Scapular Notching is a problem frequently seen in Reverse shoulder arthroplasties (RSAs), produced by a collision between the humeral component and the scapula. The main objective of this study is to analyze whether this problem decreases with the surgeons experience. As secondary objectives, assessing whether there is a relationship between its appearance and the clinical and functional outcome of patients.
MethodsWe retrospectively reviewed 101 patients with 105 RSAs; we analyzed complications, focusing on scapular notching. Main follow-up time was 36 month (12–72). The clinical and functional outcomes were evaluated with the Constant scale and the QuickDash questionnaire.
ResultsForty-two patients (40%) had some degree of scapular notching. Of these, 25 patients had grade I, 14 had grade II and 3 had grade III notching. The average postoperative Constant score for the entire series was 60.72. A tendency toward a reduced incidence of notching was observed with increasing numbers of operated cases and experience of the surgeon (p = 0.04). In the group of patients who had notching, the average postoperative Constant score was 56, and in the group that developed notching, the average score was 63. Patients with notching had significantly lower pain scores (p = 0.012).
ConclusionsScapular notching is a common problem of RSA. In RSA, the experience of the surgeon reduces the appearance of problems and complications. Scapular notching is related to poorer clinical outcomes with respect to pain.
La erosión o muesca escapular (notching escapular) es un problema que se observa con frecuencia en las prótesis invertidas de hombro, producido por un choque entre el componente humeral y el cuello de la escápula. El objetivo principal de nuestro trabajo es analizar si disminuye el notching escapular con el aumento de la experiencia del cirujano. Como objetivos secundarios, el valorar si existe una relación entre su aparición y el resultado funcional y clínico en los pacientes.
Material y métodosSe realiza una revisión retrospectiva de 101 pacientes con 105 prótesis invertidas de hombro, valorando radiográficamente la aparición de notching escapular. El tiempo medio de seguimiento fue de 36 meses (rango, 12–72). Se objetivan los resultados clínico-funcionales con la escala Constant y el cuestionario QuickDash.
ResultadosCuarenta y dos pacientes (40%) presentaron algún grado de notching escapular. De ellos, 25 pacientes tenían un grado I, 14 un grado II y tres un grado III. El Constant postoperatorio medio para toda la serie fue de 60,72. Se observó una tendencia a disminuir la incidencia de notching conforme aumentaba el número de casos intervenidos y la experiencia del cirujano (p = 0,04). En el grupo de los pacientes que presentaban notching escapular, el Constant postoperatorio fue de 56 y en el grupo que no desarrolló notching fue del 63. Los pacientes con notching presentaban puntuaciones inferiores en cuanto al dolor siendo la diferencia estadísticamente significativa (p = 0,012).
ConclusionesEl notching escapular es un problema frecuente en las prótesis invertidas de hombro, en las cuales la curva de aprendizaje influye positivamente en la diminución de su aparición. La aparición de notching escapular está relacionado con peores resultados clínicos en cuanto al dolor se refiere.
Since its introduction by Grammont in 1985,1 reverse shoulder arthroplasty has become widely accepted treatment for the management of shoulder arthropathy due to massive rotator cuff tears.2–7 The satisfactory outcomes obtained have led to the indications for reverse arthroplasty extending to other conditions in which the rotator cuff is not functional, such as massive rotator cuff tears without osteoarthritis, post-traumatic osteoarthritis, prosthetic revision, acute fractures, or inflammatory diseases such as rheumatoid arthritis accompanied by cuff tears.7–13
However, the number of complications and problems that arise from this surgery is much higher than with anatomical prostheses. Zumstein et al.14 report complication rates of 24%, as well as a reoperation and revision rate of 13.5% for reverse shoulder prostheses.
Scapular erosion or notching is one of the most common problems following shoulder replacement surgery. Its incidence has been reported to be around 35%–96%.6,14,15 It is a mechanical problem where scapular notching is caused by impingement between the humeral component of the prosthesis and the scapular neck. It is not yet clear whether scapular notching has any effect on the clinical outcomes of reverse prostheses or whether it can lead to loosening of the glenoid component over time. However, it remains an important concern, especially with the use of reverse prostheses in young people.
The aim of our study was to observe the occurrence of scapular notching in our series of reverse prostheses and to see whether the condition decreased as surgeons gained more experience in fitting them.
Our secondary objectives were to assess whether there is a relationship between occurrence of scapular notching and patients’ functional and clinical outcomes. The null hypothesis was that the percentage of scapular notching in this type of surgery would decrease with acquired experience and surgical skills.
Material and methodWe retrospectively reviewed all reverse shoulder arthroplasties performed consecutively in our centre from January 2007 to January 2013. We included in the review all the reverse prostheses placed during this period, using the deltopectoral approach, regardless of the reason for placement of the prosthesis. Patients who had died at the time of the review, patients who could not be located, and those in whom an approach other than the deltopectoral approach was used were excluded from the study. The mean follow-up time was 36 months (range, 12–72).
All patients, except those in whom the reverse prosthesis was implanted after an acute fracture, were assessed preoperatively by recording active range of motion with a goniometer and measuring strength with a dynamometer. Preoperative imaging included plain radiography in the anteroposterior plane of the scapula in internal rotation, neutral and external rotation, and computed tomography or magnetic resonance imaging was used to assess rotator cuff integrity and glenoid erosion.
All the surgeries were performed by shoulder surgeons.
All patients were operated using a deltopectoral approach, with the patient placed in the beach chair position, paying special attention to the subscapularis tendon which was reinserted with transosseous stitches at the end of the procedure in cases where the tendon was intact.
The postoperative rehabilitation protocol was the same for all patients. The shoulder was immobilised for one month in a sling, with the arm in internal rotation. Passive mobility with pendular exercises was allowed from the first postoperative day, avoiding external rotation beyond 0° and elevation above 90° to allow for subscapularis healing.
Intraoperative or postoperative complications and problems were recorded according to the definition proposed by Zumstein et al.14 Zumstein et al. define "problem" as any intraoperative or postoperative event that is unlikely to affect the patient's final outcome, including radiographic images of scapular notching, and define "complication" as any intraoperative or postoperative event that is likely to negatively influence the final outcome, such as fractures, dislocations, aseptic loosening, or nerve palsies.
All patients were evaluated clinically and radiographically by an independent examiner. The Constant and Murley scale (absolute and age- and sex-adjusted) and the QuickDASH (Disabilities of the Arm, Shoulder and Hand) questionnaire were used for the clinical assessment. The Constant and Murley scale16 was completed by one of the authors in the presence of the patient, while the QuickDash questionnaire was completed by the patients themselves without the presence of either author.17 The force measurement method for the Constant scale was performed with 45° abduction for four seconds with the IDO dynamometer (Isometer, Innovative Design Orthopaedics, London, UK) placed on the wrist, recording the average maximum force of three measurements. In addition, subjective pain data were collected using the visual analogue scale (VAS). The radiographic examination assessed the position of the implants, the existence of radiolucency lines around the implants, the finding of heterotopic calcifications, and the presence of inferior scapular notching, assessed according to the Sirveaux classification.5
An independent investigator performed the statistical analysis. Data were summarised as mean and range for continuous variables and absolute and relative values for categorical variables. A linear model, followed by a Tukey contrast analysis was used to analyse the differences in Constant values between diagnoses. Another linear model was used to assess the influence of the degree of notching on the Constant values. The likelihood of occurrence of notching as a function of the number of previous operations of the surgeon was analysed using a linear logistic mixed model. P-values less than .05 were considered statistically significant. R (version 3.1.1) and the R mgcv package (version 1.8-4) were used for all analyses and graphs.
ResultsWe retrospectively reviewed a series of 118 consecutive reverse shoulder arthroplasties performed in our centre from January 2007 to January 2013. Thirteen patients were excluded from the study because they did not meet the inclusion criteria, nine of them because they had died, three because they could not be located at the time of the study, and one because they underwent a different approach (transdeltoid). A total of 105 prostheses were evaluated in 101 patients (four bilateral) with a mean age of 70 years (range, 51–88). The sample consisted of 20 men (19.8%) and 81 women (80.2%). The mean follow-up time was 36 months (range, 12–72).
Thirty-nine prostheses (37.1%) were implanted for irreparable massive rotator cuff tears, 28 (26.6%) for rotator cuff tear arthropathy, nine (8.5%) for post-traumatic sequelae, eight (7.6%) after an acute proximal humerus fracture, and five (4.7%) for acute proximal humerus fracture, 5 (4.7%) for primary osteoarthritis, 1 (0.9%) was placed in a shoulder affected by rheumatoid arthritis, 6 (5.7%) in the context of a long-standing shoulder dislocation and 1 (0.9%) for a pseudarthrosis of the proximal humerus. The series also includes 8 revision prostheses, 3 after failed hemiarthroplasty for primary osteoarthritis and 5 after painful hemiarthroplasty for fracture of the proximal humerus.
The prosthesis models used in this series included 68 SMR (LimaCorporate, Udine, Italy), 15 Delta III, 19 Delta Xtend (Depuy, Warsan, In, USA) and 3 Aequalis Reverse II (Tornier, MN, USA).
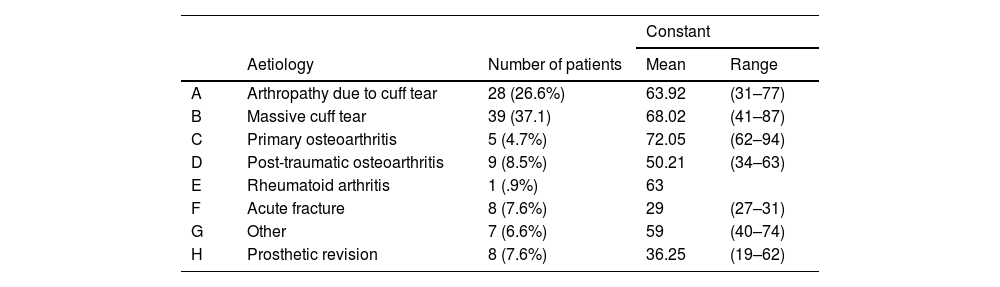
The postoperative Constant score for the entire series was 60.72 ± 4.3. According to aetiology, patients who underwent surgery for post-traumatic osteoarthritis or prosthetic revision achieved significantly lower scores than those operated on for massive cuff tear, cuff tear arthropathy or primary osteoarthritis (p < .05) (Table 1). Similarly, patients undergoing prosthetic revision had worse clinical outcomes, resulting in significantly higher Quick-Dash scores than the rest (p < .001).
Constant score according to aetiology.
| Constant | ||||
|---|---|---|---|---|
| Aetiology | Number of patients | Mean | Range | |
| A | Arthropathy due to cuff tear | 28 (26.6%) | 63.92 | (31–77) |
| B | Massive cuff tear | 39 (37.1) | 68.02 | (41–87) |
| C | Primary osteoarthritis | 5 (4.7%) | 72.05 | (62–94) |
| D | Post-traumatic osteoarthritis | 9 (8.5%) | 50.21 | (34–63) |
| E | Rheumatoid arthritis | 1 (.9%) | 63 | |
| F | Acute fracture | 8 (7.6%) | 29 | (27–31) |
| G | Other | 7 (6.6%) | 59 | (40–74) |
| H | Prosthetic revision | 8 (7.6%) | 36.25 | (19–62) |
Nine patients (8.5%) had complications. These included three glenoid loosening, three prosthetic instabilities (two of which required reoperation) and three infections (which were treated by two-stage replacement). In terms of radiographic changes, 40% had scapular notching and 14.3% had heterotopic ossification images.
Forty-two patients (40%) had some degree of scapular notching. Of these, 25 patients had grade I, 14 had grade II, and 3 had grade III. Since this is a radiographic diagnosis, if the projection is not good, notching cannot be ruled out in that patient, and therefore we labelled these cases as not assessable (5%).
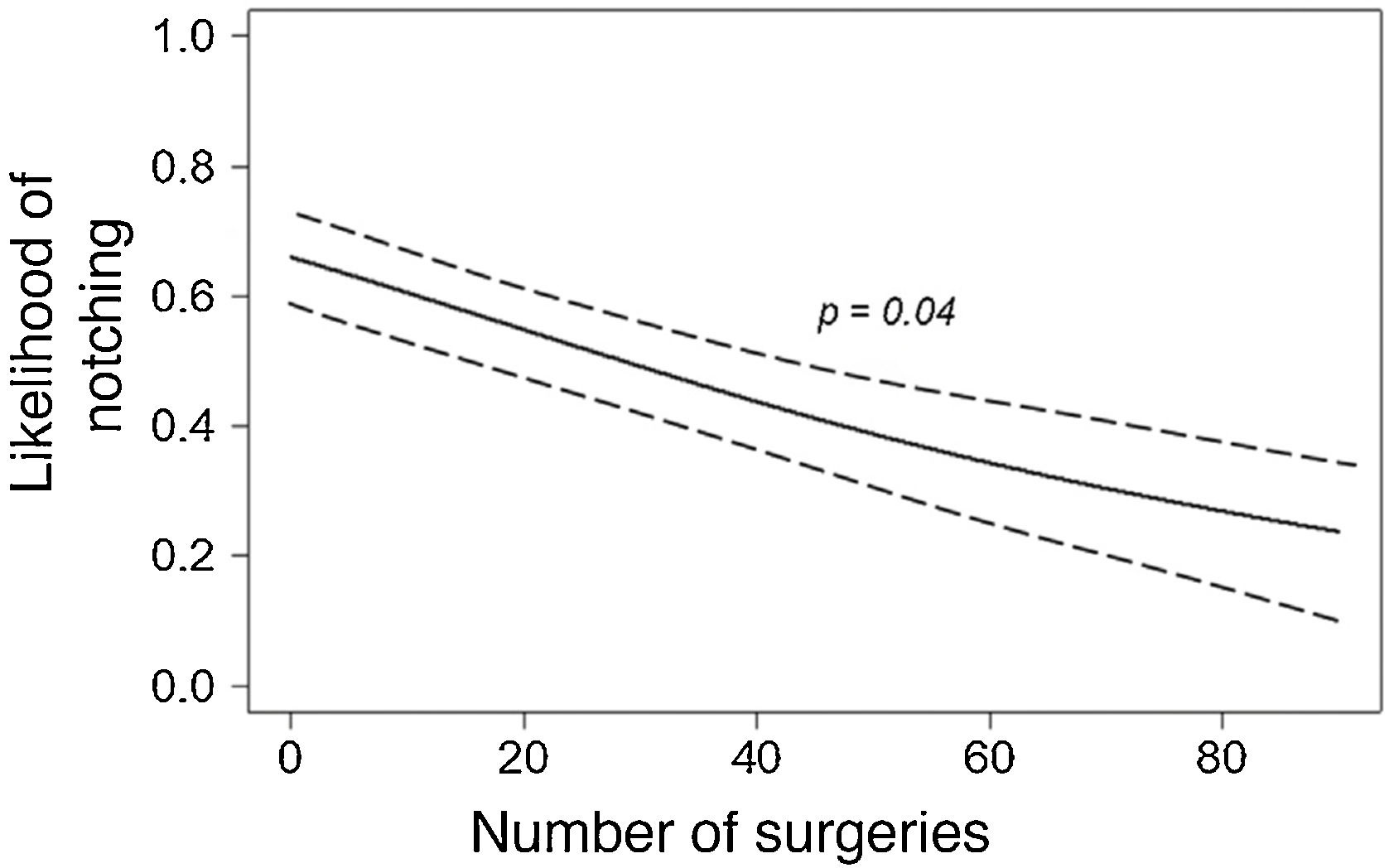
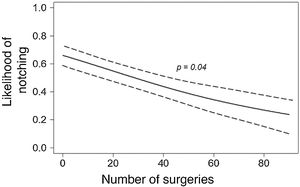
Notching occurred in all cases during the first 12 months after surgery, occurring in the first three months in 19 prostheses, between the third and sixth month in 13 prostheses, between the sixth and ninth month in 6 prostheses, and in the fourth postoperative quarter in 4 prostheses. Scapular notching appeared in 63.3% of the first 30 prostheses implanted, while in the next 70 prostheses this percentage decreased to 29.3%. Fig. 1 shows the decrease in the tendency to develop scapular notching as the number of reverse arthroplasties performed in our centre increases (p = .028), with a likelihood of .2 (20%) at the end of the series.
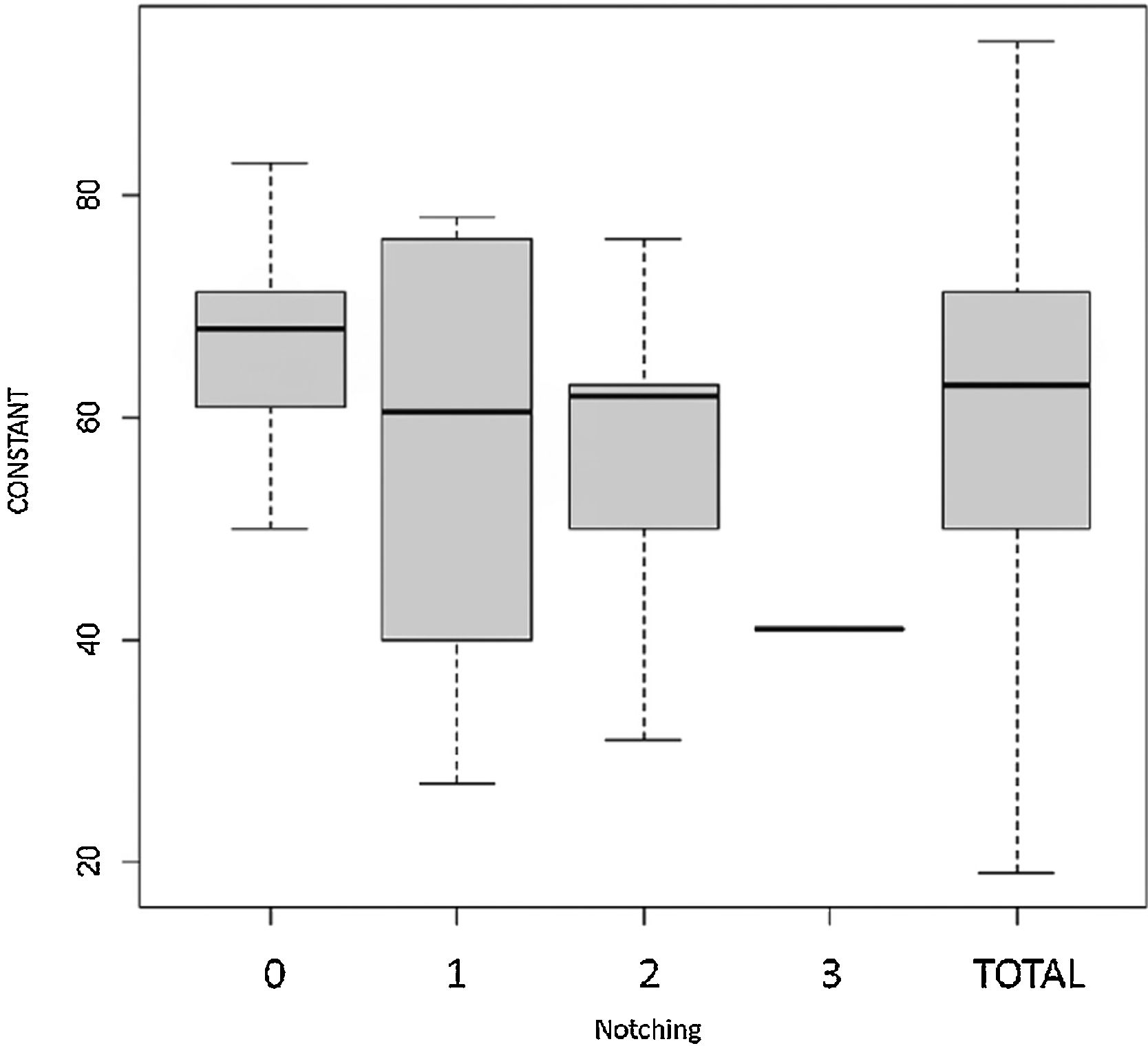
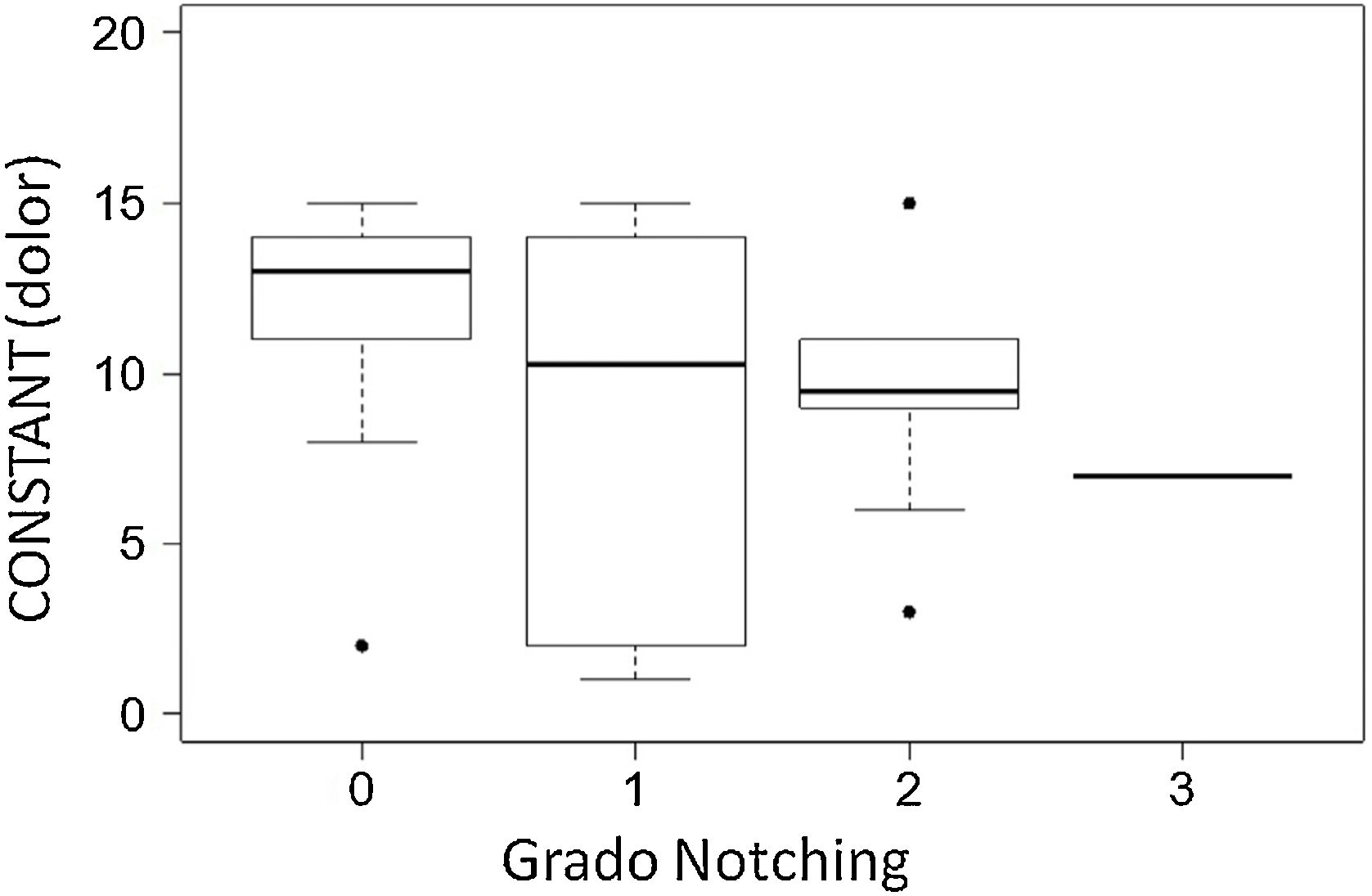
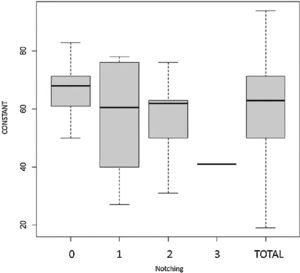
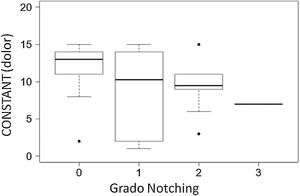
Patients with scapular notching tended to have lower Constant scores (mean 56) than those who did not develop scapular notching (mean 63), this difference was not statistically significant (Fig. 2). In contrast, the presence of notching in any of its degrees is associated with a lower Constant pain score, this difference being statistically significant (p = .012) (Fig. 3).
DiscussionAs shown in the results, 40% of the patients had some degree of scapular notching. However, Fig. 1 shows that the occurrence of scapular notching decreases as the number of prostheses fitted in our centre increases. In our series there is a clear trend towards a decrease in the occurrence of scapular notching – expressed in terms of likelihood – over time. At the end of follow-up, the likelihood of notching was .2. There are numerous proposals in the literature to avoid scapular notching.
Wilde et al.18 conclude that inferior placement of the glenoid component is the most effective measure to prevent scapular notching. Our experience corroborates these studies, as inferior placement of the glenoid component is the main measure we have adopted to reduce the frequency of this problem. In the first prostheses placed in our hospital, the glenoid component was placed very centrally on the glenoid, which favoured the occurrence of notching. As surgeons gained experience and following the recommendations of published studies, the glenoid was placed increasingly lower, thus reducing the occurrence of scapular notching. This learning curve, which we consider essential for any professional starting to perform shoulder replacement surgery, can be shortened over time with certain biomechanical concepts, especially when placing the glenoid component. In addition, for better visualisation of the glenoid, we recommend a deltopectoral approach.
Increasing the diameter of the glenosphere and lateralisation of the centre of rotation are the other two main measures to reduce the likelihood of scapular notching.19–22 In a recent study, Torrens et al.23 describe less scapular notching occurring with the use of larger glenospheres than with the use of smaller, eccentric glenospheres, although with no significant differences between the two groups. Despite increasing the size of the glenosphere and lateralising the centre of rotation, in our series we have not been able to improve the likelihood of scapular notching from .2 in the last prostheses fitted.
Walch et al.24 find that complications decrease as the surgeon’s experience increases. However, they do not find a decrease in the occurrence of scapular notching as experience increases.
The reverse shoulder arthroplasty is a workable solution for shoulder arthropathy secondary to irreparable rotator cuff injury. Its good clinical results have made it an option to consider in other conditions, extending its indications to other pathologies. However, we must emphasise that aetiology influences the patient’s clinical and functional outcomes. In our series, and as confirmed by previous studies,6,25 we found better clinical and functional outcomes in both Constant and Quick-Dash scores in patients undergoing reverse shoulder arthroplasty for massive rotator cuff tear, cuff tear arthropathy, or primary osteoarthritis. Those who underwent surgery for post-traumatic osteoarthritis, acute fracture or prosthetic revision had worse outcomes.
We found high rates of scapular notching (40%), similar to those published in the literature with prostheses of a similar design. Zumstein et al. published an incidence of scapular notching of 35.4% in their meta-analysis14 and Simovitch et al. published rates of 44%.15
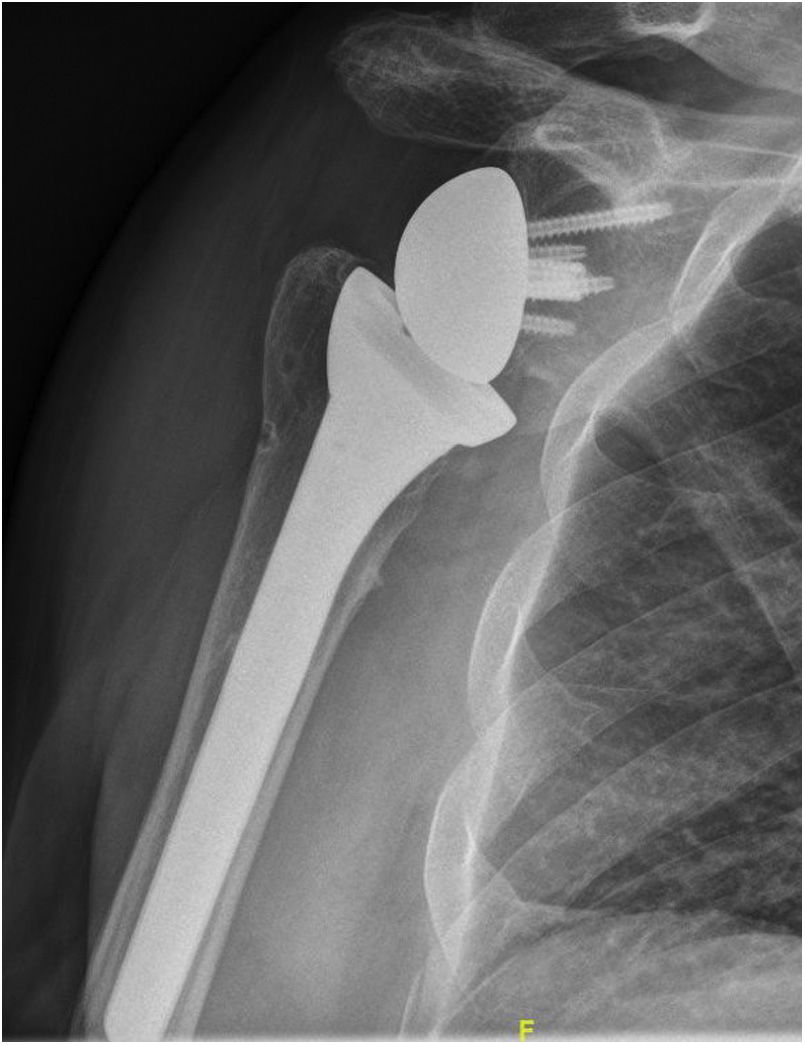
Our study also confirms the findings of Simovitch et al. who observed that if scapular notching occurs, it does so in the first 14 months.15 In all patients who presented with scapular notching images, it appeared in the first 12 months and remained stable over time. However, Lévigne et al. publish data suggesting the opposite, with a direct relationship between scapular notching and progression time.26 In our series, most of the patients who presented radiographic images of scapular notching were type I or II according to the Sirveaux classification, only three cases were type III (Fig. 4). Although the mean follow-up time was 36 months, further studies are needed to clarify the effects of scapular notching on the stability of the glenoid component, even in mild grades.
There is controversy in the literature regarding the influence of scapular notching on clinical and functional outcomes.5,15,26–28 Some studies have linked scapular notching to worse clinical outcomes. In contrast, other authors such as Lévigne et al.26 found no differences in clinical outcomes based on the presence or absence of scapular notching. Most widely accepted in the scientific literature seems to be that scapular notching has a negative influence on the stability of the glenoid component, causing it to loosen.5,18,29
We could not find statistically significant differences in Constant scores between patients who had some degree of scapular notching and those who did not (Fig. 2). In contrast, our series does show a statistically significant association between the presence of scapular notching and a worse pain score (Fig. 3). Patients with scapular notching grade I had more pain than patients without notching. Patients with scapular notching grade II and III had worse results than those with grade I, and all these associations were statistically significant. Therefore, like Simovitch et al.,15,27 we believe that scapular notching is not only a biomechanical problem, but also a clinical problem.
It is possible that the failure to completely eliminate scapular notching is due to the design of the prostheses used, with an angle of 155 ° that facilitates impingement of the humeral prosthetic component against the external scapular pillar. Other designs with sharper cutting angles have managed to reduce this complication.30
Our study has some limitations to consider. The first is inherent to its retrospective design. Secondly, we do not have a long follow-up period, the mean being 36 months. Thirdly, the inclusion within the study of different pathologies leading to the reverse shoulder arthroplasty could be considered a limitation, as some are related to a lower incidence of scapular notching. For example, in reverse prostheses placed for fractures, the wide glenoid exposure during surgery favours more accurate placement of the glenoid component. Fourthly, only the measurement of the grade of scapular notching is assessed by plain radiographic study. Finally, including three different reverse prosthesis models may also condition the final results.
ConclusionThe results of our study suggest that the occurrence of scapular notching after reverse shoulder arthroplasty has decreased as the surgeons’ experience has increased. This is possibly related to the fact that positioning of the glenoid component has improved (positioned more inferiorly) in the learning curve. The occurrence of scapular notching is related to a lower Constant pain score, although no statistically significant differences in total Constant score were found between patients with scapular notching and patients without notching. Further long-term studies are needed to determine whether comparable results are sustained over time.
Level of evidenceLevel of evidence III.
Conflict of interestThe authors declare no conflict of interest regarding the research, authorship, and/or publication of this article.
FundingThe authors declare that they have received no funding for the conduct of the present research, the preparation of the article, or its publication.
Data confidentialityThe authors declare that they have followed the protocols of their work centre regarding the publication of patient data. The publication of patient data and that no patient identifiable data appear in this study.
Right to privacy and informed consentThe authors declare that this study does not contain data that would allow the identification of the patient.
Please cite this article as: Alonso Pérez-Barquero J, Aroca Navarro JE, Navarro Bosch M, de la Calva Ceinos C, Pina Medina A. Notching escapular en las prótesis invertidas de hombro. Su relación con la experiencia del cirujano y con los resultados clínicos. Rev Esp Cir Ortop Traumatol. 2022;66:2–8.