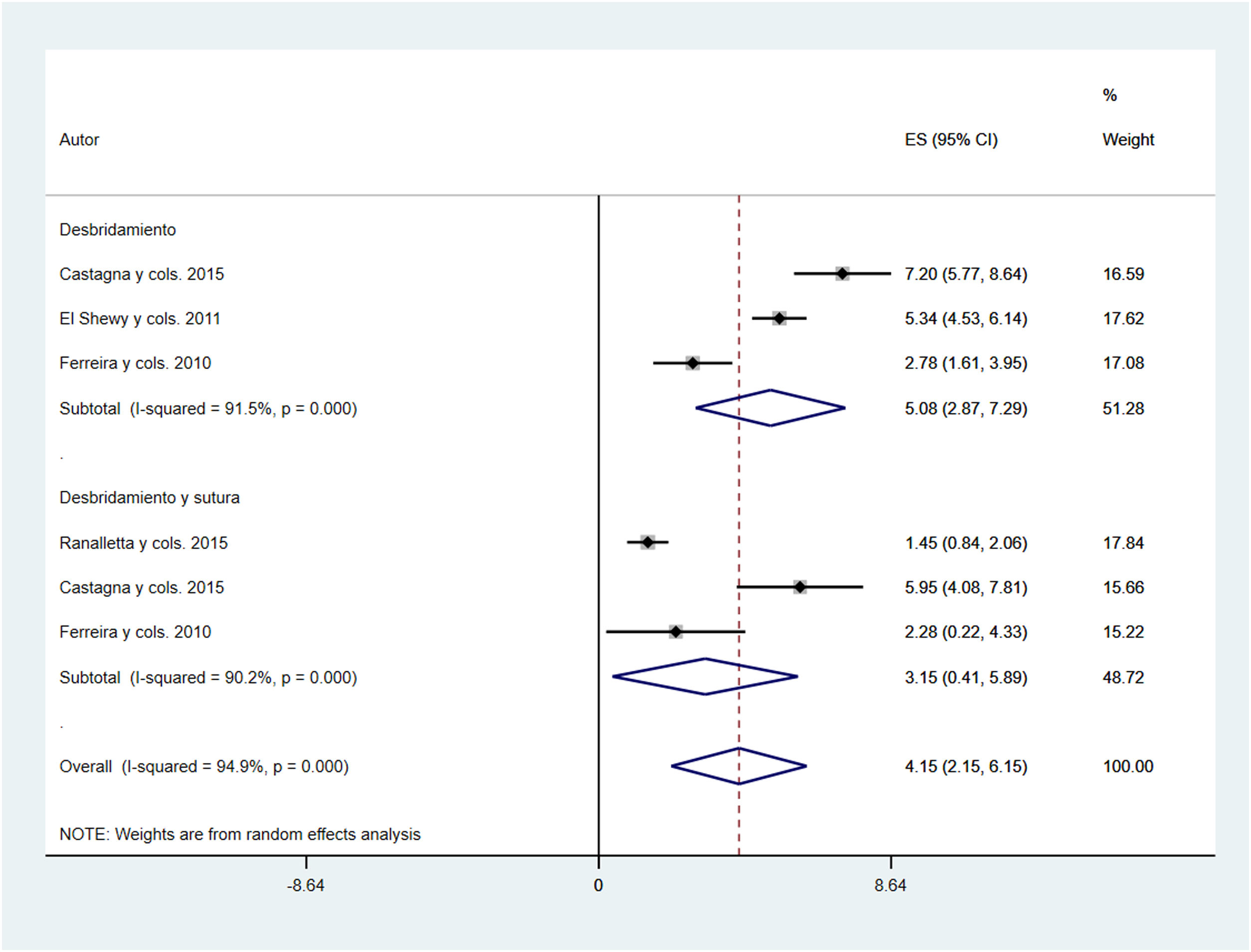
Meta-analysisThe pooled effect size estimates for total VAS scale scores were 4.59 (95% CI: 3.40–5.78; I2=91.5%) for debridement and 5.45 (95% CI: 3.49–7.40; I2=89.2%) for debridement combined with suturing. The total effect size estimate was 4.89 (95% CI: 3.92–5.85; I2=90%) (Fig. 1). The pooled effect size estimates for total ASES scale scores, were 2.28 (95% CI: 1.41–3.14; I2=88.7%) for debridement and 3.56 (95% CI: 2.78–4.34; I2=0%) for debridement combined with suturing. The total effect size estimate was 2.70 (95% CI: 1.93–3.48; I2=85.6%) (Fig. 2).
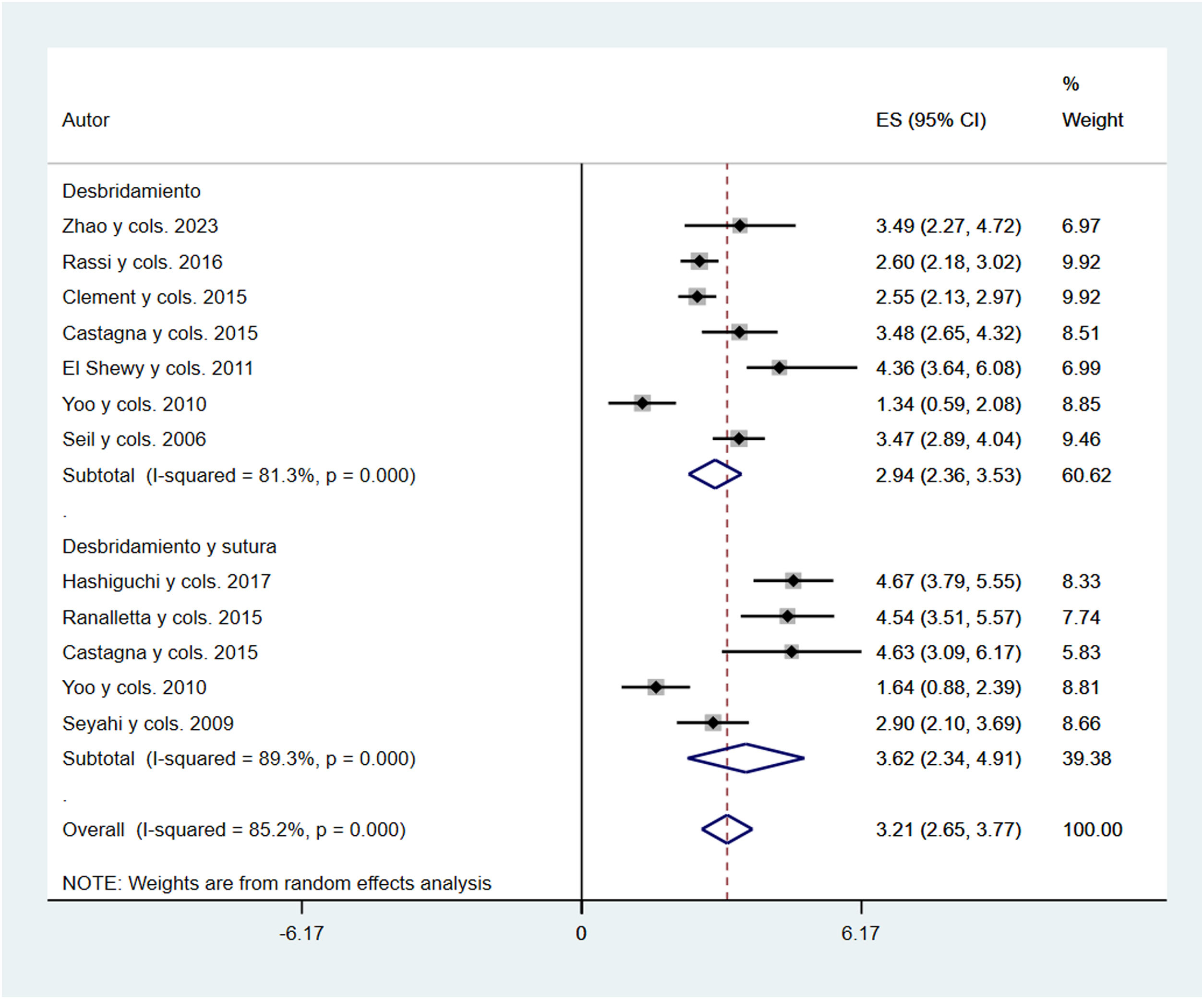
The pooled effect size estimates for total UCLA scores were 5.08 (95% CI: 2.87–7.29; I2=91.5%) for debridement and 3.15 (95% CI: .41–5.89; I2=90.2%) for debridement combined with suturing. The total effect size estimate was 4.15 (95% CI: 2.15–6.51; I2=83.7%) (Fig. 3). The pooled effect size estimates for the total Constant scale scores were 2.94 (95% CI: 2.36–3.53; I2=83.7%) for debridement and 3.62 (95% CI: 2.34–4.91; I2=89.3%) for debridement combined with suturing. The total effect size estimate was 3.19 (95% CI: 2.60–3.78; I2=86.4%) (Fig. 4).
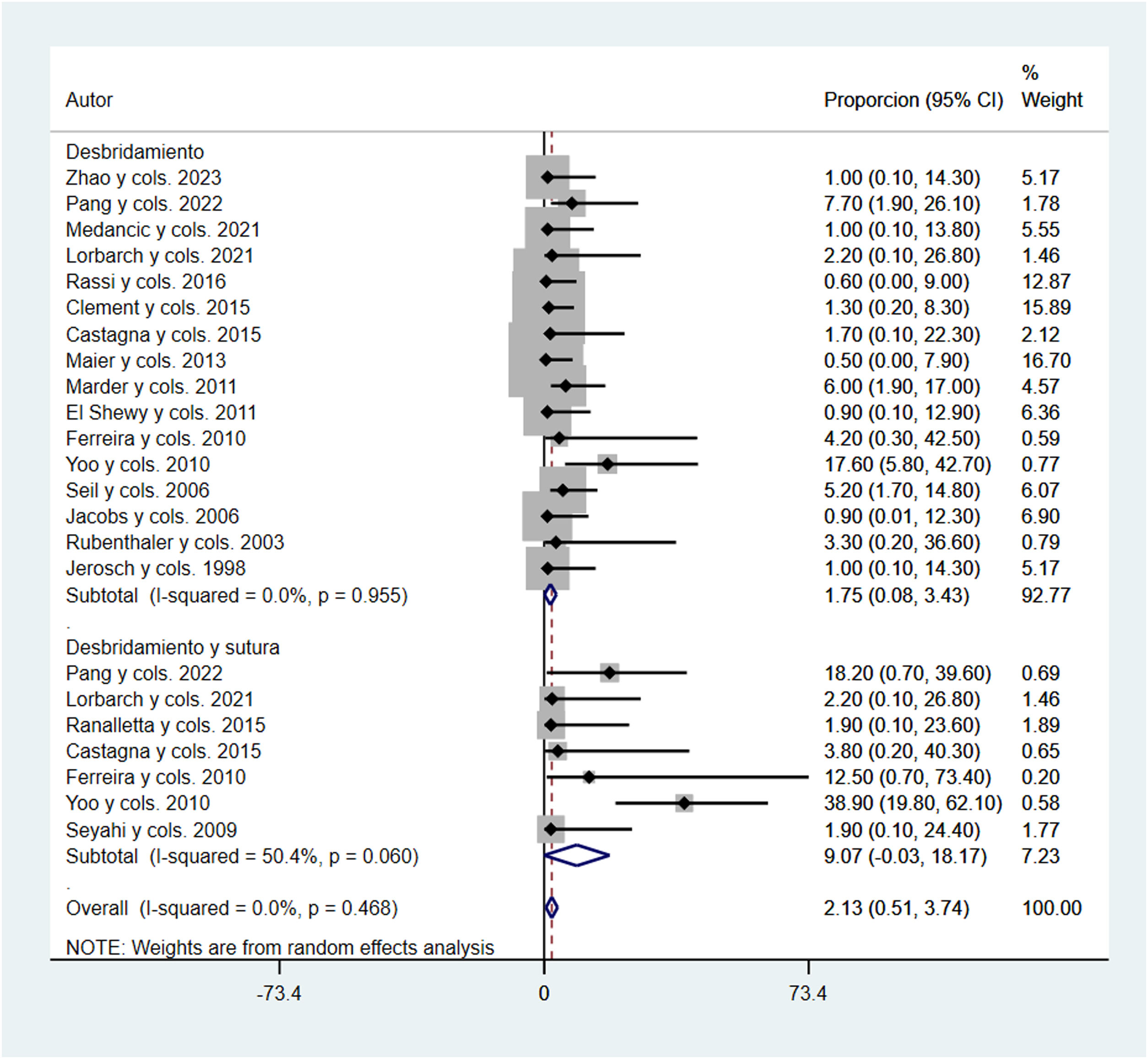
Finally, the pooled effect size estimates for the number of total complications were 1.75% (95% CI: .08–3.43; I2=0%) for debridement and 9.07% (95% CI: −.03 to 18.17; I2=50.4%) for debridement combined with suturing. The total effect size estimate was 2.13 (95% CI: .51–3.74; I2=0%) (Fig. 5). The only complication described in the papers that collected the number of complications was postoperative stiffness.
Sensitivity and meta-regression analysisNo individual study (with the exception of the Castagna et al. study31 for the UCLA dimension, debridement and suturing) modified the pooled estimate of effect size when examining the effect of the studies individually, removing studies from the analysis one-by-one (Supplementary Table S3).
In addition, the meta-regression analyses showed that the percentage of women and mean age influenced the association between both types of surgeries and the scales assessed (VAS, ASES, Constant, and UCLA) (Supplementary Table S4).
Publication biasEvidence of publication bias was identified using Egger's test,23,24 for the effect of debridement surgery on VAS score (p<.001) (Supplementary Table S5).
DiscussionThis systematic review and meta-analysis aimed to compare the outcomes of debridement versus debridement combined with suturing in arthroscopic CT surgery in terms of functional outcomes using the VAS, ASES, UCLA, and Constant scales. Our indices showed that both surgical techniques (debridement and debridement combined with suturing), improved the scores of the scales analysed. However, a higher proportion of complications was found in the combined debridement and suturing group.
Lorbarch et al.4 recently concluded that additional repair after debridement of the calcific deposit resulted in better clinical and structural outcomes. However, in the present study we see that both techniques, when conservative options have been exhausted for a period of at least 6 months, produce very favourable outcomes. We found no differences between the two techniques in the four functional scales studied, but we did find a significant increase in postoperative stiffness in the suture group. Therefore, although the level of evidence in this meta-analysis is limited, we must ask ourselves whether it is really necessary to repair all partial tears after removing the calcific deposits or whether this additional procedure is not necessary.
Although several studies have previously demonstrated good to excellent clinical outcomes after arthroscopic treatment of CT of the shoulder,32,33,38,43 this is the first systematic review to analyse the functional outcomes of arthroscopic surgery in CT of the shoulder. Although the functional outcomes vary between patients,44,45 many of them return to the same sporting activity as before the injury.46
CT does not appear to predispose to additional partial rotator cuff tears, as these two entities have a different aetiopathogenesis.4 However, Balke et al.,33 in their study where they do not perform rotator cuff sutures, conclude that the rate of partial supraspinatus tendon tears appears to be higher after calcium removal. However, with the present study, we can see that the functional and quality of life results, at least in the midterm, are very acceptable with both techniques.
Some authors favour partial removal of the calcium deposit to reduce potential tendon damage during surgery,3,47 and also report good clinical outcomes. Others prefer complete removal of the deposit,36,41,48 as some studies showed better results after complete excision.5 In addition, several authors have established a relationship between leaving calcific deposit remains and a higher rate of revision surgery,4,42 persistence of pain, and worse scores on the Constant scale.48
On the other hand, Balke et al.33 conclude that subacromial decompression appears to reduce postoperative pain; however, Marder et al.34 take a different view, since those patients in whom they combined subacromial decompression after debridement of the calcific deposit needed more time to return to normal activity without restrictions and without pain. In the present study we did not analyse the impact of combining a subacromial decompression, since we wanted to focus on the impact of suturing or not suturing the defect after removal of the calcific deposit, but it might be interesting to analyse this factor in a future study.
The topic we cover in this paper is very difficult to protocolise in a generic way, as the intraoperative decision depends on many factors. During arthroscopic surgery, Porcellini et al.48 perform isolated debridement on small partial tears and suture partial tears larger than 1cm and complete tears by side-to-side suturing or suture anchors. Yoo et al.36 in their surgical protocol suture large defects (>1.5cm) with anchors and minor defects with side-to-side suturing. However, the latter report an increase in postoperative stiffness in patients who are sutured.
LimitationsFirstly, the study had the limitations common to systematic reviews and meta-analyses, such as selection bias and limited availability of complete information from study reports. Secondly, significant publication bias was detected using Egger's test for the effect of debridement surgery on VAS score. Thirdly, most of the included studies were non-randomised, retrospective studies or case series, and all of them scored moderate in the risk of bias assessment. Therefore, the results of this work should be read with caution and future prospective, randomised studies are needed to increase the level of evidence. Fourth, there was considerable heterogeneity in the included studies, possibly due to methodological diversity in design, outcomes, and measurement tools. Fifth, numerous factors may have influenced both clinical and patient-related outcomes, such as type of intervention, associated procedures, surgeons’ skills, and comorbidities. It was not possible to include these factors in the analyses due to lack of information in the included studies. Postoperative functional tests in most studies were performed at 24 months follow-up, however, the range was 6–84 months between the different studies. In the present study, acromioplasty was not included as an added factor in the functional outcomes, but it was found that the distribution of patients who underwent acromioplasty was homogeneously distributed between groups and therefore did not act as a possible bias. Finally, we cannot rule out a selection bias due to the inclusion of studies written only in English and Spanish.
ConclusionsOur data show that good to excellent outcomes can be achieved after arthroscopic treatment of CT, regardless of whether or not tendon repair is performed after arthroscopic debridement. Both arthroscopic procedures improve the overall score significantly on the VAS, ASES, UCLA, and Constant scales. However, we observed a higher proportion of complications when suturing is performed, and therefore we should consider whether it is really necessary to repair all partial ruptures after removal of calcific deposits.
Level of evidenceLevel of evidence III.
FundingNo funding was received for this manuscript.
Conflict of interestsThe authors have no conflict of interests to declare.
The first author would like to thank Clara, Inés, and Nicolás for all their help with this and much other work.
This article is eligible for the “SECOT Foundation prize for the best systematic review or meta-analysis article”.