Pelvic ring tumours pose a challenge due to the difficulty in obtaining adequate surgical margins. Tools such as surgical navigation or 3D printing for the fabrication of patient-specific surgical positioning templates help in preoperative planning and intraoperative execution. Their correct positioning is essential in complex locations such as the pelvis, so it is necessary to identify positioning errors. The aim of this study is to demonstrate the reliability of 3D template placement for pelvic ring osteotomies.
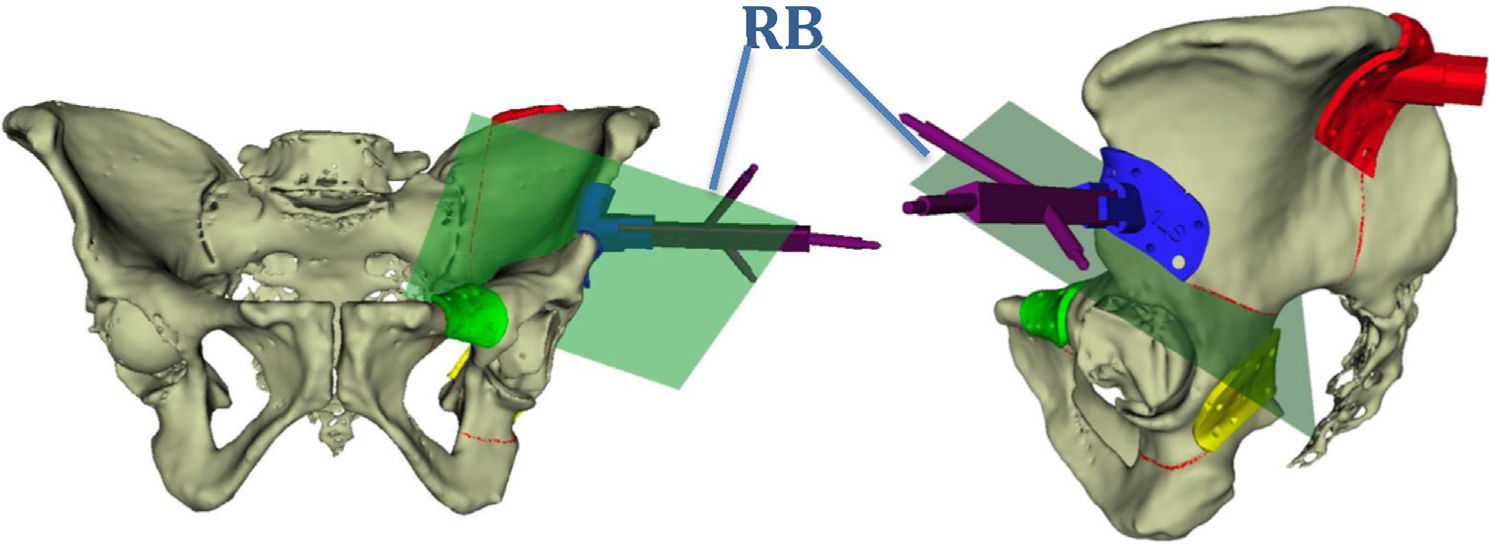
Material and methodsExperimental study in cadaver with 10 hemipelvis. CT was performed to obtain the three-dimensional model, planning of osteotomies, design of positioning templates in ischiopubic (I), iliopubic (P), supracetabular (S) and iliac crest (C) branches; and a positioning marker (rigid-body) on the C and S templates for navigation. The templates and rigid-body are 3D printed and positioned according to pre-planning. Navigation allows the final position of the inserts and osteotomies to be checked.
ResultsThe positioning of the templates with respect to the preoperative planning varied depending on the location, being greater the error in those of the iliac crest. Using navigation the mean error of distance to the cutting plane is 3.5mm, except in pubis (5–8mm), being conditioned by the position of the rigid body.
ConclusionThe use of patient-specific templates printed in 3D is a reliable tool for performing osteotomies in pelvic cancer surgery.
Los tumores del anillo pélvico suponen un reto por la dificultad de obtener márgenes quirúrgicos adecuados. Herramientas como la navegación quirúrgica o la impresión 3D para la fabricación de plantillas de posicionamiento quirúrgico paciente-específicas ayudan en la planificación preoperatoria y la ejecución intraoperatoria. Su correcta colocación es fundamental en localizaciones complejas como la pelvis, por lo que es necesario identificar los errores de posicionamiento. El objetivo de este estudio es demostrar la fiabilidad en la colocación de plantillas 3D para la realización de osteotomías en el anillo pélvico.
Material y métodosEstudio experimental en cadáver con 10 hemipelvis. Se realizó TC para la obtención del modelo tridimensional, planificación de osteotomías, diseño de plantillas de posicionamiento en rama isquiopubiana (I), iliopubiana (P), supracetabular (S) y cresta ilíaca (C) y se utilizó un marcador de posicionamiento (rigid-body) sobre las plantillas C y S para la navegación. Las plantillas y el rigid-body fueron impresos en 3D y se colocaron según la planificación previa. La navegación permitió comprobar la posición final de las plantillas y de las osteotomías.
ResultadosEl posicionamiento de las plantillas respecto a la planificación preoperatoria varió dependiendo de la localización; el error fue mayor en las de cresta ilíaca. Utilizando la navegación, la media de error de distancia al plano de corte estuvo en 3,5mm, excepto en el pubis (5-8mm), que está condicionado por la posición del rigid-body.
ConclusiónEl uso de plantillas paciente-específicas impresas en 3D es una herramienta fiable para las osteotomías en cirugía oncológica pélvica.
Pelvic ring tumours are rare but pose a major challenge from an oncological viewpoint. They are usually large-sized tumours when diagnosed due to delayed symptoms, and extensive resection is limited because of the anatomical features of this region,1 with difficulty in obtaining block resection with negative margins. For this reason, local recurrence continues to be a problem compared with that of extremities.2 In all of them the prognosis will be marked by the histological grade, the presence of metastasis on diagnosis and appropriate resection margins. Hence the importance of increasing accuracy when performing oncological resection.3
Extensive resection may cause major functional impairment both due to possible involvement of nerve roots and due to the proximity of the hip joint, which often needs to be reconstructed. Margins must therefore be adjusted to achieve adequate oncological resection aimed at preserving maximum functionality for the patient.4
Advances in imaging techniques and the development of navigation systems have facilitated preoperative planning and improved intraoperative accuracy of tumour resection.5,6 Other technological tools, such as 3D printing, allow the manufacture of patient-specific templates7 to guide the osteotomies to be performed and personalise them according to the patient and the tumour involvement present, as they are designed to adapt to a specific bone region. Although there are studies that defend the reliability of these patient-specific positioning templates,8 there are very few studies that study the positioning of the templates and the cutting planes with respect to preoperative planning.
The aim of this study is to demonstrate that the use of patient-specific templates obtained with a desktop 3-D printer is high reliable in terms of translating such planning into reality.
Material and methodsAn experimental study was designed in freeze-preserved cadavers, including 10 hemipelvises of both men and women and with size variability, in which the use of patient-specific templates using desktop 3D planning and printing systems was analysed. Firstly, a computed tomography of each specimen was performed to obtain the images.
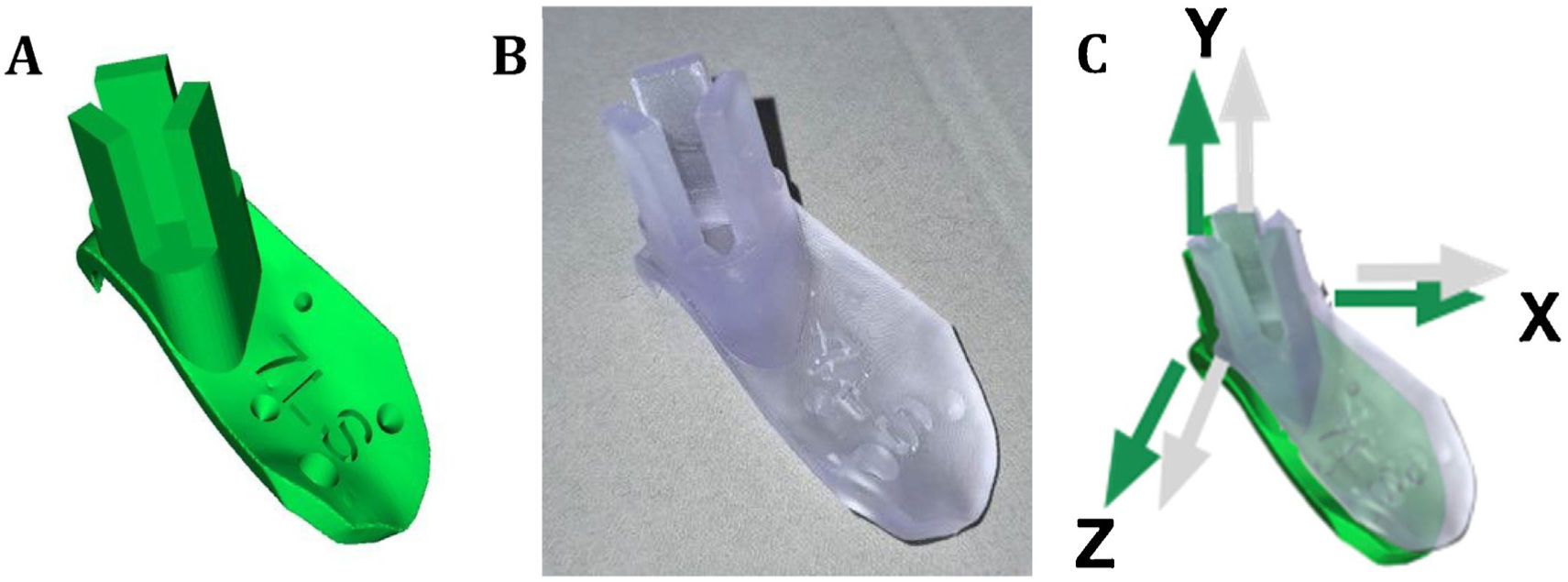
The processing and segmentation of the image studies is carried out with an open access programme (3D slicer) that allows a three-dimensional model to be obtained in stl format. For positioning template design another open access programme is used (Meshmixer, Autodesk), and after obtaining the three-dimensional mesh in stl format of each of the guides they are printed in biocompatible resin9 on a desktop 3D printer (FormLabs; Form 2) with working technology based on laser stereolithography. The planning of the osteotomy planes follows the classic osteotomy lines of the different types of internal hemipelvectomies I, II and III according to the classification of Enneking and Dunham10 (Fig. 1).
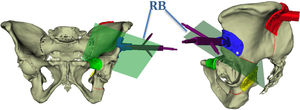
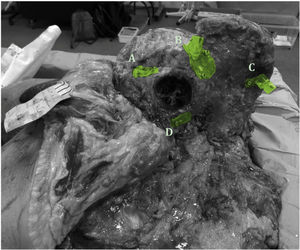
Using the same templates, a navigation system is developed through the use of rigid-body marking devices that serve to position the pelvis in space. Each guide is identified with a letter and a number to identify the specimen to which it corresponds and its location in the pelvis: S for the supracetabular guide, C for the iliac crest, P for the iliopubic branch and I for the ischiopubic branch. In addition, 4 reading points for navigation are placed in each of the guides and 2 holes for subsequent fixation to the bone by means of screws (Fig. 2).
When printing the orientation of the templates is taken into account to obtain a solid and non deformable guide on intervention.11 Double printing is made and a posterior process is made with a UV curing station to solidify them. They are then sterilised with ethylene oxide at 50° to reproduce the real conditions of intraoperative use.
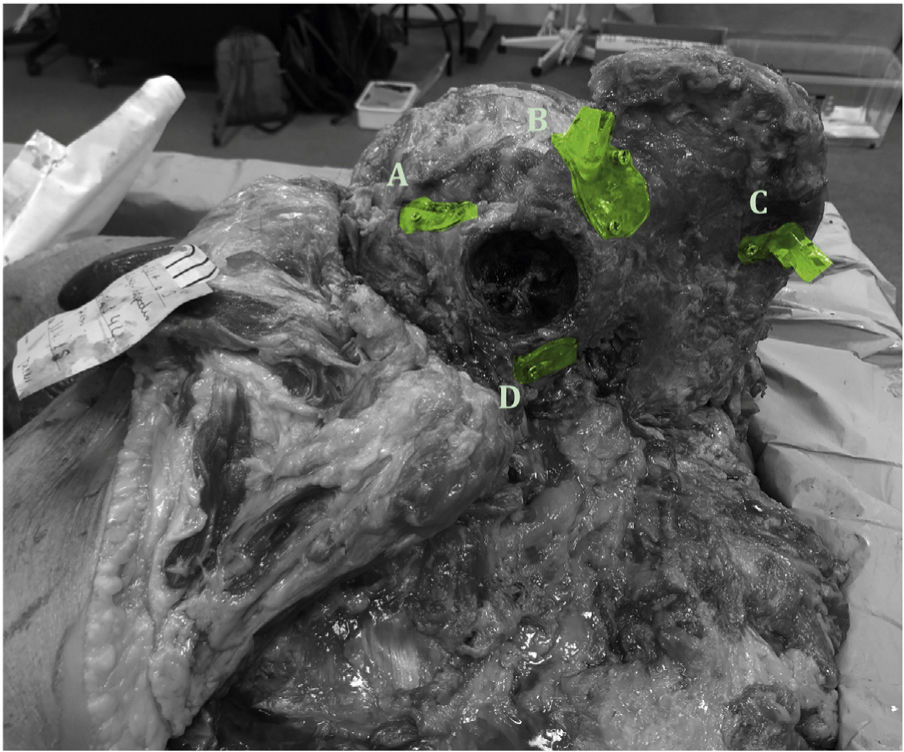
The pelvises are previously thawed in the dissection room and the usual approach is made for an internal hemipelvectomy, maintaining the structures to be preserved in vivo. Once the osteotomy areas are exposed at bone level, all the templates are placed and fixed with screws (Fig. 3). After placement, the individual incomplete osteotomies are performed so that a proper measurement can be taken later.
To check the position of the templates, a different navigation protocol is used depending on the rigid-body positioning. In hemipelvises 1–5 the rigid body was placed in the supracetabular template, while in hemipelvises 6–10 it was placed in the iliac crest template. In both cases, 4 points (cones) are picked up on the navigation guides to make the registration between virtual and real, as well as several points along the osteotomy performed (Fig. 4).
During planning a reference system is used based on the 3 specific space axes (x, y, z) for each hemipelvis. By superimposing the measurements obtained from the surgical navigation on this previous reference system, it is possible to measure the translations (distance) present in the 3 planes of space, in relation to the previous positioning of the templates for each hemipelvis (Fig. 2), as well as the possible errors of deviation along the entire osteotomy line.
To obtain the definitive results, the maximum osteotomy deviations are measured for each configuration, i.e., the maximum distance between the osteotomy that would be performed following the virtual planning and the osteotomy obtained in reality. With this reference, the mean and standard deviation values are obtained for each osteotomy plane for the different patient-specific guides.
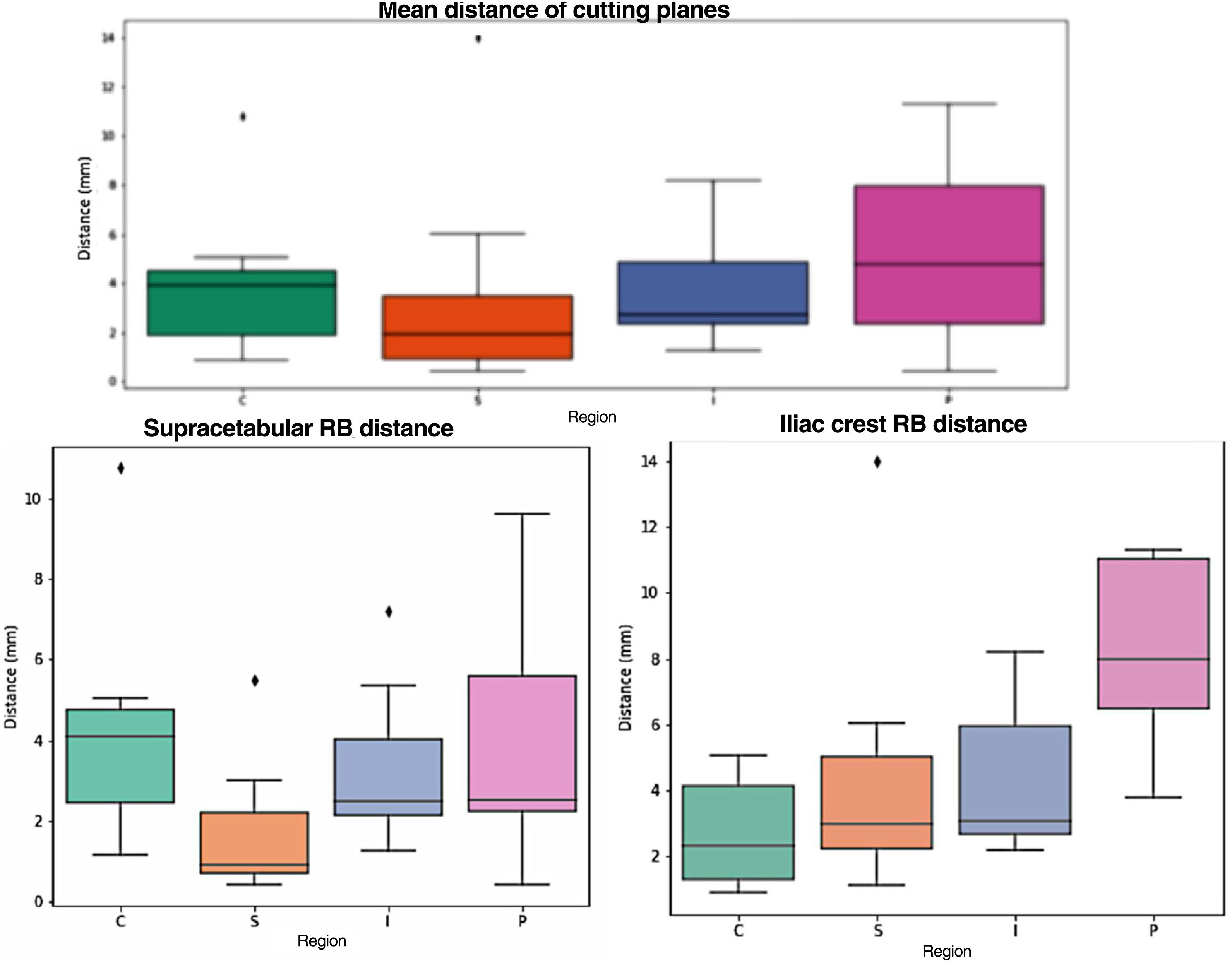
ResultsAfter comparative analysis of the position of the guides in the virtual model and in the real model a different mean distance error is obtained depending on where the guides are placed:
- •
Iliac crest guides: 7.2mm for the left and 4.8mm for the right.
- •
Supracetabular guides: 3.7mm for the left and 3.4mm for the right.
- •
Iliopubic branch guides: 3.8mm for the left and 3.06mm for the right.
- •
Ischiopubic branch guides: 4.7mm for the left and 3.04mm for the right.
With the exception of the guidewires placed in the iliac crest, which present more variability when adapting to the bony anatomy, in the rest of the locations the average placement error with respect to what was planned is less than 4mm, and 4.7mm in the case of the guidewires in the left ischiopubic branch.
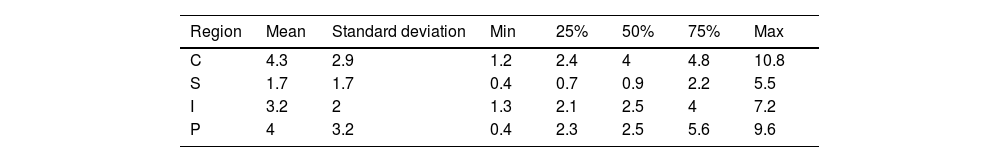
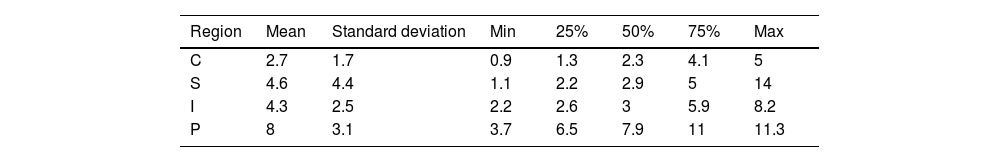
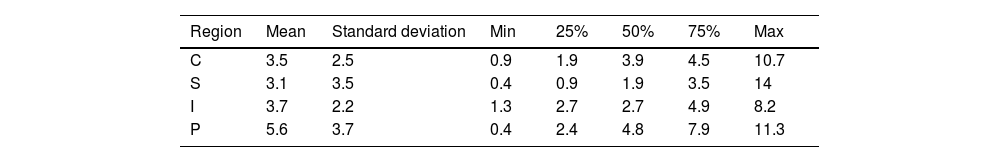
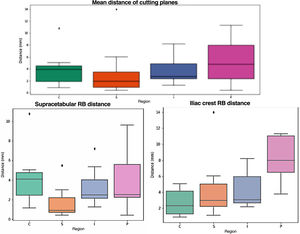
As for the navigation results (Fig. 5), the distance between the previously planned cutting plane and the osteotomy performed following the 3D templates and validated with navigation is analysed. The mean error is around 3.5mm, except in the pubis (5.6mm), with 75% of the cases showing errors below 5mm The standard deviation is around 3mm (Table 1). When analysing the results according to rigid body placement, when the rigid body was placed in the supracetabular position, the mean was <5mm in all cases (Table 2). In pelvises where the rigid body was placed in the iliac crest guide, navigation errors were <5mm in all regions except the pubic region, which had a mean error of 8mm (Table 3).
Top: Comparison between the planned osteotomy line (black line) and the minimum and maximum values for each guide; green: iliac crest; orange: supracetabular; blue: ischium; pink: pubis. Below left: comparative when rigid body is placed in the supracetabular (supracetabular) guidewire (iliac crest). Below right: rigid body placement in iliac crest guidance.
The particularities of the pelvic ring, as well as its anatomical relationships, allow the growth of large tumour masses before the patient is diagnosed, making any surgical procedure particularly difficult. Achieving tumour-free surgical margins should be a priority in pelvic oncological surgery, but even when performed by expert oncological surgeons, adequate margins are obtained in only 52% (CI: 37%–67%),1 making the treatment of malignant tumours of the pelvis one of the most difficult problems in musculoskeletal oncological surgery.12
In order to improve the precision of oncological resection, intraoperative navigation systems have been developed for pelvic bone tumour surgery.13 Patient-specific templates obtained by 3D printing have also been developed to perform the different osteotomies, improving surgical margins.14 This work provides an in-house and portable navigation system thanks to the use of patient-specific 3D printing tools that provide a margin of error of less than 5mm, improving precision and minimising possible calculation errors in comparison with those made following the present anatomical references.15
When analysing the results, the greatest variability is given by the guidewires located on the iliac crest, since due to its anatomy the guidewire can be adapted to various areas of the crest; hence the placement error is on average around 7mm In these cases, associating these guides with intraoperative navigation or establishing the distance to certain anatomical references such as the anterosuperior and posterosuperior iliac spines in prior planning could reduce placement errors and, therefore, precision when performing the osteotomy, which will have a direct influence on the resection margins.
With regard to the navigation system, it will be influenced by the position of the rigid body, since in the hemipelvises where the marker was placed on the iliac crest template, the error measured was greater the further away from the rigid body. When the marker was placed at the supracetabular level, the translation results of the actual versus planned osteotomy were <5mm
There are not many articles in the literature validating the accuracy of these patient-specific templates. Among these, Wong et al.16 also compared the accuracy of patient-specific templating and navigation in the treatment of periacetabular tumours compared to conventional techniques, using 12 surgical templates to obtain the results. Similarly, Sallent et al.8 obtained similar results in terms of accuracy below 5mm when using patient-specific templates, without using an associated navigation system.
The use of patient-specific guide in daily clinical practice can help us to improve the quality of oncological resection. Several authors have reported their experience in using navigation technology to resect bone tumours, and significant improvements in surgical margins can be observed. Jeys et al.17 demonstrated a significantly reduced local recurrence rate. In another study, Evrard et al.14 demonstrate a lower local recurrence rate in cases where 3D patient-specific guides were used to perform tumour resection.
As a limitation, this is a cadaver study, which does not exactly reproduce the real intraoperative conditions, although the same approach routes were used. Often pelvic tumours are associated with soft tissue masses that we cannot reproduce in the cadaver and that will condition both the resection and the possible placement of the guides. To improve precision in these cases, we can design the guides in the areas that will be accessible during surgery and combine them with navigation systems to perform the osteotomy with adequate resection margins.18
Another limitation is that the results of the positioning of the guides and osteotomies will be influenced by whether the rigid body is placed more centrally (supracetabular) or more peripherally (iliac crest).
ConclusionsThe use of patient-specific templates obtained by 3D printing is a useful and reliable tool for obtaining osteotomies in the desired cutting planes in pelvic oncological surgery.
By using optical navigation combined with cutting guides, we obtain osteotomy errors that are on average below 5mm In view of the results, when choosing where to place the rigid body, it is best to place it closest to the osteotomy level, as this increases the accuracy of the osteotomy.
By using desktop 3D printers and a portable navigation system, a more cost-effective and affordable system for performing pelvic osteotomies on tumours in this location with high accuracy of execution is developed.
Level of evidenceLevel of evidence III.
FundingFunding by the SECOT Foundation through the 2018 research initiation grant and the PI18/01625 project (Ministry of Science, Innovation and Universities, Instituto de Salud Carlos III, and European Regional Development Fund; A way of doing Europe).
Conflict of interestThe authors declare that they have no conflict of interest in the undertaking of this study.
Our thanks to Surgical Training and to the Universidad Cardenal Herrera of Madrid, without which we would not have been able to obtain specimens and carry out this study.