Body donation is in the basis of transplantation programs, founded on receptor and donor rights. Nevertheless, if the purpose is not directed to healthcare, the regulation is different both in live or deceased individuals.
“Imaging techniques” generates digital files containing the “virtual body” of the patient, raising a new possibility: virtual body donation, which is not regulated in Spain and would not be compliant with legal requirements for other ways of donation.
A pioneer program for virtual body donation is presented, analysing its characteristics, medico-legal issues, organisation and functioning.
Having an unlimited number of virtual specimens (normal and pathological) could support a new way for teaching and research. These resources would also have the advantage of learning virtual biopsy (virtopsy).
It is thought that these programs, pioneers in Spain, could be useful for introducing similar initiatives that would have unlimited applications in teaching and research both in forensic and morphological sciences.
La donación corporal es la base de los programas de trasplantes, cuya regulación se fundamenta en los derechos del donante y receptor.
Sin embargo, si su objetivo no es asistencial, la normativa difiere tanto en vivos como en fallecidos.
Las llamadas «técnicas de imagen» permiten obtener ficheros digitales con el cuerpo virtual del paciente, lo que brinda una nueva posibilidad: la donación corporal virtual, no regulada en España y tampoco ajustada a la normativa del resto de las donaciones.
Presentamos un programa de donación corporal, analizando sus características, aspectos médico-legales, clínicos, de organización y funcionamiento.
Contar con un número ilimitado de especímenes virtuales impulsa una nueva forma de docencia e investigación. Tiene, además, ventajas para la formación de los profesionales en técnicas de autopsia virtual.
Creemos que este programa, pionero en España, puede servir para extender iniciativas similares de utilidad ilimitada en docencia e investigación en ciencias forenses, morfológicas y afines.
Donating body parts for clinical purposes forms the basis of the organ and tissue transplant programs: the Spanish model is one of the most respected world-wide.1,2 Legislation for these programs3 takes both receptor and donor rights into consideration.4,5
However, if the objective of the donation is not healthcare but, for example, education or research, the legislation is different. It is usually established by Faculties of Medicine based on donor-institution agreement. In Spain, each faculty manages donations according to its own criteria. In practice, written consent signed during the donor's lifetime constitutes the principal rule.6 Body donation for educational or research purposes involves evident ethical and healthcare problems.7 Apart from that, only a limited number of bodies are currently available, insufficient for academic or research needs.
Medical diagnosis has recently experienced a revolution with the incorporation of “imaging techniques” (computed tomography [CT] scan, magnetic resonance imaging [MRI], positron-emission tomography [PET], etc.). Despite the name, any of these tests generate digital files that contain not only a viewable representation of the organism (image), but also other data that can be analysed or transformed.
This brings us to a new possibility of donation for use in education or research: virtual body donation (VBD). However, such donation is not regulated in Spain, nor does it fit completely the legislation established for the rest of donations.
In this study, we analyse the clinical and legal issues of a VBD program recently introduced in our hospital. We believe that its features, as well as the clinical and legal issues underlying its creation and functioning, can serve as a guide for other similar programs in Spain or outside of it, and can boost this type of donations.
Having an unlimited number of body parts (both normal and pathological) available can provide the momentum for a new form of education and research in anatomy and other related sciences, such as pathology and forensic anthropology. In addition, this program possesses clear clinical advantages for training of professionals and for research applied to healthcare.
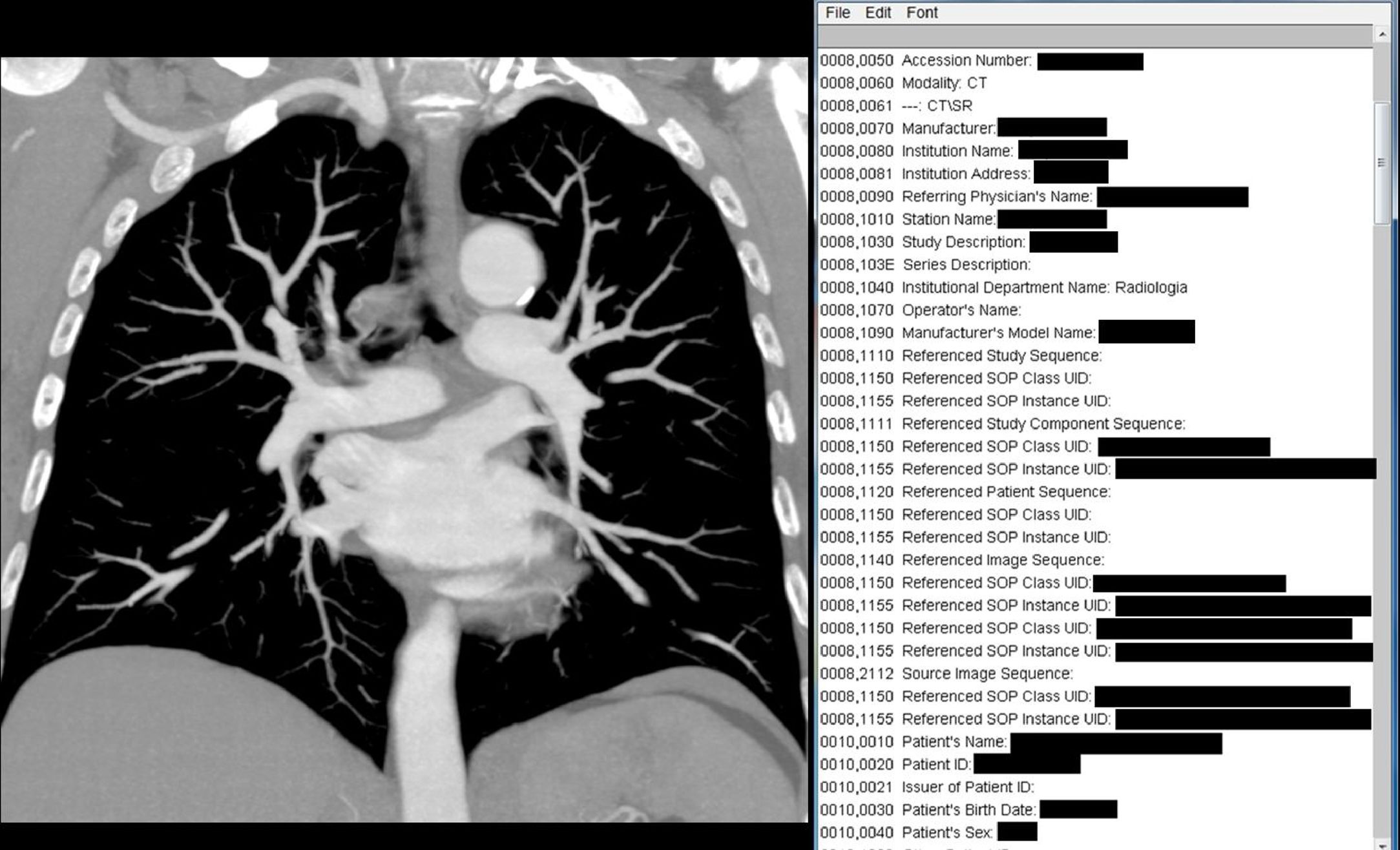
Material and methodsMedical imaging and virtual donationMedical imaging is based on files that follow the Digital Imaging and Communications in Medicine (DICOM) protocol. Images are obtained from tests such as MR, CT and others, and they are stored in the Picture Archiving and Computer System (PACS) of the hospital.8 The DICOM protocol was developed for CT and MR images by the National Electrical Manufacturers Association and the American College of Radiology.9
A DICOM file contains a header with data about the patient (such as the name, date of birth, weight and other facts) and the acquisition (type of imaging technique, place, hospital name and the like), together with image information (calibration, grey levels, bits per pixel, resolution and so forth).10 The file is like a stack of images described by an index, which is called DICOMDIR. This allows us to “pile up” the images and generate a three-dimensional (3D) reconstruction of the area.
We can visualise the files and take action, either on the raw images (cuts from the series) or on the reconstructions (multiplanar, volume, surface, etc.). This interactive visualisation also makes it possible to manipulate the model (such as move it, cut it, clone it, duplicate it and separate its fragments or organs, for example). The actions are performed using analysis and image processing tools (application programming interface [API])11 that make it possible to obtain all types of cuts, views, 3D models and so on.
After applying these techniques, we normally obtain new elements, such as a volume with a single organ. These new “objects” can be placed in different interaction and visualisation settings: for example, in a computer, but also in augmented or virtual reality, or printed in 3D. This is useful in the healthcare environment because it makes it possible to practice interventions, develop new techniques, plan operations, navigate in real time and so forth. But it is also of use in education and research and for forensic purposes: for example, we can practice virtual autopsy (virtopsy) techniques with these specimens or study injury biomechanics in bone fractures.
Medico-legal issues in a virtual donation programIn the first place, the virtual body donors are live patients who are consequently in full exercise of their legal capacity. In the second place, virtual donation does not affect the integrity of the subject, given that it is not an invasive procedure.
Consequently, the basis of these donations is the will of the patient, freely exercised, after receiving information about the characteristics, purpose, advantages and drawbacks of the procedure. In other words, the basic element of these donations is informed consent.
Informed consentIn Spain, informed consent is regulated by Law 41/200212 and by autonomous-community provisions that are very similar to that legislation. Article 2.2 in that law establishes that “every action in the healthcare setting requires, as a general rule, prior consent from the patients or users. Consent, which must be obtained after the patient receives adequate information, will be given in writing in the circumstances referenced in the law.”
The interest of VBD lies in the possibility of using specimens in tasks that differ from healthcare purposes. It is clear that, for healthcare use, the patients have already given their consent. In the case of VBD, it would be a matter of discussion as to whether we find ourselves in a healthcare activity or not, because the purpose is not directly healthcare-oriented.
The law uses the term setting, so once the healthcare action has begun, the setting for obtaining consent for a VBD will be healthcare. Consequently, informed consent is required. However, Article 3 defines informed consent to be “the free, voluntary and conscious agreement of a patient, manifested in the full use of his or her faculties after receiving adequate information, for an action that affects his or her health to take place.”
Given that VBD does not “affect the health of the patient,” it should be understood that informed consent, as stated in this law, is not applicable to VBD with non-healthcare purposes. There is consequently a certain legal void that would place VBD for teaching or research purposes outside the scope of that law.
On the other hand, Article 8.4 indicates that all patients or users have the “right to be warned about the possibility that the prognostic, diagnostic and therapeutic procedures that might be applied to them could be used in an educational or research project, which will not in any case involve additional risk for their health.”
Theoretically, this article would cover both the patients who have not given their written consent to the healthcare action and those who did indeed give such consent. Consequently, it could be interpreted to mean that the DICOM files of any patient could be used for education or research, as long as the patient has been advised of this possibility, in conformity with what is established in the law.
However, in practice this poses various problems. The first stems from the fact that patients who have not signed a consent document are not normally advised that their tests may be used for education or research. In general, invasive test protocols contain this indication, but this does not occur in the other examinations. Specifically, the majority of consents for x-ray examinations do not warn the patient about the possibility of a non-healthcare use.
In Spain, Law 14/2007 (3 July) on Biomedical Research13 regulates, among other issues, the use of invasive procedures in research. However, the virtual donation program has no place in that law, given that it does not involve research itself and, above all, the purpose of the tests donated has been exclusively healthcare-related.
Right to privacy and professional confidentialityThe second problem has to do with the fact that the DICOM contain a large amount of personal information (metadata) such as patient sex, age, weight, date of birth, date and type of exam, time of the examination, physician ordering the procedure, hospital where performed and many additional facts (Fig. 1). This means that third parties involved in education or research could access these data.
The third problem is that 3D reconstruction provides a very exact image of the specific anatomical part. The subjects can be recognised, because their features are faithfully reproduced. Other anatomical parts, such as genital organs, can be visualised as well. Patients are unaware of these possibilities and might not agree to the fact that third parties could recognise them or could inspect these body areas. They believe that these tests are visualised as X-rays, and they are surprised when they are shown reconstructions of their faces.
Article 16.3 in Law 41/2002 establishes that access to a patient's case history for judicial, epidemiological, public health, research or educational purposes is governed by the dispositions in Organic Law 15/1999, of 13 December, on Protection of Data of a Personal Nature, and in Law 14/1986, of 25 April, General Healthcare, and by other regulations applicable to each case. This makes it obligatory to store the personal identification data separately from clinical-healthcare data to ensure patient anonymity, unless the patient him- or herself consents to keeping such data together.
Healthcare data is separated from identifying data (the DICOM are identifying). The need for an ad hoc informed consent for virtual donations is clear, because the post-processing result (3D objects, volumes, and the like) could otherwise remain disconnected from a patient's clinical variables. This would seriously affect many research issues. The Biomedical Research Law13 establishes in Article 5.2 that “the assignment of personal data to third parties outside the medical-healthcare activity or to biomedical research will require express written consent from the party concerned.”
Another problem arises from potential transfer of patient files to third parties to, for example, generate personalised implant models. This would have a healthcare purpose; however, transferring the material to third parties without the patient's knowledge and authorisation could infringe data protection legislation, given the special characteristics of these DICOM files. The situation is even more complex if the companies have business interests and use the material transferred for purposes other than healthcare in the specific case.
Consequently, for examinations involving DICOM files, the patient should be informed about all these matters and should grant written consent for any non-healthcare purpose.
This would be in the same line as the European Union legislation on protection of physical persons with respect to personal data and its free circulation.14
Bearing in mind everything that we have been considering, we feel that the best way to ensure patient rights is a virtual donation program with sufficient information on these files and their characteristics. The issues that we have been analysing related to the attributes of DICOM files are not included in any informed consent protocol in healthcare centres in our country. For that reason, an ad hoc consent protocol should be prepared for these purposes. Our program is, as far as we know, the first one developed in Spain.
Virtual donation programOverviewThe donations come from patients who have undergone an imaging examination (normally CT scan or MRI) for healthcare purposes. This means that the petition to be included in the donation bank always occurs after the test, and that the test corresponds to a medical indication for exclusively healthcare reasons. No donations are accepted from healthy volunteers.
The program has been approved by the hospital's Ethics Committee as well as by the institution's board and senior management. Likewise, the legal issues of the program were evaluated and approved by the legal consultancy. The Information Technologies and Communications Department evaluated and approved the issues related to integrating the program in the institution's computer system and the issues related to data protection, within the hospital framework on this matter.
DocumentationThe program includes 2 documents, described below.
Program information documentThis is a dossier containing information on the DICOM files, the ethical bases of the donation and its practical aspects, such as the following: series donated, anonymisation, destination and storage. The ethical bases include the principles of anonymity, solidarity, altruism and absence of profit-making intention.
The document explains what the procedures (API techniques) and the storage system for the post-processing products (objects created by API techniques) are. The products are stored in the hospital PACS itself in the form of an object repository. The document also contains information about the use of the files donated.
Virtual donation formThis is a hospital-approved form, which the patient signs. It contains basic information about the program, along with patient data, the series donated and the main features protecting patient rights.
The fact that any use of the digital material digital will take place after anonymisation of the DICOM files is emphasised in the form. This anonymisation ensures that the individual to whom the study belongs cannot be identified, and that the DICOM file does not contain personal data of any kind. For the specified use, the material will be prepared in such a way that the person will not be recognisable through external features or any other element of individual identification.
The patient is informed that, in compliance with what is established in Organic Law 15/1999, of 13 December, on Protection of Data of a Personal Nature, the personal data obtained by completing the “document for virtual body donation” will be recorded in a computerised data file, for purposes solely related to the donation. The file will be registered in the Data Protection Agency, in which the security measures required by the regulations in force have been established. The data will not be treated for any purposes other than the one set for the donation; furthermore, the data will not be transferred to third parties that have no relationship with the donation purpose and, specifically, with the circumstances defined.
It is also stated in the form that the donor or his/her legal representatives can revoke the donation at any time. In addition, any file that does not correspond to the original DICOM from the imaging test.
Method for obtaining donationsNormally, the physician responsible for the patient explains the program to the patient and gives her/him the information document. This physical also signs the authorisation, together with the patient.
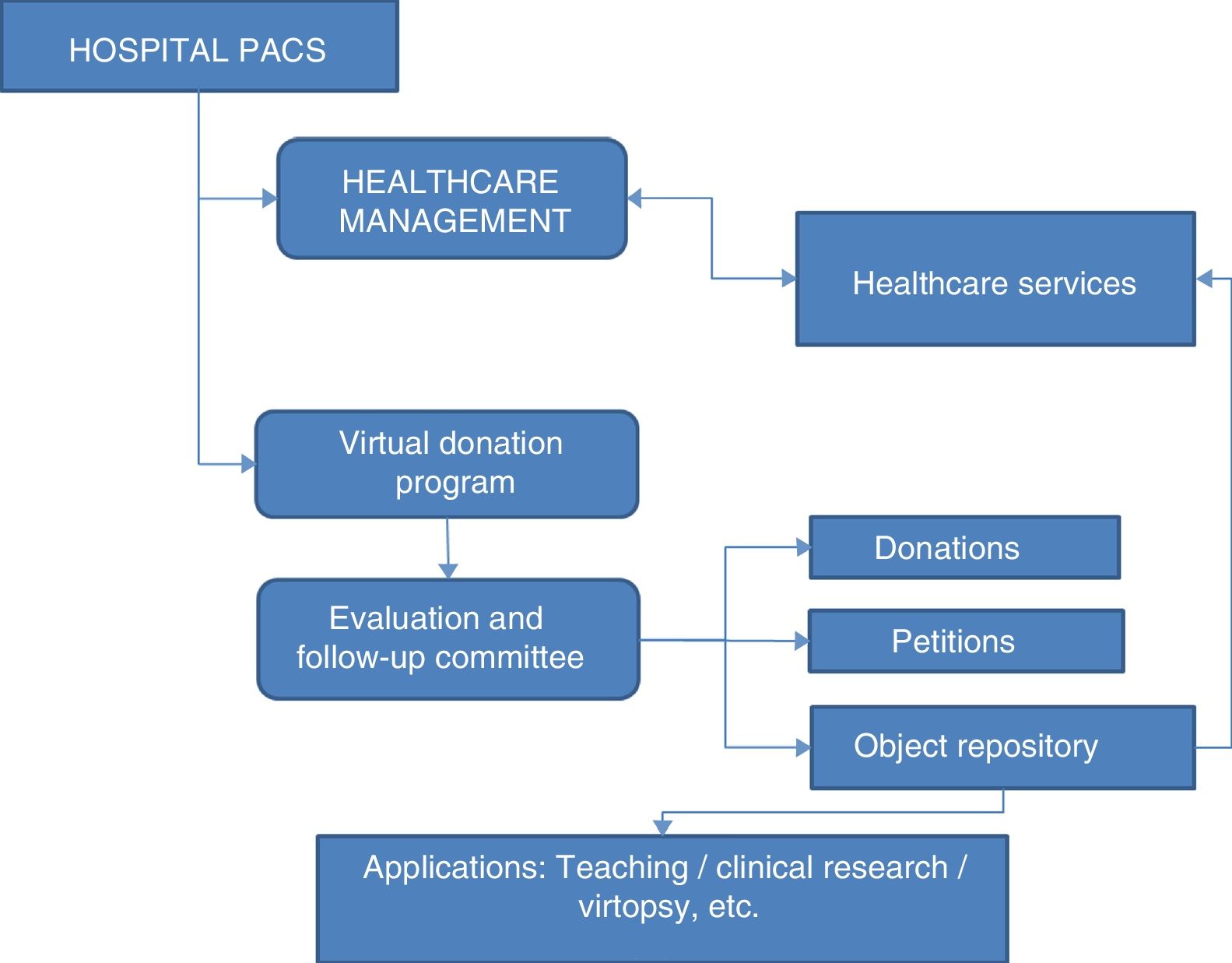
Donation bank structureThe donation bank forms part of the hospital PACS, in which the DICOM database is organised. The VBD are maintained by a database inside the server that manages the donations, the petitions for file use and the API technique products (object repository). The DICOM data remain anonymised and the objects are identified by a code that makes it possible to trace them retroactively to the hospital PACS.
Object repositoryThis is one of the most interesting parts of program and the one that is probably the most useful.
The API techniques normally produce new elements from the DICOM:
- 1.
Flat images (two-dimensional).
- 2.
Triplanar reconstructions.
- 3.
Three-dimensional reconstructions in volume format.
- 4.
Three-dimensional reconstructions in isosurface format (grid or “mesh”).
In turn, these can generate other objects by post-processing (for example, virtual anatomical preparations). All of these elements are of interest. For example, in flat images, information to be explored interactively can be embedded. Triplanar reconstructions permit internal landmarks to be positioned, without distorting the model.
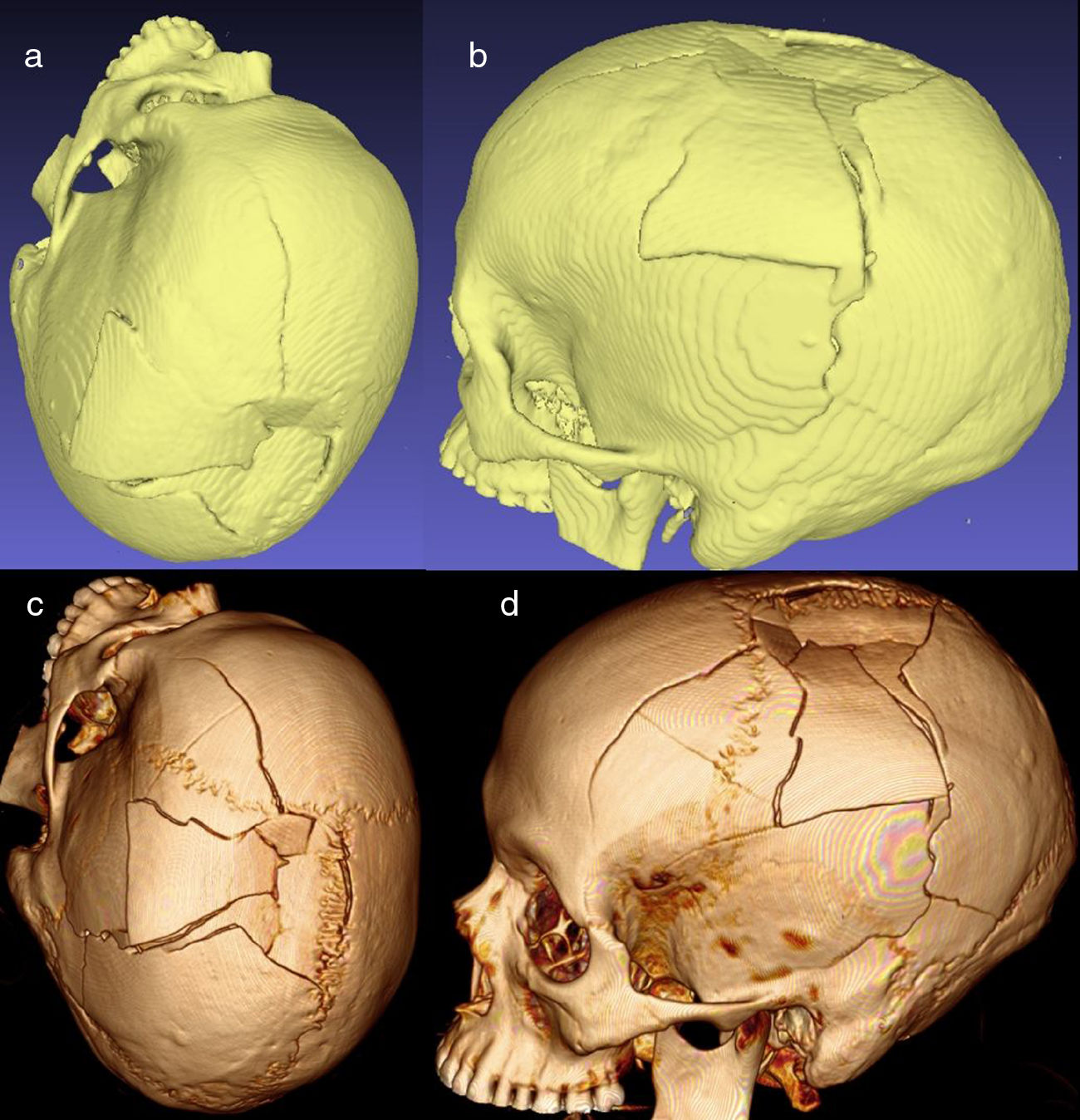
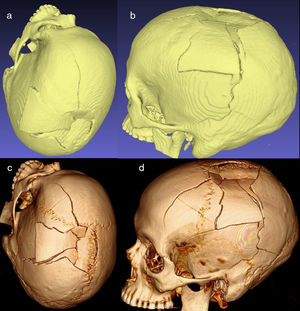
Volumes and isosurfaces are other objects of interest. Volumes consist of point-clouds (voxels) in a 3D space, each with colour, density, grey level and so forth. The volumes provide great detail, but they cannot be printed in 3D. Isosurfaces are generated from point-clouds (each with 3 spatial coordinates) that can be integrated into a surface (isosurface) composed of triangles, forming a grid (“mesh”). The result is an object viewable as a solid model that can be printed in 3D or edited using software for 3D objects (Fig. 2).
Having each of these elements available in the repository for use by teachers, clinical researchers or other professionals is one of the main strengths of the virtual donation program.
Managing the program and the object repositoryProgram and repository management is assigned to the Assessment and Follow-Up Committee. The committee consists of members of the hospital structure, including individuals from senior management, the legal department and healthcare areas. Its functions include the following: ensuring the storage and safekeeping of the petition and donation forms; granting or rejecting authorisations for use of the donation bank and of the DICOM files transferred; establishing the actions that the authorised party can perform on the material donated; and determining the file location and the way that analysis techniques and image processing happen in the files.
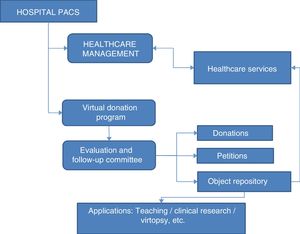
The committee will also handle object repository management. Petitions can be made for healthcare, education, research or other purposes (Fig. 3).
Image corresponding to the reconstruction in isosurface and to volume of a fractured skull. (a and b) Isosurfaces. These are multiple triangles reconstructed from points located on the vertices. (c and d) Reconstruction of volume. Here, each individual point has colour, grey-scale and other properties, which permits very detailed, realistic reconstructions, although printing the model is unfeasible. In contrast, 3D printing is possible with isosurfaces.
Using API techniques, we can perform anatomical operations such as segmentation, dissection, morphometric analysis and so on. There is a distinct advantage in being able to keep the specimen unchanged even though we get several preparations from it.
Anatomy teaching is subject to changes and contributions stemming from new technologies. These strategies have recently been reviewed.15 We believe that our program offers resources for these educational procedures through virtual dissection classrooms, virtual museums and new visualisation environments (augmented and virtual realities, 3D printing, holograms and the like). In turn, VBD can notably increase the number and type of virtual teaching-focused resources, specimens and anatomical preparations.
In addition, fields of research open because the donations include mathematical information on the specimen. This can be used for measurements and to position landmarks, calculate surfaces, volumes or indexes, carry out densitometries and perform other operations. Some research techniques, such as geometric morphometrics, find that the DICOM files constitute an ideal medium for many applications that directly affect clinical practice.16
EngineeringExamples of engineering use include the creation of finite models to test the effects accidents have on real models of normal individuals or those with a type of illness or specific corporal characteristics (for example, age, weight, body mass index or bone mineralisation).
Forensic scienceIn forensic anthropology, the program makes it possible to obtain population references for a geographical area (that of the PACS). This updated references, which come from similar populations, allow morphometric analysis and statistical reconstruction of the parts that are missing. In addition, there are many applications in virtual anthropology.
An interesting contribution is the training opportunity that is offered by using API techniques on real models for application in virtopsy. These techniques are complex and require knowledge of DICOM architecture and its use in reconstructions. This might make it easier for the forensic experts to use virtopsy techniques with any file to which they have access.
Clinical applicationsThese techniques make virtual practice possible; for example, to rehearse fracture reduction or simulate using new devices (such as implants or catheterisations) in cases with real medical conditions. It is a powerful tool for training physicians.
We would also like to emphasise that these systems are cross-disciplinary. They are not limited just to applications for Medicine. They can be used in Nursing, Physiotherapy, Occupational Therapy and other healthcare specialties.
Considerations on the current situation and future perspectivesOne of the issues is related to the validity of research studies being carried out in Spain with this type of material and procedures. It is possible that many of them are not based on the premises that have been mentioned throughout the article (donation program with ad hoc information and written consent). Consequently, these studies might suffer a certain weakness in validity, which emphasises one of the strengths of the virtual donation program that we present.
On the other hand, some tasks can be performed with the technology available today, but in the future it will be possible to extend them to fields unimaginable now: holography, studying illnesses by analysing voxels, CT scans or MRIs, brain tractography and other areas. This will require organising the existing virtual resources, so implementing and expanding this program could be of great interest for a not-too-distant future. This future perspective constitutes one of the strengths of programs such as the one that we present.
ConclusionsWe present a complete, hospital-based, VBD program. It is a pioneering program that offers teaching, research, healthcare and medico-legal resources, using new technologies on virtual body material donated by patients. The basis for the donation is the patient's consent after receiving specific information about the DICOM files and the nature and destination of the donated material.
Patient acceptance and healthcare staff response have been excellent. It can be applied in pre- and post-degree teaching in anatomy and morphological sciences in general, as well as in forensic science. The object repository is useful in training with invasive techniques, and in virtual dissection and virtopsy. The program adds to the anatomical material available (specimens and post-processing results) for multiple purposes.
The fact that there is mathematical information in the DICOM files allows all type of measuring, as well as analysis tasks (densitometry, geometric morphometrics and so on) and opens new fields to applied research in morphological and forensic sciences.
This is a pioneering initiative of great social interest, given that it is based on ethical principles sustaining and encouraging donations. It is possible that it will boost advancement in many forensic and biomedical sciences.
Conflict of interestsThe authors have no conflicts of interest to declare.
Please cite this article as: Aso-Escario J, Gil-Begué M, Sebastián-Sebastián C, Aso-Vizán A, Martínez-Quiñones JV, Consolini F, et al. Primer programa español de donación corporal virtual. Aspectos médico-legales e interés en docencia, asistencia e investigación. Rev Esp Med Legal. 2019. https://doi.org/10.1016/j.reml.2018.08.001