The thrombophlebitis of the superficial dorsal vein of the penis, called Mondor's penile disease (PMD), is a condition with a low incidence worldwide. In general, it is considered a self-limited disease that usually resolves with conservative management and very rarely requires surgical intervention. We report the case of a 41-year-old patient, who presented PMD which persists after medical treatment with nonsteroidal antiinflammatory drug and low molecular weight heparin. Surgery was decided and thrombectomy plus resection of the superficial penile vein was performed with satisfactory results. A review of the literature is presented, focusing on the limited available evidence of surgical management.
La tromboflebitis de la vena dorsal superficial del pene, también llamada enfermedad de Mondor, es una condición infrecuente que generalmente es auto-limitada. Usualmente mejora con el tratamiento conservador y rara vez requiere intervención quirúrgica. Reportamos el caso de un paciente de 41 años que a pesar del uso de antiinflamatorios no esteroideos y de heparina de bajo peso molecular no tuvo resolución del cuadro clínico. Se realizó trombectomía y resección de la vena dorsal superficial del pene de manera satisfactoria. Se presenta una revisión de la literatura, enfocada en la poca evidencia disponible sobre el manejo quirúrgico en esta enfermedad.
Mondor's disease was described for the first time as a thrombophlebitis of the superficial veins in the chest wall by Henri Mondor in 1939.1 It was until 1958 when Helm et al. published the first case affecting the superficial dorsal vein of the penis (SDVP). Since then, less than 100 cases have been reported and still being a rare and under-recognized condition. Cases needing surgical intervention after medical treatment failure are exceptional. Only 7 cases requiring surgery have been informed in the literature.2–5 Hence, we decided to report this case and to expose a narrative review of this topic.
Clinical caseA 41-year-old male presented with high intensity pain and edema in the dorsal region of the penis, experienced for the last 3 days. He had sexual relationships few days before and denied any other type of trauma. He had no urinary symptoms, urethral discharge or genital ulcer suggestive of a sexually transmitted disease. The patient had no previous diagnosed pathologies, no consumption of drugs and no history of surgical interventions. On physical examination, a subcutaneous cord-like mass was inspected in the middle and proximal dorsal third of the penis. It was indurated and painful when palpation was performed. Also, redundant foreskin was observed (Fig. 1).
Colour Doppler of the penis revealed a echogenic material in the proximal third of the SDVP suggestive of thrombus, with secondary absence of venous flow. Complete blood count, prothrombin and partial thromboplastin time were normal. No alteration in hepatic and renal function tests was found. The patient was discharged from the hospital with oral non-steroidal antiinflammatory drugs (NSAIDs) for five days and subcutaneous enoxaparin in prophylactic dose for 10 days. In outpatient care, the hematologist ruled out prothrombotic conditions including thrombophilia like a possible cause.
Three weeks later, the patient consulted in the emergency department for no improvement in the indurated area and pain exacerbation after sexual intercourse. Doppler ultrasound showed no changes comparing with the previous study, and blood laboratories were normal again. Full-dose anticoagulation with enoxaparin 80mg BID was started and opioid analgesia (hydromorphone) was needed for pain control. Because there was no satisfactory response to medical treatment, surgical management was considered.
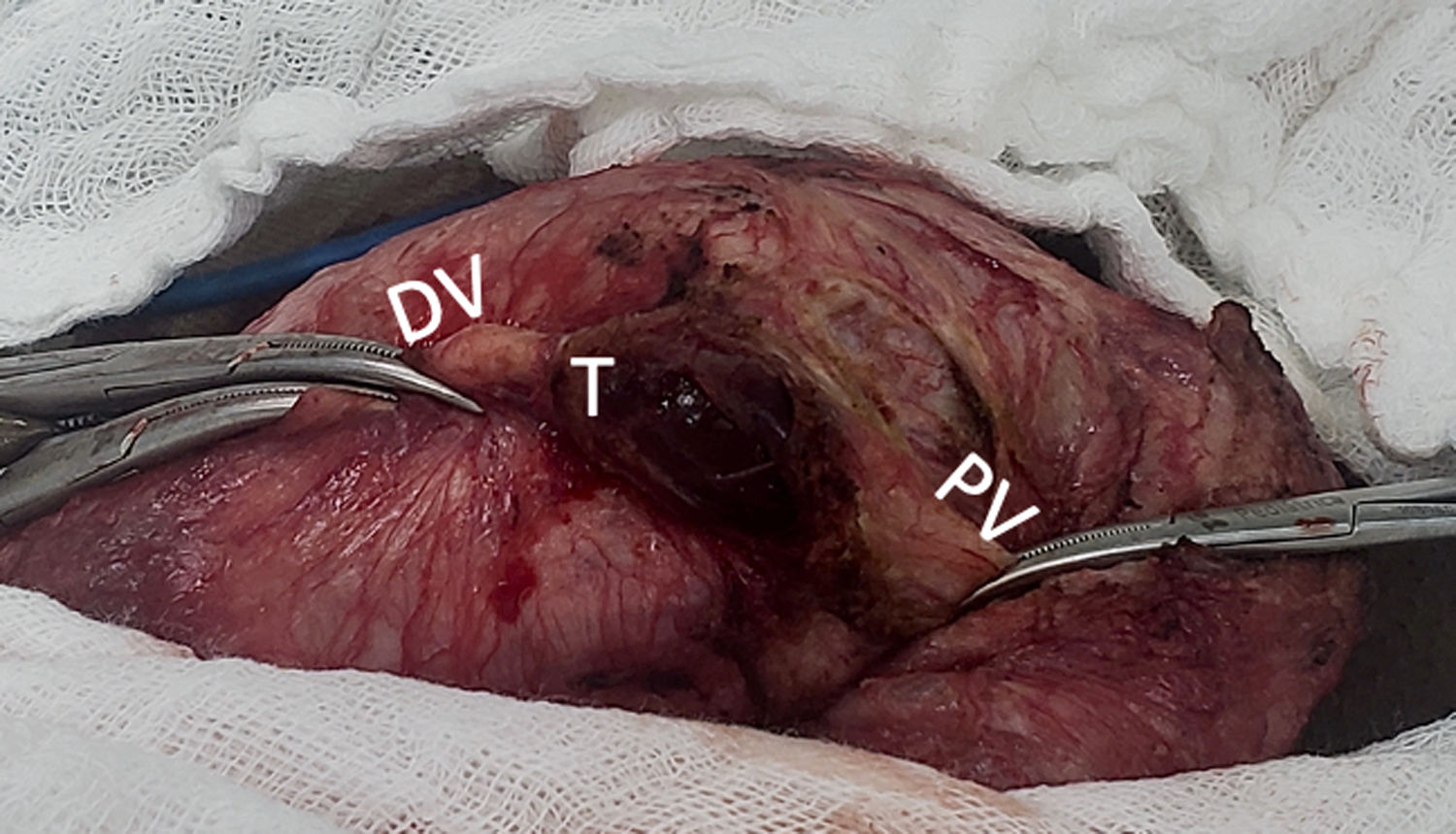
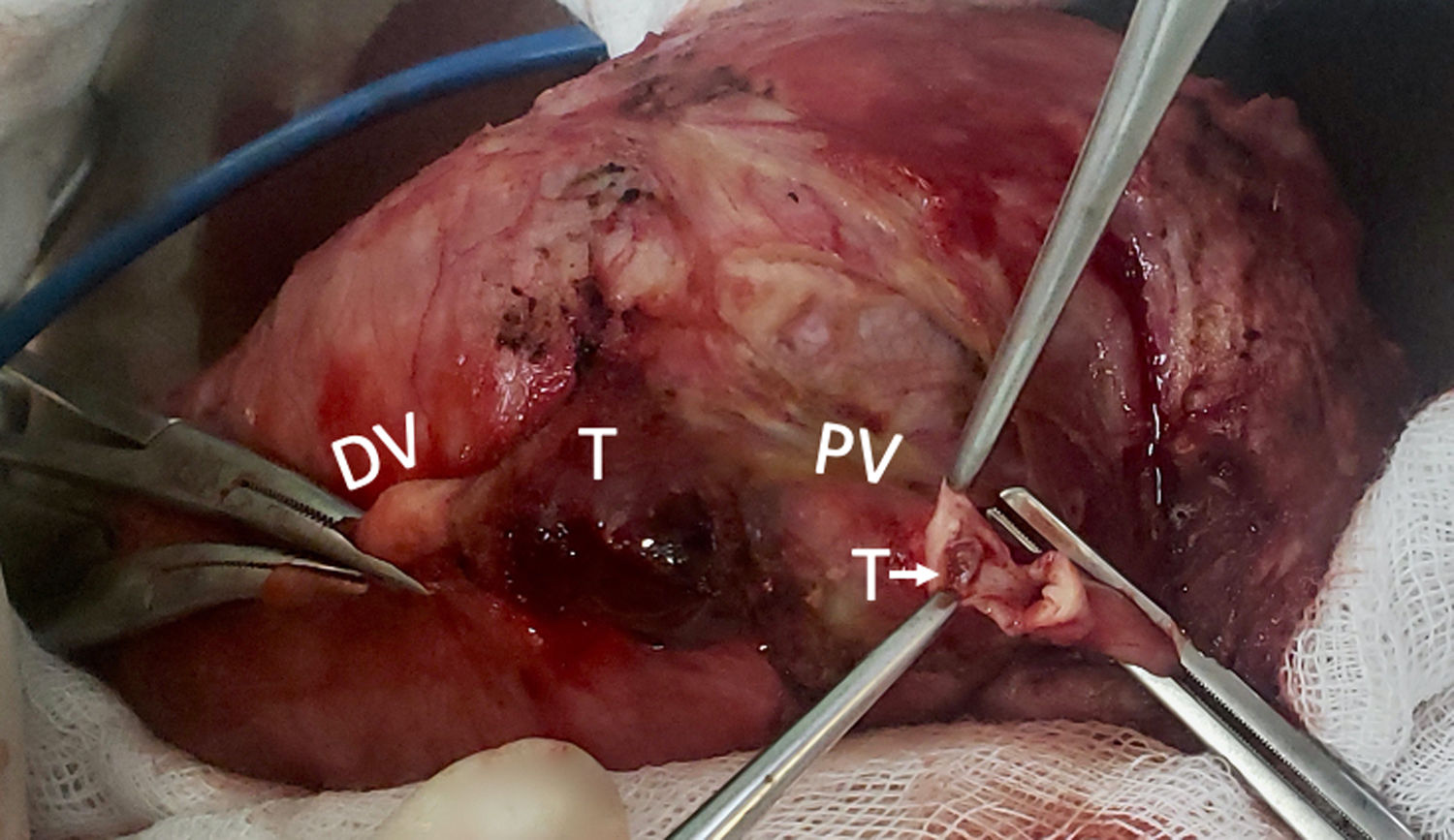
The surgical technique started by a circumferential incision near the coronal sulcus and complete degloving of the penis. The SDVP was dissected and the thrombus on its trajectory was exposed, evidencing fibrosed and indurated tissue (Fig. 2). Because of this, thrombectomy alone was not possible and vein resection was decided. Subsequently, the proximal and distal part of the SDVP was clamped. Using proximal incision the vein was washed with heparinized saline solution employing a 16 gauge jelco (Fig. 3). Proximal and distal ligation of the vein with non absorbable suture was performed and resection of the affected vein segment including the thrombus was completed. Then, circumcision was realized removing the redundant foreskin. The skin was joined to the mucous using a synthetic absorbable suture and the surgery finished without any complication.
After the surgery, his symptoms were totally resolved. On the second postoperative day, he was discharged from the hospital with oral analgesic and thromboprophylaxis with SC enoxaparin for 10 days. The patient was followed until the next 6 months and persists asymptomatic, with good esthetic results and a satisfactory sexual activity.
DiscussionMondor's penile disease (MPD) corresponds to the thrombophlebitis of the superficial penile vein of the penis, with an estimated incidence of 1.4%. It appears between 18 and 45 years old, being 29 years the average age of presentation.6 Few cases have been reported, because it is uncommon but also underdiagnosed. The largest case series involves only 25 patients included in 7 years,4 followed by a case series that reported 10 patients in a period of 3 years.5 In Colombia, the first case was reported in 2018 by Castañeda et al., only two cases have been published until now.7,8
The superficial penile venous system drains the blood from the penile skin, the prepuce and the base of the glans. Small veins from these locations converges to form the SDVP, which runs longitudinally in the subcutaneous tissue, outside the Buck's fascia. It drains into the external pudendal vein, a branch of the great saphenous vein.9 Because of the superficial trajectory, this vein is susceptible to suffer trauma during sexual intercourse. Microtrauma related with sexual intercourse causes injury to vein wall, conducing to stasis and clot formation. Therefore, frequent, prolonged and vigorous sexual activity is the most common associated etiologic factor, usually preceding the appearance of the lesion by 24–48h.10
Other less common implicated factors are: sexual abstinence, use of vacuum erection device, prolonged erection associated with the administration of a PDE5 inhibitor and intracavernosal injections. Vasculitides (e.g. Behcet's disease) and conditions with hypercoagulable state, like local or distant infections, sickle cell disease and neoplasms (especially pelvic tumors) are also related. Retroperitoneal, pelvic and lower extremity surgeries have been described as well.11
Medical history and adequate physical examination are usually enough for the diagnosis of PMD. As it was described previously, a history of intensive sexual intercourse in the recent days is common (generally less than one week). The patient typically refers localized pain and induration in the trajectory of the SDVP, or even focal sensitivity lost. The inspection usually reveals a cord-like lesion with no more than few centimeters, which is hardly indurated when palpation is performed.12 Inflammatory reaction of nearby tissue could be also present. Rarely, the lesion can extends to the suprapubic region.6
When clinical findings are not clear and doubt for the diagnosis persists, Doppler ultrasound can be helpful. Classic findings comprise the presence of echogenic material within lumen and flow absence in the SDVP. Inflammatory changes in the vein wall and increased caliber of the vein can also be observed. When Doppler is performed, it should confirm an adequate flow in the deep dorsal vein too.6 The need for additional imaging tools like magnetic resonance is exceptional, but have also been described.12
PMD is generally self-resolved at 6–9 weeks.8 Medical treatment is focused on symptomatic management, which includes pain relievers, anti-inflammatories and topical or subcutaneous anticoagulants.7,13 Infiltration with local anesthetics have also been described when pain relief is not achieved. Successful response to conservative management is high, as evidenced in the 92% of the cases reported by Al-Mwald et al.4
Surgical intervention including thrombectomy and resection of the superficial penile vein are practiced when medical treatment has failed in persistently symptomatic patients. Another indication is the absence of vein flow or the presence of thrombus in the penile doppler ultrasonography taken after six weeks of conservative management.1,14 Fortunately, this treatment option is rarely needed. In one of the largest available series, published by Al-Mwalad et al., only 2 of 25 patients required thrombectomy.4 Likewise, Sasso et al. reported that 2 of 10 male with this condition were treated with vein resection.5
Rodríguez et al. published an interesting case of a 24-years-old man with juxtafrenular venous thrombosis, an unusual form of presentation. Frenulectomy and a resection of the thrombosed juxtafrenular vessel were successfully practiced after the lack of response to conservative treatment.15 Only other two single cases requiring surgery have been reported.2,3
The conventional surgical technique involves circumcoronal incision and degloving of the penis. Thrombosed vein will appears dorsally, above the deep fascia. The compromised segment must be carefully dissected, ligated and completely excitioned. Then, the degloved skin is returned to its position and sutured. Postoperative recommendations includes sexual abstention for six weeks.3
ConclusionsMondor's penile disease is an uncommon urological condition that generally resolves with conservative management. A multidisciplimary approach involving haematology for descarting pro-thrombotic conditions is suggested. Surgical intervention should be offered after medical treatment failure, including thrombectomy or vein resection. Few cases requiring surgery have been reported, but all of them have achieved good results. Having in count the few available evidence, urologist must have these procedures in mind as the last treatment step but knowing that is a safe procedure with high success rate.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestThe authors declare that they have no conflict of interest.