Fractures of the distal femoral third are an important cause of morbidity and mortality, and their treatment is currently controversial.
ObjectivesTo compare the results between minimally invasive techniques versus exposure of the fracture site. Secondly, to evaluate the relationship between demographic factors, mechanism of injury and surgical delay with patient prognosis.
MethodRetrospective cohort study carried out between 2015 and 2021 in a tertiary hospital. Data collection was performed by reviewing medical histories, measuring demographic and hospital parameters and definitive treatment strategy. One year of follow-up was completed in all patients, assessing the occurrence of surgical complications and mortality. A stratified analysis of the variables of interest was performed among patients over 65 years of age.
Results128 fractures were recorded, with definitive osteosynthesis being performed in 117. Patients who underwent minimally invasive techniques required a shorter hospital stay (9 [7–12] vs. 12 [8.75–16] days) (p=0.007), with no differences in mortality or complications during follow-up. In those over 65 years of age, opening the fracture site was associated with an increased risk of infection compared to minimally invasive techniques (33.3% vs. 2%) (p=0.507). All the deceased were patients over 65 years of age (33.7% at one year). Surgical delay longer than 48h increased mortality by 10% among those older than 65 years (p=0.3). High-energy trauma had a higher proportion of pseudarthrosis (27.6% vs. 6.1%) (p=0.011).
ConclusionsMinimally invasive techniques decreased hospital stay but not complications or long-term mortality.
Level of evidence: IIb.
Las fracturas de tercio distal femoral son una causa importante de morbimortalidad, siendo su tratamiento actualmente controvertido.
ObjetivosComparar los resultados entre las técnicas mínimamente invasivas frente a la exposición del foco de fractura. Secundariamente, evaluar la relación entre los factores demográficos, el mecanismo lesional y la demora quirúrgica con el pronóstico de los pacientes.
MétodoEstudio tipo cohortes retrospectivas realizado entre 2015 y 2021 en un hospital de tercer nivel. La recogida de datos se realizó mediante la revisión de historias clínicas, midiendo los parámetros demográficos, hospitalarios y la estrategia de tratamiento definitivo. Se completó un año de seguimiento en todos los pacientes, evaluando la aparición de complicaciones quirúrgicas y mortalidad. Se realizó un análisis estratificado de las variables de interés entre pacientes mayores de 65 años.
ResultadosSe registraron 128 fracturas, realizándose la osteosíntesis definitiva en 117. Los pacientes intervenidos mediante técnicas mínimamente invasivas requirieron una menor estancia hospitalaria (9 [7-12] vs. 12 [8,75-16] días) (p=0,007), sin diferencias en la mortalidad o complicaciones durante el seguimiento. En mayores de 65 años, la apertura del foco de fractura asoció un aumento del riesgo de infección frente a las técnicas mínimamente invasivas (33,3% vs. 2%) (p=0,507). Todos los fallecidos fueron pacientes mayores de 65 años (33,7% al año). La demora quirúrgica superior a 48horas aumentó la mortalidad un 10% entre los mayores de 65 años (p=0,3). Los traumatismos de alta energía presentaron una mayor proporción de pseudoartrosis (27,6% vs. 6,1%) (p=0,011).
ConclusionesLas técnicas mínimamente invasivas disminuyeron la estancia hospitalaria pero no las complicaciones ni la mortalidad a largo plazo.
Nivel de evidencia: IIb.
Fractures of the distal femoral third (those involving the supracondylar and intercondylar regions) make up approximately 3–7% of all femoral fractures, and account for less than 1% of all fractures.1,2
These fractures occur in the population in a bimodal distribution. The first peak of incidence occurs in young males with high-energy trauma, while the second peak is dominated by older women, with fractures caused by low-energy trauma.2,3
Surgery is the treatment of choice for most of these fractures; there are a wide variety of surgical strategies depending on joint extension, comminution, and the trace of the fracture, and the patient characteristics.4
In recent years there has been a tendency to treat this type of fracture with the least possible aggression to the soft tissues and early consolidation for prompt recovery in young patients, and to reduce short- and medium-term complications in elderly patients. Therefore, minimally invasive techniques providing relative stability (intramedullary nailing and plates using MIPO techniques) has increased, but there is no consensus on the most appropriate surgical treatment for this type of fracture.
Therefore, knowing the different risk factors, and the suitability of each of the surgical options available to us helps us to individualise the treatment of each patient, to reduce the time necessary for functional recovery and the complications arising from these injuries and their treatment.
The primary objective of this study was to compare the progress of patients treated using minimally invasive techniques versus those whose fracture site needed to be opened during surgery. And to analyse these two treatment methods in patients over 65 years of age.
As secondary objectives, we sought to evaluate the different demographic factors, such as age or mechanism of injury, influencing the prognosis of this type of fracture, and the potential influence of delaying definitive surgery on the prognosis of patients, especially in those over 65 years of age.
Materials and methodsWe conducted an analytical retrospective cohort study in patients with distal femoral fractures operated on between January 2015 and December 2021, in a tertiary level hospital attending a population of around 440,000 inhabitants, which is the referral centre for the province. The data for the present study were obtained from the database of fractures treated in the hospital over that period.
The data collection was based on an anonymous review of the clinical history of the patients, without providing the study with identifying data. Demographic parameters were collected, such as the patients’ age and sex, and the mechanism of fracture (high or low energy), fracture classification (AO5 classification for fractures of the distal femur and Gustilo and Anderson classification in the case of open fractures), time to surgery, and length of hospital stay. Parameters such as the treatment strategy used for each fracture, onset of acute surgical complications, and in-hospital mortality were collected during admission.
All patients were followed up for one year, after which the presence of long-term complications recorded in the clinical history during follow-up, and mortality over this period were evaluated.
All patients seen in the hospital where the study was conducted, over the period indicated above, who were diagnosed with acute fracture of the distal third of the femur were included in the present study.
Exclusion criteria were determined as follows:
- •
Peri-implant or periprosthetic fractures of devices implanted in the femoral middle and distal thirds.
- •
Patients under 14 years of age.
- •
Patients who did not complete the follow-up in the hospital where the present study was conducted, and incomplete follow-ups, or follow-ups of less than one year's duration.
A digital database was created with the parameters collected. A data management programme (IBM SPSS Statistics v.25) was used for the statistical analysis of the study. First, a descriptive study of the variables was performed, and the normality of the quantitative variables was determined using the Kolgomorov–Smirnoff test. Nominal variables were described based on the relative frequencies of their respective categories. Qualitative variables were described with their median and interquartile range. Different bivariate analyses were performed, using the χ2, Mann–Whitney, Kruskal–Wallis, and Spearman statistical tests, according to the characteristics of the variables studied. Finally, those variables that showed statistically significant associations in the bivariate analysis were subjected to various multivariate tests to rule out confounding factors not controlled for during the study design, by performing binary logistic regression and linear regression of the variables.
We compared patients who underwent fracture fixation using minimally invasive techniques (using plates or intramedullary nailing) with those who underwent fixation after opening the fracture site. The need to open the fracture site to achieve reduction was considered sufficient to include patients in the ORIF group, regardless of the type of implant used.
A stratified analysis was performed by age (patients over versus under 65 years of age) according to demographic variables, surgical technique used, and time to intervention.
The potential relationship between the delay in days to fracture intervention (in the first 48h or later) and hospital stay, long-term complications, and mortality in the first year was tested.
The study was conducted in accordance with the ethical standards recognised by the Declaration of Helsinki and resolution 008430 of 1993, and was approved by the Ethics Committee for Biomedical Research of the province of Granada (CEI/CEIM Granada; code: 6hWMS821PFIRMAUegzkMz+S5FCmAr5). The patients participating in the study gave their informed consent.
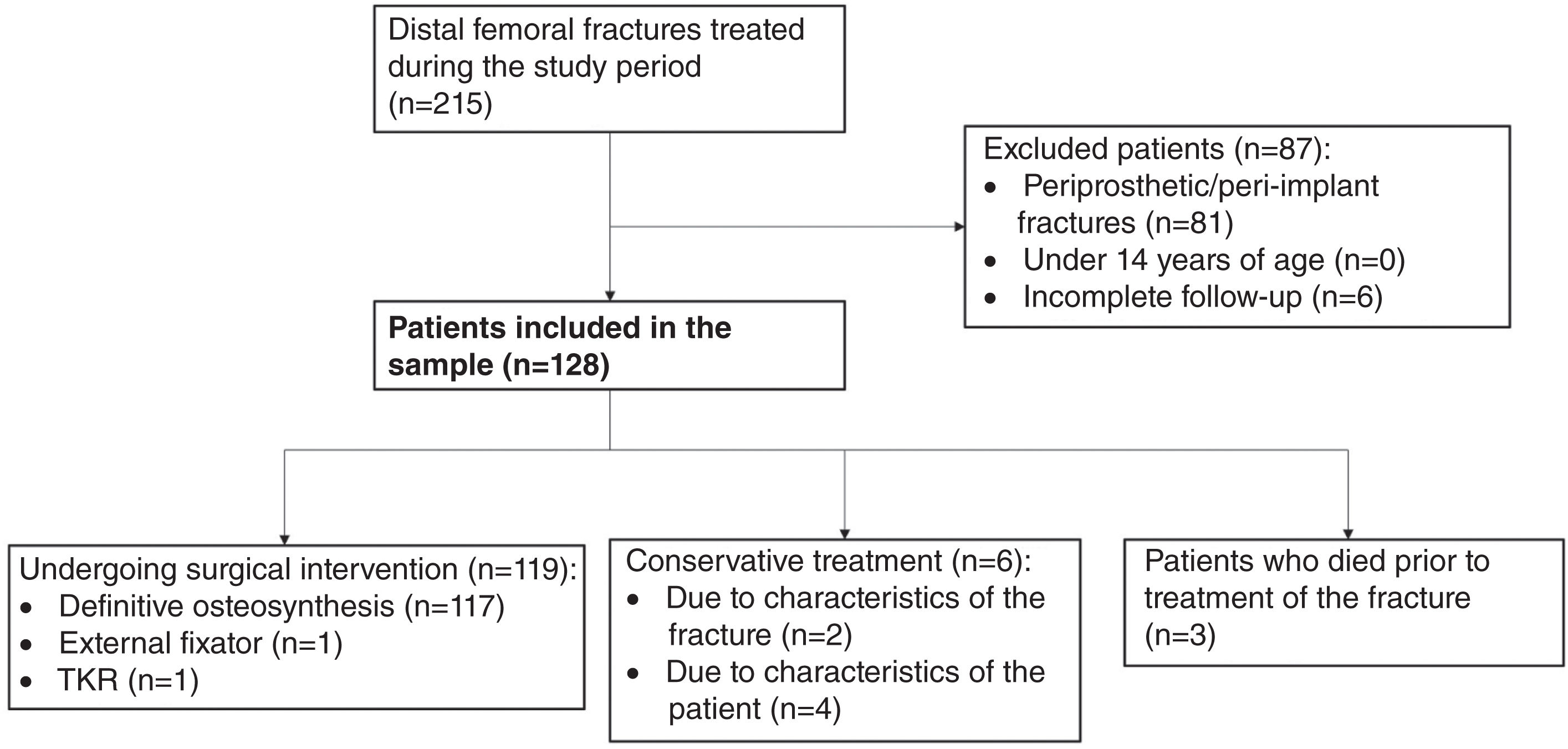
ResultsA total of 215 fractures of the distal femur were recorded during the period under study. Of these, 128 fractures met the inclusion criteria outlined above. A total of 119 fractures of the distal femur were operated, with 117 fractures undergoing definitive osteosynthesis (Fig. 1). One of the patients was treated temporarily by external fixation, but could not undergo definitive osteosynthesis due to his poor general condition during admission. This treatment was indicated in 2 of the 6 fractures treated conservatively, due to the characteristics of the fracture (minimal displacement, stable pattern), while in 4 of the cases, the patient's personal history contraindicated definitive surgery.
None of the quantitative variables showed a normal distribution during the descriptive statistical analysis of the sample.
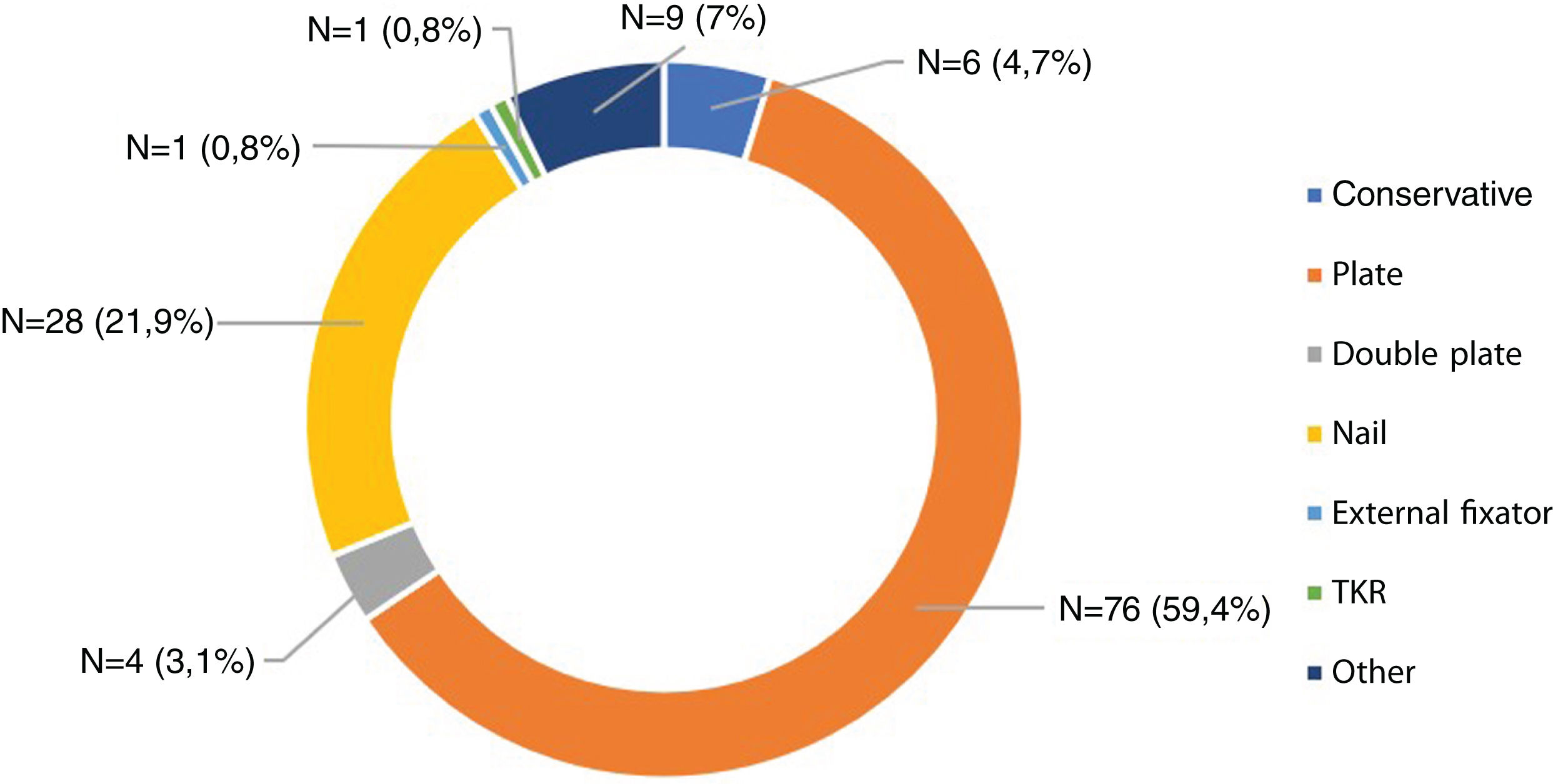
The median age of the patients included in the present study was 75 years, and the female sex predominated. Most of the fractures recorded were due to low-energy trauma. The median length of hospital stay was 10 days, with a median of 4 days until surgery if surgery was performed. A total of 92.9% of patients underwent surgery, with different plate-screw assemblies being the most commonly used (Fig. 2). Follow-up of 21 patients (16.4%) was not completed because they died within one year. Of the patients who completed follow-up, 27.3% suffered some kind of complication resulting from surgery.
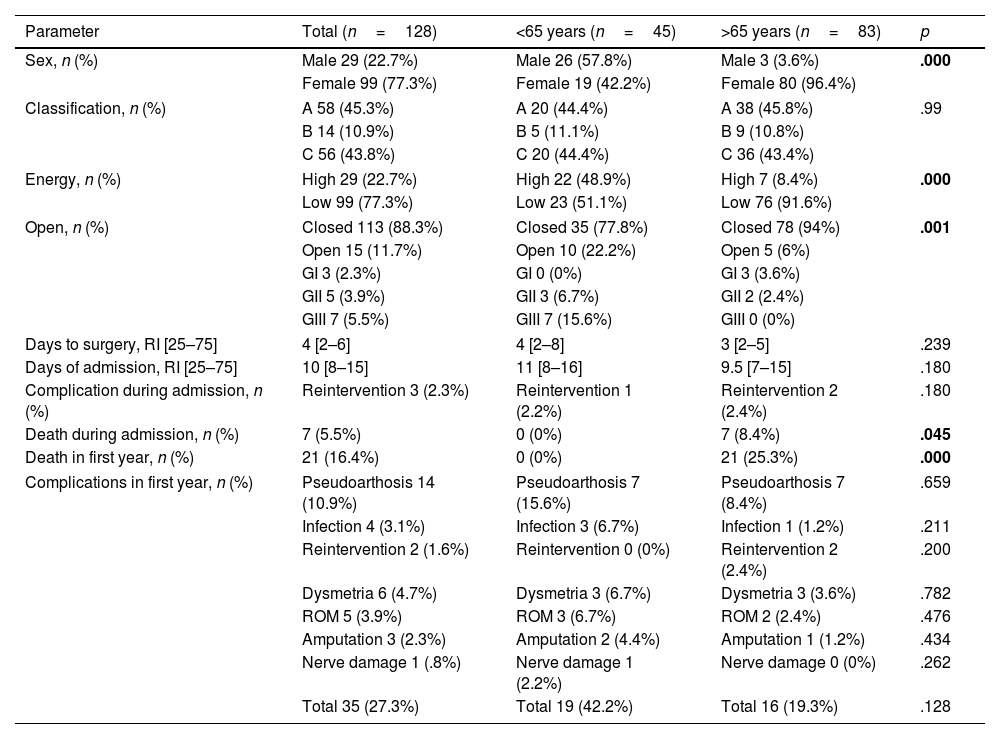
No statistically significant age-dependent differences in surgical complications during follow-up were found. Sex (p=.001) and low-energy trauma (p=.001) were shown to be a risk factor for this type of fracture in the population over 65 years of age in the multivariate analysis performed. All the deaths recorded, both in-hospital and during follow-up, occurred in this age group (Table 1).
Comparative analysis >65 years and <65 years.
| Parameter | Total (n=128) | <65 years (n=45) | >65 years (n=83) | p |
|---|---|---|---|---|
| Sex, n (%) | Male 29 (22.7%) | Male 26 (57.8%) | Male 3 (3.6%) | .000 |
| Female 99 (77.3%) | Female 19 (42.2%) | Female 80 (96.4%) | ||
| Classification, n (%) | A 58 (45.3%) | A 20 (44.4%) | A 38 (45.8%) | .99 |
| B 14 (10.9%) | B 5 (11.1%) | B 9 (10.8%) | ||
| C 56 (43.8%) | C 20 (44.4%) | C 36 (43.4%) | ||
| Energy, n (%) | High 29 (22.7%) | High 22 (48.9%) | High 7 (8.4%) | .000 |
| Low 99 (77.3%) | Low 23 (51.1%) | Low 76 (91.6%) | ||
| Open, n (%) | Closed 113 (88.3%) | Closed 35 (77.8%) | Closed 78 (94%) | .001 |
| Open 15 (11.7%) | Open 10 (22.2%) | Open 5 (6%) | ||
| GI 3 (2.3%) | GI 0 (0%) | GI 3 (3.6%) | ||
| GII 5 (3.9%) | GII 3 (6.7%) | GII 2 (2.4%) | ||
| GIII 7 (5.5%) | GIII 7 (15.6%) | GIII 0 (0%) | ||
| Days to surgery, RI [25–75] | 4 [2–6] | 4 [2–8] | 3 [2–5] | .239 |
| Days of admission, RI [25–75] | 10 [8–15] | 11 [8–16] | 9.5 [7–15] | .180 |
| Complication during admission, n (%) | Reintervention 3 (2.3%) | Reintervention 1 (2.2%) | Reintervention 2 (2.4%) | .180 |
| Death during admission, n (%) | 7 (5.5%) | 0 (0%) | 7 (8.4%) | .045 |
| Death in first year, n (%) | 21 (16.4%) | 0 (0%) | 21 (25.3%) | .000 |
| Complications in first year, n (%) | Pseudoarthosis 14 (10.9%) | Pseudoarthosis 7 (15.6%) | Pseudoarthosis 7 (8.4%) | .659 |
| Infection 4 (3.1%) | Infection 3 (6.7%) | Infection 1 (1.2%) | .211 | |
| Reintervention 2 (1.6%) | Reintervention 0 (0%) | Reintervention 2 (2.4%) | .200 | |
| Dysmetria 6 (4.7%) | Dysmetria 3 (6.7%) | Dysmetria 3 (3.6%) | .782 | |
| ROM 5 (3.9%) | ROM 3 (6.7%) | ROM 2 (2.4%) | .476 | |
| Amputation 3 (2.3%) | Amputation 2 (4.4%) | Amputation 1 (1.2%) | .434 | |
| Nerve damage 1 (.8%) | Nerve damage 1 (2.2%) | Nerve damage 0 (0%) | .262 | |
| Total 35 (27.3%) | Total 19 (42.2%) | Total 16 (19.3%) | .128 | |
| Multivariate | |||
|---|---|---|---|
| Variables | RR | CI (95%) | p |
| Sex | 1.903 | (1.313–2.756) | .001 |
| Energy | .154 | (.051–.466) | .001 |
| Open fracture | .648 | (.336–1.250) | .196 |
| Days of admission | 1.1013 | (.977–1.050) | .479 |
| Complications during admission | 1.195 | (.525–2.720) | .671 |
| Complications in the first year | .838 | (.659–1.065) | .149 |
Results that achieved statistical significance are marked in bold.
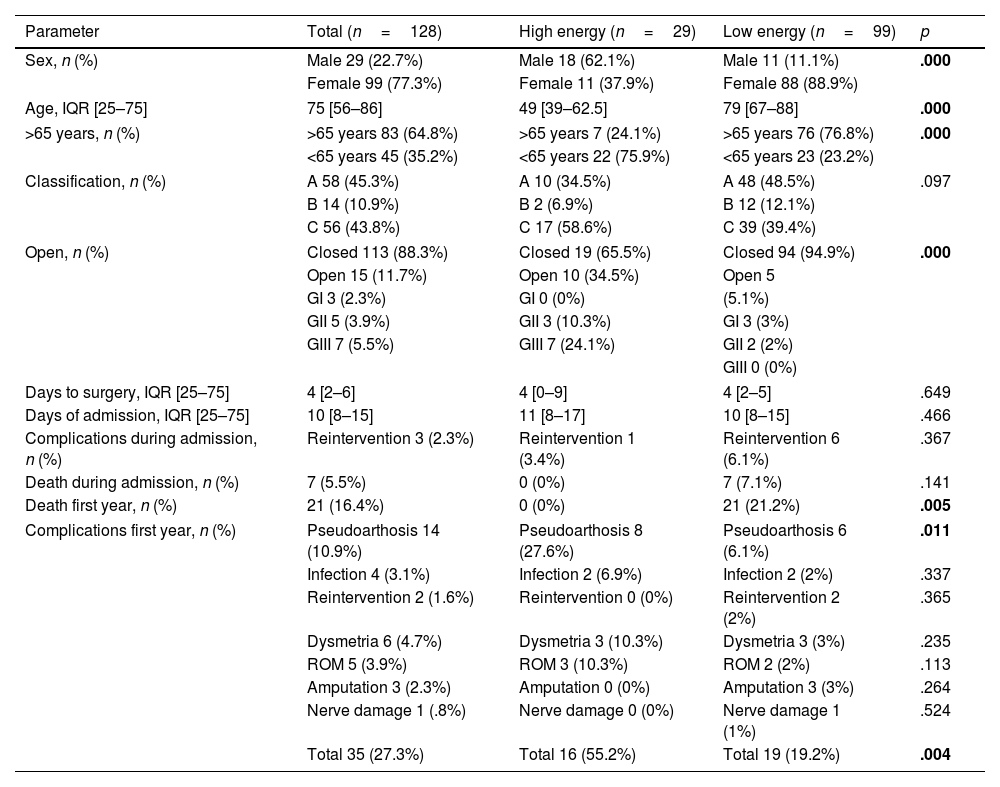
High-energy trauma showed a tendency to cause fractures in male patients (p=.015) and in those under 65 years of age (p=.000), and to cause open fractures in any age group compared to low-energy fractures (p=.046), in the multivariate study. High-energy trauma was also associated with an increased proportion of complications at one-year follow-up, especially pseudarthrosis and delayed fracture consolidation, although this did not reach statistical significance in the multivariate analysis (Table 2).
Comparative analysis of the mechanism of injury.
| Parameter | Total (n=128) | High energy (n=29) | Low energy (n=99) | p |
|---|---|---|---|---|
| Sex, n (%) | Male 29 (22.7%) | Male 18 (62.1%) | Male 11 (11.1%) | .000 |
| Female 99 (77.3%) | Female 11 (37.9%) | Female 88 (88.9%) | ||
| Age, IQR [25–75] | 75 [56–86] | 49 [39–62.5] | 79 [67–88] | .000 |
| >65 years, n (%) | >65 years 83 (64.8%) | >65 years 7 (24.1%) | >65 years 76 (76.8%) | .000 |
| <65 years 45 (35.2%) | <65 years 22 (75.9%) | <65 years 23 (23.2%) | ||
| Classification, n (%) | A 58 (45.3%) | A 10 (34.5%) | A 48 (48.5%) | .097 |
| B 14 (10.9%) | B 2 (6.9%) | B 12 (12.1%) | ||
| C 56 (43.8%) | C 17 (58.6%) | C 39 (39.4%) | ||
| Open, n (%) | Closed 113 (88.3%) | Closed 19 (65.5%) | Closed 94 (94.9%) | .000 |
| Open 15 (11.7%) | Open 10 (34.5%) | Open 5 | ||
| GI 3 (2.3%) | GI 0 (0%) | (5.1%) | ||
| GII 5 (3.9%) | GII 3 (10.3%) | GI 3 (3%) | ||
| GIII 7 (5.5%) | GIII 7 (24.1%) | GII 2 (2%) | ||
| GIII 0 (0%) | ||||
| Days to surgery, IQR [25–75] | 4 [2–6] | 4 [0–9] | 4 [2–5] | .649 |
| Days of admission, IQR [25–75] | 10 [8–15] | 11 [8–17] | 10 [8–15] | .466 |
| Complications during admission, n (%) | Reintervention 3 (2.3%) | Reintervention 1 (3.4%) | Reintervention 6 (6.1%) | .367 |
| Death during admission, n (%) | 7 (5.5%) | 0 (0%) | 7 (7.1%) | .141 |
| Death first year, n (%) | 21 (16.4%) | 0 (0%) | 21 (21.2%) | .005 |
| Complications first year, n (%) | Pseudoarthosis 14 (10.9%) | Pseudoarthosis 8 (27.6%) | Pseudoarthosis 6 (6.1%) | .011 |
| Infection 4 (3.1%) | Infection 2 (6.9%) | Infection 2 (2%) | .337 | |
| Reintervention 2 (1.6%) | Reintervention 0 (0%) | Reintervention 2 (2%) | .365 | |
| Dysmetria 6 (4.7%) | Dysmetria 3 (10.3%) | Dysmetria 3 (3%) | .235 | |
| ROM 5 (3.9%) | ROM 3 (10.3%) | ROM 2 (2%) | .113 | |
| Amputation 3 (2.3%) | Amputation 0 (0%) | Amputation 3 (3%) | .264 | |
| Nerve damage 1 (.8%) | Nerve damage 0 (0%) | Nerve damage 1 (1%) | .524 | |
| Total 35 (27.3%) | Total 16 (55.2%) | Total 19 (19.2%) | .004 | |
| Multivariate | |||
|---|---|---|---|
| Variables | RR | CI (95%) | p |
| Sex | 2.502 | (1.196–5.235) | .015 |
| Age | .951 | (.933–.970) | .000 |
| Classification | 1.292 | (.752–2.221) | .353 |
| Open fracture | 1.422 | (1.015–5.779) | .046 |
| Complications first year | .5 | (.171–1.463) | .206 |
| Pseudoarthosis first year | 2.667 | (.591–12.042) | .202 |
Results that achieved statistical significance are marked in bold.
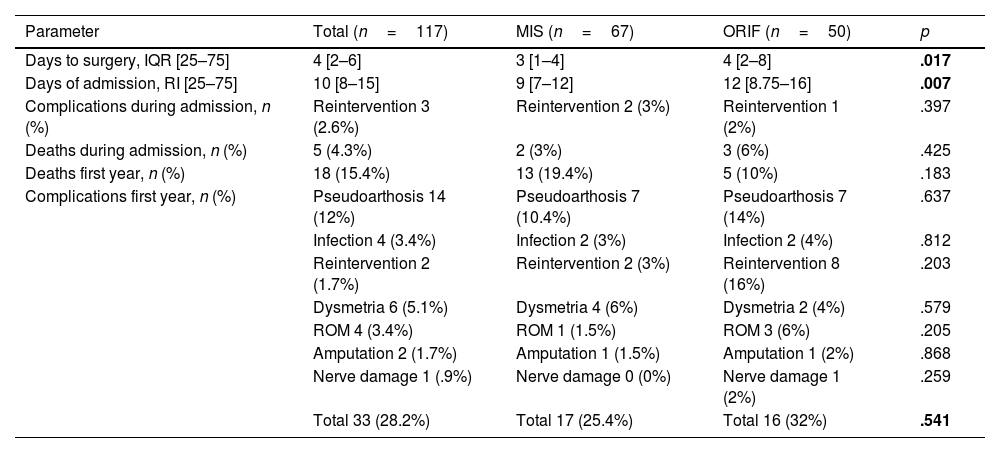
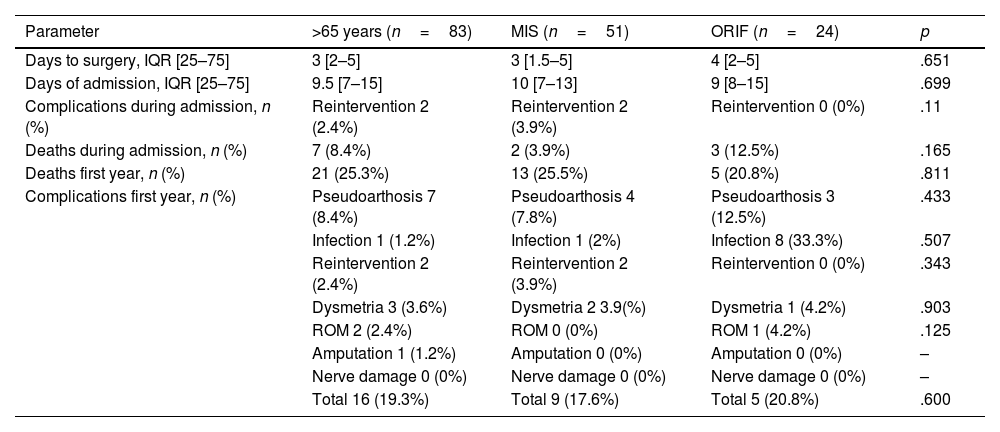
Minimally invasive techniques were associated with a shorter hospital stay, although these data were not consistent in the multivariate analysis (p=.372). No differences were found between the two groups in terms of complications or mortality during follow-up (Table 3). Similarly, no significant differences were found between the two treatment options in terms of complications or mortality when analysing the subgroup of patients over 65 years of age (Table 4).
Comparative analysis minimally invasive surgery (MIS) vs. ORIF.
| Parameter | Total (n=117) | MIS (n=67) | ORIF (n=50) | p |
|---|---|---|---|---|
| Days to surgery, IQR [25–75] | 4 [2–6] | 3 [1–4] | 4 [2–8] | .017 |
| Days of admission, RI [25–75] | 10 [8–15] | 9 [7–12] | 12 [8.75–16] | .007 |
| Complications during admission, n (%) | Reintervention 3 (2.6%) | Reintervention 2 (3%) | Reintervention 1 (2%) | .397 |
| Deaths during admission, n (%) | 5 (4.3%) | 2 (3%) | 3 (6%) | .425 |
| Deaths first year, n (%) | 18 (15.4%) | 13 (19.4%) | 5 (10%) | .183 |
| Complications first year, n (%) | Pseudoarthosis 14 (12%) | Pseudoarthosis 7 (10.4%) | Pseudoarthosis 7 (14%) | .637 |
| Infection 4 (3.4%) | Infection 2 (3%) | Infection 2 (4%) | .812 | |
| Reintervention 2 (1.7%) | Reintervention 2 (3%) | Reintervention 8 (16%) | .203 | |
| Dysmetria 6 (5.1%) | Dysmetria 4 (6%) | Dysmetria 2 (4%) | .579 | |
| ROM 4 (3.4%) | ROM 1 (1.5%) | ROM 3 (6%) | .205 | |
| Amputation 2 (1.7%) | Amputation 1 (1.5%) | Amputation 1 (2%) | .868 | |
| Nerve damage 1 (.9%) | Nerve damage 0 (0%) | Nerve damage 1 (2%) | .259 | |
| Total 33 (28.2%) | Total 17 (25.4%) | Total 16 (32%) | .541 |
| Multivariate | |||
|---|---|---|---|
| Variables | RR | IC (95%) | p |
| Days to surgery | 1.099 | (.952–1.268) | .198 |
| Days of admission | .974 | (.920–1.032) | .372 |
| Deaths first year | .365 | (.118–1.132) | .081 |
Results that achieved statistical significance are marked in bold.
Comparative analysis minimally invasive surgery (MIS) vs. ORIF in patients over 65 years of age.
| Parameter | >65 years (n=83) | MIS (n=51) | ORIF (n=24) | p |
|---|---|---|---|---|
| Days to surgery, IQR [25–75] | 3 [2–5] | 3 [1.5–5] | 4 [2–5] | .651 |
| Days of admission, IQR [25–75] | 9.5 [7–15] | 10 [7–13] | 9 [8–15] | .699 |
| Complications during admission, n (%) | Reintervention 2 (2.4%) | Reintervention 2 (3.9%) | Reintervention 0 (0%) | .11 |
| Deaths during admission, n (%) | 7 (8.4%) | 2 (3.9%) | 3 (12.5%) | .165 |
| Deaths first year, n (%) | 21 (25.3%) | 13 (25.5%) | 5 (20.8%) | .811 |
| Complications first year, n (%) | Pseudoarthosis 7 (8.4%) | Pseudoarthosis 4 (7.8%) | Pseudoarthosis 3 (12.5%) | .433 |
| Infection 1 (1.2%) | Infection 1 (2%) | Infection 8 (33.3%) | .507 | |
| Reintervention 2 (2.4%) | Reintervention 2 (3.9%) | Reintervention 0 (0%) | .343 | |
| Dysmetria 3 (3.6%) | Dysmetria 2 3.9(%) | Dysmetria 1 (4.2%) | .903 | |
| ROM 2 (2.4%) | ROM 0 (0%) | ROM 1 (4.2%) | .125 | |
| Amputation 1 (1.2%) | Amputation 0 (0%) | Amputation 0 (0%) | – | |
| Nerve damage 0 (0%) | Nerve damage 0 (0%) | Nerve damage 0 (0%) | – | |
| Total 16 (19.3%) | Total 9 (17.6%) | Total 5 (20.8%) | .600 |
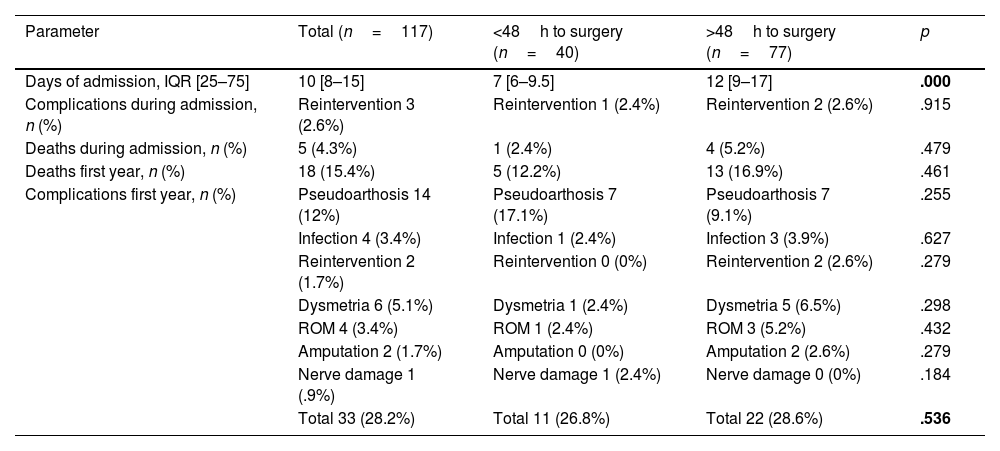
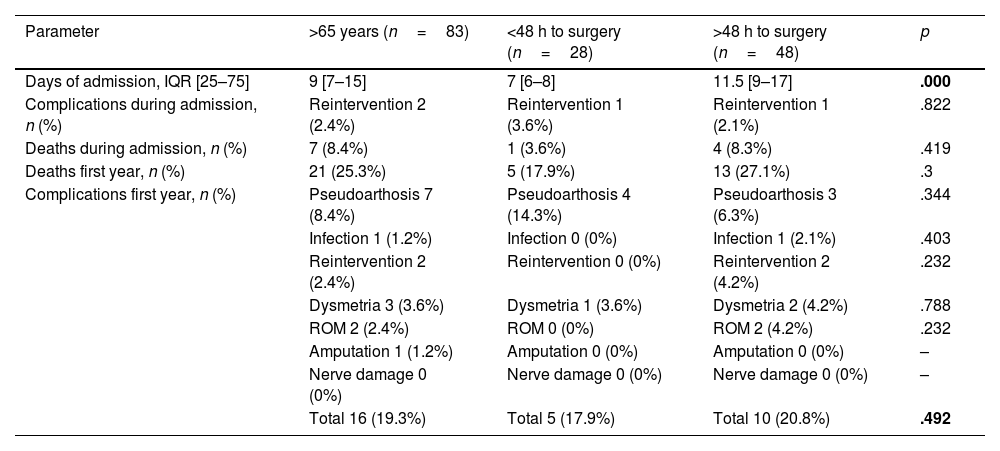
Days to fracture treatment correlated positively with days of hospital admission of patients, with a statistically significant relationship both in the overall sample (p=.000) and in the subgroup of patients over 65 years of age (p=.001) (Tables 5 and 6). The Spearman correlation index between days to intervention and hospital stay was positive with a value of .623 (p=.000). Delaying intervention beyond 48h did not show an increase in complications during follow-up. Although mortality increased by 10% among the patients older than 65 years who underwent surgery after more than 48h, this did not reach statistical significance (p=.3) (Table 6).
Analysis of time to surgery.
| Parameter | Total (n=117) | <48h to surgery (n=40) | >48h to surgery (n=77) | p |
|---|---|---|---|---|
| Days of admission, IQR [25–75] | 10 [8–15] | 7 [6–9.5] | 12 [9–17] | .000 |
| Complications during admission, n (%) | Reintervention 3 (2.6%) | Reintervention 1 (2.4%) | Reintervention 2 (2.6%) | .915 |
| Deaths during admission, n (%) | 5 (4.3%) | 1 (2.4%) | 4 (5.2%) | .479 |
| Deaths first year, n (%) | 18 (15.4%) | 5 (12.2%) | 13 (16.9%) | .461 |
| Complications first year, n (%) | Pseudoarthosis 14 (12%) | Pseudoarthosis 7 (17.1%) | Pseudoarthosis 7 (9.1%) | .255 |
| Infection 4 (3.4%) | Infection 1 (2.4%) | Infection 3 (3.9%) | .627 | |
| Reintervention 2 (1.7%) | Reintervention 0 (0%) | Reintervention 2 (2.6%) | .279 | |
| Dysmetria 6 (5.1%) | Dysmetria 1 (2.4%) | Dysmetria 5 (6.5%) | .298 | |
| ROM 4 (3.4%) | ROM 1 (2.4%) | ROM 3 (5.2%) | .432 | |
| Amputation 2 (1.7%) | Amputation 0 (0%) | Amputation 2 (2.6%) | .279 | |
| Nerve damage 1 (.9%) | Nerve damage 1 (2.4%) | Nerve damage 0 (0%) | .184 | |
| Total 33 (28.2%) | Total 11 (26.8%) | Total 22 (28.6%) | .536 |
| Multivariate | |||
|---|---|---|---|
| Variables | RR | CI (95%) | p |
| Days of admission | 1.323 | (1.16–1.5) | .000 |
Results that achieved statistical significance are marked in bold.
Analysis of days until surgery in patients over 65 years of age.
| Parameter | >65 years (n=83) | <48 h to surgery (n=28) | >48 h to surgery (n=48) | p |
|---|---|---|---|---|
| Days of admission, IQR [25–75] | 9 [7–15] | 7 [6–8] | 11.5 [9–17] | .000 |
| Complications during admission, n (%) | Reintervention 2 (2.4%) | Reintervention 1 (3.6%) | Reintervention 1 (2.1%) | .822 |
| Deaths during admission, n (%) | 7 (8.4%) | 1 (3.6%) | 4 (8.3%) | .419 |
| Deaths first year, n (%) | 21 (25.3%) | 5 (17.9%) | 13 (27.1%) | .3 |
| Complications first year, n (%) | Pseudoarthosis 7 (8.4%) | Pseudoarthosis 4 (14.3%) | Pseudoarthosis 3 (6.3%) | .344 |
| Infection 1 (1.2%) | Infection 0 (0%) | Infection 1 (2.1%) | .403 | |
| Reintervention 2 (2.4%) | Reintervention 0 (0%) | Reintervention 2 (4.2%) | .232 | |
| Dysmetria 3 (3.6%) | Dysmetria 1 (3.6%) | Dysmetria 2 (4.2%) | .788 | |
| ROM 2 (2.4%) | ROM 0 (0%) | ROM 2 (4.2%) | .232 | |
| Amputation 1 (1.2%) | Amputation 0 (0%) | Amputation 0 (0%) | – | |
| Nerve damage 0 (0%) | Nerve damage 0 (0%) | Nerve damage 0 (0%) | – | |
| Total 16 (19.3%) | Total 5 (17.9%) | Total 10 (20.8%) | .492 |
| Multivariate | |||
|---|---|---|---|
| Variables | RR | CI (95%) | p |
| Days of admission | 1.317 | (1.116–1.555) | .001 |
Results that achieved statistical significance are marked in bold.
The primary aim of the present study was to compare the evolution in terms of complications and mortality between the current different surgical approaches to treat fractures of the distal femoral third. Despite the size of our sample, we found no differences in terms of complications at one-year follow-up or mortality between opening the fracture site during surgery and the use of minimally invasive techniques.
Most of the fractures included in our study were treated surgically, we opted for conservative treatment only in patients in whom surgical intervention was not advisable, due to their baseline condition, or limited fracture displacement.
On this point, the current literature maintains that surgery is the treatment of choice for this type of fracture, with the aim of achieving rapid mobilisation of the affected limb, allowing the limb to recover its functionality6,7; and there is currently no clear recommendation as to which type of surgical technique is the most appropriate.4,8
Minimally invasive techniques, more respectful of soft tissues,9 have gained ground in the most recent literature, especially focused on elderly patients, in whom the priority objective must be early mobilisation and weight-bearing, restoring the axis of the limb, and relegating to second place the anatomical reduction of the fracture, even at the joint level.10,11
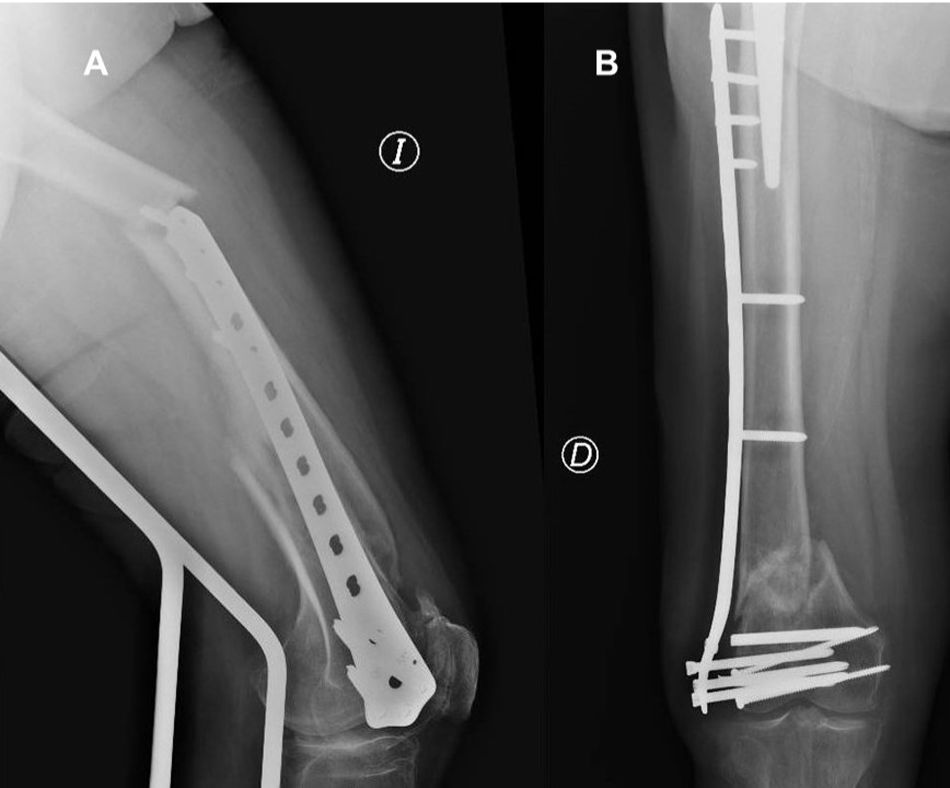
Of the surgical options deployed in our study (Fig. 2), both anatomical and locked plates were selected for implantation in most of the patients (59.4%) (Fig. 3), followed by intramedullary nailing in 21.9% of cases.
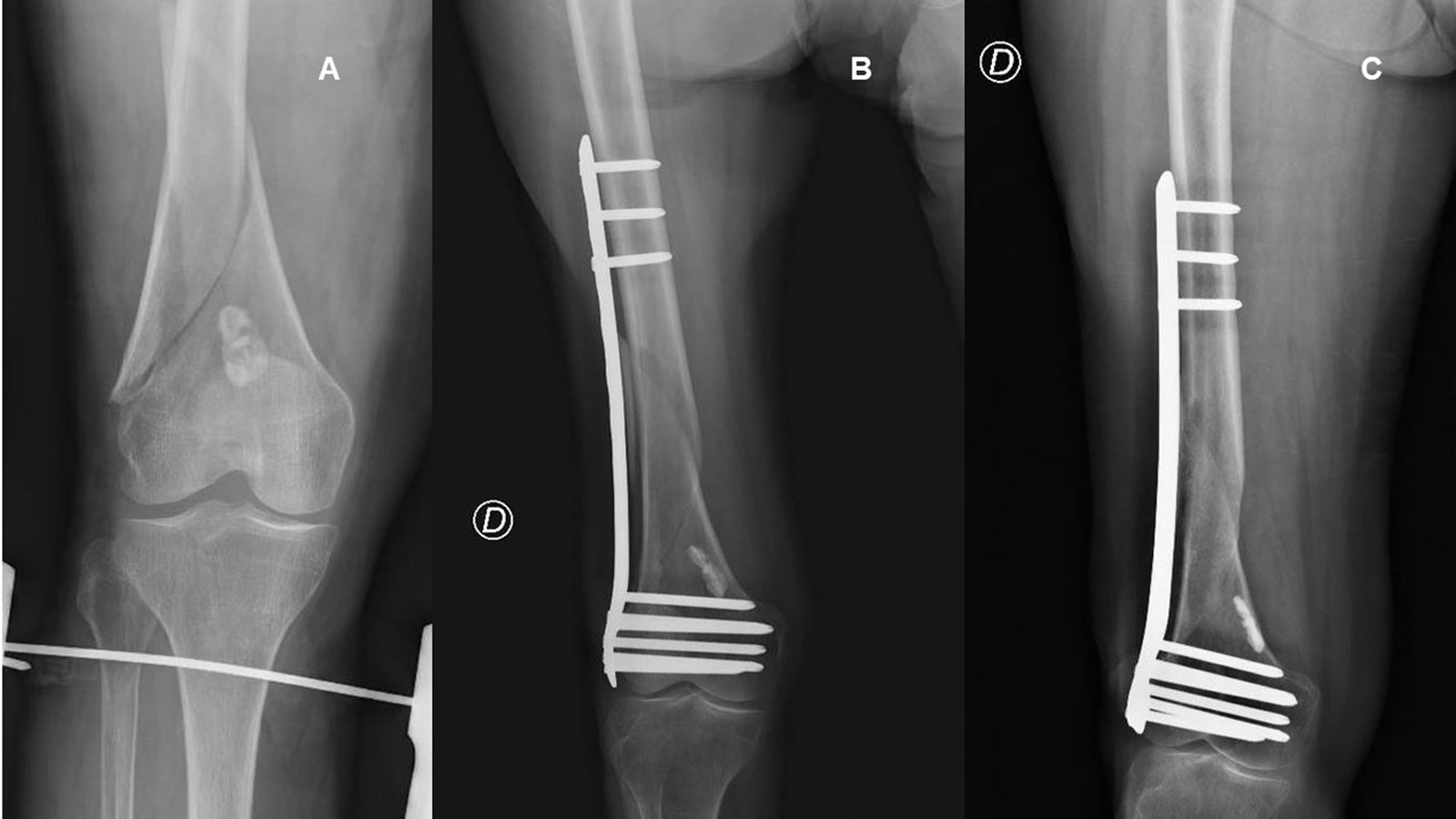
Retrograde nailing is especially indicated in the literature in extra-articular and partially articular fractures.12,13 Relative stability of the fracture synthesis is achieved with this system, which does not provide adequate control of the varus/valgus of the fracture site, which means opening the fracture site in a significant number of cases to improve fracture reduction (Fig. 4).
Condylar plates are now widely used and allow minimally invasive treatment through relative stability. The MIPO concept involves indirect reduction of the fracture by inserting the plate below the musculature and above the periosteum. The reduced dissection of soft tissue at the fracture site appears to promote fracture consolidation.14,15 This technique is especially indicated when there is significant metaphyseal involvement, in osteoporotic bone and in periprosthetic fractures.
In our study, the patients treated using minimally invasive techniques had a significantly reduced hospital stay (from 12 to 9 days compared to patients in whom the fracture site was opened), which is similar to the literature consulted.16 In the patients over the age of 65 years in our study, the difference was reduced to only one day, probably in relation to the patients’ baseline comorbidities and their lower functional reserve to cope with major surgery, regardless of the surgical technique deployed.
We found no differences in terms of complications in the first year of follow-up between the two groups in general terms, in either infection or, more specifically, delayed healing. However, in patients over 65 years of age, opening the fracture site was associated with a higher rate of infection at one year follow-up (33% versus 2% for the minimally invasive techniques). Although the small sample size of this subgroup means we should view this result with caution because it did not reach statistical significance, we consider it to be a result worth highlighting, especially on the basis of previous literature. A recent study17 relates different risk factors such as diabetes mellitus, obesity, or the presence of an open fracture as determinants for the development of surgical infection in patients in whom the fracture site was opened to achieve adequate reduction, reflecting an overall infection rate of 4%, significantly lower than the results of our study.
Along the same lines, a systematic review published by Zlowodzki et al.,18 described a reduction in the proportion of infections when minimally invasive techniques were used. However, in the same review, the authors found an increase in material failure and the need for revision surgery in these techniques, we did not have these results in our study. It is important to note at this point that the choice of implant to be used may be influenced by the fracture pattern. Therefore, implants associated with minimally invasive techniques (such as intramedullary nailing) may not be suitable for the treatment of more complex fractures which have a worse overall or functional prognosis, which is a potential source of bias both in the present study and in the previously published literature.
The risk factors for the failure of minimally invasive implants described in the literature include obesity, open fractures, infection of the surgical site, or the use of stainless steel implants19 (Fig. 5).
The mortality of patients treated by minimally invasive techniques was reduced by half compared to those in whom the fracture site was opened in the analysis of the overall group of patients (19.4% vs. 10%). The previous literature consulted found no differences in terms of mortality during patient follow-up depending on the type of osteosynthesis or implant used.20
It should be noted that, in our study, all deaths occurred in the patients over 65 years of age, adding 8.4% in-hospital mortality and 25.3% mortality at the first year of follow-up. This accumulated mortality at one year is similar to that described in similar studies in which it is around 30%, age being an independent predictor of mortality in this type of fracture.7,20 Various studies have highlighted the similarities between supracondylar fractures and hip fractures in elderly patients, with similar mortality in both and a benefit in early surgical treatment in the first 48h.21–25
When comparing the mortality of both techniques in this subgroup, we found no differences between patients treated by minimally invasive techniques and ORIF (25.5% vs. 20.8%), it was even slightly higher in those patients undergoing minimally invasive techniques. This may be explained by the high number of elderly patients treated by minimally invasive techniques in our sample, age being a potential confounding factor in the true mortality of the surgical options.
The demographic characteristics of the patients under study showed a characteristic bimodal distribution already described in previous literature2,3 (Table 1). On the one hand, most were patients over 65 years of age, predominantly women, with closed supra- and intercondylar fractures of the distal femur following low-energy trauma, associated with a personal history of osteoporosis.26 On the other hand were young patients suffering high energy trauma, which is associated with a greater number of open fractures, and more complex fracture patterns, and there was a predominance of males within this group.
We found a higher rate of complications at one year follow-up in the group of patients under 65 years of age, double the complications recorded in the older group, especially in terms of the development of delayed fracture healing and infectious fracture complications, which is probably related to the greater soft tissue damage and higher rate of open fractures in this group of patients.
High-energy mechanisms of injury were associated with a high percentage of open fractures with significant soft-tissue damage, and greater severity on the Gustilo scale. It seems logical to think that high-energy trauma involves greater tissue and associated soft tissue injury, and greater force absorption by bone tissue, resulting in greater fracture complexity. Previous studies have found similar results with increased fracture pattern complexity and a higher rate of open fractures in fractures secondary to high-energy trauma.26,27
Fractures secondary to high-energy trauma had more complications during the first year of follow-up, especially delayed consolidation (Fig. 6). Previous studies have related the presenting with an open distal femoral fracture with a delay in its consolidation,27,28 which may explain the increase in delayed consolidation in the group of patients with high-energy fractures. There being no deaths during follow-up in the group of patients who suffered high-energy trauma could be partially due to chance, as it is unlikely that there would be no deaths among polytrauma patients with distal femoral fractures.
Surgical delay of this type of fracture beyond 48 hours was associated in our sample with an increased hospital stay. This result is in line with previously published literature, such as the study by Yamamoto et al.,29 in which a delay in surgery to these fractures of more than 48h was associated with an increase in hospital stay and total hospitalisation costs.
While not statistically significant, delayed intervention beyond 48h among those aged 65 years and older resulted in increased mortality during admission, as well as a 10% increase in mortality at 1-year follow-up. We did not find a significant increase in other complications during patient follow-up. Previously published studies reinforce the importance of surgery in the first 48h, finding an increase in mortality in patients undergoing surgery late at one month, six months, and one year of follow-up, with mortality figures close to those described for hip fractures.22,23
The main limitation of our study is that it is retrospective, although the large sample size, and the similarity of the characteristics of our sample to previously published studies on the same pathology, increases its power. We cannot ignore the disparity in the surgical criteria of the different surgeons involved in the treatment of the patients in this study. The choice of different implants or techniques for similar fractures is a factor that is difficult to control within the sample. Similarly, the loss to follow-up of a high percentage of patients due to their death limits the power of the analysis of potential long-term complications. However, this loss of patients is similar to that of the literature consulted, being inherent to the progression of the condition itself. In any case, future studies with a higher level of evidence would be interesting to consolidate the conclusions reached in this study.
ConclusionsMinimally invasive techniques reduce hospital stay but not complications or long-term mortality. In people over 65 years of age, opening the fracture site was associated with an increased risk of infection during follow-up. All deaths in the study occurred in those over 65 years of age, with no differences between the different surgical techniques. A delay of more than 48 hours to surgery in those over 65 years of age increased mortality rates in hospital and during the first year of follow-up. High-energy trauma fractures had a higher proportion of complications during follow-up, especially delayed healing.
Level of evidenceLevel of evidence IIb.
Ethical considerationsThe present study was approved by the clinical research ethics committee (CEIC) of the hospital where it was conducted.
FundingNo external funding was received for this study.
Conflict of interestsThe authors have no conflict of interests to declare.