Plantar fasciitis is the main cause of heel pain in middle-aged patients. In chronic cases, limited ankle dorsiflexion caused by isolated gastrocnemius contracture is considered the main risk factor for suffering it. Therefore, in recent years the number of patients operated on by proximal fasciotomy of the medial gastrocnemius (FPGM) has increased to treat chronic plantar fasciitis.
Material and methodsSystematic review following the PRISMA guidelines. We have carried out a bibliographic search in Pubmed, Science Direct, Cochrane Library and Web of Science databases. One hundred and eighty-four articles were found. Data extraction was performed using the Covidence software, and a quality and risk of bias analysis of the included articles was performed based on the Cochrane risk of bias Tool 2.0.
ResultsThree articles were included in the review: two randomised clinical trials and one cohort study with a total of 138 patients. In the analysed studies, patients after proximal fasciotomy of the medial gastrocnemius showed significant improvements in pain and in the AOFAS score with high levels of patient satisfaction. Increases in ankle dorsiflexion angle were found after 12 months of follow-up, with no loss of gastrocnemius strength. The complication rate was low and fewer occurred in the proximal fasciotomy compared to plantar fasciotomy.
ConclusionProximal fasciotomy of the medial gastrocnemius provides clinical benefit in patients with chronic plantar fasciitis, with a low probability of complications and high patient satisfaction.
La fascitis plantar supone la principal causa de dolor en el talón en los pacientes de mediana edad. En los casos crónicos, la dorsiflexión limitada del tobillo producida por contractura aislada del gastrocnemio se considera el principal factor de riesgo de padecerla. Por lo que en los últimos años se ha incrementado el número de pacientes intervenidos mediante fasciotomía proximal de gemelo medial (FPGM) para tratar la fascitis plantar crónica.
Material y métodosRevisión sistemática siguiendo las guías PRISM. Hemos realizado una búsqueda bibliográfica en las bases de datos PubMed, Science Direct, Cochrane Library y Web of Science. Se encontraron 184 artículos. La extracción de datos fue realizada utilizando el software Covidence, y se realizó un análisis de calidad y riesgo de sesgo de los artículos incluidos, basada en Cochrane risk of bias Tool 2.0.
ResultadosFueron incluidos 3 artículos en la revisión, 2 ensayos clínicos aleatorizados y un estudio de cohortes con un total de 138 pacientes. En los estudios analizados los pacientes tras la FPGM presentaban mejorías significativas en la valoración del dolor y en la escala de la American Orthopaedic Foot & Ankle Society (AOFAS), con niveles altos de satisfacción de los pacientes. Se encontraron aumentos en el ángulo de dorsiflexión del tobillo tras 12 meses de seguimiento, sin pérdidas de fuerza del gastrocnemio. La tasa de complicaciones fue baja y menores con la FPGM que con la fasciotomía plantar (FP).
ConclusiónLa fasciotomía proximal de gastrocnemio medial aporta beneficio clínico en los pacientes con fascitis plantar crónica, con baja probabilidad de complicaciones y con una satisfacción alta de los pacientes.
In recent years a topic of interest has been the study of the Achilles-calcaneus plantar system. It is known that contractures of the triceps surae muscles and of the Achilles tendon are associated with food and ankle pathologies (plantar fasciitis, metarsalgia, Charcot neuropathy, diabetic foot ulcers, hallux valgus) as well as an alteration in the distribution of the plantar pressure from the hindfoot to the midfoot and forefoot. This is because limited ankle dorsiflexion leads to compensatory pronation in the tarsal joints, which in the long term can generate deformities in the longitudinal arch of the foot, such as flat feet and consequently excessive stretching and tension in the plantar fascia. Aronow et al.1 demonstrated that isolated gastrocnemius contractures produced the same pathological process.
One of the most salient conditions of the plantar fascia is plantar fasciitis. This condition is the main cause of heel pain, and is the reason for consultation in approximately one million cases per year in U.S.A.2 It is most prevalent in patients within the 45–60 year age group, with no gender differences.3 Plantar fasciitis occurs when the plantar fascia is subjected to excessive stress or repeated micro-trauma, producing an initial inflammatory reaction, which subsequently leads to the appearance of degenerative changes. However, the aetiology is multi-factorial in nature and is frequently found in runners; in patients with a high body mass index (BMI); in workers who spend prolonged periods of time on their feet, and in other conditions such as flat feet, pes cavus, hallux valgus, or limited dorsiflexion caused by the shortening of the Achilles tendon or gastrocnemius contracture leading to excessive pronation of the foot and increasing the tension of the plantar fascia.4–8 Regarding the latter, great advances have been made from a therapeutic viewpoint and it is now considered the most significant risk factor, especially in chronic cases.8
Approximately 80–90% of patients will improve within the first 6–12 months with conservative treatment alone or combined.3,4,6 Nowadays combined stretching of the plantar fascia plantar and gastrocnemius is considered the first option, particularly in chronic plantar fasciitis.3 Surgical treatment should be reserved for those patients in whom conservative treatment has not been effective after 6–12 months. Among the different surgical interventions available, plantar fasciotomy (PF) remains the standard. Some of the complications may be instability of the plantar arch, persistence of pain, and loss of plantar arch height or metatarsalgia,6 particularly in the case of an excessive amount of sectioned fascia.
Proximal medial gastrocnemius release (PMGR) has gained relevance in recent years, following the advance in biomechanical knowledge of the foot and ankle. Among the possible complications of the procedure are haematomas in the popliteal area, delayed healing or wound infection. Nerve injuries to the medial saphenous and medial sural nerve9 may even occur due to excessive incision lateralisation or medialisation. In the case of distal approaches, there is a greater probability of muscle complex strength loss.
Recent studies show improvement outcomes in 95% of patients who underwent PMGR compared to 60% in those in whom PF6 was performed. The objective of this systematic review was therefore to evaluate the usefulness of PMGR in the treatment of chronic plantar fasciitis.
Material and methodsWe conducted a systematic review in keeping with the PICO strategy, from which we based the subsequent article selection and data extraction process:
- -
Patients: chronic plantar fasciitis.
- -
Intervention: PMGR.
- -
Comparison: conventional treatments.
- -
Events: clinical changes, complications.
The databases used for the search were PubMed, Science Direct, Cochrane Library and Web of Science. The search strategy evolved using a combination of key words including: “plantar fasciitis”, “plantar fasciopathy”,“plantar heel pain”, “heel pain”, “heel spur”, “calcaneodynia”, “medial gastrocnemius release”, “gastrocnemius release”, “medial gastrocnemius recession”, “gastrocnemius recession”, “proximal gastrocnemius release”, “proximal gastrocnemius recession” using the Booleans “OR” and “AND” and MeSH terms when possible. Searches were limited to articles written in English or Spanish. Inclusion and exclusion criteria were marked a priori.
Inclusion criteria:
- -
Patients with chronic plantar fasciitis.
- -
Patients over 18 years of age.
- -
Isolated treatment with proximal medial gastrocnemius release.
- -
Study with level of evidence III or above.
Exclusion criteria:
- -
Other foot and ankle pathologies.
- -
Other combined treatment with proximal medial gastrocnemius release.
It was subsequently decided to exclude studies with preliminary outcomes, so as not to cause confusion between the preliminary and the final results.
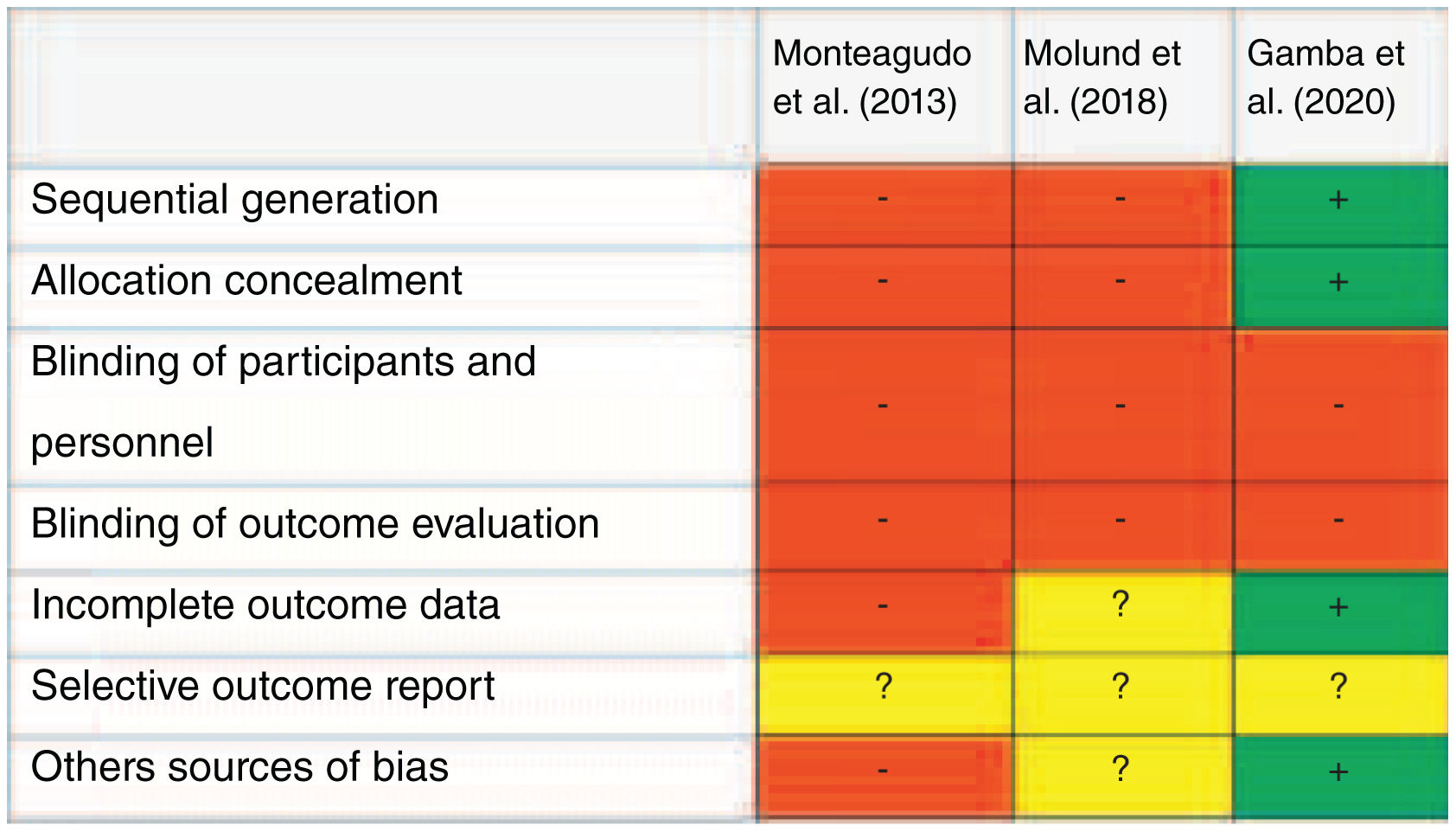
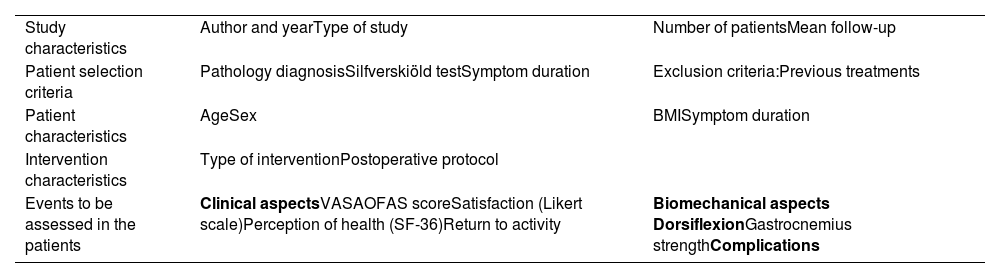
Covidence software10 was used to carry out the review. Two reviewers simultaneously and independently read the title, abstract and subsequently the full text of the selected articles at the different stages of the process. Any conflicts that arose were resolved through discussion. The definitively included studies were subjected to a quality analysis using the tool included in Covidence based on Cochrane risk of bias Tool 2.011 and a series of variables were selected for data extraction (Table 1).
Data extraction variables.
| Study characteristics | Author and yearType of study | Number of patientsMean follow-up |
| Patient selection criteria | Pathology diagnosisSilfverskiöld testSymptom duration | Exclusion criteria:Previous treatments |
| Patient characteristics | AgeSex | BMISymptom duration |
| Intervention characteristics | Type of interventionPostoperative protocol | |
| Events to be assessed in the patients | Clinical aspectsVASAOFAS scoreSatisfaction (Likert scale)Perception of health (SF-36)Return to activity | Biomechanical aspects DorsiflexionGastrocnemius strengthComplications |
AOFAS: American Orthopaedic Foot & Ankle Society; SF-36: Short Form-36 Health Survey; VAS: visual analogue scale.
The search strategy generated an initial total of 184 studies for screening. Forty-five duplicate studies were eliminated and the abstracts of the remaining 139 were read. Of these, 100 were considered irrelevant and the full text was read in 39. Four studies were included in the work, after excluding 35 studies for different reasons that can be consulted in the flow chart (Fig. 1).
The study published by Gamba et al.12 in 2019 is a publication of the preliminary results of their clinical trial and it was decided to exclude it, since these results were included in the 2020 Gamba et al.13 article.
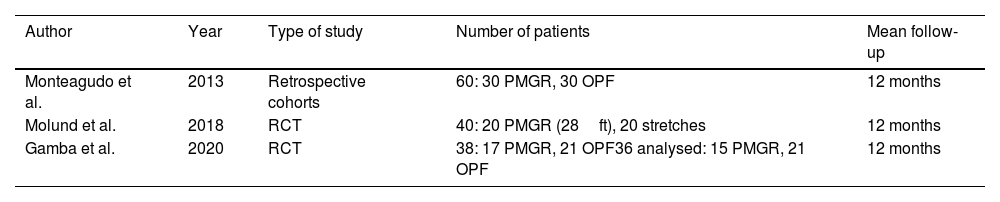
Finally, the selected studies included a level III retrospective cohort study and two level I randomised clinical trials. Table 2 contains their characteristics.
Characteristics of the included studies.
| Author | Year | Type of study | Number of patients | Mean follow-up |
|---|---|---|---|---|
| Monteagudo et al. | 2013 | Retrospective cohorts | 60: 30 PMGR, 30 OPF | 12 months |
| Molund et al. | 2018 | RCT | 40: 20 PMGR (28ft), 20 stretches | 12 months |
| Gamba et al. | 2020 | RCT | 38: 17 PMGR, 21 OPF36 analysed: 15 PMGR, 21 OPF | 12 months |
OPF: open plantar fasciotomy; PMGR: proximal medial gastrocnemius release; RCT: randomised clinical trial.
In all the studies similar inclusion criteria were adhered to. Patients over 18 years of age with chronic clinically diagnosed plantar fasciitis were selected, with or without their accompanying imaging tests.
With the exception of the studies carried out by Gamba et al.,12,13 all of them required the presence of gastrocnemius contracture (positive Silfverskiöld test). Patients included had to present an absence of clinical response to conservative treatment for at least nine months12–14 or 12 months.15 However, the average duration of symptoms varied from 14 to 32 months. With the exception of one studio,14 all authors presented a distribution by sex with a greater proportion of women to men, around 70–90%. The mean ages of the patients were 44–50 years (Table 3).
Inclusion criteria and characteristics of patients who underwent PMGR.
| Inclusion criteria | Mean time of symptoms (months) | Sex (M/W) | Mean age (range) | BMI | |
|---|---|---|---|---|---|
| Monteagudo et al. (2013) | Clinical diagnosis. Failure of minimum 9 months conservative treatment. Clinical diagnosis. Failure. Positive Silfverskiöld. | 14 (10–64) | 16/14 | 44 (21–63) | NC |
| Molund et al. (2018) | Clinical diagnosis. Failure of minimum 12 months conservative treatment. Positive Silfverskiöld. | 31 (12–252) | 5/15 | 46 (29–68) | 27.8 (20.1–49.8) |
| Gamba et al. (2020) | Clinical diagnosis. Failure of minimum 9 months conservative treatment. | 32.1 | 90.5% W | 46.2±11.1 | 31.7±3.7 |
The surgical intervention consisted of proximal medial gastrocnemius release (PMGR). All four studies compared internal gastrocnemius release with other interventions. Molund et al.15 compared PMGR with an isolated stretching protocol, whilst Gamba et al.12,13 and Monteagudo et al.14 did so with open plantar fasciotomy (OPF).
The postoperative regimen was reported in all four articles. In all of them, immediate weight bearing was allowed as tolerated. There were differences in the type of orthotics used after surgery. Both Monteagudo et al.14 and Gamba et al.12,13 used a rigid open shoe for two weeks, whilst Molund et al.15 did not report any use of material.
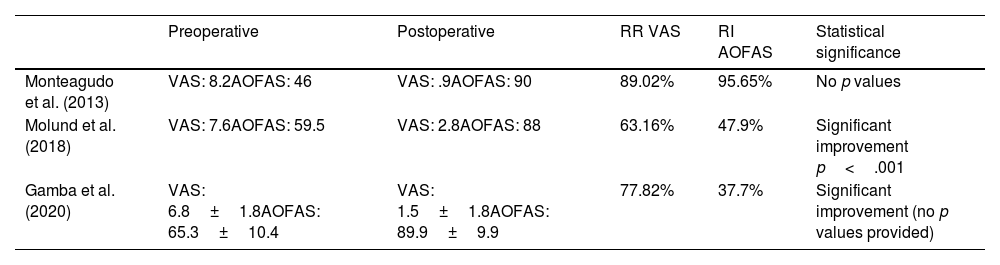
All included studies recorded preoperative and postoperative pain using the visual analogue scale (VAS). Regarding the values obtained, an average reduction in pain of 5.3±1.4 points was calculated, which corresponds to an average of relative reductions from 57.35% to 89.02%. At the same time, the American Orthopaedic Foot & Ankle Society (AOFAS) scale score was assessed, in which relative increases of up to 95.6% were observed (Table 4). These values, along with the mean values, are present in Appendices A and B. Improvements in VAS and AOFAS were reported in 20% of the patients the first week and in 60% between the first and eighth week for Monteagudo et al.14 and within the first postoperative month for Gamba et al.,12,13 unlike patients with OPF who in no case reported progress before six weeks.14
Pre and postoperative outcomes of VAS and AOFAS with MGF.
| Preoperative | Postoperative | RR VAS | RI AOFAS | Statistical significance | |
|---|---|---|---|---|---|
| Monteagudo et al. (2013) | VAS: 8.2AOFAS: 46 | VAS: .9AOFAS: 90 | 89.02% | 95.65% | No p values |
| Molund et al. (2018) | VAS: 7.6AOFAS: 59.5 | VAS: 2.8AOFAS: 88 | 63.16% | 47.9% | Significant improvement p<.001 |
| Gamba et al. (2020) | VAS: 6.8±1.8AOFAS: 65.3±10.4 | VAS: 1.5±1.8AOFAS: 89.9±9.9 | 77.82% | 37.7% | Significant improvement (no p values provided) |
RR: relative reduction; RI: relative increase.
In three studies12,13,15 a health perception questionnaire (SF-36) was administered to the participants at the end of follow-up, observing significant postoperative increases in all items after PMGR. Patient satisfaction according to the Likert scale was also collected in three12–14 of the four studies. Recommendation of the intervention to a friend or family member was recorded in one,14 with the vast majority of patients being very satisfied or satisfied, and with a high degree of recommendation. The levels of satisfaction and recommendation in the groups of patients undergoing OPF varied, depending on the study. Tables 5 and 6 contain these data.
SF-36 health perception questionnaire.
| SF-36 | |
|---|---|
| Molund et al. (2018) | Significant differences (p<.05) between MGF and isolated stretching in all items in favour of intervention |
| Gamba et al. (2020) | Significant improvement in both groups for physical functioning and pain (p .01 PMGR and p .00 OPF)No significant differences between both groups in any item (p>.3) |
Likert scale and recommendation.
| Likert scale | Recommendation | |
|---|---|---|
| Monteagudo et al. (2013) | PMGR: non worse and 24 without pain-Satisfaction: excellent 80%, good 10%, satisfactory 5%, poor 5%OPF: 2 worse and 10 without pain-Satisfaction: excellent 10%, good 30%, satisfactory 20%, poor 40% | FGM: 95%OPF: 45% |
| Gamba et al. (2020) | PMGR: 85.8% very satisfiedOPF: 89.5% very satisfied | NR |
NR: not collected.
Data regarding improvement in the ankle dosiflexion ability were provided by the Molund et al.15 study. They described significant increases in the degrees of dorsiflexion with the knee extended, varying from 6° (−3 to 15°) preoperatively, to 10.5° (0–23°) at 12 months. With the knee flexed, no such increases were reported.
Gastrocnemius strength was recorded in all included studies. However, each one objectified this measure in a different way. Monteagudo et al.14 was based on toe raising of the affected foot for one minute, Gamba et al.12,13 assessed this with 10 heel lifts of the affected foot and Molund et al.15 used a battery of six tests.
Gamba et al.13 reported finding no significant differences in plantar flexion capacity between the PMGR and OPF groups. For their part, Molund et al.15 found no significant differences between the two comparison groups for any of the tests, except for a minimal but significant decrease in jumping capacity in both the PMGR intervention group and the control stretching group, as well as a significant increase in toe lifting resistance, only in the PMGR group. The rest of the studies13,14 did not report strength losses in the muscle complex after PMGR.
Regarding the return to work and sport, only Monteagudo et al.15 provided data. Return to work was achieved at around three weeks and to sport at almost five weeks in the group operated on with proximal medial gastrocnemius release. The results were much earlier compared to the OPF group in which they returned to work at 12 weeks (not achieved on two occasions) and sports at 16 weeks (not achieved in two other cases).
Complications of the procedure were recorded in each of the studies, although there were no major complications. Molund et al.15 described swelling and prolonged pain on three occasions, one case of gastrocnemius cramps and one case of popliteal fossa pain. Gamba et al.12,13 reported a superficial wound infection and a sural nerve injury. Monteagudo et al.14 reported only one case of gastrocnemius haematoma. Complications were resolved on all occasions, except in the case of pain in the popliteal fossa, which did not resolve after one year.
Quality analysis of the studies was performed with Covidence and is summarised in Fig. 2. The highest quality study is the one published by Gamba et al.13 since it describes a correct generation of the random sequence and its concealment. None of the studies were blind. Reporting of selective outcomes was uncertain in all four studies. Furthermore, the results of incomplete data and the probability of other sources of bias were uncertain for Molund et al.,15 good for Gamba et al.,13 and high risk for Monteagudo et al.14 This shows that the included studies are of low quality except for the one published by Gamba et al.13
DiscussionMedical gastrocnemius release has been shown to have a beneficial effect in those patients affected by chronic plantar fasciitis in all studies of this review. Significant improvements were obtained in the VAS and AOFAS scores in biomechanical parameters as was significant patient satisfaction and a pleasant and rapid return to work and sports activities.
Ninety per cent of patients show a response in the first 6–12 months to conservative treatments, including gastrocnemius stretches. However, in the study by Hoefnagels et al.16 they found that of 47 patients who began treatment with stretching, 32 failed with these measures and underwent surgical treatment using distal recession of the medial gastrocnemius. Even so, treatment should begin conservatively and in those cases in which no response is obtained, surgical treatment should be considered. Molund et al.15 demonstrate how in patients in whom the course is long and no response is achieved to treatment with gastrocnemius stretching, significantly better results are obtained with PMGR than by maintaining the stretches alone.
OPF is traditionally the first surgical option. However, the studies included in this review have shown that proximal medial gastrocnemius release obtains significant benefits in VAS scores, with pain reduction from 57.35% to 89.02% and increases in the AOFAS scale of up to 95.6%.
Monteagudo et al.14 and Gamba et al.12,13 obtained favourable results with both OPF and PMGR. However, return to work and sport occurred earlier in the proximal fasciotomy group. Regarding patient satisfaction after PMGR, excellent results were obtained. No solid conclusions may be reached when comparing PMGR with OPF due to the observed variability, since for Gamba et al.12,13 satisfaction was similar, whilst for Monteagudo et al.14 it appears that the differences were greater in their satisfaction percentages and Likert scores.
Davies et al.17 support these findings by commenting that only 50% of patients can expect complete resolution of symptoms and activity restrictions after OPF, so satisfaction with the intervention is usually around 50%. In addition, they obtained the benefits approximately after seven months. This data contrasts with the results obtained in our review, since no changes were obtained in VAS and AOFAS before six weeks for the OPF, unlike the group with PMGR in which the benefits were obtained mostly in the first week or within the first eight weeks, in addition to a much earlier return to activities compared with OPF.
The studies in this review show low complication rates for OPF and in no case are major complications described, with wound problems generally predominating. However, the literature describes complications that involve biomechanical instability of the foot, generating collapse of the plantar arch and pain in the lateral column of the foot.9 This particularly occurs in cases in which the amount of fascia sectioned is more extensive, which is why it is currently recommended to section only the medial third.3 Despite the recommendations, even with a partial resection of the fascia, the biomechanics of the foot can continue to be affected by altering the support function of the foot arch.18 These types of biomechanical complications do not occur with PMGR.
Other studies have shown that PMGR improves biomechanical parameters of the foot and ankle, such as increasing postoperative dorsiflexion capacity and preserving gastrocnemius strength, although Molund et al.15 reported a minimal decrease in one of the six tests that they carried out to evaluate this.
Maintaining the strength of the muscle complex is relevant, since its defect has been one of the concerns of gastrocnemius fasciotomy,19 although the risks are greater in other types of procedures such as Achilles tendon elongation.20 The favourable findings obtained in this review could be due to the use of a proximal incision technique in all included studies.
The presence of gastrocnemius contracture has been a point of debate among some of the studies evaluated. All except Gamba et al.12,13 required a positive Silfverskiöld test to be included in the research project.
Isolated gastrocnemius contracture represents a limitation in ankle dorsiflexion, which generates biomechanical alterations and foot deformities, implying excessive tension in the plantar fascia.1 This limited dorsiflexion is considered the most important risk factor for plantar fasciitis, especially in chronic cases.8,21 It is therefore important to rule out isolated gastrocnemius contractures in patients with a long history of the pathology and who do not respond to conservative treatment.22 Despite this, Gamba et al.12,13 demonstrate how even in patients with a negative Silfverskiöld test, favourable results are obtained with PMGR.
We found no systematic review in the literature that focused solely on analysis of proximal medial gastrocnemius fasciotomy. The two most recent systematic reviews on gastrocnemius release in the treatment of plantar fasciitis analyse studies in which both a distal gastrocnemius recession and proximal medial gastrocnemius fasciotomy were performed.23,24
The review by Pickin et al.,23 contained seven articles, of which four performed a gastrocnemius recession at a distal level on the medial malleolus or at the myotendinous junction. Despite this, the VAS and AOFAS results recorded were similar to those presented in this review, even in two cases in which follow-up was longer than 12 months. This suggests that the intervention may have beneficial effects even in the long term. High satisfaction and biomechanical results were recorded but no data was collected on recovery from work and sports activity, or on changes in the dorsiflexion angle. The rates and importance of complications coincided with those of this study. However, they reported cases of objective and subjective loss of strength for plantar flexion, which could coincide with the application of a technique with a more distal approach.
Furthermore, in the review by Arshad et al.24 six articles were analysed, of which in three a medial gastrocnemius recession was performed at a distal level or at the myotendinous junction. The VAS and AOFAS results were similar to those obtained in our review. Likewise, high satisfaction and biomechanical results were obtained, with a low rate of complications, similar to those of this review. Five of the six studies included in the review by Arshad et al.24 evaluated postoperative plantar flexion strength. No loss of objective and subjective strength was described in any of them. However, only isometric and isokinetic strength was measured in one of the studies,15 showing an increase in these parameters after surgery despite having undergone surgery at the myotendinous junction.
Notwithstanding, the results should be viewed with caution, since they only measured four patients (seven limbs) and follow-up was only for three months.
One of the limitations of this review was the inability to access the full text in some of the screened articles, which may have been of interest. Also, despite meeting the planned level of evidence for inclusion (III or higher), the four studies may have contained certain biases. The number of studies was limited and they all had a small sample size. Blinding patients, researchers and analysts was not possible due to the evidence of the treatment performed. Another notable fact is that although the follow-up period should have been sufficient for patient recovery and assessment of findings, it was relatively short. Further prospective studies for PMGR with a longer observational periods are therefore required. Despite an apparent earlier recovery in PMGR compared to OPF, more studies with a longer follow-up period are required to reach a clear consensus. Furthermore, only three of the included studies12–14 made direct comparisons between PMGR and. OPF.
ConclusionIn conclusion, proximal medial gastrocnemius release as an intervention provides clinical benefits in patients with chronic plantar fasciitis, together with high satisfaction; a low probability of complications; no alterations in strength for postoperative plantar flexion, and benefits within a shorter time period than with conventional treatments. However, prospective studies with a larger number of patients and longer follow-up would be necessary to reach more reliable conclusions.
Level of evidenceLevel of evidence ii.
Conflict of interestsThe authors have no conflict of interests to declare.