A fifty-year-old healthy, Portuguese male, with prior history of paraffin injections into the penis 30 years ago, was referred for urological consultation because of a large, hardened ulcerated mass on the base of the penis causing deformity and pain. The patient underwent a biopsy that showed a benign granulomatous lesion, and then excision of the mass and penile plasty with a scrotum flap in the same surgical time. Histology confirmed the diagnosis of paraffinoma. Three months after surgery, the patient is satisfied with the functional (urinary function and erectile function) and aesthetic results.
Penile paraffinoma is a rare disease (most common in Asia and Eastern Europe) and results from an inflammatory response to the subcutaneous injection of paraffin, Vaseline or other mineral oils. Treatment is usually surgery.
Un varón de 50 años de edad, nacionalidad portuguesa y con un histórico de inyecciones de parafina en el pene desde hace 30 años, que es referenciado para la consulta de urología por una gran masa ulcerada en la base de pene, que causa deformidad y dolor. El paciente ha sido sometido a una biopsia que reveló una lesión granulomatosa benigna. Puesto esto, ha sido sometido a la escisión de la masa y a una reconstrucción plástica del pene. La histología confirmó el diagnóstico de parafinoma. Pasados 3 meses de la cirugía el paciente quedó satisfecho con los resultados funcionales (funciones urinaria y eréctil) y estéticos. El parafinoma del pene es una enfermedad rara (más común en Asia y Europa del Este) y resulta de una respuesta a la inyección subcutánea de parafina, vaselina o otros óleos minerales El tratamiento suele ser habitualmente la cirugía.
Penile paraffinoma (also called oleoma or sclerosing lipogranuloma) results from the subcutaneous injection of liquid paraffin with the aim of increasing penile volume for cosmetic purposes.1,2 Injection of paraffin or other saturated hydrocarbons (like Vaseline) in the genitals for cosmetic use was first described in the late XIX century by the Austrian surgeon Robert Gersuny, although complications from the procedure have since caused the end of its use by medical professionals.2–4 Regardless, injections of paraffin into the penis is still in practice around the globe by auto injection or administered by non-medical professionals, in uncontrolled environments, existing an increasing number of published cases describing complications.3,5 Analysing epidemiology, less than 130 cases of paraffinoma are published in literature (PubMed), most cases occurring in Eastern Europe and Southeast Asia.3
Patients with penile paraffinoma present with a vast arrange of symptoms, penile pain (30.2%), ulcers (15.4%) and deformity (11.4%). Symptoms may arise a few days after injections or years later, depending on the inflammatory response of each individual.3
The work presented describes the case of a giant penile paraffinoma and its surgical treatment, being the first case described in a Portuguese male.
MethodsClinical data was obtained by consulting the patient's medical records. Bibliographic review was conducted utilizing the terms “penile paraffinoma” and “penile oleoma” on PubMed platform.
ResultsClinical caseA 50 years old, Portuguese male, smoker, without any other relevant medical history, resorted to his doctor due to a penile ulcer with one year of evolution (Fig. 1). Patients had a prior history of subcutaneous injections of paraffin into the penis 30 years ago, having repeated the procedure 10 years after the first injections, aiming to further increase penile volume. Due to the existence of a clinical suspicion of a malignancy of the penis, the patient was orientated to a urology consult in an oncological hospital.
In the medical appointment, an ulcerated wound of 5cm in the body of the penis was identified; it was deep, with exudate and locally hardened. A notorious deformity of the base of the penis was present, with hardening extended to left hemiscrotum. The foreskin was swollen and difficult to reduce but the gland presented with no alterations. There were no palpable inguinal nodes. Miccional dynamics and erectile function were maintained.
Complementary diagnostic exams- •
Microbiology of exudate: contamination;
- •
Sexual transmitted diseases screening: HIV, syphilis, gonorrhoea and Chlamydia were negative;
- •
Pelvic and penile Magnetic resonance (MRI): penile exam of difficult characterization by artefacts of movement; inguinal and iliac bilateral lymphadenopathy, the largest in the iliac left chain with 30×22mm.
- •
Paraffinoma: Patient with a history of subcutaneous injections of paraffin, having been described complications as penile deformity cutaneous ulcers.
- •
Penile cancer: macroscopically characteristics were compatible with penile cancer, such as the deep ulcer and the mass on the base of the penis. The presence of inguinal and iliac lymphadenopathies supports this diagnosis.
- •
Infection: the presence of an ulcer with exudate and lymphadenopathies on MRI support this diagnosis. The mass at the base of the penis that causes deformity is against this hypothesis.
Surgical biopsy of the lesions was proposed to the patient (after 2 weeks of oral antibiotic with cefuroxime) with extemporaneous study. Depending on the histological result (paraffinoma or penile cancer), excision of paraffinoma or partial penectomy was proposed.
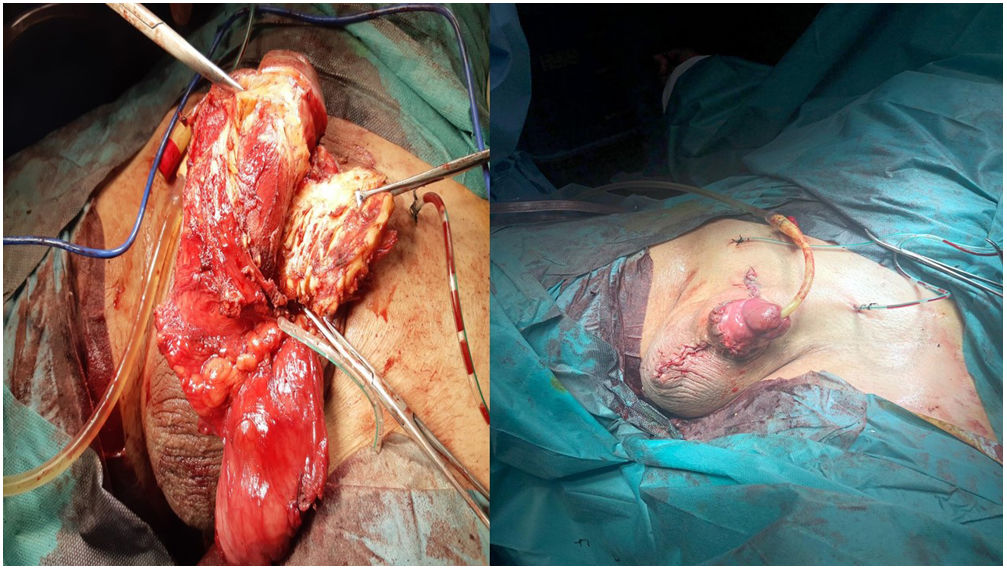
Deep tissue biopsies from the two lesions were taken (ulcer and base of the penis), having the extemporary result objectified a granulomatous lesion of benign characteristics compatible with secondary lesions from injections of paraffin as such, surgical excision of paraffinoma with the primary goal of preserving penile function was performed (Fig. 2).
Surgical technique- •
Medial incision above the base of the penis with approximately 6cm in length, to perform the previously described biopsy.
- •
Scrotal “inverted V” incision, identifying and isolating the cord and left testicle.
- •
Merger of both incisions limiting surgical margins. Excision of the paraffinoma localized in the left side of the scrotum and subcutaneous tissue around the penis.
- •
Degloving of all the penis and confirmation lesion location external to buck fascia. Excision of the remaining lesion.
- •
Plasty of the penis with a flap of scrotum skin in a modified “Y-V” fashion, due to the extension of the dissection.6
The final histological result confirmed the diagnosis of paraffinoma. Three months after surgery, patients presented with good tissue healing, maintains the ability to pass urine standing and erectile function. The aesthetical result was satisfactory to the patient (Fig. 3).
DiscussionIn an initial phase, injection of mineral oils into the penis results in an increase in penile volume. With time, the materials added can move to adjacent tissues (or even along the spermatic cord). The associated inflammation with the formation of nodules causes what in the end is called foreign body granuloma, which causes necrosis of tissue by anatomically deforming then, reducing vascularization.2,7
A recent review (124 cases of paraffinoma) identified the most common symptoms of penis paraffinoma: penile pain (30.2%), fistula/ulcer (15.4%), penile deformity (11.4%), problems in retracting the foreskin (8.7%) and difficulties in bladder emptying (5.4%). Other serious or even fatal complications may arise such as, gangrene and sepsis with palpable inguinal lymphadenopathies (4.7%).3 The present clinical case, beyond presenting almost all the descried forms of presentation has two additional peculiarities: (1) the clinical manifestation presents only after two decades of the last injection, being the medium time of presentation described of 24 months3; (2) a large volume lesion.
Both ultrasound and MRI of the penis have been used during study and planning for treatment. On the ultrasound, paraffinoma is described as an hyperechogenic lesion with thickening of the surrounding subcutaneous tissue.8 On MRI, paraffinoma is described as hypointense in T1 and T2, presenting a slight contrast effect after gadolinium.3 Changes on MRI might differ depending on the product injected, having been described hyperintense lesion in T1 and T2 after injection of silicone and baby oil.7
Treatment depends on the dimension and location of the lesion. Although some minor cases can be approached by conservative measures (antibiotics, analgesia, topical injection of corticoids),9,10 the vast majority of cases require surgery. Small lesions can be treated by incision and primary closure, although in other cases an extensive subcutaneous and penile debridement may requiring a plasty. Reconstructive technique depends on the extent of the defect and has function and aesthetic objectives. The techniques utilized include skin grafts and cutaneous flaps from the foreskin or scrotum. The most widely used technique is the scrotal skin bipeducalated flap, conducted during the same operating time, with a very good success rate.3 In a minority of cases, more complex plasty techniques are required conducted in a second operating time.3,11
It is to be noted that a case of penile cancer associated with granuloma after injection of mineral oil has been reported,12 making the exclusion of this diagnosis fundamental before surgical planning.
Regardless of the few described cases, it is likely that in some social circles many other men have resorted to subcutaneous injection of saturated hydrocarbons with the aim of increasing the size of their penis. Embarrassment due to this pathology may lead to patients not seeking medical attention or omission of previous infections. With the recent increase in the number of cases reported in the west and due to immigration fluxes, the possibility of paraffinoma must be present in the differential diagnosis of deforming and ulcerated lesions of the penis.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Financial supportNone.
Conflict of interestNone.