Achieving stability in total knee arthroplasty (TKA) is crucial for long-term implant survival. In cases of severe deformity or ligament laxity, constrained implants may be required. Traditionally, increasing constraint involved intramedullary stems. However, there are intermediary alternatives, including employing a constrained polyethylene insert without stems, thereby avoiding complications related to them. The study aims to evaluate our experience with a non-modular constrained (NMC) implant in primary TKA.
Material and methodsWe conducted a retrospective review of the clinical and radiographic outcomes of 108 non-stemmed primary TKAs performed at our institution between 2013 and 2021 in patients with at least 10° deformity or 10mm ligament laxity. Data included demographics, preoperative and postoperative deformities, clinical outcomes and revision rates.
ResultsA total of 103 patients (108 knees) with a mean age of 74 were followed up for a minimum of 2 years. The mean postoperative range of motion was 105°/0°. The median Oxford Knee Score, Knee Society Score and Knee Society Function Score were 43.5, 92 and 90, respectively. 17 knees had varus deformity (mean tibiofemoral angle of 2.7°), and 87 knees had excessive valgus deformity (mean tibiofemoral angle of 15.1°). The remaining 4 knees had a neutral alignment. The mean postoperative tibiofemoral angle was 6.8°. The overall revision rate was 6.5% (7 patients): 3 deep periprosthetic infections, 2 patellar dislocations, 1 stiffness and 1 aseptic loosening.
ConclusionOur experience demonstrates favorable mid-term outcomes with the NMC implant, providing a safe alternative to stemmed implants in primary TKA, particularly in cases of severe deformity or ligament laxity.
Alcanzar la estabilidad en la artroplastia total de rodilla (ATR) es esencial para lograr la supervivencia del implante a largo plazo. En casos de deformidad severa o laxitud ligamentosa, puede ser necesario el uso de implantes constreñidos. Tradicionalmente aumentar la constricción ha ido asociado con el uso de vástagos, sin embargo, hay opciones intermedias que evitan el uso de vástagos y, por tanto, las complicaciones asociadas a los mismos. El objetivo de este estudio es evaluar nuestra experiencia con un implante no modular constreñido (NMC) en ATR.
Material y métodosSe realizó un estudio retrospectivo de los resultados clínicos y radiológicos de 108 ATR constreñidas sin vástago implantadas en pacientes con más de 10° de deformidad o 10mm de laxitud ligamentosa, intervenidas en nuestro centro entre 2013 y 2021 en pacientes con. Se recogieron datos demográficos, radiológicos pre y posoperatorios, resultados clínicos y tasa de revisión y complicaciones.
ResultadosEn total se incluyeron 103 pacientes (108 rodillas) con una edad media de 74 con un seguimiento mínimo de dos años. La movilidad posoperatoria media fue de 105/0°. La mediana de la escala Oxford Knee Score, Knee Society Score y Knee Society Function Score fue de 43,5, 92 y 90, respectivamente. La deformidad preoperatoria fue genu varo en 17 rodillas (ángulo femorotibial medio de 2,7°) y genu valgo en 87 rodillas (ángulo femorotibial medio de 15,1°). Los cuatro restantes tenían un eje neutro. El ángulo femorotibial medio posoperatorio fue de 6,8°. La tasa de revisión global fue de 6,5% (siete pacientes): tres infecciones periprotésicas, dos luxaciones de patela, una rigidez y un aflojamiento aséptico.
ConclusiónNuestros resultados demuestran buenos resultados a mediano plazo con el implante NMC, configurándose como una alternativa segura al uso de implantes con vástago en ATR, especialmente en casos de deformidad severa o laxitud ligamentosa.
Total knee arthroplasty (TKA) is considered the gold standard for patients with end-stage knee osteoarthritis.1 The keys in order to obtain a successful outcome of TKA includes durable implant fixation, optimum alignment, balanced flexion and extension gaps and normal patellar tracking.2 Attaining stability during TKA is the cornerstone to achieve good long-term implant survival.3
It is unusual to use a more constrained prosthesis than a posterior cruciate retaining (CR) or posterior cruciate ligament stabilized (PS) in primary arthroplasty. However, there are certain clinical or adverse intraoperative situations, such as severe deformity, bone loss or collateral ligament laxity that are extremely difficult to correct with only soft tissue release. In these circumstances, additionally constrained prostheses may be required in order to obtain a stable balance postoperatively.1,4
In general, a constrained implant involves a thicker and wider post on the polyethylene insert, which conforms more intimately with the corresponding femoral box. While this design limits varus–valgus and torsional moments, thereby reducing instability, it may also induce larger bending and torsional stresses across the bone-implant interface and the underlying femoral and tibial bone.3 Repetitive stress in this region may lead to aseptic loosening. For this reason, increased constraint has been coupled with intramedullary stems, which dissipate forces away from the articular and metaphyseal bone, allowing load-sharing over the diaphyseal portion of the tibia and femur.5,6
There are some drawbacks to stem extensions, including leg and thigh pain near the tip of the stem, intraoperative fractures, embolization, increased costs, longer surgical times and greater difficulty in revision surgery.4 Therefore, alternative devices have been developed to offer an intermediary option, increasing constraint with a constrained polyethylene insert coupled with non-stemmed tibial and femoral components.
The Non-Modular Constrained implant (NMC, Exactech®, Gainesville, FL) incorporates a non-modular femoral component following the standard PS design, with a central box 2mm deeper standard protheses. The tibial component is modular with a 5cm stem and optional stem extension. The semi-constrained TKA system uses a tall tibial post that fits intimately into the femoral box, providing for ±1.5° varus/valgus and ±2° of rotational constraint. The post is reinforced by a screw to increase its bending resistance.2
The purpose of this study was to evaluate the clinical, functional and radiographic outcomes of our experience with the NMC prosthesis used in primary TKA, particularly in cases where moderate varus/valgus deformity or collateral ligament laxity were present.
Material and methodsWe conducted a retrospective review of a cohort of consecutive patients who underwent primary surgery and received NMC prostheses (non-modular femoral component, constrained polyethylene and variable tibial stem length) from the same manufacturer (Exactech®, Gainesville, FL) between 2013 and 2021 at our institution. The inclusion criteria comprised patients with knees exhibiting at least 10° varus/valgus deformity or 10mm collateral ligament laxity and a minimum follow-up of 2 years. The rationale for choosing this implant was to provide stability while avoiding the complications associated with a more constrained implant. Patients with less than 2 years of follow-up were excluded.
This study was conducted following the ethical standards outlined in the Helsinki Declaration and resolution 008430 of 1993, and it was approved by the Ethics Committee of our institution (internal approval code 23/813-E). Additionally, all patients included in this study were informed about it, and their consent to participate was obtained.
All surgical procedures were performed with patients under either general or regional anesthesia, using a straight skin incision and a standard medial parapatellar arthrotomy. A tourniquet was inflated at the beginning of the procedure and kept inflated until cementation. A standard distal femoral cut in 7° of valgus was made following intramedullary instrumentation. Distal femoral rotation was adjusted to be parallel to the epicondylar axis and externally rotated off the posterior condylar axis by 3°. The articular surface of the tibia was resected orthogonally to its mechanical axis with a 3° posterior slope, using either an intramedullary or extramedullary guide based on the surgeon's preference. Tibial stems were consistently used, with size determined subjectively based on the surgeon's perception of soft tissue instability. Patellar resurfacing was performed in all patients and all implants were cemented. Patella tracking was assessed intraoperatively, and lateral retinacular release was performed if necessary.
Preoperative data, including demographic information such as age, sex, side of surgery and American Society of Anesthesiology (ASA) score were retrospectively collected from the hospital database. Operative times, component sizes, complications and length of hospital stay were also documented. Clinical outcomes, such us range of motion (ROM), pain, stability, the Knee Society Score (KSS), Knee Society Function Score (KFS) and the Oxford Knee Score (OKS) were assessed postoperatively at each visit. Radiographic follow-up included standing anteroposterior and lateral radiographs. The most recent postoperative X-rays were compared with prior radiographs to evaluate mechanical and anatomical alignment, presence of aseptic loosening, radiolucent lines and osteolysis.
Continuous data were summarized as mean and standard deviation, while categorical data were expressed as frequencies and percentages. The statistical analysis included Kaplan–Meier survivorship analysis of all knees, with failure defined as the removal of the implant for any reason. The statistical significance level was set at 0.05 for all comparisons. All statistical analyses were conducted using SPSS software.
The authors, or their immediate families, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article.
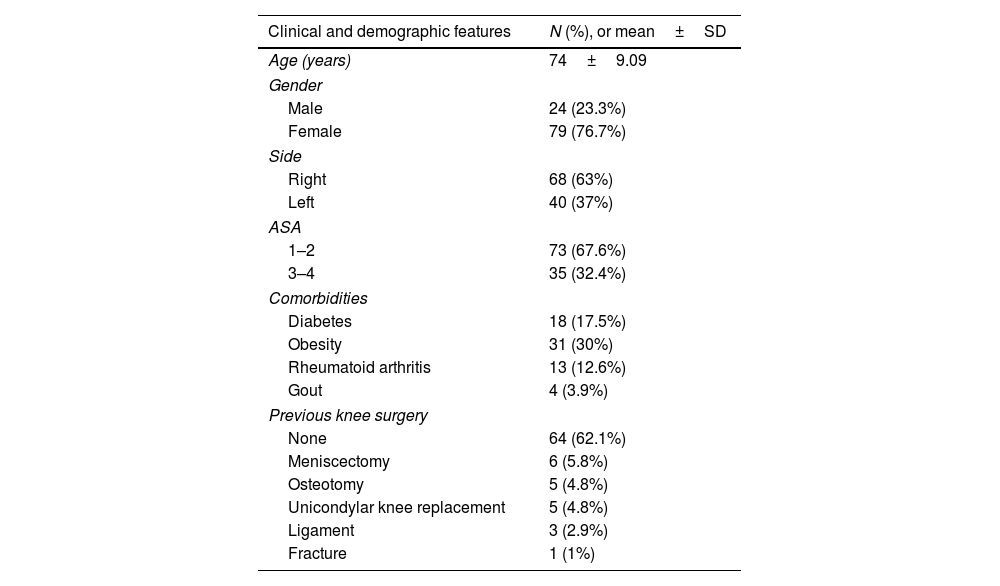
ResultsOur study cohort included 108 NMC (Exactech®, Gainesville, FL) primary knees in 103 patients, with 80 being female. The average age at surgery was 74 years (range, 66–79 years). Follow-up duration ranged between two and ten years, with an average of six years. Clinical and demographic features are summarized in Table 1.
Preoperative patients characteristics.
| Clinical and demographic features | N (%), or mean±SD |
|---|---|
| Age (years) | 74±9.09 |
| Gender | |
| Male | 24 (23.3%) |
| Female | 79 (76.7%) |
| Side | |
| Right | 68 (63%) |
| Left | 40 (37%) |
| ASA | |
| 1–2 | 73 (67.6%) |
| 3–4 | 35 (32.4%) |
| Comorbidities | |
| Diabetes | 18 (17.5%) |
| Obesity | 31 (30%) |
| Rheumatoid arthritis | 13 (12.6%) |
| Gout | 4 (3.9%) |
| Previous knee surgery | |
| None | 64 (62.1%) |
| Meniscectomy | 6 (5.8%) |
| Osteotomy | 5 (4.8%) |
| Unicondylar knee replacement | 5 (4.8%) |
| Ligament | 3 (2.9%) |
| Fracture | 1 (1%) |
N, sample size; SD, standard deviation.
The mean operative time was 110min (range, 90–115min), and the mean tourniquet time was 90min (range, 75–100min). 72 patients (66.7%) had 10° varus or valgus deformity or more and 36 (33.3%) had collateral ligament laxity. The size of tibial stems was determined based on the surgeon's perception of soft tissue instability (25mm in 4.7%, 40mm in 40.2%, 80mm in 52.3% and 120mm in 2.8%). To address bone loss, tibial augments were required in 8 knees (7.5%). The mean duration of hospitalization after surgery was 7 days (range, 6–9 days).
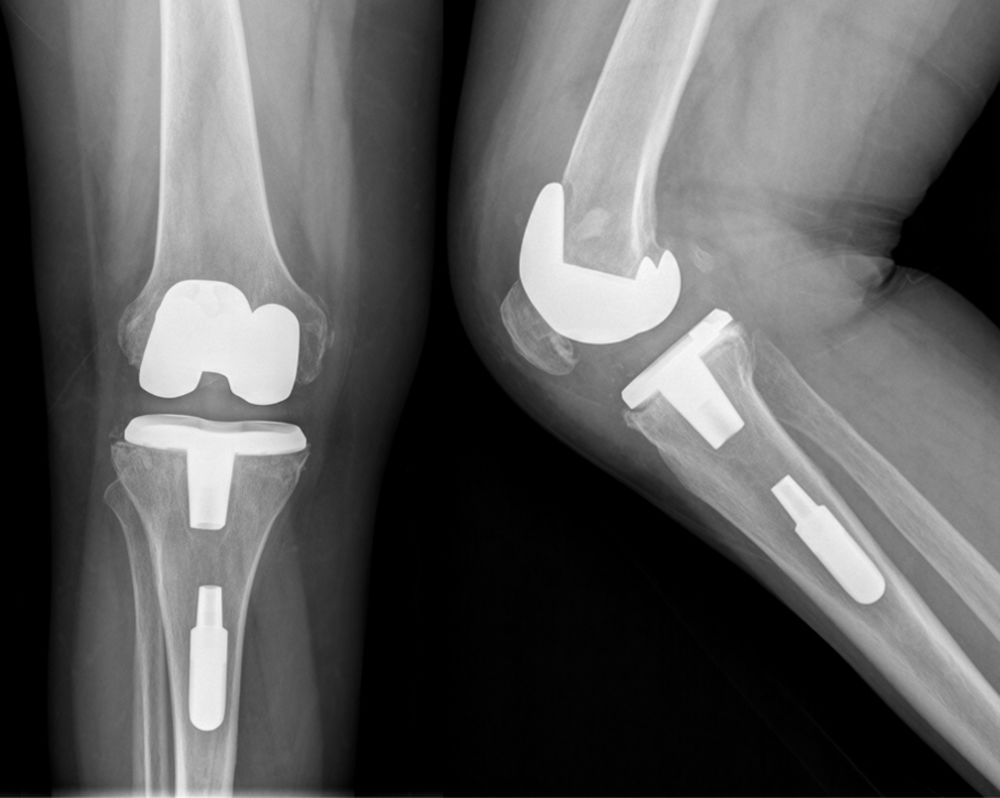
Five cases (4.6%) of intraoperative complications were reported: 1 inadvertent lateral collateral ligament rupture, 1 tibial plateau fracture, 1 tibial tubercle fracture and 2 cases in which it was not possible to adequately screw the stem to the polyethylene, leaving the stem inside the canal with no connection to the prostheses (Fig. 1).
At the final follow-up, the mean ROM was 105/0°, with only 15 patients (13.8%) exhibiting an extension lag. The median OKS, KSS and KFS were 43.5/48 (interquartile range, 34.7–47), 92/100 (interquartile range, 81–97) and 90/100 (interquartile range, 70–100), respectively. Moreover, patients reported a high level of satisfaction at the final follow-up, with 85.7% of them expressing that they would choose to undergo the same surgery again. Complete clinical results and patient-reported outcomes can be found in Table 2.
Clinical results and patient reported outcomes.
| Outcome measure | % or median (IQR) |
|---|---|
| Pain | |
| None | 65.79% |
| Mild (only stairs) | 14.47% |
| Mild (always) | 13.16% |
| Moderate (occasional) | 6.58% |
| Walking | |
| Unlimited | 60.53% |
| 30–60min | 31.58% |
| <30min | 5.26% |
| Housebound | 2.63% |
| Stairs | |
| Normal up and down | 44.74% |
| Normal up; down with rail | 27.63% |
| Up and down with rail | 23.68% |
| Unable | 3.95% |
| Walking aids used | |
| None used | 57.89% |
| Use of cane | 27.63% |
| Two canes/sticks | 2.63% |
| Crutches or frame | 11.84% |
| KSS knee | 92 (81–97) |
| KSS function | 90 (70–100) |
| OKS | 43.5 (34.75–47) |
%, percentage; IQR, interquartile range.
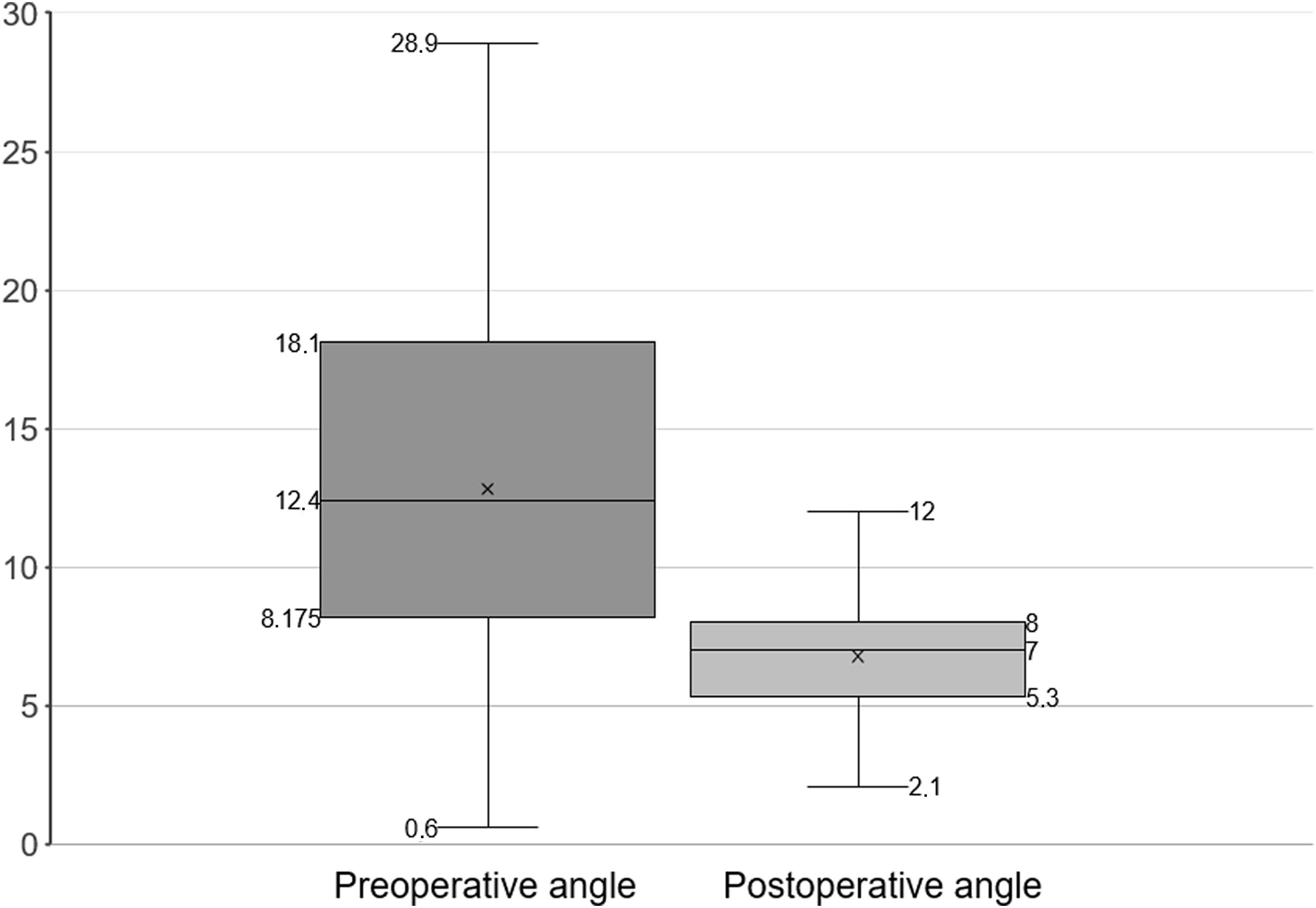
Preoperative radiographs revealed varus deformity in 17 knees (15.7%) with a mean tibiofemoral angle of 2.7° (SD 1.1) and excessive valgus deformity in 87 knees (80.6%) with a mean tibiofemoral angle of 15.1° (SD 5.3). The remaining 4 knees were neutral (5–7° of tibiofemoral angle). The mean postoperative tibiofemoral alignment was 6.8° (SD 1.9). The distribution of tibiofemoral angle values before TKA and at the last follow-up is shown in Fig. 2. Furthermore, radiolucent lines were present in 18 (16.7%) and osteolysis was observed in 16 (14.8%) patients.
During follow-up, 7 patients (6.5%) required revision of one or more components: 3 for deep periprosthetic infection (2.8%), 2 for dislocation of patellar component (1.8%), 1 for stiffness (0.9%) and 1 for aseptic loosening (0.9%). The average time to reoperation was 1.5 years (interquartile range, 0.6–2.6).
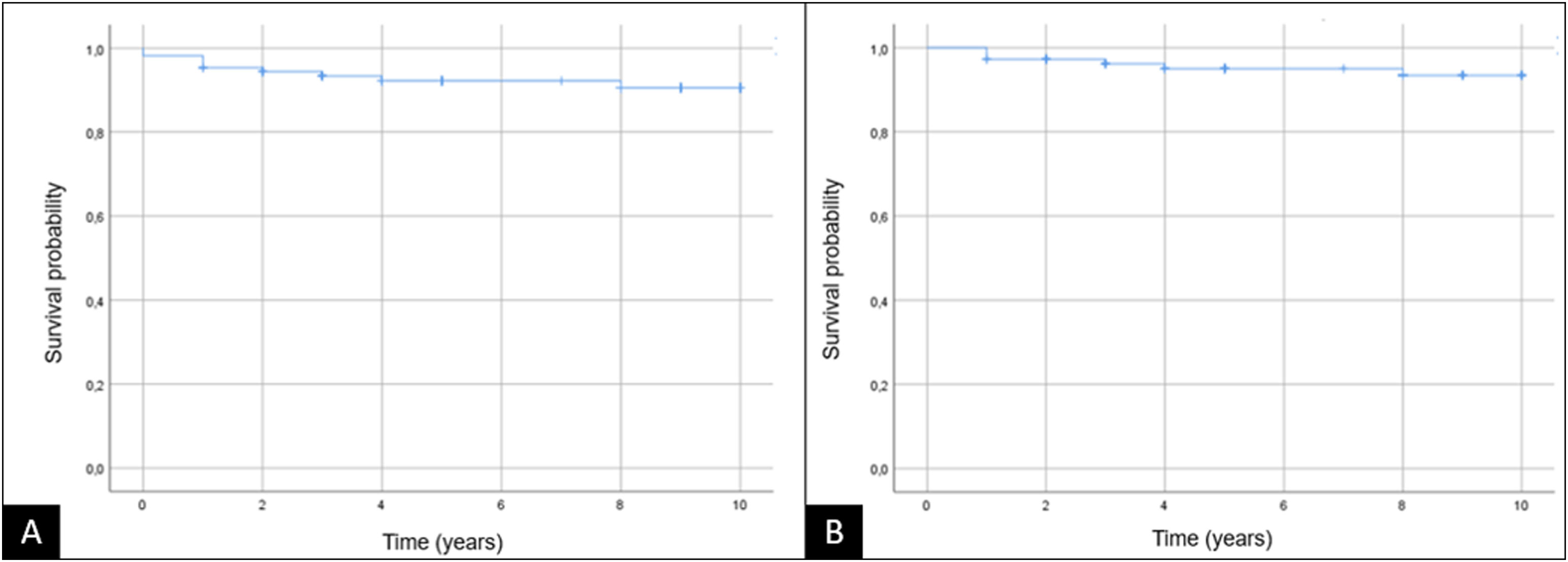
The five-year survival rate, with revision for any reason as the endpoint was 92.2%. When using revision for aseptic loosening as the endpoint, the five-year survival rate was 95% (Fig. 3).
DiscussionCurrently, instability after primary TKA is a major cause of revision, accounting for up to 21% of indications at 2 years and 27% at 5 years.1 There are situations where traditional soft tissue balancing techniques alone may be insufficient to achieve a well-balanced and stable knee, especially in cases of significant angular deformities or incompetent collateral ligaments. In such situations, more constrained implants might be necessary to achieve knee stability.1,4 Generally, increasing constraint in TKA involves a larger tibial post with a deep femoral box to provide anterior-posterior, medial-lateral and rotational stabilization.3
Despite the increased stability, constraint implants have some theoretical disadvantages. First, since constraint implants limit internal and external rotation and coronal plane mobility, there is concern about potential restriction in ROM. However, several studies have described comparable ROM and functional outcomes in both primary PS-TKA and primary constrained stemless TKA. Deshmukh et al.7 and Dayan et al.8 retrospectively compared postoperative ROM, pain and function in 486 (244 PS-TKA versus 242 CCK-TKA) and 404 knees (163 PS-TKA versus 241 CCK-TKA) respectively, and found no significant differences between PS-TKA and CCK-TKA in terms of ROM, pain and function. Additionally, in a recent systematic review, Mancino et al.1 reported that ROM, clinical and functional outcomes in patients receiving primary constrained implants are comparable to those with non-constrained PS implants. This study reported postoperative range of motion ranging from 60° to 130° (average 105.6°) and postoperative KSS and KFS ranging from 40 to 100 (average 84) and 0 to 100 (average 64.8), respectively. Our clinical results are comparable to these studies, suggesting that the use of a stemless constrained prosthesis, if necessary, would not be detrimental to the patient.
Traditionally, constrained implants have been used in conjunction with intramedullary stems to allow load-sharing over the diaphysis of the tibia and femur. However, there are potential disadvantages to using stem extensions, including leg and tight pain, increased bone loss, reaming of canals and possible embolization, difficulty of removal and more challenging surgery at revision, increased costs, longer operative time and potentially an increased risk of periprosthetic infection.4
Recently, some devices have been designed to allow the use of a constrained polyethylene insert without the need for stems. Moussa et al.3 compared revision rates of 871 primary constrained TKAs with 817 primary PS TKAs at 4.5 years of follow-up and reported a 6-fold greater revision rate for mechanical failure in the constrained group. Similarly, Pitta et al.,9 in a prospective TKA registry, found that the failure rate was up to 2-fold greater in patients with constrained implants. These results are believed to be related to the use of stemless non-modular first-generation implants.1 Additionally, Nam et al.6 compared 190 stemless NMC implants and 140 PS implants, reporting similar failure rates (4.2% and 4.3%) at 7 and 6 years follow-up, respectively. Interestingly, the main cause of revision in the NMC group was femoral component loosening while in the PS group, it was instability. Additionally, some studies described lower rates of aseptic loosening in stemless constrained implants: Anderson et al.10 and Ruel et al.11 reported revision rates for aseptic loosening of 0.5% and 3.8%, respectively. Our study retrospectively reviewed 108 stemless constrained implants, reporting a very low rate of loosening (0.97%, 1 knee). These findings support the use of stemless constrained implants, thus avoiding the potential drawbacks of stem extensions.
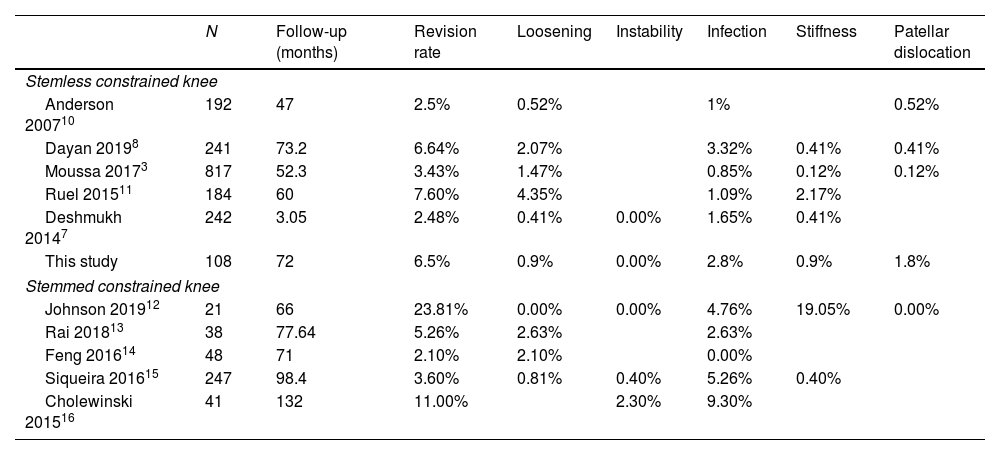
In this paper, the overall revision rate was 6.5%, which is consistent with previous studies involving similar prostheses and indications (Table 3). Additionally, the current study did not show a significantly higher loosening rate compared to literature results of stemmed implants (Table 3).
Case series previously reported.
| N | Follow-up (months) | Revision rate | Loosening | Instability | Infection | Stiffness | Patellar dislocation | |
|---|---|---|---|---|---|---|---|---|
| Stemless constrained knee | ||||||||
| Anderson 200710 | 192 | 47 | 2.5% | 0.52% | 1% | 0.52% | ||
| Dayan 20198 | 241 | 73.2 | 6.64% | 2.07% | 3.32% | 0.41% | 0.41% | |
| Moussa 20173 | 817 | 52.3 | 3.43% | 1.47% | 0.85% | 0.12% | 0.12% | |
| Ruel 201511 | 184 | 60 | 7.60% | 4.35% | 1.09% | 2.17% | ||
| Deshmukh 20147 | 242 | 3.05 | 2.48% | 0.41% | 0.00% | 1.65% | 0.41% | |
| This study | 108 | 72 | 6.5% | 0.9% | 0.00% | 2.8% | 0.9% | 1.8% |
| Stemmed constrained knee | ||||||||
| Johnson 201912 | 21 | 66 | 23.81% | 0.00% | 0.00% | 4.76% | 19.05% | 0.00% |
| Rai 201813 | 38 | 77.64 | 5.26% | 2.63% | 2.63% | |||
| Feng 201614 | 48 | 71 | 2.10% | 2.10% | 0.00% | |||
| Siqueira 201615 | 247 | 98.4 | 3.60% | 0.81% | 0.40% | 5.26% | 0.40% | |
| Cholewinski 201516 | 41 | 132 | 11.00% | 2.30% | 9.30% | |||
We found a 5-year follow-up survival rate of 92.2% when revision for any reason was set as the endpoint and 95% when aseptic loosening was set as the endpoint. Our results were comparable with another cohort reported by Ruel et al.11 where they noted a 96.7% survival rate at 5-years follow-up when aseptic loosening was set as the endpoint (Fig. 3).
We are aware of the fact that our study has several limitations. Firstly, it is a retrospective study conducted at a single institution by multiple surgeons. Secondly, the decision to implant a NMC prosthesis rather than another implant and the choice of tibial stem size were based on the surgeon's subjective assessment. Additionally, the study lacked a matched group and involves only the NMC implant. Finally, although clinical outcomes were reported, preoperative clinical data were not routinely collected.
ConclusionOur experience demonstrates favorable mid-term clinical and radiographic outcomes following primary NMC TKA in patients with severe valgus deformity and/or incompetent collateral ligaments. We believe that NMC TKA is a reliable option for providing sufficient stability, correcting deformities, achieving a high rate of success and survivorship and maintaining a low rate of loosening. Therefore, it should be considered as an alternative in cases of complex primary TKA, thereby avoiding the use of stems and its complications.
Level of evidenceLevel of evidence iii.
Ethical considerationThis study has the approval of the Ethics and Research Committee of the Clínico San Carlos Hospital (23/813-E). Informed consent was obtained from all individual participants or their relatives included in the study.
FundingThe authors declare that no funds, grants or other support were received during the preparation of this manuscript.
Conflict of interestNone.