Retrospective review of long term biphosphonates treated patients who sustained a subtrochanteric or diaphyseal femoral fracture with an atypical pattern. A literature review is presented as an update of the topic.
Material and methodsA retrospective study was conducted on 13 subtrochanteric or diaphyseal fractures in female patients treated with biphosphonates at our institution from September 2007 to March 2011.
ResultsFour cases of subtrochanteric fractures and 13 diaphyseal fractures were detected. Four patients had bilateral fractures. All cases but one (that affected only the lateral cortex) were complete fractures. Surgically, these kinds of fractures are demanding due to the hardness of the bones.
DiscussionIt is difficult to know if there is any relationship between bisphosphonates treatment and atypical femoral fractures. Nevertheless, current literature supports a greater benefit of their use in preventing vertebral and non-vertebral fractures. For this reason, biphosphonates continue being considered as a first choice in the prevention of osteoporotic fractures.
ConclusionsPatients on long-term treatment with bisphosphonates may present atypical femoral fractures as a complication. It is considered that the maximum period for biphosphonates treatment should not exceed 5 years.
Realizamos una revisión retrospectiva de los pacientes en tratamiento de forma prolongada con bifosfonatos que presentaron fracturas subtrocantéreas y diafisarias de fémur de patrón atípico. Revisión de la literatura existente con el fin de realizar una actualización del tema con consideraciones de interés para el cirujano ortopeda y traumatólogo.
Material y métodosRevisión de 13 pacientes en tratamiento con bifosfonatos con fracturas subtrocantéreas y diafisarias de fémur tratadas en nuestro centro entre septiembre de 2007 y marzo de 2011.
ResultadosSe detectaron 4 casos de fracturas subtrocantéreas y 13 de fracturas diafisarias. Cuatro pacientes presentaron fracturas bilaterales. Todas las fracturas eran completas salvo un caso en el que era incompleta con afectación de la cortical lateral. La intervención quirúrgica fue más demandante técnicamente por encontrarse un hueso pétreo como consecuencia de la medicación con bifosfonatos.
DiscusiónExiste la dificultad de establecer la relación causal directa entre el tratamiento prolongado con bifosfonatos y las fracturas atípicas femorales. No obstante, la literatura actual refiere un beneficio superior en la prevención de fracturas vertebrales y no vertebrales y, por tanto, se continua considerando a los bifosfonatos como un fármaco de primera elección en la prevención de las fracturas osteoporóticas.
ConclusionesLos pacientes con tratamiento prolongado con bifosfonatos pueden presentar fracturas atípicas femorales como complicación. Se considera que debe evaluarse en un periodo medio menor a 5 años la sustitución parcial o definitiva por otro fármaco, teniendo en cuenta el riesgo residual de fractura estimado en ese momento.
Bisphosphonates represent the first choice in the treatment of osteoporosis.1 They exert their therapeutic action by reducing bone resorption, thus allowing a decrease in bone remodelling and improving bone structures and properties and thereby reducing the risk of fractures.2 The level of reduction in bone replacement and the appropriate duration of bisphosphonate treatment has been the subject of numerous studies.3 Response to the treatment should be evaluated by densitometry every 2–3 years. There is no general agreement on the optimal duration of treatment, although a mean duration of 5 years is suggested. After this period it is necessary to assess the continuation of treatment, its temporary or permanent suspension or switching to another drug, taking into account the estimated residual risk of fracture at that point in time.4
Multiple cases5–13 and series14–19 of atypical femoral fractures associated with long-term bisphosphonate treatment have been published in recent years. The first cases were reported in 2005 and were described as atypical due to the type of pattern which they presented.20 Since then, given the considerable interest and alarm generated by such fractures, the literature contains series of up to 141 cases with radiological criteria pointing to atypical fractures.6 The present journal has published a series of 4 clinical cases.13 Various studies have pointed to the possibility that an excessive decrease in bone resorption and its remodelling capacity for a prolonged period of time could result in an accumulation of microtraumas. These would not be resolved satisfactorily and would result in increased bone fragility, eventually leading to atypical fractures of the femur, both diaphyseal and subtrochanteric, caused by stress without a previous triggering trauma.21,22
The aim of this work is, on the one hand, to present a descriptive study of a series of clinical cases related to the administration of these drugs evaluating the fracture pattern, coexisting risk factors and consolidation time thereof, and on the other hand, to conduct a review of the existing literature in order to assess the current situation on this subject, with considerations for trauma surgeons and orthopaedists.
Material and methodsThis was a descriptive study of 17 cases of atypical, subtrochanteric or diaphyseal fractures of the femur, treated at our hospital between September 2007 and March 2011, among patients in continuous treatment with bisphosphonates who were reviewed retrospectively. For their selection, we reviewed the cases of subtrochanteric and diaphyseal fractures of the femur treated at our centre during this period of time. Fractures were defined as subtrochanteric when they affected the region between 3cm distal to the lesser trochanter.
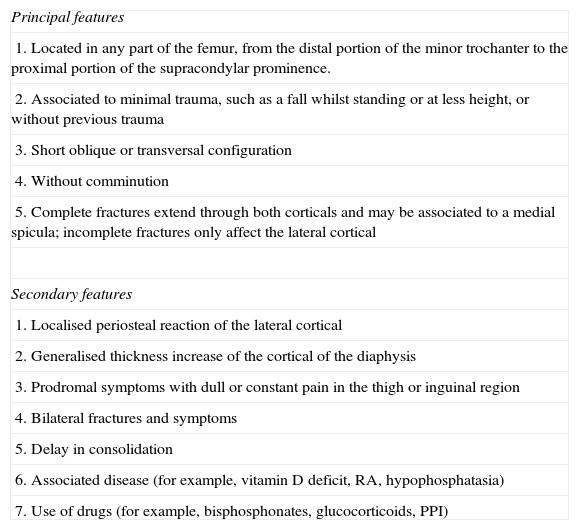
Radiographic studies of the hip and femur were conducted on all patients in order to define the fracture pattern. We searched for previous radiographs of the lower limbs conducted due to prodromal symptoms or for some other reason, in order to detect the presence of radiographic variables such as cortical thickening prior to the fracture. We evaluated the presence of primary and secondary variables described for atypical fractures (Table 1).4 We considered as atypical and, therefore, included in the series, those that met all the primary variables defined.
ASBMR criteria for the diagnosis of atypical femoral fractures.3
| Principal features |
| 1. Located in any part of the femur, from the distal portion of the minor trochanter to the proximal portion of the supracondylar prominence. |
| 2. Associated to minimal trauma, such as a fall whilst standing or at less height, or without previous trauma |
| 3. Short oblique or transversal configuration |
| 4. Without comminution |
| 5. Complete fractures extend through both corticals and may be associated to a medial spicula; incomplete fractures only affect the lateral cortical |
| Secondary features |
| 1. Localised periosteal reaction of the lateral cortical |
| 2. Generalised thickness increase of the cortical of the diaphysis |
| 3. Prodromal symptoms with dull or constant pain in the thigh or inguinal region |
| 4. Bilateral fractures and symptoms |
| 5. Delay in consolidation |
| 6. Associated disease (for example, vitamin D deficit, RA, hypophosphatasia) |
| 7. Use of drugs (for example, bisphosphonates, glucocorticoids, PPI) |
PPI: proton pump inhibitors; RA: rheumatoid arthritis.
The causative mechanism of the fracture and the presence or absence of prodromal pain were reviewed for all cases upon registration. We only included low-energy or atraumatic fractures. We recorded any medication being taken at the time and any which had been taken within a minimum of 5 years earlier, particularly seeking other drugs related to bone remodelling alterations (glucocorticoids and proton pump inhibitors). We recorded the type of bisphosphonate, duration of treatment and medical history, especially if patients suffered vitamin D deficiency, hypophosphatasia and hypoparathyroidism, which represented exclusion criteria for our study.
We identified a total of 13 female patients who met these criteria. Of these, 4 suffered bilateral, diaphyseal fracture of the femur. All had been diagnosed with osteoporosis and were following treatment with bisphosphonates at the time of the fracture.
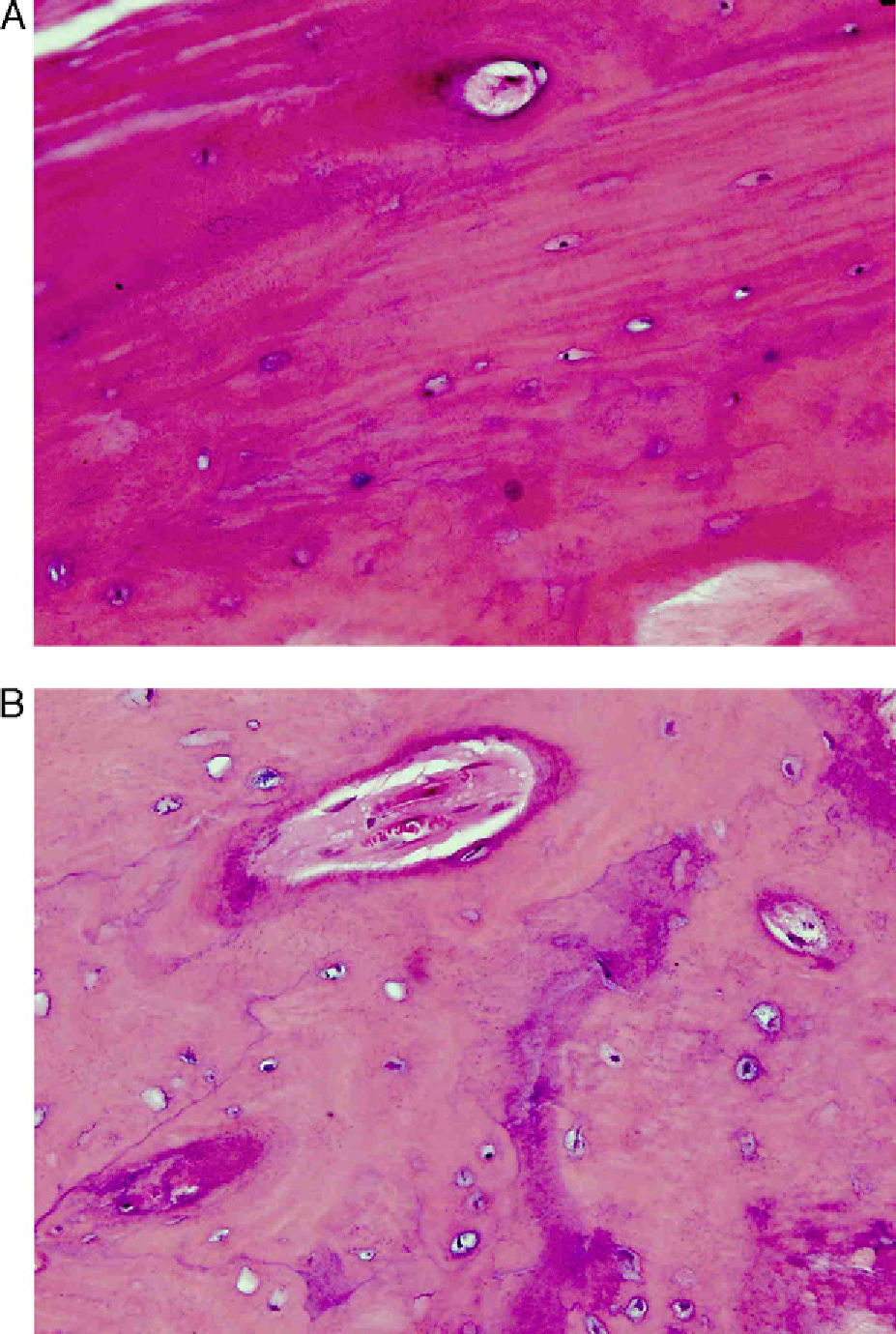
In some cases (3 of the total) we conducted an analytical study upon admission. This study included a thyroid profile, calcium-phosphorus balance and tumour markers, in order to rule out other possible causes of subtrochanteric or diaphyseal fractures of the femur without low-energy or any previous trauma. These cases were detected by the authors at the time of admission, rather than during the retrospective review. An analytical study for the differential diagnosis of secondary osteoporosis and other metabolic conditions was not part of the protocol at our centre, and was only performed in cases of clinical or radiological suspicion. In some of these cases detected from the start we also performed an intraoperative biopsy of the fracture foci. A sample of material was obtained during the drilling of the channel for the subsequent introduction of intramedullary nails (5 cases). These samples underwent haematoxylin–eosin staining. The fact that biopsies and analytical studies were only obtained in cases identified from the start could represent a limitation of our study.
We noted the fixation system used. Moreover, we also reviewed the consolidation time of fractures, a point of interest in the reviews within the existing literature. Nevertheless, some patients had less than 6 month follow-up at the time of writing this article, which could represent a limitation of the study.
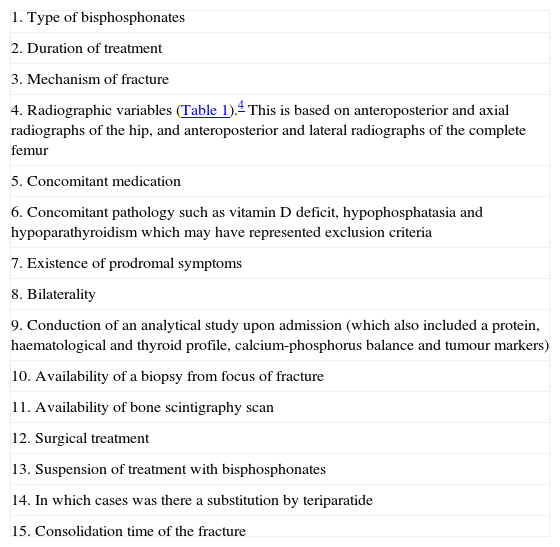
Other variables considered were the suspension or not of bisphosphonate treatment, and whether some other alternative medication for osteoporosis had been prescribed. Table 2 summarises the variables reviewed in each case of the series.
Variables reviewed in each case of atypical fracture.
| 1. Type of bisphosphonates |
| 2. Duration of treatment |
| 3. Mechanism of fracture |
| 4. Radiographic variables (Table 1).4 This is based on anteroposterior and axial radiographs of the hip, and anteroposterior and lateral radiographs of the complete femur |
| 5. Concomitant medication |
| 6. Concomitant pathology such as vitamin D deficit, hypophosphatasia and hypoparathyroidism which may have represented exclusion criteria |
| 7. Existence of prodromal symptoms |
| 8. Bilaterality |
| 9. Conduction of an analytical study upon admission (which also included a protein, haematological and thyroid profile, calcium-phosphorus balance and tumour markers) |
| 10. Availability of a biopsy from focus of fracture |
| 11. Availability of bone scintigraphy scan |
| 12. Surgical treatment |
| 13. Suspension of treatment with bisphosphonates |
| 14. In which cases was there a substitution by teriparatide |
| 15. Consolidation time of the fracture |
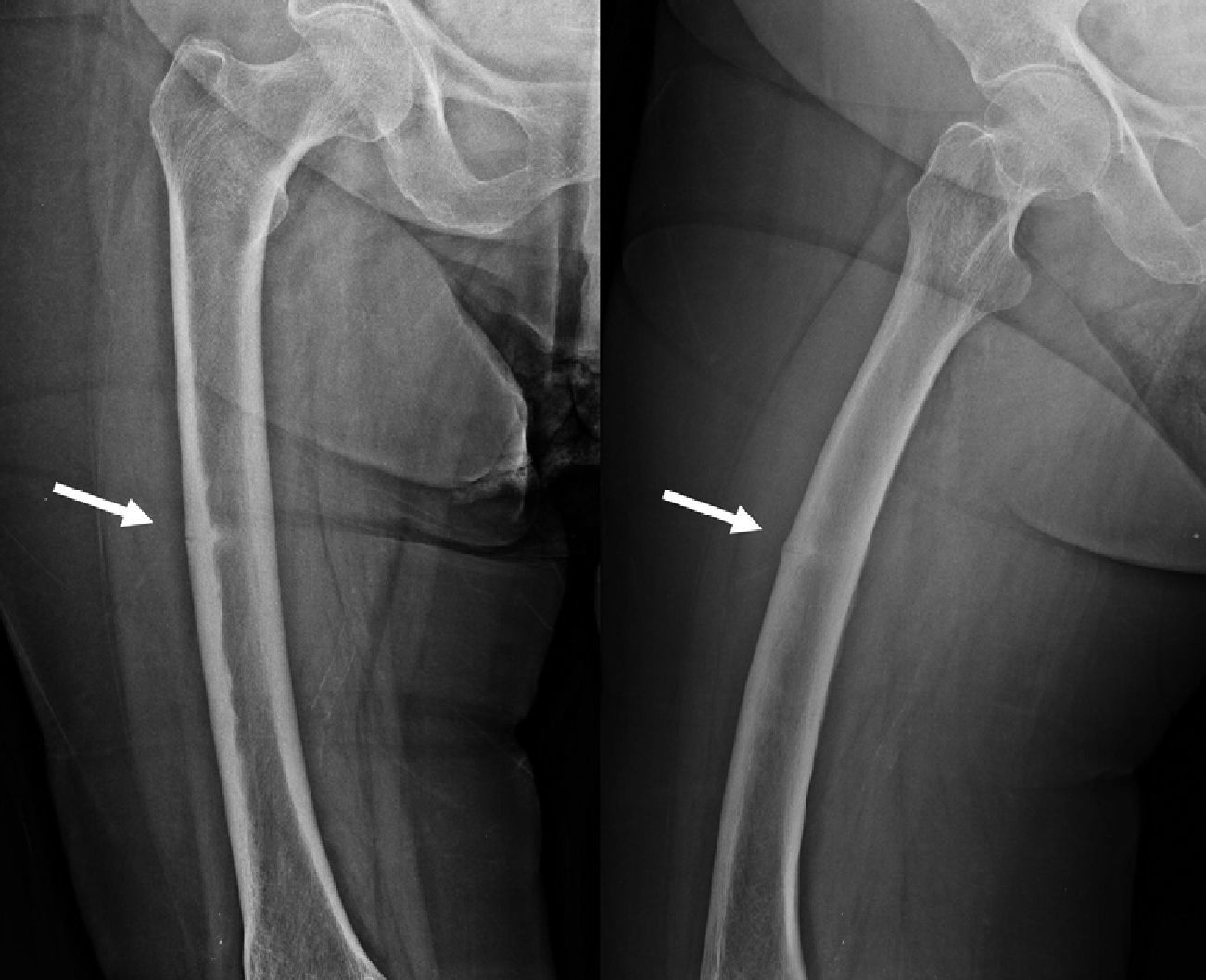
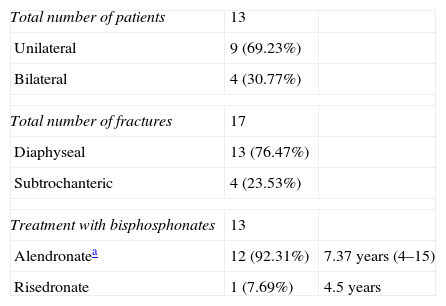
We identified a total of 13 patients with atypical fractures. Of these, 9 cases presented unilateral femoral fracture (30.77%) and 4 cases were bilateral (69.23%). In 1 case, the bilateral fracture occurred simultaneously, whilst in the other 3 bilateral cases the mean time between both fractures was 10 months (range: 0–24 months). Therefore, our series consisted of 17 fractures with atypical patterns, of which 4 were subtrochanteric (23.53%) (Fig. 1) and 13 were diaphyseal (76.47%) (Fig. 2) (Table 3). The mechanism of the fractures was an accidental fall from own height in all cases except for 2, in which no previous trauma was reported.
Results.
| Total number of patients | 13 | |
| Unilateral | 9 (69.23%) | |
| Bilateral | 4 (30.77%) | |
| Total number of fractures | 17 | |
| Diaphyseal | 13 (76.47%) | |
| Subtrochanteric | 4 (23.53%) | |
| Treatment with bisphosphonates | 13 | |
| Alendronatea | 12 (92.31%) | 7.37 years (4–15) |
| Risedronate | 1 (7.69%) | 4.5 years |
The mean age of patients was 72.39 years (range: 63–86 years). All (100%) patients were taking bisphosphonates as a continuous treatment at the time of the fracture. Patients started this medication at the time of diagnosis of primary osteoporosis as outpatients. A total of 12 patients (92.31%) were taking alendronate (alendronic acid) with a mean treatment duration of 7.37 years (range: 4–15 years). One patient had taken alendronate for 5 years, but this had been replaced by ibandronate (ibandronic acid) in the 2 months prior to the fracture. One patient (7.69%) had been in treatment with risedronate (risendronic acid) for 4.5 years. A total of 3 cases were taking glucocorticoids concurrently or prior to the fracture. In 3 patients we conducted analytical studies which ruled out alterations in their nutritional and thyroid profiles, as well as tumour markers.
Regarding the characterisation of fractures, all cases presented all the primary variables necessary to define an atypical femoral fracture4: subtrochanteric or diaphyseal location, short oblique or transverse and without comminution, all complete fractures presented involvement of both corticals, with the presence of medial spicula in the fracture foci. The case of incomplete fracture only involved the lateral cortical at the diaphyseal level (Fig. 3).
Of the variables considered as secondary,4 periosteal reaction located in the lateral cortex was detected in 13 cases (Fig. 4), whilst a general increase in cortical thickness was detected in 16 cases. A delay in healing was observed in 8 of the 13 patients with over 6 month follow-up (mean value of 10.25 months). One of these cases required nail dynamisation due to delayed consolidation at 6 months after surgery. Another case presented nonunion or pseudoarthrosis, and is currently awaiting treatment. The mean consolidation time of the 13 patients in general, without excluding those with delayed consolidation, was 7.9 months (range: 4–15 months). The remaining patients at the time of drafting this article have had a follow-up periods of less than 6 months, thus consolidation time cannot be assessed.
Patients reported prodromal symptoms in 6 of the 17 cases. These were defined as a diffuse pain in the middle third of the thigh without previous trauma. One case suffered the symptoms 1 day before the occurrence of the fracture, 3 cases in the 2 weeks prior and 2 cases during the previous 2 years.
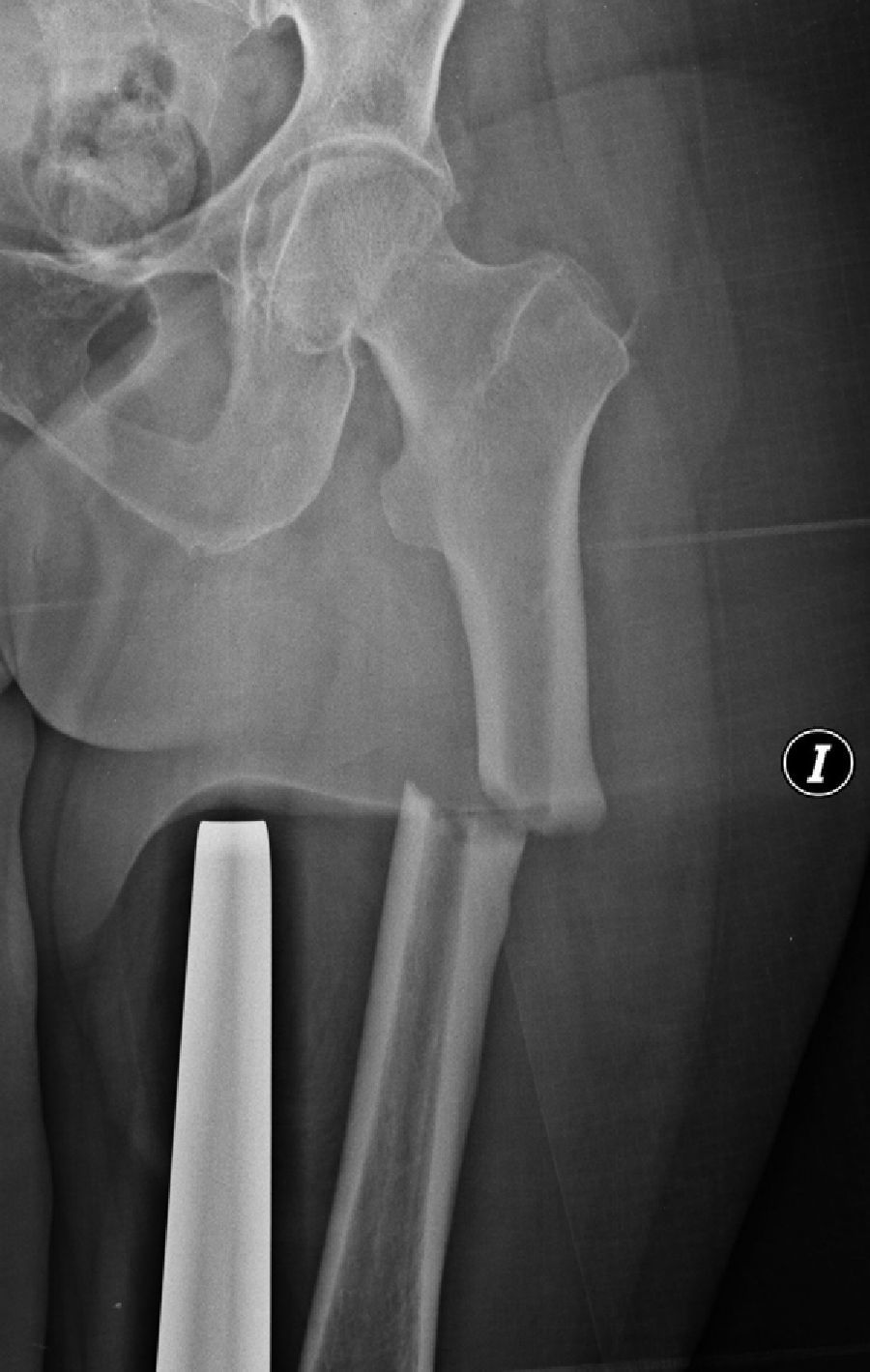
A total of 15 patients underwent internal fixation with long, cervico-diaphyseal, intramedullary nails through static locking drilling (Fig. 5A). The thickness of the nails was not different to those normally used for other patients with the same age. Drilling was carried out up to 1.5mm over the diameter of the nail. In 1 case we performed a retrograde intramedullary nailing (Fig. 5B), and in another case an osteosynthesis or fixation with plates (Fig. 5C) due to large alterations in the axis of the limb caused by hip arthrodesis secondary to septic arthritis at the age of 17 years. As previously indicated, 1 case of antegrade intramedullary nailing required dynamisation due to delayed consolidation, whilst another antegrade case is currently suffering pseudoarthrosis.
The patient with a partial diaphyseal fracture of the femur with exclusive involvement of the lateral cortex was initially treated by conservative treatment, with limb unloading and replacement of the alendronate treatment by teriparatide. After 4 months of unloading, the patient resumed ambulation with load, and at 8 months reported persistence of pain symptoms which led to nailing of the fracture.
Bisphosphonate treatment was stopped in all cases. However, in the 3 bilateral and non-simultaneous cases, the treatment had not been suspended after the first fracture, but it was interrupted after the second fracture. In 2 patients teriparatide was prescribed after the fracture: 1 was the incomplete fracture, as previously indicated, and the other case was due to presenting a consolidation delay which eventually required dynamisation of the nail. In the remaining cases, subsequent treatment of osteoporosis was left for evaluation by the corresponding GP or rheumatologist.
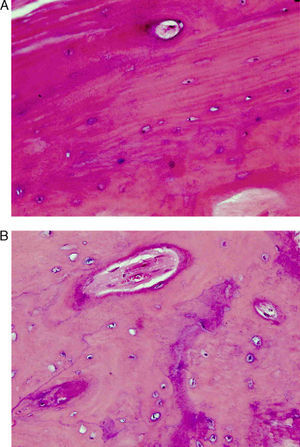
A total of 5 patients underwent intraoperative biopsy of their fracture foci. All cases showed decreased bone activity with a decreased number of osteoclasts. Neoplastic involvement of the fracture foci was ruled out (Fig. 6A and B).
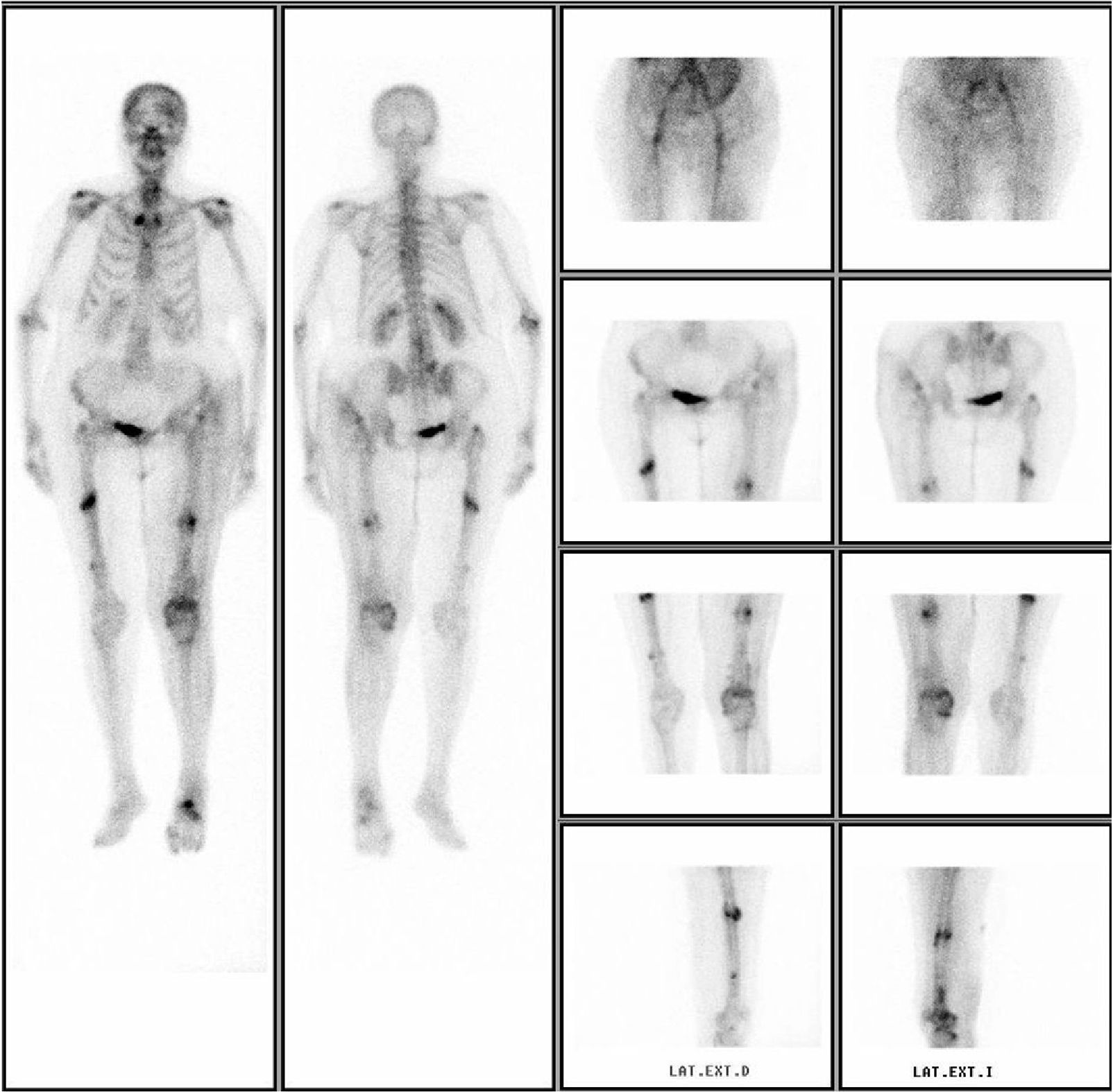
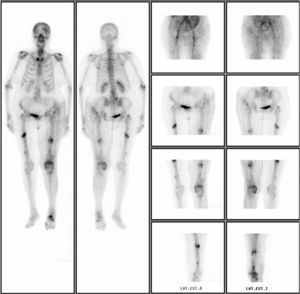
In 5 patients, the physician in charge requested a bone scintigraphy scan labelled with technetium, which revealed hyperuptake at the subtrochanteric or diaphyseal level, suggestive of a stress fracture (Fig. 7). These were requested without following a specific protocol for this type of fracture, but rather by indication of the responsible physician, in order to carry out differential diagnosis and rule out other possible patterns of hyperuptake which may have corresponded to other conditions.
DiscussionThere is extensive experience in the clinical use of bisphosphonates, with their safety and efficacy having been proven in continued treatment for 10 years.23,24 Nevertheless, new and severe adverse effects, such as maxillary osteonecrosis25 and multiple cases5–13 and series14–19 of atypical femoral fractures have been reported in association with long-term treatment with bisphosphonates. Recently, the incidence of these fractures has been published as 1.78/100,000/year (95% confidence interval), increasing to 113.1/100,000/year with exposures of between 8 and 9 years.26 Other articles report figures of 32/1,000,000/year, increasing 10% annually with continuity of treatment.27All these articles suggest an association between the use of bisphosphonates and femoral fractures due to insufficiency or stress (atypical). However, the small number of cases, the lack of consistency in defining these fractures, the lack of homogeneity between studies and the fact that they are mostly retrospective, observational studies, represent a major impediment towards finding some degree of evidence in this association.28–30
In 2005, Odvina et al.20 were the first to observe a possible pathophysiological link. Subsequently, in 2008, Neviaser et al.18 published one of the first retrospective studies in which they observed that 36% of patients with these types of fractures were previously taking alendronate and that 76% of patients taking bisphosphonates presented an atypical pattern, with a simple horizontal line. The authors determined that prolonged treatment with alendronate could be related to the occurrence of these fractures.
Bisphosphonates exert their therapeutic action by reducing bone resorption and increasing bone mineral density, thus decreasing the incidence of vertebral and non-vertebral osteoporotic fractures by up to 50%.1,2 When the treatment is stopped after 5 years, the physiological effect on bone resorption remains for a further 5 years and the risk of fractures does not increase in this period.14 Some patients present a more marked suppression of bone resorption, with inhibition of bone formation and suppression of bone remodelling.21,22 The profound suppression of bone remodelling induced by these drugs could have a negative effect on the mechanical strength of bones, especially after 4 years of continuous treatment, which would entail the possibility of suffering diaphyseal and subtrochanteric stress fractures of the femur.20,31
There are differences between the various drugs in the family known as bisphosphonates. Alendronate has a higher affinity for fixing to hydroxyapatite than other drugs in the same family, so that its effect and permanence on bones would be greater.32 This would facilitate that patients treated with alendronate would be more susceptible to the accumulation of microtraumas and that, therefore, cases of atypical femoral fracture were described mainly in patients taking this substance for long periods.
In contrast to these publications, Abrahamsen et al.19 subsequently reported that only 7% of patients with atypical fractures were receiving treatment with alendronate, the same percentage of patients who suffered hip fractures with an osteoporotic profile. Thus, they concluded that such fractures could be considered as a consequence of osteoporotic disease, rather than as a complication of bisphosphonates. Subsequently, Black et al.14 reported that the incidence of subtrochanteric or diaphyseal femoral fractures that could be related to prolonged treatment with bisphosphonates was very low. These authors did not observe a significant increase in relative risk.
In addition, there is the difficulty in establishing a direct causal relationship between prolonged treatment with bisphosphonates and the appearance of atypical femoral fractures, since numerous patients in the different series published received concomitant treatment with other substances which also caused a suppression of bone remodelling, including glucocorticoids, estrogens, TNF-alpha inhibitors and proton pump inhibitors.33 It is possible that, in some patients, the suppressive effects were exacerbated by these concomitant medications. Giusti et al.6 concluded their work with the hypothesis that treatment with bisphosphonates was present in most cases, and that this was not an essential fact for the development of this type of fractures. They noted other conditions, such as treatment with corticosteroids or with proton pump inhibitors, which were probably involved.
Some published studies have conducted iliac crest biopsies on patients with atypical femoral fractures34 and observed histological findings of bone remodelling suppression among two thirds of these patients. However, the remaining one third of cases presented no such findings, thus suggesting that some other factor besides the suppression of bone remodelling was involved in the onset of these fractures.
Given the considerable controversy of the subject, the American Society for Bone and Mineral Research (ASBMR)4 conducted a review of the data published until 2010 which has become a significant reference on the topic. It states that, according to the published data, the incidence of these fractures can be considered very low. It recognises the difficulty of establishing a causal relationship between bisphosphonates and atypical fractures, although it does point out that the risk of these fractures increases with increasing drug exposure, emphasising the need for establishing research models which determine the true extent of the condition, as well as its relationship with long-term treatment using these drugs.
Although these adverse effects associated with the use of bisphosphonates are being described, the latest reviews emphasise the greater benefit associated with the use of bisphosphonates in the prevention of vertebral and non-vertebral fractures, pointing out the very low incidence of atypical fractures, so that their use is still recommended and validated by years of clinical experience.35 Along with the American agency, the European Society on Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) and the International Osteoporosis Foundation conducted a review led by Rizzoli et al.36 This review acknowledged the existence of a link with the prolonged use of alendronate, but also stated that the balance between the risk of atypical fractures and the benefit of protection against osteoporotic fractures favoured the use of these drugs, since the amount of fractures avoided was considerably greater than those which could occur theoretically.Atypical subtrochanteric and diaphyseal fractures of the femur present a consistent pattern of cortical thickening, mainly of the lateral cortex, in the subtrochanteric or diaphyseal region of the femur, with short oblique or transverse fractures and medial spicula.17 Various cases5–13 and series14–19 have described the characteristics of this type of fracture. In order to standardise the definition of atypical femoral fractures, the ASBMR created a working group which addressed the study of this entity and which published its findings in 2010.4 The group defined the principal and secondary characteristics of complete and incomplete atypical femoral fractures and recommended the presence of all the principal features in order to consider a femoral fracture as atypical. These features include a location in the subtrochanteric or diaphyseal region of the femur, short oblique or transverse line, absent or minimal associated trauma, medial spicula in the case of complete fractures and absence of comminution. The secondary characteristics (which may or may not be present) include cortical thickening, a periosteal reaction of the lateral cortex, prodromal pain, bilaterality, delayed consolidation, associated comorbidities and concomitant exposure to drug treatments, including bisphosphonates, other antiresorptive agents, glucocorticoids and proton pump inhibitors (Table 1).4 Although the possible presence of cortical thickening on radiographs is widely extended, it remains a secondary variable, since its finding actually increases the risk of intertrochanteric fractures among the general population, regardless of treatment with bisphosphonates.37 The same review attempted to reach a consensus on the therapeutic strategy to be followed in cases of diaphyseal or subtrochanteric atypical fractures of the femur. Treatment should be surgical in cases of complete fractures.15–18,38–40
As in our series, the most widely used method of fixation was long intramedullary nailing, since the bone characteristics lead to a high failure rate in cases of osteosynthesis with angular stability plates. It is recommended to drill at least 2.5mm over the diameter of the nail, in order to compensate for a narrow medullar diameter and facilitate insertion.4,13 Some publications refer to the technical difficulty of adequately determining the entry point of the nail and starting its progression manually, due to the particular hardness of the proximal end of the femur.13 The proximal femoral fragment will possibly require further drilling so as to facilitate nail insertion and avoid misalignment of the fracture.
Some studies41 refer abnormally long healing times (up to 22 months) for these fractures. In our series, the mean consolidation time was 7.9 months. Other publications have reported mean consolidation times of 4 months.38
All publications emphasise the need for close monitoring and follow-up of patients being treated with bisphosphonates in order to avoid diaphyseal or subtrochanteric stress fractures of the femur. Obtaining radiographs is recommended in cases of prodromal symptoms including thigh pain without previous trauma. Performing an MRI or bone scintigraphy scan with technetium may help to confirm the diagnosis.4,38
The appropriate duration of bisphosphonate treatment is a subject of ongoing debate and discussion, and is not yet well-defined.3 The latest reviews report an increased risk and incidence of these fractures in treatments for periods exceeding 5 years.4 Reassessing the continuation of the treatment is recommended after that period, and in case of alert signs such as pain in thighs or cortical thickening on radiographs, it should be substituted by other agents to continue the treatment of osteoporosis.
The tendency is to recommend preventive nailing in cases of incomplete fractures with pain.15–18,38–40 Conservative treatment may be considered in cases with minimal pain, limiting the load on the limb. However, fixation should be considered if there is no improvement in symptoms and/or radiographs after 2–3 months of conservative treatment. In cases of incomplete fractures and absence of pain, physical activity should be limited until there are no traces of bone oedema in MRI scans.4 Nevertheless, these are recommendations from the literature, which require more epidemiological studies of incomplete fractures, so there are no clear action guidelines.42 In the series of bilateral fractures published by Capeci et al. in 2009,38 these authors raised the option of prophylactic nailing of the contralateral limb after the first diagnosis of fracture. This prophylactic nailing was performed in 3 of their cases with atypical diaphyseal fractures and prodromal symptoms of pain in the diaphyseal middle third and radiographic changes of cortical thickening in the contralateral limb. However, the same authors also mentioned the need for more studies in order to recommend prophylactic fixation systematically.
Regarding drug therapy, the recommendation of ASBMR4 is that treatment with antiresorptive agents should be discontinued in all cases of stress reaction or subtrochanteric or diaphyseal femoral fracture, either complete or incomplete. Dietary calcium contributions and vitamin D levels should be assessed and the right supplements should be prescribed. Some published case reports and some empirical evidence suggest that treatment with teriparatide could improve or accelerate the consolidation of these fractures.4,41,43 Moreover, in line with a considerable amount of data from animal tests,44 certain clinical data45–47 indicate that teriparatide has a positive effect on fractures which are not consolidated. Teriparatide administration is considered adequate in patients who suffer these fractures, especially if there are scarce signs of consolidation between 4 and 6 weeks postoperatively.4
In conclusion, from the case reports and clinical series published in recent years, it is possible to define a characteristic pattern in this type of stress fractures. It would include mainly female patients with osteoporosis, who were following treatment with bisphosphonates, and who may or not suffer thigh pain days, weeks or months before a spontaneous, transverse, subtrochanteric or diaphyseal fracture of the femur, without an injury mechanism to justify it or in the context of low-energy trauma. A bone scintigraphy scan or MRI study could be used for early diagnosis, since the femoral diaphysis presents changes before the fracture takes place. In general, it would be necessary to reassess the use of these drugs after a period of 5 years, since an increased incidence of atypical fractures has been described after this time. Further studies are needed to clarify the pathophysiology of these fractures and to better define their origin and which patients are more prone to suffering them.
Level of evidenceLevel of evidence iii.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare that this work does not reflect any patient data.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Méndez-Gil A, et al. ¿ Qué sabemos de las fracturas atípicas en los pacientes en trata-miento con bifosfonatos? Revisión bibliográfica a raíz de una serie de casos. Rev Esp Cir Ortop Traumatol. 2013;57:95-105.