Posterior MIPO approach in the humerus has been described by using a 4.5mm LCP plate. Although straight plates have shown good results, they have not been designed to adapt to the distal humeral metaphysis. The goal of the study was to test the null hypothesis that there is no difference in hardware removal after posterior MIPO with either a straight or a pre-contoured plate.
MethodsPatients older than 18 years, who had suffered mid-distal humeral shaft fracture, were treated by a posterior MIPO technique with a locking plate and had a minimum of 12-month follow-up were retrospectively included. Patients were separated into: group 1 (LCP 4.5mm straight plate); and group 2 (3.5mm anatomically shaped plate). Clinical and radiological evaluations were performed in the postoperative period. Patient-reported outcomes and the need of hardware removal because of pain were assessed.
ResultsSixty-seven patients fulfilled the inclusion criteria. Twenty-seven patients in group 1 and 40 in group 2. No patient was lost to follow-up. There were no statistical differences between in patient reported outcomes measures. All the fractures healed. Within group 1, 18% (95%CI: 6–38%) of the patients required implant removal while in group 2 this incidence was 0% (95%CI: 0–9%) (P 0.009).
ConclusionThese results suggest that the use of a 4.5mm LCP compared to an anatomical 3.5mm LCP in posterior MIPO of the humerus generates greater discomfort and therefore leads to a 18% increase in the risk of implant removal.
El abordaje posterior percutáneo del húmero se ha descrito utilizando una placa LCP de 4,5mm. A pesar de que las placas rectas han demostrado buenos resultados, estas no han sido diseñadas para adaptarse a la metáfisis del húmero distal. El objetivo de este estudio es probar la hipótesis nula de que no existen diferencias en la extracción de la osteosíntesis después de una MIPO posterior utilizando una placa recta comparado a una placa anatómica.
Materiales y métodosSe incluyó retrospectivamente en 2 instituciones a pacientes mayores de 18 años que habían sufrido una fractura diafisaria de húmero distal tratados mediante técnica percutánea posterior con una placa bloqueada y con un seguimiento mínimo de 12 meses. Los pacientes se dividieron en: grupo 1 (placa recta LCP de 4,5mm) y grupo 2 (placa de forma anatómica de 3,5mm). Durante el postoperatorio se reportó la evaluación clínica y radiológica, así como la necesidad de retirar el implante debido al dolor.
ResultadosSesenta y siete pacientes cumplieron los criterios de inclusión. Veintisiete pacientes en el grupo 1 y 40 en el grupo 2. No se perdió ningún paciente durante el seguimiento. Dentro del grupo 1, el 18% (IC del 95%: 6-38%) de los pacientes requirieron extracción del implante, mientras que en el grupo 2 esta incidencia fue del 0% (IC del 95%: 0-9%) (p = 0,009). No hubo diferencias estadísticas entre las medidas de resultado informadas por los pacientes; todas las fracturas consolidaron.
ConclusiónLos resultados de nuestro estudio demostrarían que el uso de placas LCP rectas de 4,5mm comparado a las placas anatómicas LCP de 3,5mm en MIPO posterior de húmero genera mayores molestias y, por lo tanto, conllevan un incremento en el riesgo de extracción del implante de un 18%.
The treatment of diaphyseal fractures of the humerus has evolved over recent years, and osteosynthesis techniques with a minimally invasive plate have become more popular. As several anatomical studies such as the one by Fernandez-Medina et al.1,2 have shown, percutaneous approaches have been developed to achieve a more biological fixation, while also reducing the probability of complications associated with the reduction compared to a conventional open approach. Percutaneous techniques have been described for humerus fractures that use straight plates on the anterior,3–5 anterolateral6,7 and posterior faces of the bone.8,9 The majority of series of patients with diaphyseal fractures of the humerus treated using minimal invasive plate osteosynthesis (MIPO) have shown good functional as well as radiological results.4,6,10 The anterior MIPO technique is chiefly indicated for diaphyseal fractures of the median third, while the anterolateral technique is used in patients with fractures of the proximal third. The posterior technique is reserved for the treatment of distal third of the humeral diaphysis.5,9 MIPO using a posterior approach has been described using a straight 4.5mm LCP.9 Although the straight plates have given good results in terms of bone consolidation, these implants were not designed to fit the distal metaphysis distal of the rear face of the humerus. Due to this, some series report the removal of these plates because of pain or discomfort in the posterior face of the elbow.10 On the other hand, the locking compression plate 3.5mm (LCP) for the distal extra-articular humerus is an angular anatomically shaped system with stable fixation for fractures of the distal humerus outside the joint. As this plate is anatomically designed to fit the distal humerus, it permits proximal diaphyseal fixation, while the other end fits the distal epiphysis of the humerus without the need for shaping. It should be underlined that currently neither implant has a formal indication for removal once the fracture has consolidated.
This study was therefore designed to examine the incidence of extraction associated with pain due to the implant, comparing the straight LCP and the anatomical extra-articular LCP in a series of patients with diaphyseal fractures of the distal third of the humerus treated using a posterior MIPO technique. Our aim is to test the null hypothesis that there is no different in the extraction of the implant due to pain between both types of osteosynthesis.
Material and methodsFor this observational retrospective study, we identified patients with diaphyseal fractures of the distal third of the humerus who had been treated using a posterior MIPO technique with a straight or anatomical LCP in 2 different institutions. The inclusion criteria were: (1) patients over the age of 18 years at the moment of the injury; (2) fractures of the distal third of the humeral diaphysis; (3) internal fixation of the humerus with a locked plate; (4) use of a posterior MIPO technique, and (5) a follow-up time of at least 12 months. There was no randomization in terms of the implant use (an anatomical 3.5mm plate vs. a straight 4.5mm LCP), as one hospital always used the anatomical plate while the other used the straight plate because of the lack of commercial availability of the anatomical implant in this country. The patients were then divided into 2 groups: group 1 (straight plate), defined as patients who fulfilled the inclusion criteria and who were treated using the straight 4.5mm LCP, and group 2 (anatomically shaped plate), defined as patients who fulfilled the inclusion criteria and who were treated with an extra-articular 3.5mm LCP.
Posterior approachA minimally invasive posterior approach was used in all cases.10
Fracture reductionThe fracture was reduced using indirect manoeuvres with axial traction, rotation and compression.
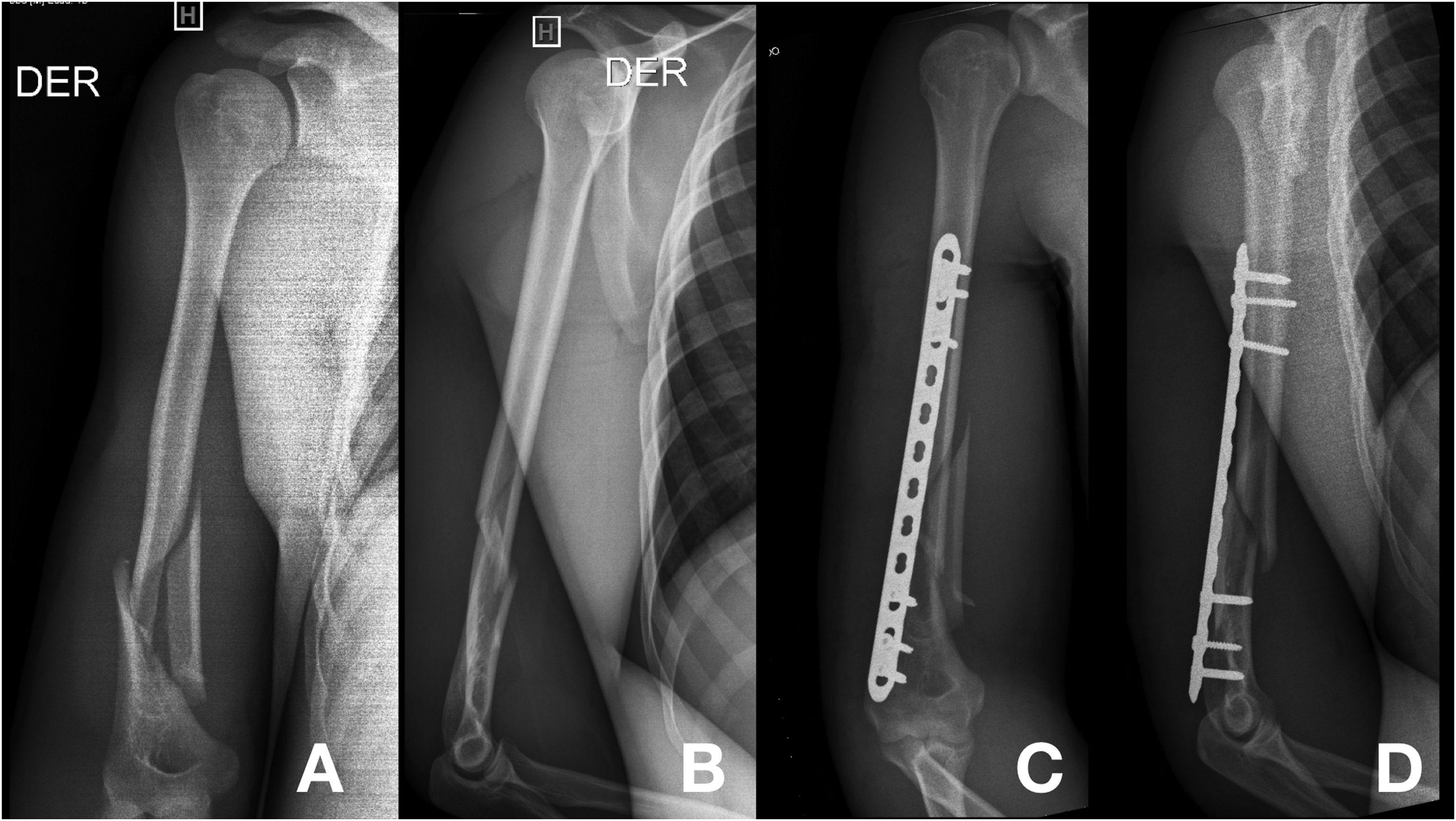
OsteosynthesisThe narrow 4.5mm LCP should be placed on the posterior face of the lateral column of the distal humerus, between the olecranon fossa and the epicondyle. The distal end of the plate is placed lateral to the olecranon fossa. In cases where the fracture is proximal to the olecranon fossa or lies within it, it is necessary to use a distal location for the plate so that 3 screws can be inserted in the distal humerus. In some cases, the plate may even be located just on the posterior face of the humeral capitellum. In the majority of patients 3 locked screws are inserted in the distal segment of the plate, and a cortical screw accompanied by 2 locked screws are inserted in its proximal end (Fig. 1).
Respecting the anatomical plate, its position must be such that it is possible to insert the distal screws through the lateral column, so that they deeply penetrate into the trochlea. At a distal level this plate accepts up to 5 locked 3.5mm screws, facilitating the use of more screws in the distal fragment (Fig. 2).
(A and B) Preoperative anteroposterior and lateral X-ray images of a type AO A1 diaphyseal fracture of the humerus. (C and D) Postoperative anteroposterior and lateral X-ray images of the fracture fixed with a 3.5mm locked plate (LCP) for the distal extra-articular humerus. In image D note the smaller profile of the plate and its anatomical shape which has to fit the posterior distal humerus.
All of the patients were instructed to use a sling to increase their comfort during the postoperative period. They were encouraged to use the operated arm in their everyday activities, as well as active moving exercises as much as they were able to tolerate, while avoiding external rotation movements or supporting weight with the shoulder in abduction during the first month after surgery.
Postoperative evaluationClinical evaluation used a hand goniometer to measure the range of active movement (ROM) of the shoulder in anterior flexion and the elbow in flexed extension. Radiological evaluation included anteroposterior (AP) and lateral projections of the arm. Consolidation was defined as the absence of pain and the presence of a bone callus bridging the fracture in the aforesaid projections. Pseudoarthrosis was defined as the lack of progression in the radiographically observed consolidation process during a period of 3 months.8 The axial alignment of the humerus was evaluated using the latest AP X-ray images obtained during follow-up. Patients were requested to complete a DASH questionnaire combined with an analogue visual scale (AVS) to describe their pain (range: 0–10). Postoperative complications were considered to be a dichotomy (yes or no) in the statistical analysis, after which they were also described. The need to extract the implant due to pain was recorded specifically as a dichotomy (yes or no) together with the month of follow-up when this occurred. This study was approved by the Ethics Committee of our institution (registration code 3048).
Statistical analysisContinuous variables are described as an average and standard deviation (SD). Nominal and ordinal variables are described as frequency counts and percentages. Radiographic alignment was compared between both groups by using a T test for independent samples. Fisher's test was used to compare the association between the type of osteosynthesis used and extraction of the same, together with its 95% confidence interval (CI).
ResultsSixty-seven patients fulfilled the inclusion criteria. 27 of these patients were treated using the straight plate (group 1) and the other 40 patients were treated with the anatomical plate (group 2). In group 1, the patients were operated by 3 different surgeons with a degree of expertise of IV (highly experienced specialist), while only 2 surgeons took part in group 2, and these too had a IV degree of expertise.11 No patient was lost during the postoperative follow-up. The average age of the patients was 35 years (SD±13) in group 1 and 37 years (SD±15) in group 2. 18 (66.7%) of the patients in group 1 were men, as were 24 (60%) of the patients in group 2. The main cause of fracture in group 1 was a fall on the same level, while in group 2 the number of falls equalled that of traffic accidents (Table 1). No patient had involvement of the soft tissues. The distribution of the fractures between the groups according to AO/ASIF classification is shown in Table 1. The average follow-up in group 1 lasted for 23 months, and the average elbow flexion was 136° (SD: 6°), the average extension of the elbow was 6° (SD: 8°), and the average shoulder flexion was 158° (SD: 22°). In group 2, with an average follow-up of 14 months, the average flexion of the elbow was 127° (SD: 7°), the average extension of the elbow was 4° (SD: 5°) and the average shoulder flexion was 148° (SD: 11°). There were no statistically significant differences between both groups in the DASH questionnaire, with an average score of 7.8 (SD: 6.9) in group 1 and 10.7 (SD: 7) in group 2. Nor was there any statistically significant difference in the pain AVS, with a median score of 0.6 (SD: 0.9) in group 1 and 1.1 (SD: 1.4) in group 2, respectively. The alignment shown by the final X-ray imaging was similar in both groups, with an average varus deviation of 4° (SD: 5°) in group 1 and an average varus deviation of 1° (SD: 1°) in group 2 (Table 2).
Demographics.
| Variable | Group 1 | Group 2 |
|---|---|---|
| N | 27 | 40 |
| Sex | ||
| Female, n (%) | 9 (33.3) | 16 (40) |
| Male, n (%) | 18 (66.7) | 24 (60) |
| Age, average (SD) | 35 (13) | 37 (15) |
| Cause, n (%) | ||
| Traffic accident | 7 (26) | 17 (42.5) |
| Falls at the same height | 19 (70.3) | 18 (45) |
| Arm wrestling | 1 (3.7) | – |
| Fire arm injury | – | 5 (12.5) |
| AO/ASIF classification, n (%) | ||
| A1 | 2 (7.4) | 3 (7.5) |
| A2 | – | 4 (10) |
| A3 | – | – |
| B1 | 8 (29.6) | 9 (22.5) |
| B2 | 2 (7.4) | 6 (15) |
| B3 | 12 (44.5) | 5 (12.5) |
| C1 | – | 4 (10) |
| C2 | – | 4 (10) |
| C3 | 3 (11.1) | 5 (12.5) |
| Follow-up in months, average (SD) | 23 (13) | 14 (4) |
SD: standard deviation.
Results.
| Variable | Group 1 | Group 2 | p-Value |
|---|---|---|---|
| DASH, average (SD) | 7.8 (6.9) | 10.7 (7) | 0.1 |
| VAS, median (SD) | 0.6 (0.9) | 1.1 (1.4) | 0.1 |
| Rx alignment, average (SD) | 4.2 (4.9) | 2.6 (1.4) | 0.1 |
| Extraction of the osteosynthesis due to pain associated with the implant | 5 (18%) | 0 (0%) | 0.009 |
| n (total percentage – CI 95%) | (6–38%) | (0–9%) |
SD: standard deviation; CI 95%: 95% confidence interval.
In group 1 18% (C I95%: 6–38%) of the patients required implant extraction after 7, 8, 9, 10 and 13 months of follow-up, while the incidence of this in group 2 was 0% (CI 95%; 0.9%) (P .009). It should be underlined that in the first group all extractions of the osteosynthesis were associated with pain and intolerance of the plate on the distal humerus, while in the second group, the only extraction of the implant was due to the express request of the patient, without being associated with pain or other complications. This is why this patient was excluded from the comparative analysis. There were no cases of pseudoarthrosis in either group. Two patients in each group suffered postoperative radial paralysis and recovered completely, without sequelae.
DiscussionThe main aim of surgical treatment of extra-articular fractures of the humerus is to restore its alignment and achieve stable fixation that permits early mobilization of the elbow and shoulder. Classically the literature has recommended conservative treatment of diaphyseal fractures of the humerus by using a functional splint. However, a recently published controlled randomized trial that compared the MIPO technique with non-surgical treatment concluded that surgical treatment has a lower rate of pseudoarthrosis and an earlier functional recovery.12
The MIPO technique in humeral fractures was first described on the anterior face of the same.3–5 Zhiquan el al.13 reported the results of 13 patients with diaphyseal fractures of the humerus treated with an anterior MIPO technique. After an average follow-up of 15.5 months, all of the fractures showed consolidation of the bone without complications. Average elbow flexion was 135° and average elbow extension was 1.5°. 5 cases showed normal alignment, with poor varus alignment in the other patients. Shen el al.14 compared the results of the anterior MIPO technique using two different implants, the 4.5mm DCP and the 4.5mm LCP. Although the two groups had different follow-up times, they found no differences in the clinical results when both groups were compared. As complications they reported one case of transitory neuropraxia of the external cutaneous antebrachial nerve, as well as in the radial nerve, and in one case consolidation was faulty with a rotational deformity. In a series of humeral fractures treated with an anterior MIPO, Chen et al.15 retrospectively reviewed 128 patients. After an average follow-up of 23 months, all of the fractures showed consolidation and the clinical results were satisfactory according to the Constant-Murley and HSS elbow scores. 4 cases of faulty consolidation in varus were reported, and there were no nerve complications.
The main limitation of the anterior MIPO technique is associated with the distal extension of the fracture, which cannot be prolonged beyond 6cm proximal to the coronoid fossa if a stable distal fixation is to be achieved. Livani and Belangero4 described the anterior MIPO technique for fractures of the distal third, fixing the distal fragment in the lateral column. Nevertheless, the complications associated with the poor distal position of the plate on the anterior face of the lateral column of the distal humerus have been linked to limitations in elbow flexion due to contact between the osteosynthesis and the coronoid apophysis or the radial dome or with the lack of stability of the distal fragment that arises in pseudoarthrosis.5,16,17
Posterior MIPO technique has been tested in cadavers,18 and it overcame the limitations of anterior MIPO described above as it makes it possible to stabilize fractures of the distal third of the humerus without compromising elbow movement. However, to properly affix the diaphysis and the lateral distal column with a straight 4.5mm LCP, it has to be placed sufficiently distally to properly fix the distal humerus. Nonetheless, this location on the distal humerus is also associated with up to 7% implant intolerance according to some series.10 Unlike a straight plate, the 3.5mm extra-articular distal humerus LCP has an anatomical design which makes it possible to fix it close to the humeral diaphysis and the lateral column of the distal epiphysis of the humerus. At this end the plate narrows to minimize irritation of the soft tissues, and it accepts up to five locked 3.5mm screws. In its proximal end the plate is based on the 4.5/5.0 narrow LCP with combined holes to give stable or dynamic angular fixation. Like the majority of modern lockable plates, the extra-articular posterior humeral 3.5mm LCP was developed to improve the fixation of periarticular fractures. Páramo-Díaz et al.19 reported a series of 23 patients with humeral fractures that were stabilized using this implant and with no complications associated with the implant over an average follow-up of one year. They underline the advantages of the pre-formed plate in giving these results. Jitprapaikulsarn et al.20 reported a series of 18 patients with an average follow-up time of 14 months without any complications associated with the implant. In our series, although we found no differences in terms of fracture alignment (Table 1) between the straight plate and the anatomical one, we did find a statistically significant difference in terms of implant extraction due to intolerance of the same on the distal humerus.
The limitations of this work can be said to include the lack of randomization in the implant used. Nevertheless, the anatomical 3.5 LCP is not commercially available in the country where the participants in group 1 live. Secondly, randomizing the use of both techniques within group 2 – where surgeons are used to using the anatomical plate – would increase the risk of bias due to “differential expertise”.21 Notwithstanding this, randomization by group (with its respective implant) would have balanced both populations demographically, as falls at the same level predominate in group 1, while there was a greater percentage of high energy impacts in group 2. This imbalance between the groups also explains why paradoxically there was a higher average of postoperative pain in group 2 together with a significantly lower rate of implant extraction. This study was designed to evaluate the incidence of implant extraction due to the pain it caused. The pain mentioned by patients in group 2 was not caused by the implant but was due to peri- and post-traumatic factors which are beyond the scope of this study.22 Nevertheless, it is important to emphasize that defining the pain variable as a dichotomy rather than a quantitative variable may hinder the reproducibility of this study, as it is based on decision by the doctor and patient together, and this is not a decision that could be measured.
Thirdly, the retrospective nature of this study explains the absence of certain data which it would have been of interest to analyze. This also explains the difference between both groups in the postoperative follow-up, as in group 1 the MIPO technique with a posterior approach was adopted earlier than was the case in group 2. Nevertheless, we believe that measuring the primary result of this study (implant extraction) in the form of a dichotomy is robust, and it is not affected by this limitation. This is because an observational study is an appropriate means of answering a research question such as the one we raised.23
ConclusionThe results of our study show that the use of straight 4.5mm LCP compared with using 3.5mm anatomical LCP in posterior MIPO technique on the humerus leads to greater discomfort and therefore increases the risk of implant extraction by 18%. This possible complication should be discussed with the patient when indicating minimally invasive surgery using a straight implant.
Level of evidenceLevel of evidence iv.
FinancingThe authors declare that they received no financial support for this work.
Conflict of interestsThe authors have no conflict of interests to declare.
Right to privacy and informed consentThe authors have obtained informed consent from the patients and/or subjects referred to in the article. This document is held by the corresponding author.
Ethics committee approvalResearch approved by the Ethics Committee of the Hospital Italiano de Buenos Aires.