Synthesis with cannulated screws is one of the accepted methods in femoral neck fractures, although its optimal configuration is a subject in continuous debate. The main objective was to compare the results of the patient with a femoral neck fracture fixed with three screws in triangle and inverted triangle configuration in the frontal plane.
Materials and methodsRetrospective and comparative study of 53 patients with femoral neck fracture, operated between 2015 and 2022 with fixation with three cannulated screws, 22 with a triangle configuration (triangle group) and 31 in an inverted triangle (inverted triangle group). Functionality was evaluated using the modified Merlé d’Aubigné scale, walking ability using the Koval scale, as well as postoperative complications.
ResultsOn the Merlé d’Aubigné scale, the mean score was 16.7 in the triangle group and 16.1 in the inverted triangle group (p=.259). On the Koval scale, a significant decrease was observed, going from 1.6 preoperative mean to 2.2 after surgery (p=.000), finding no differences between groups. There were six postoperative complications in the triangle group and three in the inverted triangle group (p=.140).
ConclusionThe configuration of the screws in the femoral neck, both in the form of a triangle and an inverted triangle, did not influence the functional or mechanical outcomes of the patients with a femoral neck fracture fixed with three cannulated screws.
La síntesis con tornillos canulados es uno de los métodos aceptados en las fracturas de cuello femoral, aunque su óptima disposición es un tema en continuo debate. El objetivo principal fue comparar los resultados del paciente con fractura de cuello de fémur fijada con 3 tornillos en configuración triangular y en triángulo invertido en el plano frontal.
Materiales y métodosEstudio retrospectivo y comparativo de 53 pacientes con fractura de cuello femoral intervenidos entre los años 2015 y 2022 mediante fijación con 3 tornillos canulados: 22 conformados en triángulo (grupo triángulo) y 31 en triángulo invertido (grupo triángulo invertido). Se evaluó la funcionalidad mediante la escala modificada de Merlé d’Aubigné, la capacidad para la deambulación con la escala de Koval, así como las complicaciones postoperatorias.
ResultadosEn la escala de Merlé d’Aubigné la puntuación media fue de 16,7 en el grupo triángulo y de 16,1 en el grupo triángulo invertido (p=0,259). En la escala de Koval se observó una disminución significativa, pasando de 1,6 de media preoperatoria a 2,2 tras la cirugía (p=0,000), no hallando diferencias entre grupos. Hubo 6 complicaciones postoperatorias en el grupo triángulo y 3 en el grupo triángulo invertido (p=0,140).
ConclusiónLa configuración de los tornillos en el cuello femoral, tanto en forma de triángulo como en triángulo invertido, no influyó en los resultados funcionales ni mecánicos de los pacientes con fractura de cuello de fémur fijada mediante 3 tornillos canulados.
Fractures of the femoral neck are relatively common, constituting almost 50% of all hip fractures. Its surgical treatment will vary depending mainly on the fracture pattern and the age of the patient, considering synthesis with screws a valid method in young patients1 and in non-displaced patients,2 even in older patients.3
The purpose is to stabilise the fracture and protect the vascularisation of the femoral head using parallel screws, although their number and arrangement in the femoral neck is a topic of continuous debate. Most authors defend the use of three screws,4–6 with greater disparity regarding their optimal configuration. While some studies showed that the inverted triangle configuration could achieve greater stability,7,8 others found better results with the triangle arrangement,5,6 the majority being biomechanical research.
The main objective of this study was to analyse the functional results and mechanical complications of patients with femoral neck fracture synthesised with three screws, comparing the results according to the arrangement of the screws in the anteroposterior (AP) plane in triangle or in inverted triangle. The hypothesis was that the configuration of the screws in the femoral neck would not influence the results.
Material and methodA retrospective study was designed and approved by our institutional ethics committee, without requiring informed consent as it was considered an evaluation of clinical practice. Patients with femoral neck fractures treated surgically with screws between January 2015 and January 2022 were identified from the service's database. The inclusion criteria were aged 50 years or over, acute femoral neck fracture synthesised with three cannulated screws, surgery within 48h after hospital admission, good reduction quality according to Baumgaertner,9 and with a minimum postoperative follow-up of 12 months. Exclusion criteria were considered cases with linear configuration of the screws in the AP plane, pathological fracture, deep or implant infection defined by infrafascial infection that required surgical revision, the need for open reduction of the fracture and the patient with severe cognitive dysfunction. During the initial evaluation of the patients, in a standardised manner, cognitive status was assessed using the Pfeiffer questionnaire (Short Portable Mental Status Questionnaire).10 Patients with severe cognitive dysfunction (8–10 errors out of the 10 questions asked) were excluded from the study due to the difficulty in complying with the postoperative discharge indicated in these cases.
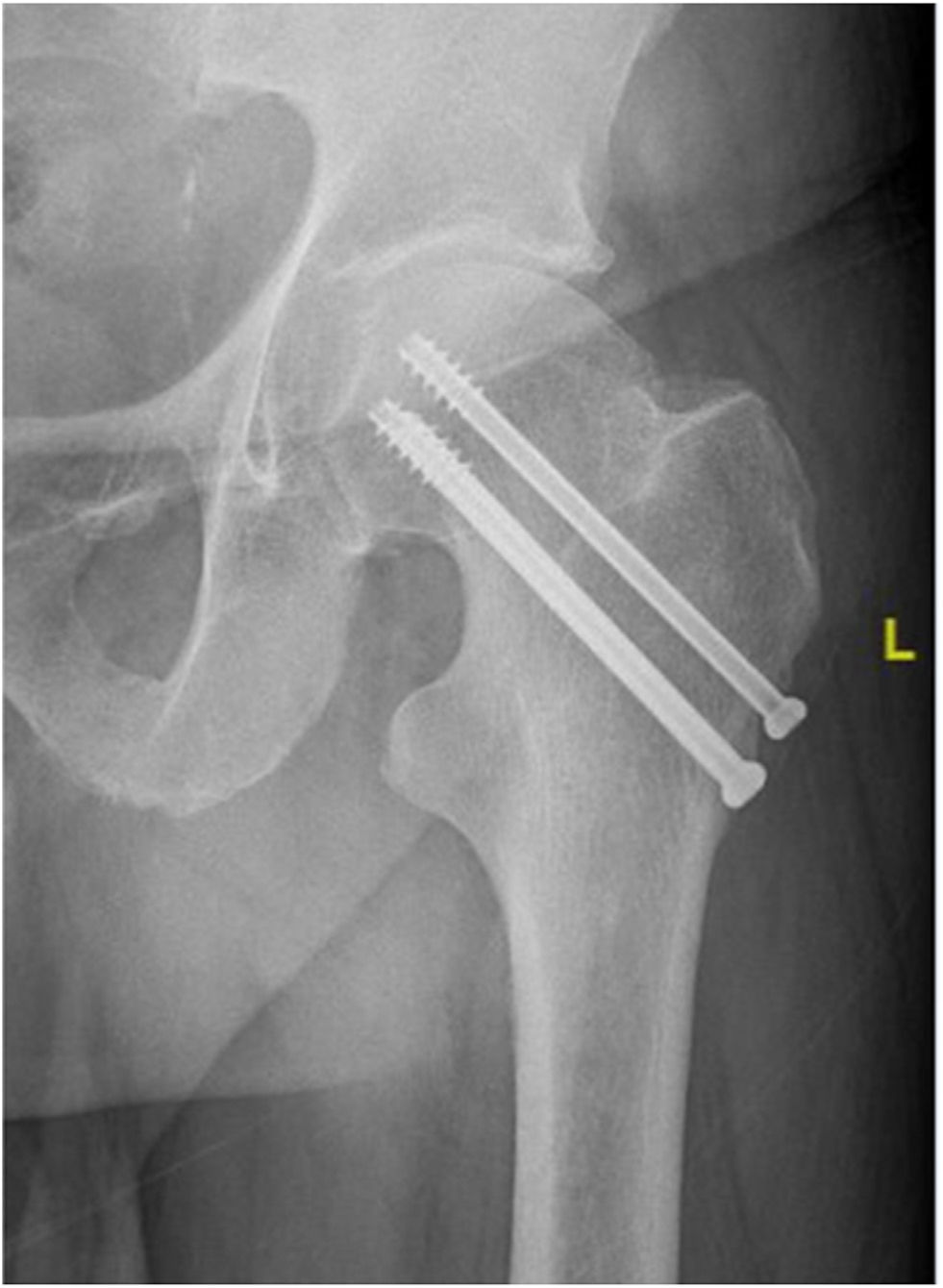
The results were compared according to the arrangement of the screws in the femoral neck in the AP radiological projection, distributing the series into two groups: cases with two inferior and one superior screws formed the triangle group (Fig. 1), while those with one lower and two superior screws constituted the inverted triangle group (Fig. 2).
Fifty-three patients – 35 women (66%) and 18 men (34%) – met the inclusion and exclusion criteria: 22 in the triangle group and 31 in the inverted triangle group, with a mean age of 69.8 years (SD: 15.5).
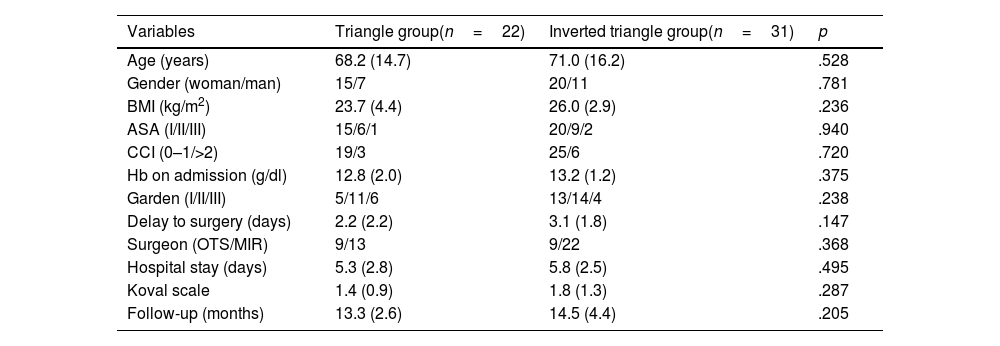
Table 1 contains the baseline characteristics of both groups.
Baseline characteristics of the study groups.
| Variables | Triangle group(n=22) | Inverted triangle group(n=31) | p |
|---|---|---|---|
| Age (years) | 68.2 (14.7) | 71.0 (16.2) | .528 |
| Gender (woman/man) | 15/7 | 20/11 | .781 |
| BMI (kg/m2) | 23.7 (4.4) | 26.0 (2.9) | .236 |
| ASA (I/II/III) | 15/6/1 | 20/9/2 | .940 |
| CCI (0–1/>2) | 19/3 | 25/6 | .720 |
| Hb on admission (g/dl) | 12.8 (2.0) | 13.2 (1.2) | .375 |
| Garden (I/II/III) | 5/11/6 | 13/14/4 | .238 |
| Delay to surgery (days) | 2.2 (2.2) | 3.1 (1.8) | .147 |
| Surgeon (OTS/MIR) | 9/13 | 9/22 | .368 |
| Hospital stay (days) | 5.3 (2.8) | 5.8 (2.5) | .495 |
| Koval scale | 1.4 (0.9) | 1.8 (1.3) | .287 |
| Follow-up (months) | 13.3 (2.6) | 14.5 (4.4) | .205 |
ASA: American Society of Anaesthesiologists; BMI: body mass index; CCI: Charlson comorbidity index; Hb: haemoglobin; MIR: hospital resident doctor; OTS: specialist in orthopaedic surgery and traumatology.
Continuous variables offered as mean (standard deviation).
In our service, non-displaced intracapsular fractures (Garden II) and minimally displaced ones (Garden I and III), in young patients with good bone quality, are treated by fixation with three parallel cannulated screws, while in the older patient only when the fracture is impacted in valgus.
All patients underwent surgery under spinal anaesthesia on an orthopaedic traction table, using a mini-approach on the lateral aspect of the thigh and intraoperative radioscopic control. The screws used were 6.5mm titanium and with a distal thread. In the frontal plane, the arrangement of the screws in the femoral neck was decided intraoperatively, according to the surgeon's preference, while in the axial projection, on the contrary, the same protocol was always followed, constantly positioning two screws in the posterior area, and the third, more anterior. In a standardised manner, in all cases unloading was prescribed for 4 weeks, starting specific physiotherapy of the operated hip in the immediate postoperative period, allowing progressive loading of the lower limb from the fifth postoperative week.
AssessmentsThe clinical data of all patients with hip fractures operated on in our service are collected prospectively in a standardised manner in a specific registry, with postoperative follow-up at 1, 3, 6 and 12 months.
The patient's function was evaluated using the modified Merlé d’Aubigné,11 as well as dependence for ambulation according to the Koval scale.12 In the latter, the state prior to the fracture was also determined. The modified Merlé d’Aubigné scale presents items that simply describe the function of the hip by evaluating pain, mobility and stability in walking, demonstrating its high reliability and reproducibility in previous studies.11 The Koval scale12 classifies walking dependence into seven grades: independent (grade 1), community ambulation with cane (grade 2), or walker/crutches (grade 3), independent home ambulation (grade 4), with a cane (grade 5), or with a walker/crutches (grade 6), and non-functional ambulation (grade 7). Community ambulation refers to a person who can walk indoors or outdoors, either independently or with assistive devices. Home ambulation is restricted to walking indoors, either independently or with assistive devices. Non-functional ambulation refers to a person who is bedridden or needs help moving from a bed to a chair. For the statistical analysis, on the modified Merlé d’Aubigné scale, excellent and good results were considered satisfactory, while average and poor were considered unsatisfactory. In the Koval scale, each grade was transformed into a numerical variable (score) for subsequent statistical analysis (for example, grade 7 would be equivalent to 7 points, and grade 1, to 1 point), considering dependent wandering as the need any external help to walk.
The radiological evaluation was carried out with the AP and axial radiological projections of the hip on admission, immediately after surgery and in subsequent follow-ups, analysing the quality of reduction according to the Baumgaertner criteria,9 the type of fracture according to the Garden classification, the configuration of the screws in the AP plane and the measurement of the postoperative cervico-diaphyseal angle in the AP view. Digital computer software was used (Centricity Universal Viewer ZeroFootprint®, GE Healthcare, USA), with a precision for angular measurements of 0.1°.
Complications that could appear after surgery were also recorded, both biological (pseudarthrosis, bone necrosis) and mechanical (fracture collapse, screw migration), as well as the need for secondary surgery. For their diagnosis, complementary tests (CT, MRI) were used when necessary. The assessment of shortening of the femoral neck (fracture collapse) was established by comparative measurement of the distances in the AP projection of the postoperative radiological control and during follow-up, determining as a reference the distance from the centre of the femoral head to the cortical bone, lateral of the proximal femur, following the central axis of the femoral neck. Fracture collapse was established as a difference greater than 1cm compared to the radiographs of the first postoperative day.
For data analysis, postoperative outcomes at 12-month follow-up were considered.
Statistical analysisStatistical analysis was performed with SPSS software, v.25 (SPSS Inc., Chicago, USA). Normal distribution was evaluated with the Kolmogorov–-Smirnov test. To determine the association between qualitative variables, the chi-square and Fisher's exact tests were used. Student's t tests and non-parametric Mann–Whitney U tests were used to compare means. To determine the degree of correlation between quantitative variables, Pearson's correlation coefficient and Spearman's non-parametric correlation were used. A multivariate analysis was performed to identify predictors of functional outcome and postoperative mechanical complications, presented as odds ratio (OR) with its 95% confidence interval (CI). To evaluate the goodness of fit, the Hosmer–Lemeshow test was used, where a value of p>.05 indicated a good fit of the logistic regression model.
In all analyses, statistical significance was considered for values of p<.05.
ResultsAll patients had a mean follow-up of 14.0 months (SD: 3.8; range: 12–24).
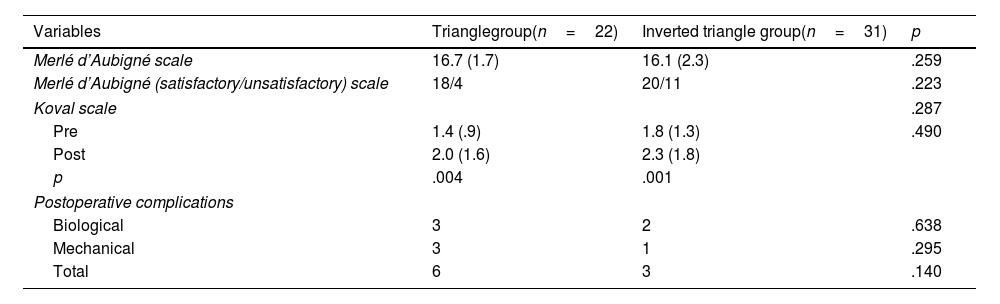
In the functional assessment, according to the modified Merlé d’Aubigné scale, the mean score was 16.7 (SD: 1.7) in the triangle group and 16.1 (SD: 2.3) in the inverted triangle group (p=.259). Categorising the results, there were no differences between both groups (Table 2). Age over 75 years (p=.012), a Charlson comorbidity index 2 (p=.047), surgery performed by a resident internal physician (p=.007), a preoperative dependent walking (p=.000) and longer surgical delay (p=.011) were significantly associated with an unsatisfactory functional outcome. Overall, a moderate correlation of the final score with age was observed (r=−.585; p=.000). In the logistic regression model, the only predictive factor of satisfactory functional outcome after surgery was the ability to perform independent walking before the hip fracture (OR: 33.0; 95% CI: 3.3–324.0; p=.003), with a value of p=.466 in the Hosmer–Lemeshow test.
Functional assessments and complications.
| Variables | Trianglegroup(n=22) | Inverted triangle group(n=31) | p |
|---|---|---|---|
| Merlé d’Aubigné scale | 16.7 (1.7) | 16.1 (2.3) | .259 |
| Merlé d’Aubigné (satisfactory/unsatisfactory) scale | 18/4 | 20/11 | .223 |
| Koval scale | .287 | ||
| Pre | 1.4 (.9) | 1.8 (1.3) | .490 |
| Post | 2.0 (1.6) | 2.3 (1.8) | |
| p | .004 | .001 | |
| Postoperative complications | |||
| Biological | 3 | 2 | .638 |
| Mechanical | 3 | 1 | .295 |
| Total | 6 | 3 | .140 |
Post: postoperative; Pre: preoperative.
Continuous variables offered as mean (standard deviation).
In the evaluation of the displacement capacity, according to the Koval scale, a significant decrease was observed globally at one year compared to the state prior to the fracture, going from 1.6 on average (SD: 1.1) to 2.2 (SD: 1.7) (p=.000), without significant differences between groups (Table 2). In the last postoperative follow-up, in grade 1 of the scale (independent walking) there were 14 patients in the triangle group (63.6%) and 18 in the inverted triangle group (58.1%) (p=.683). Age greater than 75 years (p=.000), preoperative dependent walking (p=.000), and longer surgical delay (p=.000) were significantly associated with dependent walking. Overall, there was a good correlation of the level of ambulation one year after surgery on the Koval scale with age (r=.671; p=.000). In the logistic regression model, the only risk factor for a level of dependent ambulation after surgery was age over 75 years (OR: 6.8; 95% CI: 1.7–26.8; p=.006), with a value of p=.861 in the Hosmer–Lemeshow test.
Regarding the presence of complications after surgery, there were six cases in the triangle group (27.2%) and three in the inverted triangle group (9.6%) (p=.140). Regarding biological complications, in the triangle group there were two cases of nonunion and one femoral head necrosis, while in the other group there were two bone necrosis (p=.638). In relation to mechanical complications, in the triangle group there were three fracture collapses with lateral migration of the cannulated screws, and only one in the inverted triangle group (p=.295). All required secondary surgery. In patients with nonunion and bone necrosis, the screws were removed and a cementless total hip prosthesis was implanted, an average of 7.5 months from the primary surgery. Cases with lateral migration of a screw required its removal after consolidation of the fracture. In the multivariate analysis, screw configuration was not a risk factor for the presence of postoperative complications (OR: 4.0; 95% CI: .8–19.7; p=.085).
Radiologically, the cervico-diaphyseal angle was 139.2° (SD: 6.0) in the triangle group and 135. 8° (SD: 8.0) in the inverted triangle group (p=.112). Overall, it did not influence either the functional outcome (p=.236) or the level of ambulation (p=.286).
DiscussionThe main finding of the present study was that in the treatment of femoral neck fracture, the triangle or inverted triangle configuration of the screws did not influence the functional outcome or the level of ambulation one year after surgery. There were also no significant differences regarding postoperative mechanical complications, although the result could be clinically relevant.
The functional worsening of patients after hip fracture surgery13,14 is a widely contrasted fact in the literature, despite achieving a good reduction of the fracture.15 The age of the patient, the previous functional status and the quality of the fracture reduction have been reported as risk factors for the unsatisfactory result of internal fixation in femoral neck fracture.16–18 In this study, age was also a predictive factor for the final functional outcome. Cases with incomplete reduction of the fracture, being a clearly established risk factor, were excluded in order to homogenise the study sample and avoid confounding factors in the analysis of results.
Several biomechanical studies have analysed the different configurations of the screws used in the fixation of intracapsular hip fracture.5,7,19,20 Selvan et al.7 studied six different types of configurations in synthetic bone models divided into two groups: triangular configurations, with two parallel screws and a third screw placed on the top, bottom, anterior or posterior part, and linear configurations with two or three screws in a vertical line, finding that the triangular configurations had greater resistance, with the proximal apex having greater resistance compared to the inverted triangle. Others6,19,21 have studied the mechanical conditions of different configurations using finite element analysis, with disparities in results. Coinciding with the findings of Selvan et al.,7 Li et al.21 also found more mechanical advantages with the triangle arrangement, while Zhang et al.6 observed that the standard triangular configuration with a certain obliquity obtained superior performance than the inverted triangle. In contrast, Mei et al.19 found that the optimal configuration was the inverted triangle, and this formation was also defended by Oakley et al.22 due to the lower risk of subtrochanteric fracture, arguing that perforations in the lateral cortex for the placement of the two distal screws can double the risk of fracture. The present study did not detect any subtrochanteric fractures during postoperative follow-up.
Clinical studies also offer mixed results. Jordan et al.17 found no consistent evidence that screw configuration was a significant predictor of outcome, although Yang et al.8 found triangular screw fixation, a displaced fracture, and poor reduction as risk factors of pseudarthrosis. Recently, Zhu et al.23 found that fixation with four screws in a rhombic configuration was superior to the inverted triangle configuration with respect to postoperative pain, union time, and complication rate. In contrast, Guo et al.24 published that fixation with four screws did not improve clinical results or reduce complications in patients with femoral neck fractures.
The overall rate of postoperative complications in the present study was 15%, in line with other publications,3,23,25 finding no significant differences between groups, although the complication rate in the triangle group seems clinically relevant (27.2% vs 9.6%). Toh et al.26 found that the development of bone necrosis or nonunion was not related to fracture displacement, the number of screws used, osteoporosis, screw parallelism, or surgeon experience. Gurusamy et al.20 found no association between the positioning of the screws and their angulation in the frontal plane with the presence of nonunion. On the contrary, Yang et al.8 did observe that the triangular configuration was significantly associated with a greater risk of nonunion, presenting an odds ratio of 2.92 compared to the inverted triangle configuration.
There are some limitations in the present study. The retrospective design of the study presents an inherent limitation in the collection and accuracy of the data, although the data were collected prospectively based on a standardised protocol. The series is small, which may lead to an underestimation of the true complication rate. The configurations in all patients in both groups (triangle or inverted triangle) were not identical and the surgical procedures were performed by several surgeons, although there were no significant differences between groups when evaluating whether the surgery was performed by a specialist physician or by a resident internal physician with extensive training in these techniques. We consider that the surgical technique is one of the most important factors, and should not underestimate a supposedly simpler technique when compared to total hip arthroplasty.
ConclusionsThe configuration of the screws in the femoral neck, either triangular or inverted triangle, did not influence the functional or mechanical results or the level of ambulation of patients with femoral neck fractures fixed with cannulated screws. Age was the only significant predictor of unsatisfactory postoperative clinical outcome, both in the functional evaluation scale and in the level of ambulation after surgery.
Level of evidenceLevel of evidence III.
Ethical approvalThe study was approved by the institutional ethics committee (Ref. PI2022-094).
FundingThis research did not receive specific support from public sector agencies, the commercial sector or non-profit entities.
Conflict of interestsThe authors have no conflict of interests to declare.