To investigate the association between positive lesions detected by 99mTc-PSMA SPECT/CT and blood levels of prostate-specific antigen (PSA) and alkaline phosphatase (ALP) in patients with prostate cancer (PCa) and bone metastasis undergoing endocrine therapy.
MethodsA retrospective analysis was performed on 43 patients diagnosed with PCa bone metastasis who underwent endocrine therapy. PSA, ALP, whole body bone imaging and 99mTc-PSMA SPECT/CT imaging were collected from all patients (Among them, 17 cases were re-examined 99mTc-PSMA SPECT/CT imaging). According to the results of the first 99mTc-PSMA SPECT/CT imaging for detecting bone metastasis, all cases were divided into two groups: positive group and negative group. The relationship between 99mTc-PSMA imaging and PSA and ALP was analyzed by ROC curve. Fisher exact probability method was used to examine the changes in imaging radioactivity uptake, PSA, and ALP levels in 17 patients after treatment, and P < 0.05 was statistically significant.
ResultsAll 43 patients had different degrees of radioactive concentrations on whole-body bone imaging. The first 99mTc-PSMA SPECT/CT imaging showed positive bone metastases in 31 cases and negative bone metastases in 12 cases. ROC curve analysis of PSA and ALP, AUC were 0.778 and 0.770, respectively. When PSA > 1.13 ng/mL, 99mTc-PSMA SPECT/CT imaging diagnostic sensitivity was 93.55%, and specificity was 66.67%. When ALP was >86U/L, the diagnostic sensitivity of 99mTc-PSMA SPECT/CT imaging was 64.52%, and the specificity was 83.33%. In 17 cases, the PSA level decreased in 7 and increased in 10. There were 10 cases of increased ALP and 7 cases of decreased ALP levels. In the second 99mTc-PSMA imaging lesion, there were 9 cases with decreased or no uptake, and 8 cases with increased uptake or number of lesions. The changes in 99mTc-PSMA uptake by Fisher’s exact probability method were statistically significant (P < 0.05, P = 0.006, and P = 0.006, respectively), and ALP level was not statistically significant (P = 0.563).
Conclusion99mTc-PSMA SPECT/CT imaging can detect PCa bone metastases, which are related to PSA levels. When PSA > 1.13 ng/mL, the sensitivity of diagnosis and detection of positive bone metastases is higher, and when ALP is >86U/L, 99mTc-PSMA imaging has higher specificity.
Investigar la asociación entre las lesiones positivas detectadas por 99mTc-PSMA SPECT/CT y los niveles sanguíneos de antígeno prostático específico (PSA) y fosfatasa alcalina (ALP) en pacientes con cáncer de próstata (CaP) y metástasis óseas sometidos a terapia endocrina.
MétodosSe realizó un análisis retrospectivo de 43 pacientes diagnosticados de metástasis ósea de CaP que fueron sometidos a terapia endocrina. Se obtuvieron imágenes de PSA, ALP, imágenes óseas de todo el cuerpo e imágenes de SPECT/CT con 99mTc-PSMA de todos los pacientes (entre ellos, 17 casos fueron reexaminados con imágenes de SPECT/CT con 99mTc-PSMA). Según los resultados de la primera imagen SPECT/TC con 99mTc-PSMA para detectar metástasis óseas, todos los casos se dividieron en dos grupos: grupo positivo y grupo negativo. La relación entre las imágenes de 99mTC-PSMA y el PSA y la FA se analizó mediante la curva ROC. Se utilizó el método de probabilidad exacta de Fisher para examinar los cambios en la captación de radiactividad por imágenes, los niveles de PSA y ALP en 17 pacientes después del tratamiento, y P < 0,05 fue estadísticamente significativo.
ResultadosLos 43 pacientes tenían diferentes grados de concentraciones radiactivas en las imágenes óseas de todo el cuerpo. Las primeras imágenes SPECT/TC con 99mTc-PSMA mostraron metástasis óseas positivas en 31 casos y metástasis óseas negativas en 12 casos. En el análisis de la curva ROC de PSA y ALP, el AUC fue 0,778 y 0,770, respectivamente. Cuando el PSA > 1,13 ng/mL, la sensibilidad diagnóstica por imágenes SPECT/CT con 99mTc-PSMA fue del 93,55 % y la especificidad fue del 66,67 %. Cuando la FA era >86 U/L, la sensibilidad diagnóstica de la SPECT/CT con 99mTc-PSMA fue del 64,52 % y la especificidad fue del 83,33 %. En 17 casos, el nivel de PSA disminuyó en 7 y aumentó en 10. Hubo 10 casos de aumento de ALP y 7 casos de disminución de los niveles de ALP. En la segunda lesión por imágenes con 99mTc-PSMA, hubo 9 casos con captación disminuida o nula y 8 casos con captación aumentada o número de lesiones. Los cambios en la captación de 99mTc-PSMA mediante el método de probabilidad exacta de Fisher fueron estadísticamente significativos (P < 0,05, P = 0,006 y P = 0,006, respectivamente), y el nivel de ALP no fue estadísticamente significativo (P = 0,563).
ConclusiónLas imágenes SPECT/CT con 99mTc-PSMA pueden detectar metástasis óseas de CaP, que están relacionadas con los niveles de PSA. Cuando el PSA es >1,13 ng/mL, la sensibilidad del diagnóstico y la detección de metástasis óseas positivas es mayor, y cuando la FA es >86 U/L, las imágenes con 99mTc-PSMA tienen una mayor especificidad.
The incidence of prostate cancer (PCa) has increased in recent years. It is one of the most common malignancies in men and has a lifetime risk of approximately 12.5%. Owing to the hidden progression of the disease, most patients have metastases at the time of treatment. Bone is the most common site of PCa metastasis, and approximately 90% of patients who die from PCa often have bone metastases.1 The high incidence of bone metastases has led to the inclusion of bone imaging in most of the national and international treatment guidelines. Timely detection of PCa bone metastasis active lesions is conducive to accurate treatment and improves patient prognosis. Whole-body bone imaging is a sensitive method for diagnosing bone metastasis of PCa. However, it is affected by many factors, such as fractures, blood system diseases, and benign bone and joint lesions; therefore, it lacks diagnostic specificity.2 Bone imaging is based on chemisorption and ion exchange processes. Therefore, for patients treated for bone metastasis, whole-body bone imaging may also show a high uptake of radioactivity due to active bone metabolism during bone repair. Therefore, it is impossible to determine whether bone metastases exhibit tumor activity, and better imaging methods are needed to distinguish active bone metastases.
PSMA secreted by epithelial cells around the prostate duct is a type II transmembrane protein overexpressed by most PCa cells, especially on the surface of poorly differentiated, metastatic, and androgen independent PCa cells. Its expression level is 10–1000 times higher than that in normal tissues (kidney, intestine, etc.). After binding to ligands such as specific antibodies and small molecular antagonists, PSMA is phagocytosed by cells and PSMA will be retained in lysosomes or released into the cytoplasm. Based on this biological effect, PSMA is a specific target for the diagnosis and treatment of PCa.3 99mTc-PSMA imaging (a small molecular inhibitor analog of 6-hydrazino nicotinic acid (HYNIC), a bifunctional chelator introduced based on the glutamate-urea core, can be highly concentrated in tumor model imaging with high expression of PSMA and can be quickly cleared from the body).4 It can perform specific imaging of PCa and its metastatic foci and obtain whole-body plane and local tomographic images.5–7 Based on this biometric analysis, 99mTc-PSMASPECT/CT imaging is an effective method for the diagnosis of PCa and is useful for detecting metastatic bone lesions in these patients.8
Alkaline phosphatase (ALP) is an indicator of bone metabolism and can reflect osteogenic activity to a certain extent. Studies have shown that ALP has predictive value for bone metastasis.9 This study aimed to assess the association between two blood markers, prostate-specific antigen (PSA) and ALP, and 99mTc-PSMASPECT/CT imaging findings in patients with recurrent PCa bone metastasis.
MethodsStudy populationA retrospective analysis was performed on 43 patients with bone metastasis of PCa underwent endocrine therapy between December 2019 and November 2021 at Henan Provincial People's Hospital, China. Data from 99mTc-PSMA SPECT/CT imaging, pathology, whole-body bone imaging, and PSA and ALP levels were collected from all patients. Based on the results of bone metastasis on 99mTc-PSMA imaging, the patients were divided into positive and negative groups, and the relationship between the imaging results and PSA and ALP levels was determined. Seventeen patients underwent the aforementioned evaluation six months after their initial treatment, which included orchiectomy or luteinizing hormone-releasing hormone (LH-RH) agonists, with or without antiandrogen therapy. All examinations were conducted within a one-week timeframe. This study conformed to the Declaration of Helsinki regarding research involving human subjects and passed the review of the Medical Ethics Committee of Henan Provincial People's Hospital [(2019) No. 108]. All patients provided written informed consent before each examination.
Inclusion and exclusion criteriaThe following criteria10 were met for inclusion: (1) SPECT/CT whole-body bone imaging showed multiple (≥2) abnormal concentrations; (2) for a single lesion, SPECT/CT fusion images showed osteolytic or osteoclastic changes; (3) the patient had symptoms of bone pain site, SPECT/CT scans indicated lesions at the bone pain, after excluding all benign lesions and symptom relief after anti-tumor treatment; (4) no osteogenic drugs were used in all patients; and (5) patients over 18 years of age agreed to participate in this examination and signed an informed consent form.
The exclusion criteria were as follows: patients with prostate cancer were excluded from recent bone surgery, benign osteoarthropathy, and trauma history; the relevant examination could not be improved in time, unwillingness to sign the informed consent form, and inability to cooperate with patients to complete the examination.
MeasurementsSPECT/CT image acquisition and reconstruction: The patient did not require special preparation. 99mTc-PSMA15-25mCi was injected into the elbow vein, and adequate hydration metabolism was achieved with adequate drinking water. Planar whole-body (WB) images and SPECT/CT data acquisition were performed using a GE T16 SPECT/CT scanner (NM/CT 670 SPECT/CT, American GE Discovery instrument), 2 h after injection with a low-energy high-resolution collimator. Following planar image acquisition, SPECT/CT of the thoracic and abdominal regions was performed in each patient. WB planar scintigraphy (anterior and posterior) was performed using a low-energy high-resolution collimator with a 256 × 1024 matrix and a scan speed of 15 cm/min. The imaging parameters for SPECT were as follows: 6° angular resolution and 30 s per step, with a 256 × 256 matrix. Low-dose CT scan parameters were 130 kV and 25 reference mA modulation. After the collection was completed, iterative reconstruction was performed, image fusion analysis was carried out using the supporting special post-processing software, and the area of interest was marked. If the position is added, the method is the same as before.
The criteria for determining positive foci of PSMA imaging8: SPECT/CT images were reviewed by two experienced nuclear medicine physicians, and a final diagnosis was achieved by consensus. Both nuclear medicine physicians were blinded to the clinical information. A positive lesion was identified if 99mTc-PSMA uptake in the lesion was higher than that in the surrounding normal tissue, and was not associated with physiological uptake (salivary gland, eye socket, liver, gallbladder, spleen, small intestine, kidney, and bladder). If the local histomorphology of the same SPECT/CT showed abnormal structural changes but the level of uptake was similar to or reduced in the surrounding area, it was considered a negative lesion.
SPECT/CT whole body bone imaging0.2 mCi/kg intravenous injection of 99mTC-MDP, 3−6 h later imaging, the patient supine position; acquisition instrument: American GE Discovery NM/CT 670 SPECT/CT instrument, using low-energy high-resolution collimator; acquisition parameters: energy peak 140 keV, window width 20%; matrix 256 × 1024, zoom 1, bed speed 15 cm/min, while the whole-body front and rear image scanning.
Biochemical variablesSerum PSA and ALP levels were detected using a chemiluminescence and biochemical analyzer (Roche E6000, Germany) with a reference range of 0−4 ng/mL and 45–125 U/L, respectively.
Statistical analysisStatistical analyses were performed using SPSS software (version 25.0; IBM/SPSS Corp., Armonk, NY, USA). The Kolmogorov–Smirnov test was used to determine data normality. Parametric and non-parametric variables are expressed as mean ± standard deviation (mean ± SD) and median (P25, P75), respectively. The association between PSA and ALP levels in the positive and negative 99mTc-PSMA bone metastases in 43 patients was analyzed using the ROC curve plotted using MedCalc software. Fisher exact probability method was used to examine the changes in 99mTc-PSMA imaging of primary lesions and ALP levels in 17 patients after re-treatment. Statistical significance was set at P < 0.05.
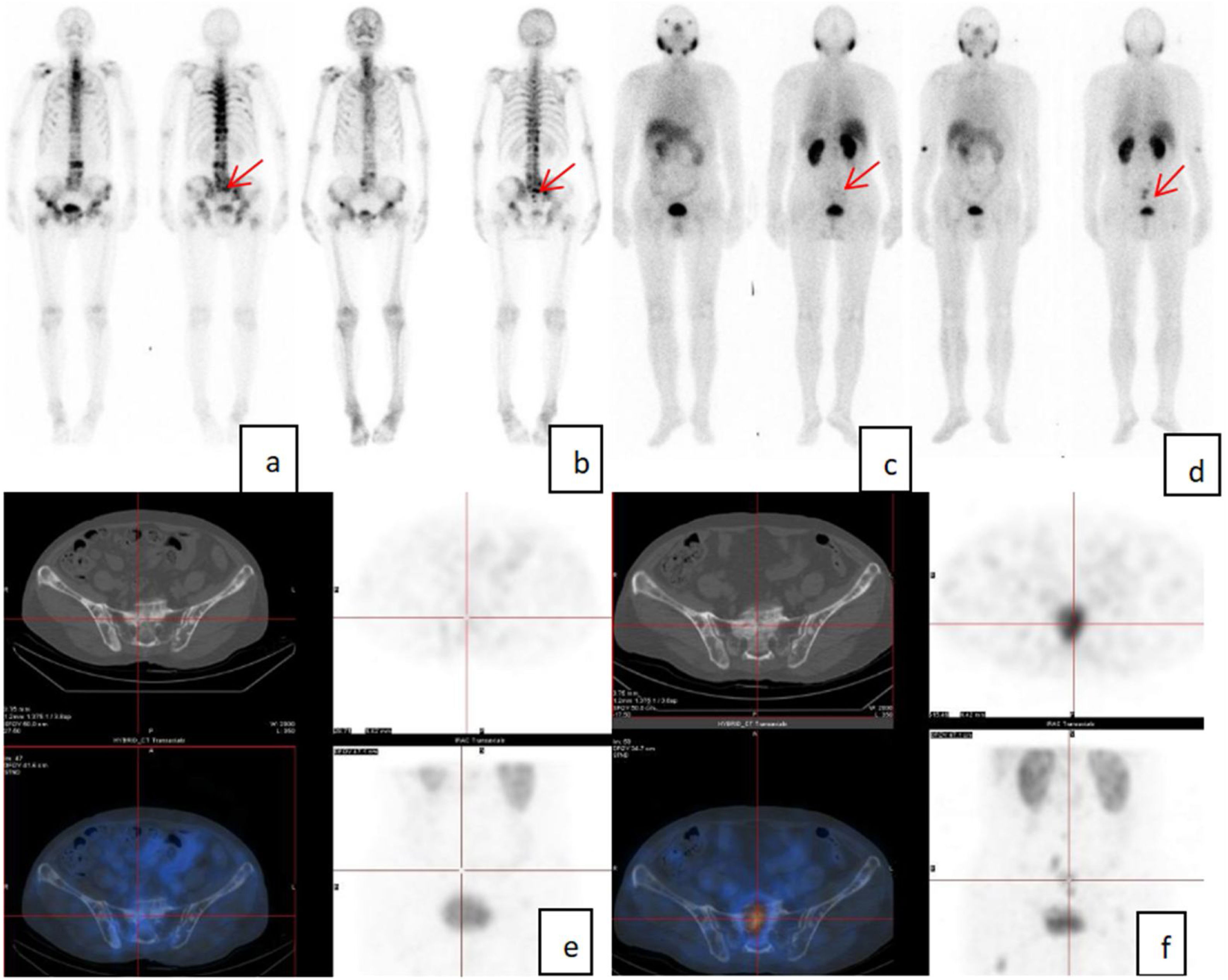
ResultThe mean age of the 43 patients was 69.51 ± 8.31 years old. Whole-body bone imaging showed different degrees of radiation concentrations in all patients. 99mTc-PSMA imaging revealed 31 positive and 12 negative bone metastases. The results of the K-S test showed that PSA and ALP levels did not conform to a normal distribution The median serum level of PSA was 14.30 ng/mL (1.19 ng/mL, 146.20 ng/mL) range from 0.003−2000 ng/mL; The median serum level of ALP 86.000U/L (63.00 U/L, 144.00 U/L) range from 47−3709 U/L. In 17 patients, 99mTc-PSMA imaging was performed again 3–8 months after treatment to detect positive bone metastases in 15 patients, negative bone metastases in two patients, lower PSMA uptake in 7 patients, and higher uptake or increased number of lesions in 8 patients. PSA levels decreased in 7 and increased in 10 patients, with a median serum level of 15.53 ng/mL (0.90 ng/mL, 284.75 ng/mL). ALP increased in 10 patients and decreased in seven patients, with a median serum level of 103.00 U/L (62.50 U/L, 194.00 U/L) (Table 1). The typical cases are shown in Fig. 1.
Patient 99mTc-PSMA imaging and serum levels of PSA and ALP.
| Preliminary diagnosis patient information | subsequent visit | |
|---|---|---|
| Total number | 43 | 17 |
| Age | 69.51 ± 8.31 | 66.88 ± 8.11 |
| 99mTc-PSMA imaging | Positive focus: 31 | Positive focus: 15 (lower uptake in 7; higher uptake lesions number increase in 8) |
| Negative focus: 12 | Negative focus:2 | |
| PSA (ng/mL) | 14.300 (1.19, 146.20) | 15.53 (0.90, 284.75) |
| Rang: 0.003−200 | Decreased:7; Increased:10 | |
| ALP (U/L) | 86.000 (63.000, 144.00) | 103.000 (62.50, 194.00) |
| Rang: 47−370 | Decreased:7; Increased:10 |
A 77-year-old man was diagnosed with PCa 1 year ago, with PSA:3903 ng/mL, ALP: 203U/L; Whole-body bone imaging suggested multiple bone metastases (a). Bone imaging after 1 year of endocrine therapy showed a slight decrease in radiation uptake (b); PSA:15.73 ng/mL, ALP:81U/L;99mTc-PSMA imaging was performed (c, e), which showed that bone destruction was seen in many parts of the bones, and some PSMA uptake was slightly increased, considering that tumor activity was still present in some lesions after bone metastasis treatment. After six months of re-treatment, the re-examination of PSA:47.30 ng/mL, ALP:107U/L, 99mTc-PSMA imaging (d, f) indicated that the tumor activity of some lesions after bone metastasis treatment was still present, and the concentration degree was increased compared with that before treatment (shown by the red arrow at the same site).
ROC curve analysis showed that the highest Jorden index for PSA was 0.60 with AUC = 0.77, 93.55% sensitivity, and 66.67% specificity with PSA cut-off > 1.13 ng/mL for 99mTc-PSMA imaging diagnosis of clinically significant PCa. Moreover, ALP: AUC = 0.770, Jorden index = 0.48, and when ALP > 86U/L, the 99mTc-PSMA imaging diagnostic sensitivity and specificity were 64.52% and 83.33%, respectively (Fig. 2).
Comparative results of 17 patients after treatmentAmong the 17 patients reviewed, PSA levels in seven cases were lower than before, and there was no change or increase in 10 cases. In 99mTc-PSMA imaging, there were seven cases with decreased radioactive uptake, two cases with no radioactive uptake, and eight cases with increased radioactive uptake. ALP levels increased in 10 cases and decreased in 7 cases. The results are presented in Table 1. The changes in 99mTc-PSMA uptake were statistically significant (Table 2).
DiscussionGiven that PSMA is primarily overexpressed in 90–100% of PCa lesions, it has received increasing attention as an attractive diagnostic target. A large body of literature confirms that 68Ga and 18F labeled PSMA PET-CT imaging is a promising method for detecting prostate cancer.11,12 Although PCa diagnosis may be less sensitive than 68Ga-PET/CT, given the broad availability of SPECT/CT devices, lower instrumentation, and radionuclide costs, SPECT/CT systems have great prospects for application to improve PSMA imaging capacity as more patients with prostate cancer undergo PSMA imaging.
In this study, bone imaging showed different degrees of radioactive concentrations in 43 patients. In some patients, even if the PSA level was lower than 0.01, bone imaging still showed mild radioactive concentration, which may be related to bone repair activity, whereas 99mTc-PSMA imaging detected positive bone metastases in 31 cases and no radioactive uptake in 12 cases. Among the 12 patients without radioactive uptake of bone metastases, 10 were soft tissue-positive. Therefore, 99mTc-PSMA imaging was more effective than bone imaging in detecting lesion activity in PCa patients with bone metastases, especially those who were re-examined after treatment, effectively distinguishing simple repaired lesions for accurate diagnosis and treatment.
In this study, ROC curve analysis of the correlation between PSA and this imaging technology found that active bone metastases could still be detected when PSA was as low as 1.13, with a diagnostic sensitivity of 93.55% and specificity of 66.67%, indicating that this imaging technology still has high diagnostic value in patients with biochemical relapse, even when PSA levels are low. This is consistent with the findings of Schmidkonz et al.13 Wellington et al. reported that when ALP > 90, bone metastasis may occur and ALP can effectively reflect osteogenic activity.14 This study showed that when ALP was > 86, the sensitivity of detecting active bone metastases was 64.52% and the specificity was 83.33%, which was similar to a previous study, indicating that ALP has a certain value in predicting the activity of bone metastases. To a certain extent, this can avoid the missed diagnosis of low-activity lesions and assist in the diagnosis of bone metastasis in PCa.
Studies have shown that PSA level is an effective indicator for monitoring biochemical recurrence and therapeutic efficacy in PCa.13,15 In this study, 17 patients were treated again with the original or changed treatment plan, and the reduction in PSA levels after treatment was considered an effective standard of treatment. Among the 17 patients, seven were effective and 10 were ineffective; the PSMA uptake of the imaging lesions decreased in seven cases, no PSMA uptake in two cases, and increased PSMA uptake in eight cases. The Fisher exact probability test showed that 99mTc-PSMA imaging could effectively monitor the therapeutic effect of PCa. Among them, PSA increased slightly in two cases, but both did not exceed 1.00 ng. 99mTc-PSMA imaging suggested that there was no PSMA uptake, which may be related to the low PSA level. ALP was not statistically significant, and there were differences from Schlack K's research,16 which may add to the identification of bmCRPC patients with favorable prognosis, which may be related to the small number of cases. ALP is widely distributed in the human liver, bone, intestine, kidneys, and placenta. Later, endocrine therapy was changed to radiotherapy and chemotherapy for some patients. Chemotherapeutic drugs can also cause ALP changes during liver function damage.17 Therefore, a larger sample size is required to supplement this study.
This study has several limitations. First, this was a small retrospective study, and the results should be interpreted with cautious. Second, when the PSA level is low after endocrine therapy, 99mTc-PSMA imaging may yield false-negative results, and previous studies have reported that when PSA levels are low, 99mTc-PSMA SPECT/CT detection of lesions is lower than 68Ga-PSMA PET/CT.18 Moreover, 99mTc-PSMA SPECT/CT may be a potential alternative to 68Ga-PSMA PET/CT in high-risk patients.
Conclusion99mTc-PSMA SPECT/CT imaging can detect PCa bone metastases, which are related to PSA levels. When PSA > 1.13 ng/mL, the sensitivity of diagnosis and detection of positive bone metastases is higher, and when ALP > 86U/L, 99mTc-PSMA imaging has higher specificity. However, it is easily affected by multiple factors, and attention should be paid to whether relevant influencing factors exist in the application process.
Ethics approvalMedical Ethics Committee of Henan Provincial People's Hospital [No. (2019)108].
Authors contributionsXR: Responsible for data statistics and paper writing.
YG: Responsible for experimental guidance and paper revision.
FundingNone.
Conflicts of interestThe authors declare no conflict of interest.
Data availability statementThe data that support the findings of this study are available on request from the corresponding author.
This work was supported by cases and data provided by the Nuclear Medicine Department of Henan Provincial People's Hospital.