This study aimed to investigate to what extent people with carpometacarpal thumb osteoarthritis that are socioeconomically disadvantaged and have psychological disorders report higher pain levels and worse patient-rated upper-extremity functionality after surgical treatment.
Material and methodA single centre, retrospective observational cohort study analysing 100 patients diagnosed with thumb carpometacarpal osteoarthritis between 2013 and 2019. Patients were divided into two groups (50/50), depending on whether they received surgical or conservative treatment. The socio-economic status (ESeC classification) and presence of psychological comorbidities were investigated. Functional outcomes were assessed using the Visual Analogue Scale (VAS), Q-DASH questionnaire and Kapandji score. Current mental disorders were evaluated using STAI, PHQ-9 and PCS screening scales.
ResultsMeasures of functional hand scores (Q-DASH) were higher and had considerably less pain in surgically treated participants, although thumb mobility (Kapandji) was more restricted. They were also associated with higher scores on psychological assessment scales. Sixty-four per cent of the patients came from lower socio-economic classes and suffered from poorer scores on the mental health screening questionnaires. Of the patients manage surgically, 54% were diagnosed of dysthymic disorder and showed significantly worse patient-rated upper-extremity function (Q-DASH questionnaire, median [IR]: 31.8 [20.5–54.6] than patients without psychological disorders (median [IR]: 13.6 [2.3–36.5]). No differences were found for patients with and without dysthymic disorder managed nonoperatively.
ConclusionsPatients with higher rates of depression, anxiety and pain catastrophizing behaviour showed significantly worse outcomes after surgery for osteoarthritis of the first carpometacarpal joint. Lower socio-economic class significantly influences levels of depression and anxiety but did not affect functional outcome. Surgical treatment of carpometacarpal thumb osteoarthritis achieved better self-perceived hand function (QDASH, VAS, Kapandji) than conservative treatment.
Investigar si los pacientes en grupos socioeconómicos más desfavorecidos y con alteraciones psicológicas identificadas, presentaban más dolor y peor función tras el tratamiento quirúrgico de la artrosis trapecio-metacarpiana.
Material y métodoEstudio observacional de cohortes retrospectivo de un solo centro hospitalario. Se incluyeron 100 pacientes con diagnóstico de artrosis trapecio-metacarpiana entre los años 2013 y 2019. Se dividieron en 2 grupos según hubieran recibido tratamiento quirúrgico o conservador (50/50). Se analizó la presencia de comorbilidades psicológicas (depresión, ansiedad, trastorno distímico) y el tipo de profesión desempeñada (clasificación ESeC). La evaluación funcional se realizó mediante la escala visual analógica (EVA), el cuestionario Q-Dash y la movilidad según el test de Kapandji. Se analizó, además, el estado psicológico actual mediante las escalas STAI, PHQ-9 y PCS.
ResultadosComparado con el grupo conservador, el grupo quirúrgico mostró mejores resultados funcionales (Q-DASH) y menor dolor (escala EVA), aunque la movilidad (test de Kapandji) fue menor. También tenían puntuaciones más altas en los 3 cuestionarios sobre los trastornos del estado de ánimo. El 54% de los pacientes tratados quirúrgicamente presentaban diagnóstico de trastorno distímico, y mostraron significativamente peor funcionalidad de la mano (Q-DASH, (mediana [RIC]: 31,8 [20,5-54,6] respecto a los pacientes sin factores psicológicos previos (mediana [RIC]: 13,6 [2,3-36,5]). El 64% de estos pacientes procedían de clases socioeconómicas bajas, existiendo asociación con peores puntuaciones en los cuestionarios psicológicos. No se hallaron diferencias entre los pacientes con y sin trastorno distímico del grupo conservador.
ConclusionesLos pacientes quirúrgicos con mayores índices de depresión, ansiedad y comportamiento catastrófico ante el dolor muestran significativamente peores resultados funcionales (QDASH) tras la cirugía de la artrosis trapecio-metacarpiana, aunque no se halló asociación para el grupo conservador. La clase socioeconómica influye en los niveles de depresión y ansiedad, pero no en el resultado funcional del tratamiento. No obstante, los pacientes tratados quirúrgicamente presentaban mejores resultados funcionales (Q-DASH) y mayor mejoría del dolor pretratamiento (escala EVA), que los tratados conservadoramente, aunque la movilidad de la articulación trapecio-metacarpiana (test de Kapandji) resultó ser menor en el grupo quirúrgico.
Osteoarthritis of the first carpometacarpal joint is a degenerative disease which causes pain and loss of function of the hand for normal activities.1
Initially patients are treated conservatively, using manual and occupational therapy, outhouses and injections. This treatment is effective in reducing pain in some patients, thereby avoiding the need for surgical treatment.2
The surgical alternatives used in rhizarthrosis are based on 5 fundamental techniques: osteotomies of the first metacarpal; total or partial trapeziectomies; ligamentoplasties; arthroplasties, and arthrodeses. These can be performed alone or in combination with one another.
When conservative treatment is initiated, the level of pain experienced by patients improves randomly, with this improvement in disability and degree of pain only partially explained by demographic characteristics, such as age and sex, or specific to the degenerative disorder, such as radiological osteoarthritis or grip strength.3 This suggests that there must be other factors related to the clinical evolution of trapeziometacarpal osteoarthritis, which for now remain unknown.
Several studies on the surgical management of osteoarthritis, including hip and knee arthroplasty,4 and some specific surgical techniques for trapeziometacarpal osteoarthritis,5 have found an association between certain psychological factors (such as dysthymia, catastrophising behaviour towards pain and illness perception) and poorer clinical results, both before and after treatment. In addition, recent studies have suggested that interventions that improve catastrophising behaviour and negative illness perception,6 have a beneficial effect on osteoarthritis symptoms.
Although there is evidence of an association between psychological factors and symptom severity in both hip and knee osteoarthritis, this association has been much less studied in patients treated for trapeziometacarpal joint osteoarthritis.7 It is unknown whether there is an association, and to what extent, between psychological factors and the pain reported by these patients, which is the main symptom of trapeziometacarpal osteoarthritis.8 Furthermore, while in other disorders such as knee osteoarthritis, the perception of the disease has been shown to be a prominent factor, few studies have investigated how much the perception of the disease influences the pain reported in trapeziometacarpal osteoarthritis.7
The effect of socioeconomic factors and preoperative expectations on the surgical outcome of hip and knee arthroplasties has also been evaluated.9 There appears to be a positive correlation between patient perspectives and improved outcomes, such that patients from high socioeconomic groups may have higher expectations and better surgical outcomes after joint replacement.10 In fact, there are studies showing that socioeconomic status and preoperative standard of living have a greater influence on the surgical outcome after a cementless hip replacement than factors directly related to the implant.11 However, the influence of these types of factors on the surgical outcome of trapeziometacarpal osteoarthritis has not been analysed either.
The possibility of preoperatively identifying those patients with a poorer outcome after surgical treatment of trapeziometacarpal osteoarthritis could help implement measures prior to surgery in this selected group to improve their final results.
The aim of our study was to determine whether patients in more disadvantaged socioeconomic groups and with identified psychological disorders had more pain and poorer function after surgical treatment of trapeziometacarpal osteoarthritis. To determine how much surgery influenced the natural evolution of the disease, these patients were also compared with a group of patients managed conservatively.
Material and methodA retrospective observational cohort study was conducted in a single tertiary university hospital centre, providing for a population area of approximately 500,000 inhabitants. The study was conducted in accordance with the ethical standards recognised by the Declaration of Helsinki and resolution 008430 of 1993 and was approved by the Institution's Ethics Committee (internal code 21/178), with informed consent obtained from all patients who participated in the study.
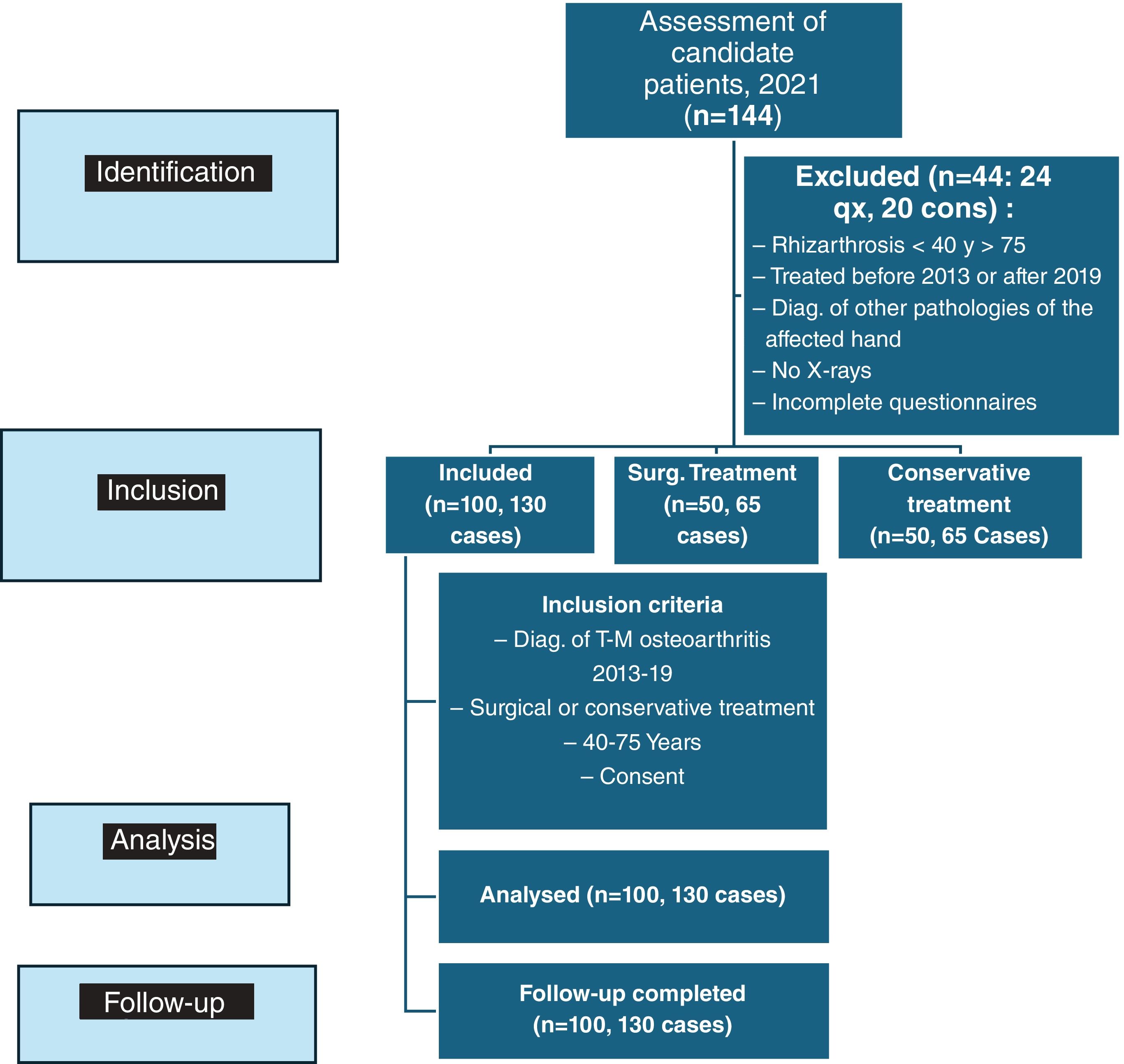
Consecutive patients were included: (1) diagnosed with osteoarthritis of the trapeziometacarpal joint, (2) undergoing any type of surgical or conservative treatment, (3) between 40 and 75 years of age, (4) treated at our centre between 2013 and 2019, and (5) who gave their consent to participate in the study. Patients were identified in the outpatient clinics of the hospital, as well as in the 3 Peripheral Specialty Centres attached to the health area. Patients diagnosed with trapeziometacarpal osteoarthritis outside the defined age range, or treated in previous or subsequent years, were excluded, as well as those who presented an associated pathology of the upper limb that made it difficult to assess the affectation attributable to the trapeziometacarpal joint. Those who did not have X-rays available, or did not complete the questionnaires, were also excluded.
Patients diagnosed with trapeziometacarpal osteoarthritis were divided into 2 groups, according to the type of surgical or conservative treatment they had received. In the surgical treatment group, the techniques used were: trapecectomy with ligament plasty (FCR hemitendon, accessory abductor or suspension system), trapeziometacarpal arthrodesis and joint replacement prosthesis. In the conservative treatment group, unloader outhouses; analgesia; corticosteroid injection, and rehabilitation therapy, or combinations of these, were used.
One hundred patients were included in the study with a diagnosis of trapeziometacarpal osteoarthritis between 2013 and 2019 out of a total of 144 patients analysed. Both surgical and conservative groups consisted of 50 patients. There were 15 patients in the conservative group diagnosed with bilateral rhizarthrosis and another 15 in the surgical group, so that 65 observations per group were analysed. Twenty-four patients in the surgical group and 20 patients in the conservative group were excluded for not meeting the inclusion criteria or for lack of response to any of the questionnaires (Fig. 1). No patient in the conservative group underwent surgery during the follow-up period.
Demographic data including age, sex, laterality of the affected hand relative to the dominant hand, and profession, as well as the type of treatment performed, were collected retrospectively. The existence of a previous diagnosis of mood disorder or any other psychological factor, recorded in both the hospital and primary care records, as well as the presence of pain in other joints, was also identified. The degree of trapeziometacarpal osteoarthritis was classified by evaluating plain digitalised radiographs and using the Eaton-Littler classification12 as a grading method. All radiographs were analysed by the same surgeon. Socioeconomic level was determined according to the European Socio-Economic Classification [ESEC]),13 which segregates levels into 10 categories, from least disadvantaged (1) to most disadvantaged (10), and was developed jointly by the European Commission among several countries, making it very appropriate for international comparisons.
All patients treated and included in the analysis completed a series of questionnaires to assess their symptom severity, psychological status, and pain behaviour. The State-Trait Anxiety Inventory [STAI])14 is a tool designed to measure anxiety in adults, with a total score ranging from 0 to 63: 0–9, normal or no anxiety; 10–18, mild to moderate anxiety; 19–29, moderate to severe anxiety; and 30–63, severe anxiety. The Patient Health Questionnaire-9 (PHQ-9) is a 9-item questionnaire that assesses depressive symptoms. The Spanish version of this questionnaire has a score range of 0–27 and can be organised into 4 categories: 0–4 (minimal), 5–9 (mild), 10–14 (moderate), 15–19 (moderate to severe), and 20–27 (severe).15 The PHQ-9 was developed as a screening tool, with recommended cut-off scores of 8–11 for probable major depression. The Pain Catastrophising Scale (PCS) is a grading system that assesses feelings and thoughts about pain and contains 13 items across 3 dimensions (rumination, magnification, and despair). In its Spanish version, they are scored on a Likert scale from 0 to 4. The theoretical range of the instrument is between 0 and 52, with low scores indicating little catastrophism, and high values, high catastrophism.16
For assessment of the functional situation after the treatment, the abbreviated upper limb function scale (Quick-DASH) was used, a shortened 11-item version of the DASH,17 which is used to quantify the function of the upper limb; each item of the DASH is scored between 1 (no difficulty at all) and 5 (unable to do so), with higher scores indicating greater disability (11–55). The final score is obtained as an average (sum of n answers/n), obtaining a result from 1 to 5, which has been expressed as a percentage (subtracting 1 and multiplying by 25). A Q-DASH questionnaire was considered complete when at least 10 of the 11 possible items had been answered. Visual analogue scale (VAS) scores were also collected to estimate the presence of pain both before and after treatment and hand mobility was assessed using the Kapandji test. All patients had a minimum follow-up of one year (1–10 years).
Data analysisA descriptive statistical analysis was performed on both groups of demographic variables, as well as the presence of psychological factors prior to treatment and the type of profession according to the ESEC socioeconomic classification. Taking into account the type of variables used, their normality was assessed with the Shapiro–Wilk test. Variables with a normal distribution are summarised with mean and standard deviation (SD), while those that do not meet normality criteria are summarised as median and interquartile range [IQR]. For categorical variables, the numbers and percentages of each category with respect to the total are indicated.
An analysis was made of whether there was a relationship between the functional outcome of the treatment (post-treatment pain according to the EVA scale, Q-DASH results and mobility according to the Kapandji test), with the existence of previous psychological factors and the type of profession in each of the 2 groups. For this purpose, Fisher's exact test was used for categorical variables and Spearman's correlation coefficient for ordinal and continuous variables.
The existence of psychological comorbidities and socioeconomic classification were also studied, with the scores on the questionnaires on anxiety (STAI), depression (PHQ-9) and catastrophising behaviour in response to pain (PCS) using the Fisher exact test and the Spearman correlation coefficient, except for the STAI values, which were compared with the Student's t test.
The functional results achieved in each group and the presence of anxiety, depression and catastrophising behaviour in each of the groups were also compared, using the Wilcoxon 2-sample test.
For all comparisons, a level of statistical significance of p≤.05 was established. For the statistical analysis, the SAS tool (SAS Institute, Cary, North Carolina, USA) was used, and support was also available from the statistics department and from the centre's Biomedical Research Institute where the study was conducted.
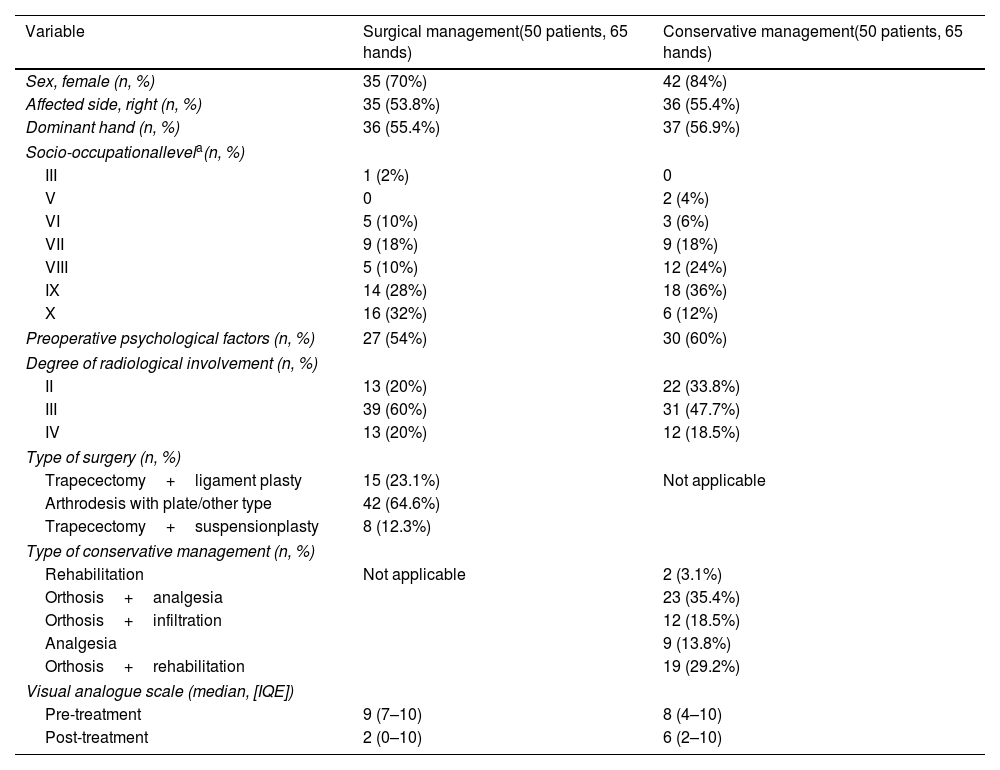
ResultsThe group of 100 patients, with 130 cases included in this retrospective study, had a mean age of 58.2 years. Twenty-three of the patients were men, with 6 bilateral cases (23.3% of the subjects), and 77 were women with 23 bilateral cases (66.7%). A mean of 7 years (1–18 years) had elapsed between surgery and the clinical assessment and aforementioned questionnaires, and a mean of 6 years (3–8 years) between conservative treatment and assessment for this study. Table 1 summarises the demographic data, profession; presence of previous psychological factors; radiological classification, and type of treatment received by each patient in both groups, in addition to the pain record according to the pre- and postoperative VAS scale and the scores on the functional and psychological scales.
Demographic and descriptive data of included patients.
| Variable | Surgical management(50 patients, 65 hands) | Conservative management(50 patients, 65 hands) |
|---|---|---|
| Sex, female (n, %) | 35 (70%) | 42 (84%) |
| Affected side, right (n, %) | 35 (53.8%) | 36 (55.4%) |
| Dominant hand (n, %) | 36 (55.4%) | 37 (56.9%) |
| Socio-occupationallevela(n, %) | ||
| III | 1 (2%) | 0 |
| V | 0 | 2 (4%) |
| VI | 5 (10%) | 3 (6%) |
| VII | 9 (18%) | 9 (18%) |
| VIII | 5 (10%) | 12 (24%) |
| IX | 14 (28%) | 18 (36%) |
| X | 16 (32%) | 6 (12%) |
| Preoperative psychological factors (n, %) | 27 (54%) | 30 (60%) |
| Degree of radiological involvement (n, %) | ||
| II | 13 (20%) | 22 (33.8%) |
| III | 39 (60%) | 31 (47.7%) |
| IV | 13 (20%) | 12 (18.5%) |
| Type of surgery (n, %) | ||
| Trapecectomy+ligament plasty | 15 (23.1%) | Not applicable |
| Arthrodesis with plate/other type | 42 (64.6%) | |
| Trapecectomy+suspensionplasty | 8 (12.3%) | |
| Type of conservative management (n, %) | ||
| Rehabilitation | Not applicable | 2 (3.1%) |
| Orthosis+analgesia | 23 (35.4%) | |
| Orthosis+infiltration | 12 (18.5%) | |
| Analgesia | 9 (13.8%) | |
| Orthosis+rehabilitation | 19 (29.2%) | |
| Visual analogue scale (median, [IQE]) | ||
| Pre-treatment | 9 (7–10) | 8 (4–10) |
| Post-treatment | 2 (0–10) | 6 (2–10) |
ESEC categories: III: high-level white-collar employee; VI: Supervisors and lower-ranking technicians; VII: lower-ranking service and trade workers; VIII: skilled manual workers; IX: unskilled workers; X: excluded from the labour market and long-term unemployed.
IQR: interquartile range.
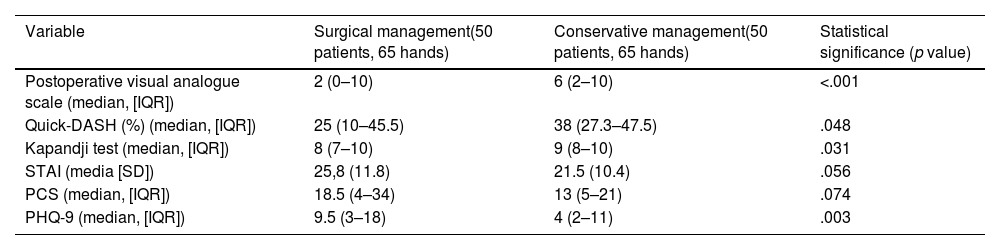
Patients treated surgically had better functional results on the Q-DASH and less pain on the VAS scale at the time of the study than patients treated conservatively, although mobility on the Kapandji test was lower. They also had higher scores on the 3 questionnaires used for mood disorders (STAI, PCS and PHQ-9), this comparison being statistically significant only for the PHQ-9 questionnaire, which assesses depressive symptoms (Table 2).
Comparison of functional outcomes and scores on anxiety, depression and pain catastrophising scales in patients managed surgically and conservatively.
| Variable | Surgical management(50 patients, 65 hands) | Conservative management(50 patients, 65 hands) | Statistical significance (p value) |
|---|---|---|---|
| Postoperative visual analogue scale (median, [IQR]) | 2 (0–10) | 6 (2–10) | <.001 |
| Quick-DASH (%) (median, [IQR]) | 25 (10–45.5) | 38 (27.3–47.5) | .048 |
| Kapandji test (median, [IQR]) | 8 (7–10) | 9 (8–10) | .031 |
| STAI (media [SD]) | 25,8 (11.8) | 21.5 (10.4) | .056 |
| PCS (median, [IQR]) | 18.5 (4–34) | 13 (5–21) | .074 |
| PHQ-9 (median, [IQR]) | 9.5 (3–18) | 4 (2–11) | .003 |
IQR: interquartile range; PCS: Pain Catastrophising Scale, measures pain catastrophising; PHQ-9: Patient Health Questionnaire-9, assesses depressive symptoms; SD: standard deviation; STAI: State-Trait Anxiety Inventory, assesses anxiety.
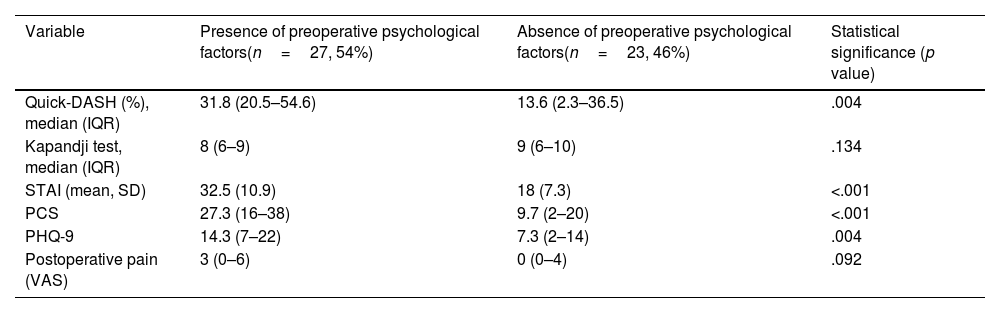
Among those patients treated surgically, 54% had a diagnosis of dysthymic disorder prior to treatment for trapeziometacarpal osteoarthritis. Patients without a previous diagnosis of mood disorder had better functional results on the Q-DASH questionnaire (median [IQR]: 13.6 [2.3–36.5]), than those patients with previous psychological factors (median [IQR]: 31.8 [20.5–54.6]; p=.004). No association was found between the previous diagnosis of psychological factors and the mobility or pain that patients presented after surgical treatment (Table 3).
Results of patients treated surgically, comparing the presence or absence of preoperative psychological factors.
| Variable | Presence of preoperative psychological factors(n=27, 54%) | Absence of preoperative psychological factors(n=23, 46%) | Statistical significance (p value) |
|---|---|---|---|
| Quick-DASH (%), median (IQR) | 31.8 (20.5–54.6) | 13.6 (2.3–36.5) | .004 |
| Kapandji test, median (IQR) | 8 (6–9) | 9 (6–10) | .134 |
| STAI (mean, SD) | 32.5 (10.9) | 18 (7.3) | <.001 |
| PCS | 27.3 (16–38) | 9.7 (2–20) | <.001 |
| PHQ-9 | 14.3 (7–22) | 7.3 (2–14) | .004 |
| Postoperative pain (VAS) | 3 (0–6) | 0 (0–4) | .092 |
IQR: interquartile range; PCS: Pain Catastrophising Scale, measures pain catastrophising; PHQ-9: Patient Health Questionnaire-9, assesses depressive symptoms; SD: standard deviation; STAI: State-Trait Anxiety Inventory, assesses anxiety; VAS: visual analogue scale.
Patients with dysthymic disorders had significantly higher scores on all 3 questionnaires for anxiety, depression, and pain catastrophising: STAI (mean [SD]: 32.5 [10.89] points (equivalent to severe anxiety) vs. 18 [7.26] points (mild or moderate anxiety), PHQ-9 (14.3 [7.00–22.00] points (equivalent to moderate depressive symptoms) vs. 7.3 [2.00–14.00] points (mild symptoms), and PCS (27.3 [16.00–38.00] points vs. 9.7 [2.00–20.00] points for patients with and without preexisting dysthymic disorders, respectively) with p<.05 for all comparisons (Table 4).
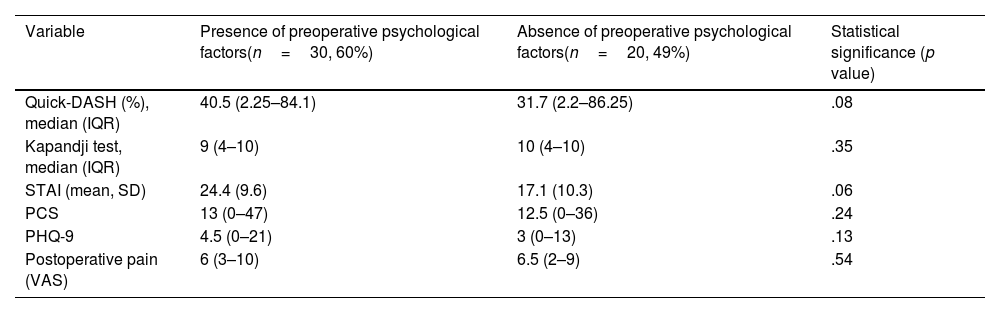
Results of patients treated conservatively, comparing between those patients who had pre and postoperative psychological factors.
| Variable | Presence of preoperative psychological factors(n=30, 60%) | Absence of preoperative psychological factors(n=20, 49%) | Statistical significance (p value) |
|---|---|---|---|
| Quick-DASH (%), median (IQR) | 40.5 (2.25–84.1) | 31.7 (2.2–86.25) | .08 |
| Kapandji test, median (IQR) | 9 (4–10) | 10 (4–10) | .35 |
| STAI (mean, SD) | 24.4 (9.6) | 17.1 (10.3) | .06 |
| PCS | 13 (0–47) | 12.5 (0–36) | .24 |
| PHQ-9 | 4.5 (0–21) | 3 (0–13) | .13 |
| Postoperative pain (VAS) | 6 (3–10) | 6.5 (2–9) | .54 |
IQR: interquartile range; PCS: Pain Catastrophising Scale, measures pain catastrophising; PHQ-9: Patient Health Questionnaire-9, assesses depressive symptoms; SD: standard deviation; STAI: State-Trait Anxiety Inventory, assesses anxiety; VAS: visual analogue scale.
Sixty-four percent of the patients treated surgically were long-term unemployed or unskilled workers. Only one patient was a skilled worker with a higher education level. Patients from the lowest socioeconomic levels on the ESeC classification scale had significantly higher scores on the STAI, PCS and PHQ-9 questionnaires (p<.05), suggesting greater anxiety, depression and pain catastrophising among patients from lower socioeconomic levels. No significant association was demonstrated between profession and the degree of postoperative pain, the Q-DASH score (p=.866) or mobility according to the Kapandji test (p=.220) after surgery.
Patients treated conservativelyRegarding the non-surgically managed group, 60% of patients had a diagnosis of mood disorder at the start of the study. No significant association was found between the presence of psychological factors and the results of the Q-DASH questionnaire, hand mobility or pain level after treatment. Patients with a previous diagnosis of psychological disorder had higher scores in the 3 questionnaires on depression, catastrophising behaviour towards pain and anxiety, with the only significant difference being for the STAI questionnaire (median [IQR]: 24.40 [9–45] points) for p<.02 (Table 4).
Ninety per cent of patients undergoing conservative treatment for trapeziometacarpal osteoarthritis were service or manual workers, unskilled workers or long-term unemployed. No significant association was found between the profession and the results of conservative treatment. No relationship was found between job performance and scores on questionnaires for anxiety, depression, and pain catastrophising.
DiscussionThe results of our study suggest that psychological comorbidities such as depression, anxiety, and pain catastrophising may influence the medium-term improvement experienced by patients after any type of surgical treatment for trapeziometacarpal osteoarthritis. Furthermore, the questionnaires used in our study for the diagnosis of psychological disorders have proven useful in predicting those patients diagnosed with rhizarthrosis who may experience a poorer surgical outcome.
Our findings are in line with other published data suggesting that depression and pain catastrophising may influence patient-perceived outcomes after upper limb surgery.18,19 For example, patients with symptoms of major depression reported disproportionate pain levels and had worse functional outcomes measured with the DASH questionnaire 2 weeks after minor hand surgery for carpal tunnel syndrome, trigger finger, or benign tumours.20 Similarly, psychological status was a predictor of perceived outcome after carpal tunnel surgery at 2 years of evolution, with patients diagnosed with depression being more dissatisfied.21 A cross-sectional study of patients treated for trapeziometacarpal osteoarthritis obtained similar results. In addition, there were no significant differences in the diagnosis of psychological comorbidities between patients who chose surgical and conservative treatment.22 Other authors demonstrated that, in patients with knee osteoarthritis treated with total arthroplasty, those diagnosed with depression and anxiety showed poorer functional outcomes and greater persistent postoperative pain from 3 months to 5 years after the intervention.23 However, in our study we found no significant association between the presence of psychological comorbidities and the functional results of conservative treatment. Dysthymic disorder was also present in 60% of patients in this group, showing higher scores in the questionnaires on psychological factors (STAI, PCS and PHQ-9), with a significant difference only for the STAI.
Given that the health area in which the research project was carried out is a depressed area of the community of Madrid, patients were classified according to their basic job, finding 4 types of possibilities: employers, self-employed, employees and those who were directly and involuntarily excluded from paid employment. Sixty-four per cent of patients undergoing any type of surgical treatment for rhizarthrosis were long-term unemployed and unskilled workers, and they had significantly higher scores on the questionnaires of anxiety, depression and catastrophic behaviour in the face of pain (STAI, PHQ-9 and PCS). No significant association was demonstrated between the socio-occupational level and the functional results of the intervention. We could deduce from this that patients from lower socioeconomic levels have a higher percentage of psychological disorders, but there is no direct association between their job category and the functional impact of the surgical treatment. In the group of patients undergoing conservative treatment, no evidence of a significant relationship was found, either with functional outcomes or with scores on mental health questionnaires. There are studies that have shown how socioeconomic deprivation is associated with a higher incidence of musculoskeletal diseases, and in most cases, the most disadvantaged patients incur higher health care costs.24 A systematic review25 concluded that unemployed patients had a worse prognosis, regardless of the treatment received and the severity of the depressive disorder, than patients with a job. Interventions to help the population to achieve or maintain employment, or to obtain stable housing, have been effective in improving quality of life, functioning and depressive symptoms.26
Patients treated surgically presented greater perceived functional improvement in the Q-DASH questionnaire and less post-treatment pain than patients treated conservatively. This finding may be related to the fact that the initial situation, both clinical and radiographic, was worse in this group. In addition, in the group of patients treated surgically, the scores on the psychological questionnaires were higher than in the group treated conservatively, although this was only significant for the PHQ-9 depression scale. We can conclude that pain related to the progression of the disease can cause frustration, anxiety and depression,27 although further studies are needed in this regard.
This is, to our knowledge, one of the first studies that includes socioeconomic inequality and psychological comorbidities for the study of the functional outcome of both surgical and conservative treatment of trapeziometacarpal osteoarthritis.
We are aware of the limitations of our study. Firstly, data from psychological questionnaires were collected after the treatment was applied to the patient, so it was difficult to distinguish whether it was a trigger or a consequence of the treatment, although the diagnosis of anxiety-depressive disorders prior to surgery was considered. In general, these patients presented higher scores in the questionnaires used on anxiety, depression and behaviour towards pain. However, both the STAI questionnaire and the PHQ-9 explicitly indicate in their instructions that the answers should be based on the current moment and the last 15 days, respectively. This means that temporary life events, such as an acute illness or, in the case of our cohort, hand pain, can influence the patients’ responses, so that the score may not be due only to a clinically diagnosed depression. This highlights the limitations inherent in research that attempts to study the effect of depression using a questionnaire in patients with other chronic health processes such as osteoarthritis.
Secondly, in both cohorts there were multiple types of interventions performed by multiple clinicians, and perhaps one type of treatment or particular style of doctor/patient relationship was more effective than another in particular subgroups of patients. Our study was not able to perform a subgroup analysis.
An additional limitation is that we defined all events (patient status, diagnosis, and treatment) based on patient responses and care provided in the clinic. We did not take into account changes in patient status, comorbidities that might influence patient perception of their condition, or the possibility of alternative treatments that might also affect the final outcome. Finally, there was also no group of patients diagnosed with trapeziometacarpal osteoarthritis who received no treatment at all, and therefore it is not possible to know whether the improvement shown in the surgical treatment group was due to the surgery, the natural course of clinical presentations, the placebo effect, or other unmeasured factors.
It has been hypothesised that assessment and treatment of depression, anxiety, and pain catastrophising could improve surgical outcomes, limit unnecessary interventions, reduce pain, and increase patients’ quality of life.28 Other authors have shown that treatment of depression and pain catastrophising with cognitive-behavioural therapy has led to improved psychological outcomes and reduced pain scores in patients with chronic pain.29
In the field of public health, understanding that socioeconomic disadvantages are associated with a higher rate of psychological comorbidities suggests that reducing socioeconomic inequalities could improve mental health. Knowing the prognosis of the disease according to the treatment received can help us limit the incidence of mental problems.30
It would be interesting to conduct additional studies to determine whether the use of questionnaires to diagnose psychological comorbidities and their treatment prior to surgery in patients with trapeziometacarpal osteoarthritis could produce an even more favourable postoperative functional outcome.
ConclusionsPatients with higher rates of depression, anxiety, and pain catastrophising behaviour showed significantly poorer functional outcomes (QDASH) in surgical treatment of trapeziometacarpal osteoarthritis. Socioeconomic class influenced levels of depression, anxiety, and pain behaviour in a selection of patients, but not the functional outcome of rhizarthrosis treatment. However, patients treated surgically had better functional outcomes and greater pain relief than those treated conservatively, although trapeziometacarpal joint mobility was lower in the surgical group.
Level of evidenceLevel of evidence iii.
Ethical considerationsThe authors took into account the “Ethical responsibilities” contained in these stipulations, including: (a) that the procedures followed in the research match the ethical standards of the responsible committee on human or animal experimentation (institutional or regional) and are in accordance with the World Medical Association and the Declaration of Helsinki; (b) that they guarantee the right of their patients to privacy and confidentiality as described in the corresponding section of these rules, and that any type of identifying data in text or images has been avoided in the article and, in any event, (c) that they are in possession of informed consent from the patients to participate in the study and to publish the results in print and electronic format (Internet) in the REVISTA ESPAÑOLA DE CIRUGÍA ORTOPÉDICA Y TRAUMATOLOGÍA and that they have declared this to the EES.
FundingThis project was funded by the SECOT Foundation, within the scholarships for research projects awarded in 2022.
Conflict of interestsOne or more of the authors of this work have declared potential conflicts of interest, which may include the receipt of direct or indirect payments, and institutional support or that related to an entity in the biomedical field.