Cardiac diseases often underlie sudden deaths. Sudden death has a great social and economic impact and generates loads of media attention. When it occurs in young people, it is usually due to genetic causes (inherited heart diseases). This group includes cardiomyopathies, channelopathies, and familial thoracic aortic aneurysm/dissection. Inherited heart conditions are rare diseases in terms of prevalence and little knowledge is still available from most of them, so their management requires specialised and multidisciplinary training. Sudden death usually occurs in the out-of-hospital setting, and there has to be a forensic autopsy. These autopsies should be performed according to the minimum quality standards of the European guidelines. The clear genetic background justifies the need for a family screening to enable early diagnosis and also to rule it out in other family members at risk using a multidisciplinary approach offering personalised medicine to the affected families. In addition to medical issues, this scheme enables the provision of early psychological support and genetic counselling to plan new gestations. In Spain there is a great legal void in the approach to sudden death and its prevention, with a lack of homogenisation among the different counties, both at the judicial and healthcare levels due to the variable recognition of acquired skills and to the differences in the judicial and territorial forensic organisation throughout the country. It would be desirable that the consultative panels of both Ministries (Health and Justice) developed a comprehensive plan to ensure the quality in post-mortem studies and a proper subsequent clinical and genetic family study in public health services. Thus, the clinical-preventive potential of the autopsies would take shape and become a clear benefit for the affected families and for the society in general. This measure would also favour the teaching and the research of inherited cardiac diseases, which is of paramount importance to improve the current knowledge in this field, so unknown and so devastating.
La muerte súbita es fundamentalmente cardiaca y tiene un gran impacto social, económico y mediático. Cuando acontece en personas jóvenes, suele obedecer a causas genéticas (cardiopatías familiares). En este grupo se incluyen las miocardiopatías, canalopatías y el aneurisma/disección aórtica familiar. Las cardiopatías familiares son enfermedades raras en términos de prevalencia y poco conocidas, por lo que su manejo requiere formación especializada y multidisciplinar. La muerte súbita suele acontecer en el ámbito extrahospitalario y es objeto de una autopsia forense. Estas autopsias deberían realizarse de acuerdo a los estándares mínimos de calidad de las guías europeas. El claro sustrato genético justifica la necesidad de un screening familiar para realizar diagnósticos precoces y también para descartarla en otros familiares en riesgo a través de un abordaje multidisciplinar que ofrezca una medicina personalizada a las familias afectadas. Además de las cuestiones médicas, este esquema permite ofrecer apoyo psicológico precoz y consejo genético de cara a planificar nuevas gestaciones. En España existe un gran vacío legal en el abordaje de la muerte súbita y su prevención, con una falta de homogenización entre las distintas comunidades autónomas tanto a nivel judicial como asistencial debido a las características del proceso de transferencia de competencias y a la organización territorial judicial y forense. Sería deseable que, desde los órganos consultivos de ambos ministerios (Sanidad y Justicia) se elaborara un plan de actuación global que asegurara la calidad en el estudio post mortem y su continuidad en el posterior estudio familiar clínico y genético. Así, el potencial clínico-preventivo de las autopsias tomaría cuerpo y revertiría en un claro beneficio para las familias afectadas y para la sociedad en general favoreciendo asimismo la docencia y la investigación, tan importantes para el avance del conocimiento en este ámbito tan desconocido y devastador.
Sudden death (SD) is usually defined as an unexpected death which occurs within an hour from the onset of symptoms, although other time intervals have sometimes been used.1 It is an event which has a major social and financial impact and which generates a good deal of media attention. The primary cause of sudden death is heart-related, and in particular ischaemic heart disease,2 with a polygenic and multifactorial origin. Inherited cardiac conditions (ICCs) (channelopathies, cardiomyopathies and familial thoracic aortic aneurysm/dissection) tend to disproportionately affect children and young adults, where they represent the leading cause of sudden cardiac death (SCD).3 Unlike ischaemic heart disease, ICCs have a clear genetic substrate which justifies the indication for adequate testing of the first-degree relatives of the deceased, with a cascading expansion of the testing circle depending on the results.1 The most common type of inheritance is autosomal dominant, where 50% of offspring will be affected.1 This family testing, with clinical and genetic tests, should ideally be carried out by a multidisciplinary team (forensic experts, pathologists, geneticists, paediatricians, basic researchers and cardiologists) which has experience in the field of ICCs,1,2,4 given their status as rare diseases, their short course from when they were discovered and the difficulties in establishing definitive diagnoses.
The forensic autopsy, starting point for family testingAs it is an unexpected event, sudden death should give rise to the opening of a judicial procedure, as the legal system justifies forensic autopsies in these cases. Specifically, Article 343 of the Spanish Law on Criminal Procedure states that, in cases of violent death or suspected crime, an autopsy will be carried out. Furthermore, Recommendation No. (99) 3 of the Committee of Ministers of the Council of Europe, for the methodological harmonisation of medico-legal autopsy rules,5 specifies that an autopsy should be carried out in the event of a sudden unexpected death.
The medico-legal autopsy fulfils its legal objective of ruling out a violent death but often, despite the efforts of the professional in charge, it is not able to develop its research potential (examining the biological substrate causing the SD in more detail) or its clinical-preventive potential (by allowing the findings obtained in the autopsy to be turned into a direct benefit for family members by carrying out screening, or for society as a whole by expanding the knowledge available on ICCs).
Thus, in addition to identifying the cause of death (dilated, hypertrophic, arrhythmogenic cardiomyopathy, ascending thoracic aortic dissection, structurally normal heart, etc.), the forensic autopsy should:
- •
Provide important morphological data for the phenotype-genotype correlation and to potentially influence the risk stratification of the affected family members.
- •
Store (ideally sine die) biological samples of an incalculable value (minimum required: two tubes of blood in EDTA properly frozen).
- •
Direct the families towards multidisciplinary working groups.
The autopsy will not tell us which gene was involved in the SD of a given patient, but sometimes the integration of all the clinical information gathered from the deceased and from his/her family members can guide genetic testing in an extremely useful way.
The solution: personalised medicine and coordination between public bodies (health and justice)ICCs have a high degree of heritability as most have an autosomal dominant inheritance pattern.1 In this regard, all articles published about SCD with a suspected or definitive diagnosis of ICC highlight the need to implement familial screening to look for asymptomatic carriers.1,4,6 Ultimately, it is a matter of implementing a multidisciplinary approach that makes it possible to offer personalised medicine to families affected by the SD of a potential family member to resolve medical and psychological questions regarding the diagnosis and the treatment. Genetic counselling is also frequently offered in order to plan new pregnancies. The right approach to this group of diseases is captured perfectly by this sentence from Dr W. J. McKenna: “If you are treating a patient with an ICC; you are not treating a patient, you are treating a family”.
In Europe, in particular in the United Kingdom, the Ministry of Health was a pioneer (2005) in publishing an initiative for the testing of families with ICCs and SD in its National Plan for the Prevention of SD (National Service Framework. Chapter 8: Arrhythmias and Sudden Cardiac Death).7 For the first time, the need to refer the family members of SCD victims to centres where they may receive comprehensive care was recognised. The responsibility of the health system as a guarantor that such measures are effective, and that there are therefore guidelines as to what is considered good clinical practice, was also recognised. The plan identifies the key points in which the pathologist and the medical examiner play a fundamental role, as, sadly, this is the starting point for many families. When a case of SCD or a potential case of SCD is identified, the family needs support and also a correct clinical assessment. The autopsy findings, the tissue samples and the availability of biological material from the deceased for possible genetic testing will be crucial factors for the subsequent assessment of the rest of the family.
In Spain, this need for familial prevention has been declared since the 1990s, after the finding of a cardiomyopathy in the autopsy of an SD victim. The forensic pathologists, Beatriz Aguilera and María Paz Suárez, working alongside the major European groups on cardiovascular disease,8 have repeatedly presented this premise in their presentations and papers.9 However, Spain still lacks a national regulation like the British one, which regulates the processing of cases of SCD and the commitment of the Government to inform and refer affected families to centres where they can be appropriately attended to. The most common situation in Spain was that a variable percentage of families collected the definitive autopsy report. This report established the cause of death as “natural”, but it may or may not have stated that the cause of death was probably genetic, and that the family members should therefore go to their doctor. The actions of the primary care doctors of each family member were not coordinated when they were deciding if an electrocardiogram was sufficient or if they should be referred to Cardiology (each family member to their own referral centre, thereby decentralising the information about the family as a whole).
Fortunately, the multidisciplinary approach from the sudden death until the assessment of the family members at risk has become more widespread throughout the other autonomous communities. This is thanks to the tireless efforts of the Sociedad Española de Cardiología [Spanish Society of Cardiology] and the Sociedad Española de Patología Forense [Spanish Society of Forensic Pathology] Working Group on Inherited Cardiac Conditions, with a greater awareness of the group of medical examiners and cardiologists, although with a different degree of institutional involvement.
There are significant barriers to implementing these protocols, given that each judicial file of a forensic autopsy is subject to pre-trial secrecy. The efforts of forensic experts and pathologists, on the one hand, and cardiologists and paediatricians, on the other, run in parallel and independently in the face of the legal impossibility of sharing data and impressions on concrete cases, to guide families affected by an SD at risk of having an inherited heart disease which may affect other family members. In light of the current evidence in the literature, it is essential to implement a change in the legal framework (either at national or regional level) which makes it possible to promote teamwork from the health and justice ministries in this context for health, social, economic and scientific benefits.
Action guidelinesTaking the accumulated knowledge as a reference framework, the European Society of Cardiology Working Group published a consensus statement as a guide for the testing of family members of patients with cardiomyopathies who are at risk of having inherited them.10 Given the similarities which have already been discussed, the Spanish Society of Cardiology Working Group on Inherited Cardiac Conditions recently published study and follow-up recommendations across the entire spectrum of ICCs, also including channelopathies and inherited aortic diseases.4 Also in recent years, making the most of major advances in the field of cardiogenetics, clinical practice guidelines for the conduct of genetic testing in the context of these diseases have been published. In general, the indication for conducting genetic testing in living patients with these diseases is class I or IIa and a minority (restrictive cardiomyopathy or short QT syndrome) have a class IIb indication (which will undoubtedly improve when our knowledge of these diseases, and thus the efficiency of genetic testing, is increased).9
In the field of SCD autopsies, the detailed study of the heart, the conduct of relevant toxicology studies and the storage (sine die) of biological material on which genetic testing can be conducted at a later date have an indication of type I class C.1,2 In the latest update of the guidelines for the management of hypertrophic cardiomyopathy, a class IIA recommendation was established for the conduct of genetic testing on deceased individuals with HCM who died from SD.11 It is noteworthy that the same document has downgraded the degree of indication regarding the same type of testing on living patients with HCM, when the maximum benefit of these tests is the screening of family members, which is a reality in both fields. In cases of SD with a structurally normal heart (sudden arrhythmic death syndrome [SADS] and sudden infant death syndrome [SIDS]), the American Heart Rhythm Society (HRS), the European Heart Rhythm Association (EHRA)12 and the Canadian Cardiovascular Society/Canadian Heart Rhythm Society13 maintain a class IIa level of evidence C degree of recommendation for the conduct of a genetic test focusing on genes causing channelopathies. In an attempt to unify all available evidence, the latest review of the guidelines for the prevention of sudden death established a type IIa class C indication for post-mortem genetic testing focusing on genes of interest in all cases of sudden cardiac death due to cardiomyopathies or channelopathies.1
If these genetic tests identify the mutation responsible, the family members who are non-carriers can be discharged, will not require further check-ups, will not pass it on to their offspring and will be freed of the anxiety associated with uncertainty.4
The action protocol for the management of ICCs, issued by the above-mentioned Spanish Society of Cardiology Working Group on Inherited Cardiac Conditions, includes a specific reference to post-mortem testing.4
Recommendation VII: blood and/or tissue samples from individuals who have died from sudden death with suspected or confirmed ICC should be collected and stored to allow for genetic testing (“molecular autopsy”). It would be desirable that each autonomous community in Spain is provided with the resources for the creation of reference centres for the macroscopic and microscopic study of the hearts and aortas of young patients with suspected ICC who died suddenly. These units should work in a coordinated manner with the ICC units. It is recommended that stable collaboration links are in turn established between the justice (on which forensic experts and forensic pathologists depend) and health systems (on which ICC units depend).
The forensic autopsy is a key element as this will be what guides familial testing in most cases. It should be performed following the recommendations established by the scientific community in the form of guidelines. In our field, the Association for European Cardiovascular Pathology issued a guideline in 2007,2 translated into Spanish,14 and pending its next update at the time of writing this article. The guideline details the minimum standards of recommended compliance, both in the autopsy and in the histopathological study of the cardiac specimen. It is therefore necessary that they are carried out by experts with training and experience in the study of SCD,1,2 and that they are in close contact with the clinicians in the referral units (cardiologists or paediatricians, depending on the age of the deceased).
Adherence to this guideline by all Institutes of Legal Medicine and Forensic Science would ensure these quality standards in the post-mortem testing of SD in Spain, and would allow for the homogenisation of data. This is the only way in which a national registry could be created which would make it possible to compare disease patterns in different autonomous communities or different European countries.
In order to implement this much-needed project, it is fundamental that, at the legislative and administrative level, the institutions involved are aware of the important role played by the Institutes of Legal Medicine and Forensic Science (Institutos de Medicina Legal y Ciencias Forenses, IMLCF) in the study and prevention of SD on the one hand, and that they provide the resources, organisation and appropriate training to suitably equip Forensic Pathology to undertake this ambitious task.
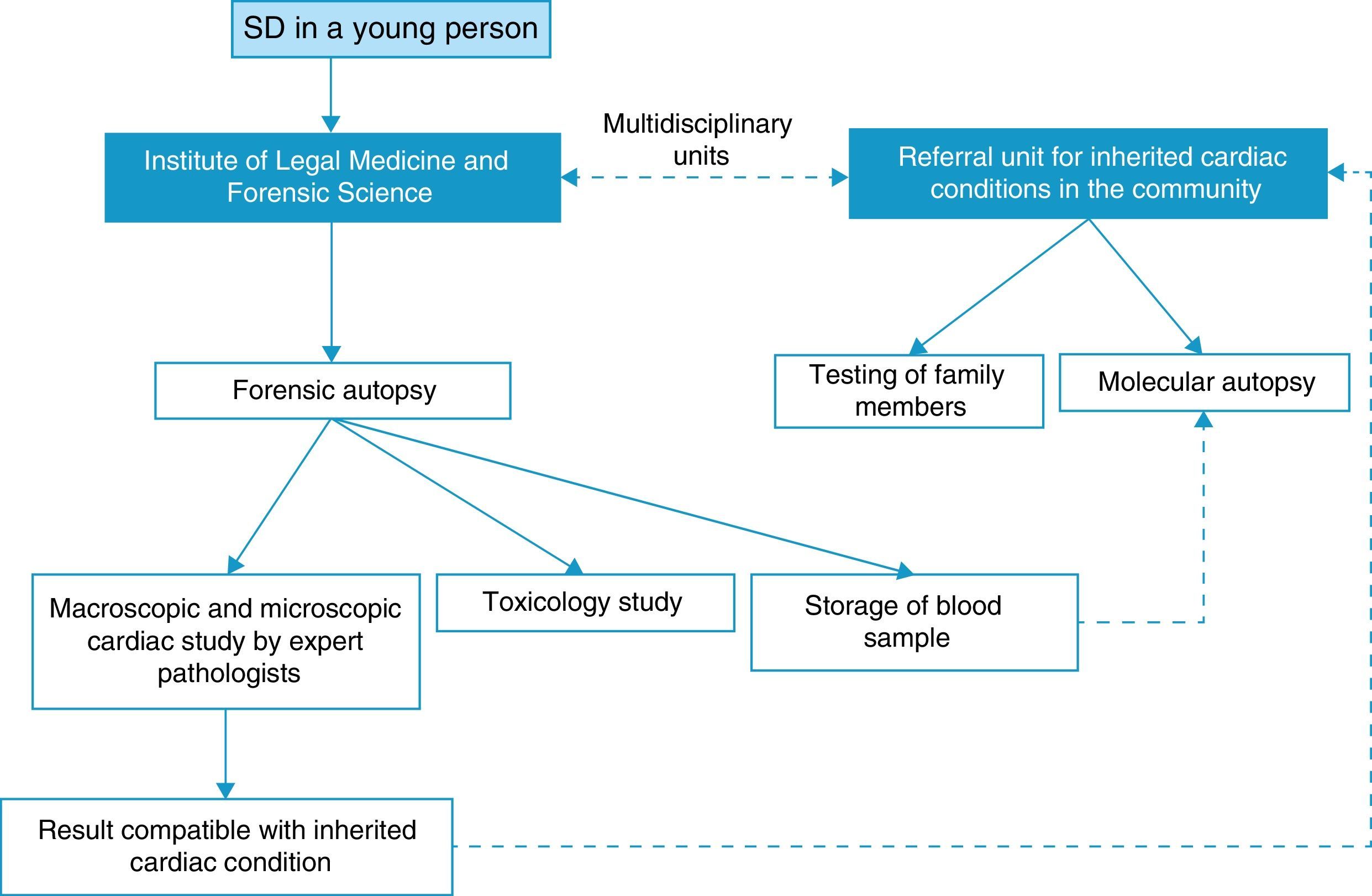
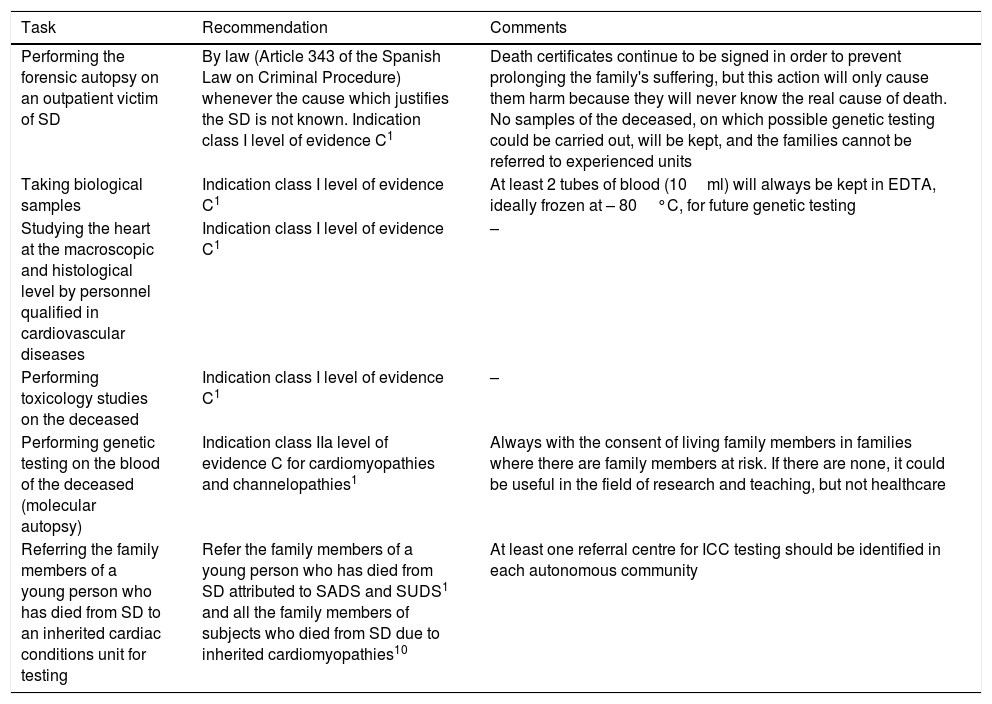
We propose following a similar work flow in all the autonomous communities, with the following recommendations (Table 1 and Fig. 1).
Recommendations of interest following a sudden death.
| Task | Recommendation | Comments |
|---|---|---|
| Performing the forensic autopsy on an outpatient victim of SD | By law (Article 343 of the Spanish Law on Criminal Procedure) whenever the cause which justifies the SD is not known. Indication class I level of evidence C1 | Death certificates continue to be signed in order to prevent prolonging the family's suffering, but this action will only cause them harm because they will never know the real cause of death. No samples of the deceased, on which possible genetic testing could be carried out, will be kept, and the families cannot be referred to experienced units |
| Taking biological samples | Indication class I level of evidence C1 | At least 2 tubes of blood (10ml) will always be kept in EDTA, ideally frozen at – 80°C, for future genetic testing |
| Studying the heart at the macroscopic and histological level by personnel qualified in cardiovascular diseases | Indication class I level of evidence C1 | – |
| Performing toxicology studies on the deceased | Indication class I level of evidence C1 | – |
| Performing genetic testing on the blood of the deceased (molecular autopsy) | Indication class IIa level of evidence C for cardiomyopathies and channelopathies1 | Always with the consent of living family members in families where there are family members at risk. If there are none, it could be useful in the field of research and teaching, but not healthcare |
| Referring the family members of a young person who has died from SD to an inherited cardiac conditions unit for testing | Refer the family members of a young person who has died from SD attributed to SADS and SUDS1 and all the family members of subjects who died from SD due to inherited cardiomyopathies10 | At least one referral centre for ICC testing should be identified in each autonomous community |
EDTA: ethylenediaminetetraacetic acid; ICC: inherited cardiac condition; SD: sudden death; SADS: sudden arrhythmic death syndrome; SUDS: sudden unexplained death syndrome.
The vague term “SD in a young person” has been used in Fig. 1 and Table 1 presented below. The cut-off point of 40 years has been established in the literature.15 Above this age, the prevalence of ICCs as a cause of SD drops significantly. Depending on the actual possibilities of each workplace, this age could be modified as, for example, the family members of a victim of SCD due to HCM are also indicated for familial assessment, regardless of the age of the deceased.
Ethical issuesWhen a healthcare professional/investigator (medical examiner, pathologist, cardiologist, paediatrician, biologist, etc.) identifies a condition which could have been caused by a genetic problem, he/she automatically acquires the ethical commitment/obligation to inform not only this person, but also the family members at risk.16 In the case of an autopsy for SD with a structurally normal heart, it has not yet been categorically established which strategy is the most cost-effective; i.e. whether it be better to delay the evaluation of the family members until the results of the molecular autopsy are received, or to contemplate the initial clinical evaluation of family members prior to conducting genetic testing in the deceased, which can sometimes provide guidance.16–20
In order to avoid ethical issues, the family members should be made aware of the presence of an ICC in both options, and the informed consent should be collected before conducting genetic testing in the deceased, as they are entitled to assert their right to not know the result of these tests. It should also be remembered that, even in the event of not identifying a pathogenic, or probably pathogenic, mutation in the molecular autopsy, the family members, who are still at risk of having inherited the same disease, even without an identified genetic substrate, should be clinically assessed.
Experience of the risk assessment unit of sudden death of a family memberIn the autonomous community of Valencia, the Risk Assessment Unit of Sudden Death of a Family Member (Unidad de Valoración del Riesgo de Muerte Súbita Familiar, UVRMSF) is a pioneer in Spain in the systematic multidisciplinary approach of families affected by SCD due to an ICC. In fact, it is the first unit in Spain with an explicit agreement between the Regional Ministries of Health and Justice (Official Journal of the Autonomous Community of Valencia [DOCV] 2008/8199). Other autonomous communities, historically with a long track record in the study of patients with ICCs and, also, more recently in autopsies for SD, have followed this same path of collaboration between the Health and Justice ministries for the overall benefit of society. So far, only the autonomous community of Murcia has obtained an official legal framework (Spanish Official State Gazette [BOE] 4/3/2013), while in the rest of the autonomous communities specific agreements are in place between particular institutions, which have not yet been published in the Official State Gazette or the Gazette of the Autonomous Community, rendering the systematics of this strategy unofficial (Catalonia, Andalusia, Galicia, Madrid and the Basque Country).
The UVRMSF was created with the support of Hospital La Fe, as well as the Regional Ministries of Health and Justice, with the scientific backing of the Colegio de Médicos de Valencia (College of Physicians of Valencia) and the Sociedad Valenciana de Cardiología (Valencian Society of Cardiology) and the financial research grant received from the Instituto de Investigación Sanitaria Carlos III (Carlos III Health Research Institute). Although it emerged with a sphere of competence for the entire Autonomous Community of Valencia, it was subsequently redefined to serve the provinces of Castellón and Valencia, with Alicante taking an independent path. Its organisational chart includes a forensic subunit and a hospital subunit.
A protocol began to be implemented in 2008, fuelled to a great extent by previous experience in the literature.12,13 In addition to family members of cases of SD, this protocol also includes families in which the proband had presented with a cardiac arrest and those families with SD in which an autopsy had not been performed but the clinical data suggested the presence of an inherited cardiac condition. The cardiology tests which are offered to first-degree relatives are determined by the classification of the proband, and their results are complemented with the results of the genetic tests.
From the creation of the UVRMSF up to 2016, the IMLCF in Valencia performed 455 standardised autopsies on cases of SD in individuals younger than 55 years of age, with the following diagnoses in ages between 1 and 55 years (405 cases): ischaemic heart disease (58%), sudden arrhythmic death syndrome (SADS) (23%), cardiomyopathies (11%: 5% hypertrophic, 3% arrhythmogenic and 3% dilated), aortic dissection (3%), myocarditis (1%), heart valve diseases (2%), coronary artery dissection (1%), congenital heart diseases (0.5%), anomalous origin of coronary artery (1%). In individuals less than one year old (50 cases): sudden infant death syndrome (54%), sudden explained death (38%) and sudden unexplained death (8%).
Hospital Universitario La Fe's Cardiology Department has tested 500 families (more than 2000 family members). Most families have been referred following an SD of potential genetic cause. Others have been referred following the diagnosis of an ICC in a living family member. In general, from the family testing derived from our protocol, an ICC has been diagnosed and preventive and/or therapeutic measures have been applied in around 50% of the subjects assessed in 2016 (from clinical follow-up in outpatient clinics, modifying lifestyle and sporting habits, lists of drugs to avoid, starting specific treatment, frequently with beta-blockers and, in selected cases, implanting defibrillators).
Clinical decisions about the frequency of examinations and end of follow-up are based on consensus statements.4,10,12 Genetic tests have been carried out, as far as possible, on samples of DNA extracted from blood obtained during the autopsy of the deceased (surplus DNA is kept and stored at −80°C to guarantee its integrity for future testing). If DNA from the deceased was not available, a family member with the same phenotype was selected. If a family member with the same phenotype cannot be found, genetic testing should not be performed in these families (i.e. genetic testing should not be indicated in asymptomatic family members without an ICC phenotype, even if one of his/her family members has died from SD). If mutation(s) are identified, the family members will be offered the opportunity to complete the clinical testing, in order to verify whether or not they have these mutations. The funding required to carry out this ambitious project has been received from mixed sources, through the healthcare and research routes. With this type of teamwork, and always under a multidisciplinary perspective, it is possible to generate more realistic statistics on SD in general and SCD in particular, to carry out research in this context by managing to bring together a sufficient sample size and, most importantly, to give the benefit of this research back to society by diagnosing and treating not only subjects affected by the same disease, but also genetic carriers at risk of developing it.
Key to the viability of a multidisciplinary approachThe direct communication flow between the forensic subunit and the hospital subunit has been key in the consolidation of the UVRMSF. Records are discussed, images are reviewed and specific studies are planned. The results obtained at the IMLCF are reported to Cardiology and vice versa. The IMLCF also serves as a link with prosecutors, judges or IMLCFs in other autonomous communities to process the bureaucracy regarding the request for samples (blood, paraffin-embedded myocardium) from deceased individuals from outside the community with family members at risk in the Valencia community health area. In addition, from a research and educational point of view, both subunits participate jointly in research projects, awareness talks, seminars in the Faculty, presentations, papers and posters at national and international conferences. Ultimately, we feel part of the project and we see the impact of our contributions benefiting families and society in general.
After almost 10 years of teamwork, all the members of the UVRMSF are committed to the project and we believe that this multidisciplinary approach could be transferred to other Spanish regions to prevent inequalities in the treatment of these families depending on the autonomous community where the SD occurs.
ConclusionsThis article underlines the great legal vacuum which exists in Spain in the approach to SD and its prevention. There is a lack of homogenisation among the different autonomous communities, both at a judicial and healthcare level. It would therefore be desirable for the advisory bodies of both ministries to draft a comprehensive action plan which would promote and ensure the quality of post-mortem testing and the subsequent familial clinical and genetic testing.
FundingThis study was funded by grants from the Instituto de Salud Carlos III–European Union, European Regional Development Fund “A way to make Europe” (RD12/0042/0029, PI14/014077 and PT13/0010/0026).
Conflicts of interestThe authors declare that they have no conflicts of interest.
We are grateful for the funding obtained from the Instituto de Salud Carlos III–European Union, European Regional Development Fund “A way to make Europe”, (RD12/0042/0029, PI14/014077 and PT13/0010/0026), the support of the Asociación Valenciana de Cardiopatías Familiares y Muerte Súbita (Valencian Association of Inherited Cardiac Conditions and Sudden Death) of the Autonomous Community of Valencia, and all those who participated at the UVRMSF for their committed effort.
Please cite this article as: Molina Aguilar P, Giner Blasco J, Izquierdo Macian I, Martínez-Dolz L, Barriales Villa R, Zorio Grima E. Unidades multidisciplinares en el estudio y prevención de la muerte súbita por cardiopatías familiares. Rev Esp Med Legal. 2018;44:46–52.