Cavernous body thrombosis is a rare condition. The etiology and pathophysiology of this entity is still poorly understood and there is no clear diagnostic and treatment algorithm. The objective of this article is to publish a clinical case of a partial segmental thrombosis of the corpus cavernosum and present a flow chart for diagnosis and treatment based on the review of the published literature on this disease.
La trombosis del cuerpo cavernoso es una afección rara. La etiología y la fisiopatología de esta entidad todavía son poco entendidas y no existe un algoritmo de diagnóstico y tratamiento claro. El objetivo de este artículo es publicar el caso clínico de una trombosis parcial segmentaria del cuerpo cavernoso y presentar un flujograma para el diagnóstico y el tratamiento basados en la revisión de la literatura.
Cavernous body thrombosis is a rare condition that consists of a thrombosis in the perineal portion of the cavernous body. It is also known as “partial segmental priapism” or “partial segmental thrombosis of the corpus cavernosum” or even as “partial idiopathic thrombosis of the corpus cavernosum”.1
In May 1976, Gottesman published in the Urology journal the first case of partial segmental cavernous thrombosis. Since these, less than 100 cases have been reported in the literature.2
The etiology and pathophysiology of this entity is still poorly understood and there is no clear diagnostic and treatment algorithm. The objective of this article is to publish a clinical case of a partial segmental thrombosis of the corpus cavernosum and present a flow chart for diagnosis and treatment based on the review of the published literature on this disease.
MethodsA 28-year-old male with no history of previous illness or surgery came to the consult for perineal pain of 30 days of evolution. He mentioned to the use of motorcycle as a means of transport and horse riding as a sporting practice. On physical examination a slight induration of the left cavernous body of the penis at its base was palpated at the level of the urogenital triangle.
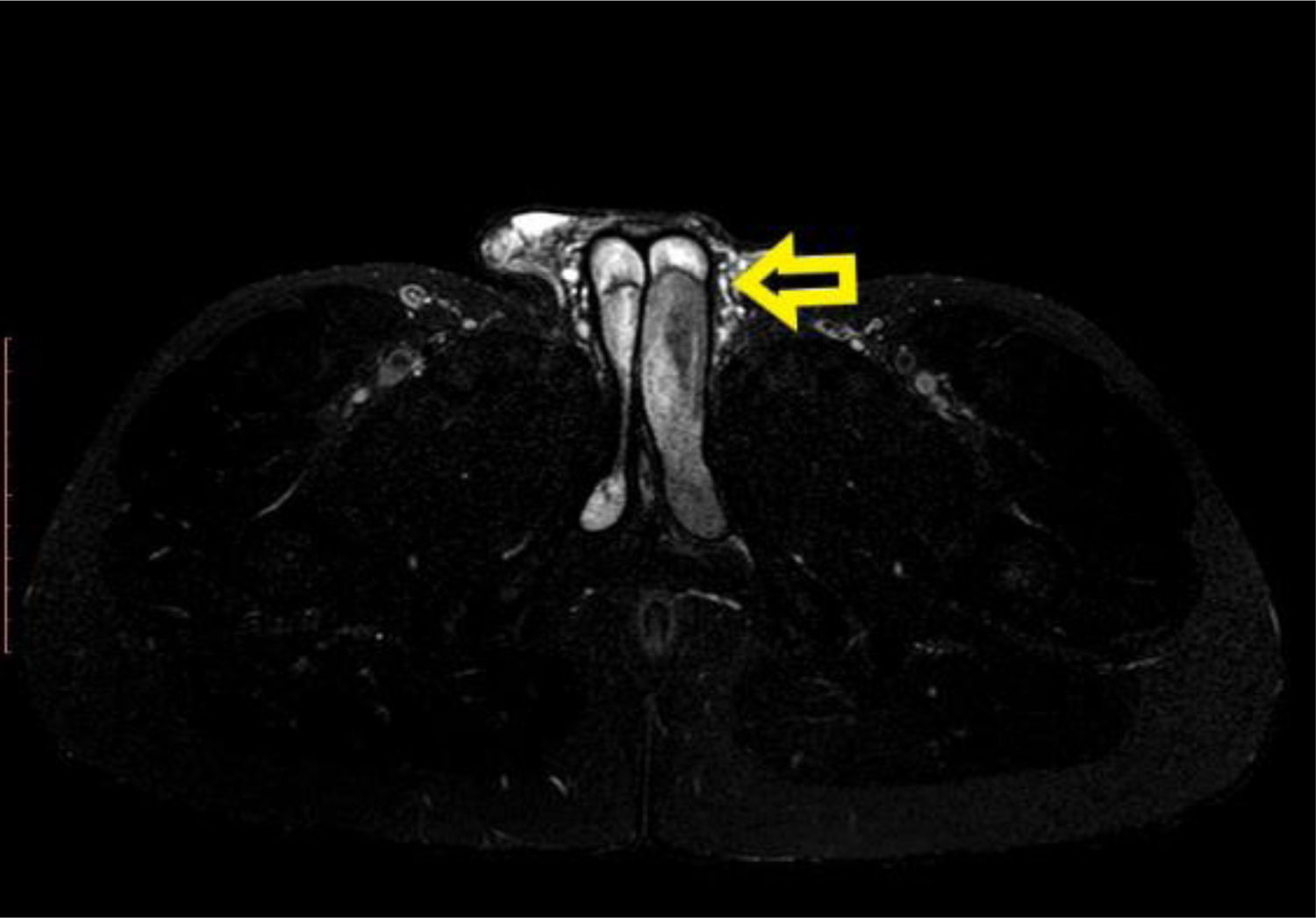
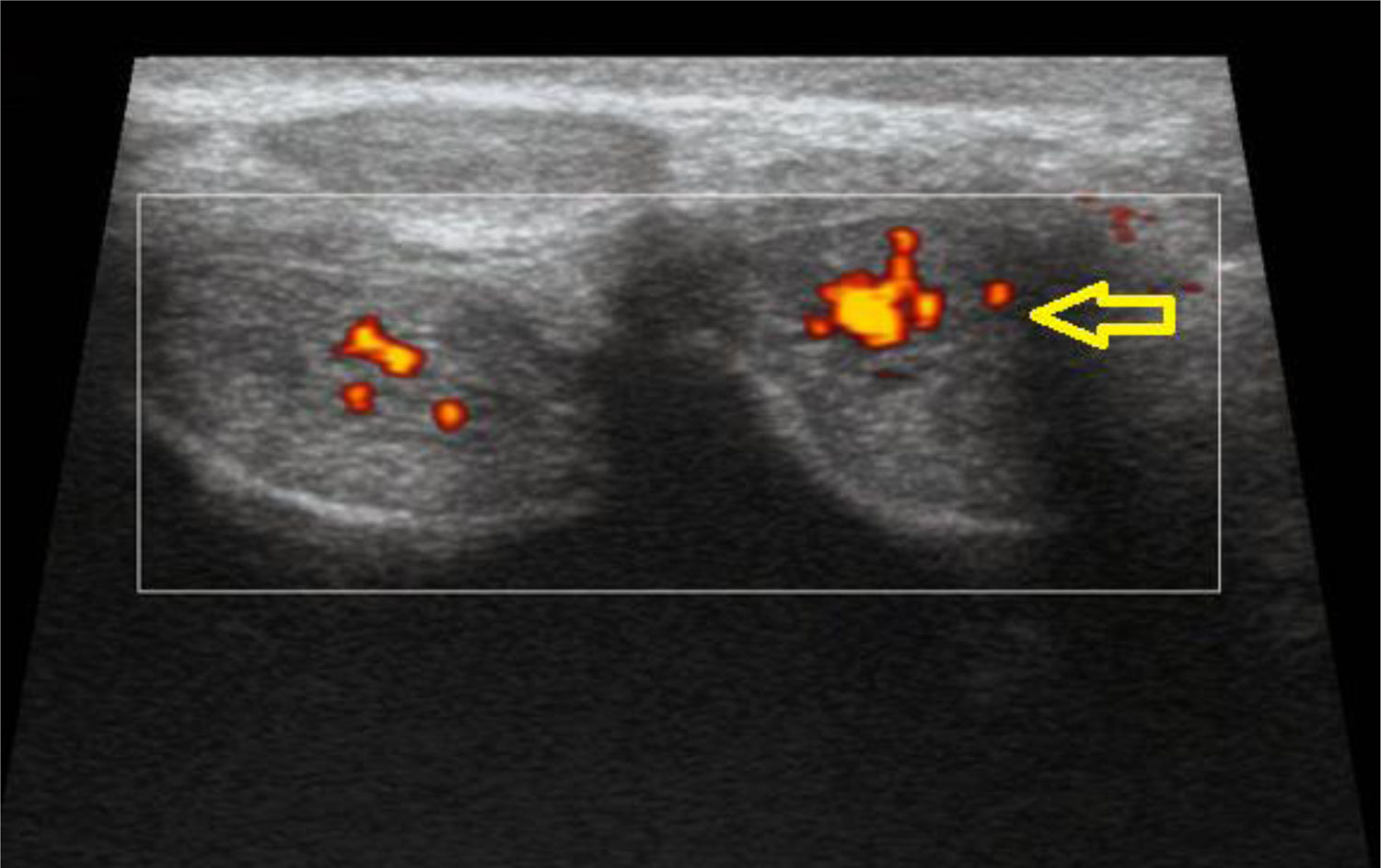
ResultsIt was requested an ultrasound of the penis that showed a frank increase in the size of the perineal portion of the left cavernous body with poor internal vascularity to the examination with Doppler. Subsequently, a Nuclear Magnetic Resonance of the pelvis with Gadolinium was performed. A left cavernous body was evidenced larger than the contralateral in its perineal path with remains of blood material separated by a thin membrane that caused a displacement and compression of the right cavernous body. The distal penile segments of both corpora cavernosa and the spongy body showed morphology and conserved intensity signal. These findings were informed as signs in favor of a partial thrombosis of the left cavernous body (Fig. 1). Blood samples obtained no significant results found.
The differential diagnoses that were considered were the priapism, penile tumor, Peyronie's disease, penile trauma and idiopathic thrombosis of the corpora cavernosa. Based on the findings found by the images, it was concluded as a definitive diagnosis of a segmental partial thrombosis of the left cavernous body.
Analgesia with diclofenac and sexual rest were indicated as treatment. The patient was referred to hematology to evaluate the possibility of anticoagulation. The hematologist confirmed anticoagulation and the patient started acenocumarol 2mg daily. Controls were indicated with monthly ultrasound.
In the first control, penile ultrasound reported a slight increase in the size of the left cavernous body at proximal level while preserved its usual echostructure without observing focal lesions. At the second control, the penile ultrasound showed a normal appearance of both corpora cavernosa with no evidence of thrombosis at the Doppler so the patient stopped the anticoagulation (Fig. 2).
DiscussionSegmental partial thrombosis of the corpus cavernosum (SPTCC) is a rare condition, usually occurring in young men with a mean age of 30 years (range 18–59 years).1,5,7
It was previously called partial priapism due to the stiffness of the corpora cavernosa (CC). However, these two entities differ because unlike priapism, in partial thrombosis only the proximal and perineal portion of the CC is affected; therefore, the distal portion of the penis is flaccid.1,8,9
In most cases the condition is unilateral.3–5 In a review of 26 cases, in 59% of cases, SPTCC was located on the left side, in 34% on the right side and in 7% the condition was bilateral.7
The risk factors associated with SPTCC are hematological abnormalities such as thrombophilia, spherositosis, sickle cell disease, leukemia or lymphoma; microtrauma secondary to exercise (cycling) or during sexual activity; alcohol or drug abuse (such as cocaine or marijuana); hypercoagulability associated with dehydration, surgery, tumors and long-distance flights; other factors have also been related, such as a history of prostatitis, treatment with tamsulosin or sildenafil, fever of unknown origin, prior idiopathic priapism and a history of hepatitis A or hyperhomocysteinemia.3,7,9 In a literature review by Weyne E et al., which included 38 cases with SPTCC, eleven patients (61%) reported being frequent cyclists and in 8 (44%) the episode occurred after or during cycling.5 In our case we identified two risk factors associated with microtrauma, motorcycle use and the equitation, not described in other case report or series of cases.
The pathophysiology of the disease is still unclear. Weyne et al. describes in 18 cases studied by magnetic resonance imaging (MRI), a fibrous network at the level of the cruro-cavernous junction or distal to it. The fibrous network was more frequently present bilaterally (59%) than unilaterally (41%). The author explained that this network is congenital and not caused by the thrombus. The presence of the fibrous network provides an explanation of the appearance of SPTCC in at least those patients who present perineal compression or any limitation to the crural venous flow. Stasis of venous blood occurs and this results in an increased risk for thrombus formation.5
In 2011, Ilicki et al. postulated a bicausality model in which primarily a transverse membrane is required, dividing the CC into a proximal and distal portion, and secondly a triggering event (possibly a microtrauma) to block the permeable parts of the membrane. If these two situations occur together, local venous stasis would occur with the production of partial thrombosis of one or both cavernous bodies.6 This theory is supported by other authors and is what we agree with.3–7
The clinical presentation includes perineal or penile pain (85%) and palpable perineal mass (81%).1,6,9,10 Painful erections are another symptom commonly reported in about half of cases and penile curvature is relatively uncommon (10%).6 Depending on the position of the thrombus, the penis may appear semierect.4 Other associated symptoms at the time of diagnosis are erectile dysfunction and the presence of urinary symptoms (dysuria and/or lower urinary tract symptoms).1,8–10
Complementary studies should include Doppler ultrasound as an initial test because it can be diagnostic when changes in volume, echogenicity and an absent vascular flow within the CC are observed.1,5–7,9 In 1985, computer tomography (CT) was first used as a diagnostic method for SPTCC.11 On CT, thrombosis will appear as an area of low density (which approximates the density of the liquid) confined to the segment of the affected cavernous body.3
In 1988, two cases of SPTCC diagnosed by MRI were reported.12 Nowadays, MRI is used to confirm the diagnosis and it can be used to differentiate between SPTCC, penile cancer, Peyronie disease, abscesses and penile fracture.1,8,9 In MRI images, the lesion will be appear as a widened segment of the cavernous body, which often compresses the contralateral cavernous body. T1-weighted images will show that this segment is hyperintense and the T2-weighted series will show that it is hypointense compared to normal cavernous structure with lack of contrast enhancement. The MRI can show the typical septum (hyperintense in T1-weighted exploration) that separates the thrombosed part (always proximal) from the non-thrombosed.1–9 These findings were identified in the MRI study in our case.
The treatment of SPTCC is currently under discussion. Historically, it was treated with surgical interventions, such as surgical corporotomy and clot evacuation. However, the latest reports clearly support a conservative management.1 Several publications have reported successful treatment with non-steroidal anti-inflammatory drugs (NSAID). However, low molecular weight heparin has been used more frequently, although the benefit over NSAIDs is unclear.1,5,8,9
Christodoulidou M et al. (2016) reported the first case treated successfully with oral rivaroxaban. This author proposed to consider a factor Xa inhibitor for treatment and suggested a prior consultation with a hematologist for a routine blood test and a thrombophilia test before starting with anticoagulants.3 Following this author, but for a better monitoring of anticoagulation and for a lower cost, our patient was prescribed with acenocoumarol. In the review of Weyne E. et al., the mean duration of treatment was 12 weeks, with a complete resolution of 97% and a recurrence after conservative treatment of 5%.5
More invasive treatments would only be recommended in cases where conservative treatment has failed.1,9
Long-term complications are still unknown after the treatment of SPTCC. For follow-up it is recommended to obtain periodic MRI images as this will identify the resolution of the thrombus.3
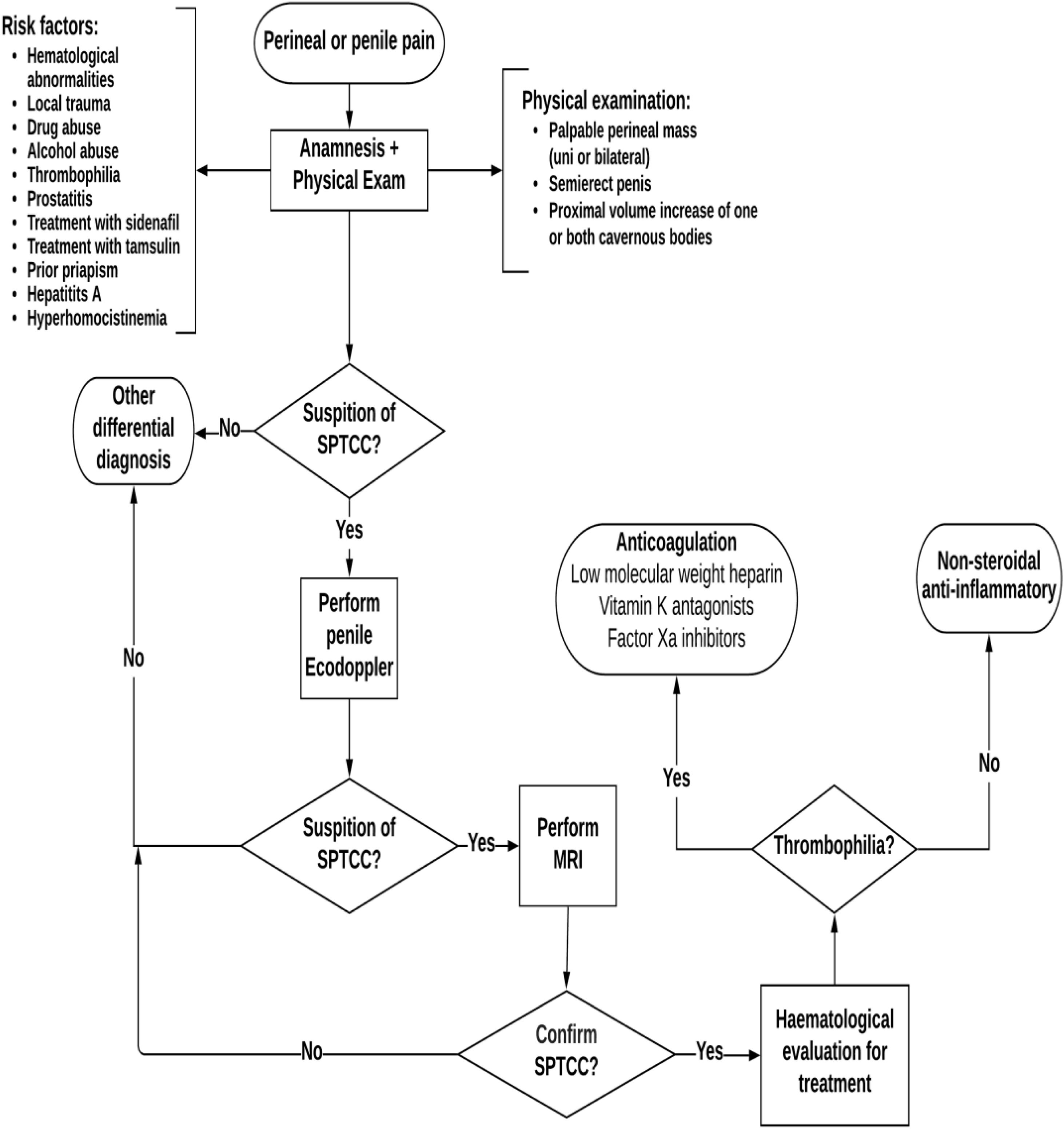
To finish, we propose a diagnostic-therapeutic algorithm for the management of SPTCC (Fig. 3).
ConclusionsSPTCC it should be suspected in cases of a painful unilateral perineal tumor with a history of previous risk factors.
Although several risk factors have been described, the exact etiology is still unclear and further studies are needed to confirm the pathophysiology of this entity.
Doppler ultrasound and MRI are imaging studies that must be requested for the diagnosis.
Conservative treatment should be the first option because provides functional satisfactory results.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent.The authors declare that no patient data appear in this article.
Conflict of interestThe authors declare that they have no conflict of interest.