Glandular ischemia is an extremely uncommon dreaded postoperative complication of inflatable penile prosthesis surgery that may lead to penile gangrene and organ loss, whose incidence is difficult to determine. We report the case of a 56-year-old male admitted to our department with complaints of cold and painful glans penis after penile implant one month before. A color Doppler examination revealed the normal intracavernosal arteries with no vascularity in the superficial glans tissues. Due to the mild severity of the ischemia, conservative management was suggested, and consisted of oral pentoxifylline and hyperbaric therapy for 10 days, achieving a significant improvement at 4 months of follow-up.
La isquemia del glande es una complicación extremadamente infrecuente de la cirugía de prótesis de pene inflable, que se trata postoperatoriamente, que puede originar gangrena y pérdida del pene, y cuya incidencia es difícil de determinar. Reportamos el caso de un varón de 56 años ingresado en nuestra unidad, que se quejaba de frío y dolor en el glande, tras un implante de pene un mes antes. El Doppler color reveló la ausencia de vascularidad en las arterias intracavernosas de los tejidos superficiales del glande. Debido a la leve gravedad de la isquemia, se sugirió tratamiento conservador, que consistió en pentoxifilina oral y terapia hiperbárica durante 10 días, lográndose una mejora significativa a los 4 meses de seguimiento.
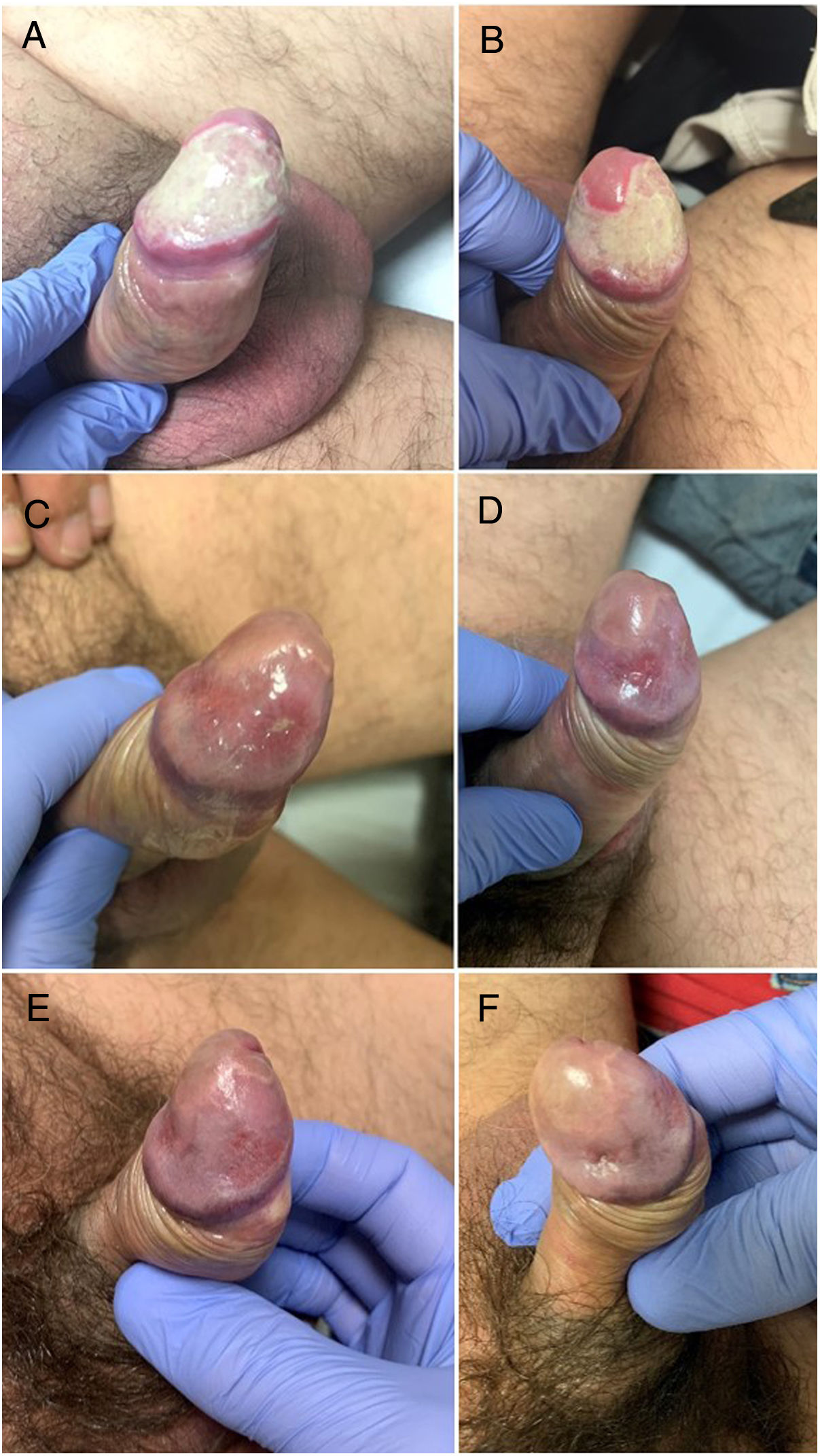
A 56-year-old male was admitted to our department with complaints of cold and painful glans penis. The patient had an infrapubic Coloplast Titan® Touch inflatable penile prosthesis (IPP) implanted by a high-volume implanter a month earlier. The procedure was uneventful, after corpora dilation up to 14mm, a 16cm IPP was inserted with satisfactory cylinder position, without corporal fibrosis or hematoma. Then, a 75 cc cloverleaf reservoir was placed in the space of Retzius through the left inguinal orifice (due to the intervention of the right inguinal hernioplasty), and a mummy wrap was applied to the scrotum and penile shaft. Patient was discharged with prosthesis partially inflated after 16-Fr latex Foley catheter removal on postoperative day 1. After 1 month, physical examination revealed the modified color and appearance on the right side of the glans, and then the prosthesis was completely deflated (Fig. 1A and B). His past medical history included: smoker of 25 cigarettes/day, diabetes mellitus, mastocytosis, hypertension, excessive alcohol intake, and a radical cystoprostatectomy 10 months ago.
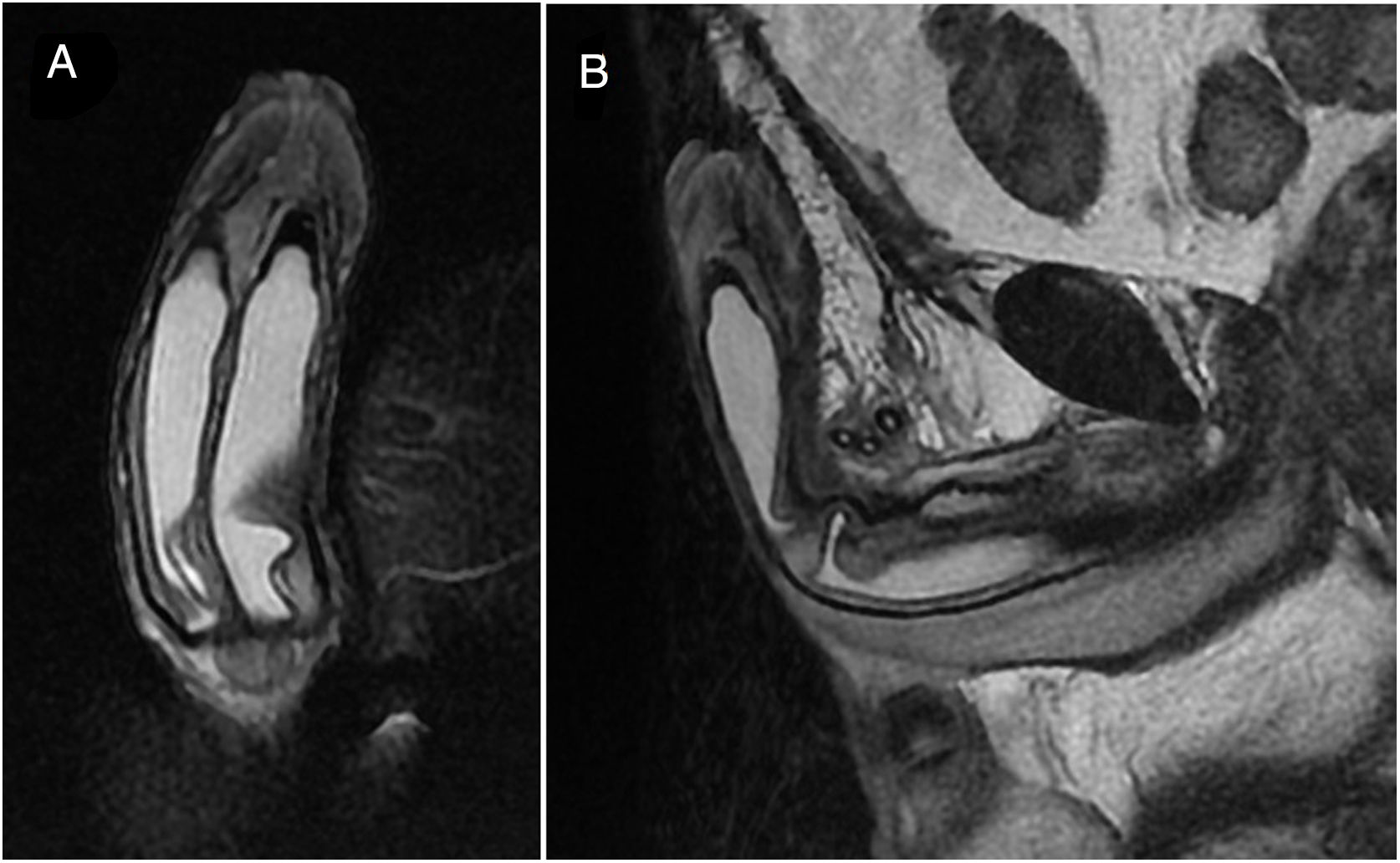
To assess the precise extent of the penile damage gray-scale and color Doppler sonographic examination was performed. Color Doppler examinations revealed the normal intracavernosal arteries with no vascularity in the superficial glans tissues. A pelvic MRI was performed checking the correct placement of the prosthesis cylinders without other signs of complication (Fig. 2A and B). A diagnosis of superficial glans ischemia was suggested and agreeing with the patient, a conservative treatment approach was recommended. Treatment started immediately with a 400mg twice daily oral pentoxifylline (PTX) and hyperbaric therapy (HT) 2.4 atmospheres 1h daily for 10 days. At 2 months of follow-up, there was a significant improvement in the appearance of the glans and symptoms referred by the patient (Fig. 1C and D), which continued to improve in the visit at 4 months follow-up (Fig. 1E and F).
DiscussionIschemia of the glans penis is rare and may result from trauma, vasoactive drugs, diabetes, vasculitis, penile strangulation, or foreign bodies.1 It is also described after circumcision, prostatic artery embolization,1 penile length and girth restoration procedures,2 and penile prosthesis implantation.3,4 Most commonly encountered complications after penile prosthesis implantation include mechanical failure, infection, erosion, and pump and reservoir complications. Glandular ischemia is an extremely uncommon dreaded postoperative complication of inflatable penile prosthesis (IPP) surgery that may lead to penile gangrene and organ loss, whose incidence is difficult to determine. Preoperative risk factors included atherosclerosis (90%), diabetes mellitus (81%), smoking (81%), previous IPP explantation (57%), and previous radiation therapy (48%).3 The most prevalent intraoperative and postoperative factors reported are subcoronal incision (86%), penile wrapping with an occlusive bandage (62%), use of sliding technique (33%), and coincident distal urethral injury repair (29%).3 Arterial blood supply to the penis originates from the external and internal pudendal arteries. Corporal dilation obliterates cavernosal artery, leaving glans perfusion to the dorsal and bulbourethral arteries branches of the internal pudendal artery. The intrinsic compressive forces from intracorporal inflated cylinders and Foley catheter combined with extrinsic pressure from a penile wrap or subcoronal hematoma lead to an ischemic effect on the end arteries of the glans penis.
The outcome of this complication ranges from transient skin ischemia and glans gangrene to penile amputation depending on the depth and on the severity of damage.5 In nearly all the cases of penile ischemia, prosthesis had to be removed, however, several cases reported success with conservative treatment. So, Migliorini et al.,6 treated successfully acute glans ischemia with hyperbaric therapy (HT) and PTX. HT enhances the amount of oxygen bound to hemoglobin and free in blood, thus increases the oxygen supply in hypoxic tissues and enhances the production of reactive oxygen and nitrogen species.7 On the other hand, PTX is a non-selective phosphodiesterase inhibitor that improves peripheral blood flow by reducing whole blood viscosity.6 Moreover, the combination of HT with PTX seems to have a synergistic effect.8 Other successful results have also been described by other authors with this conservative treatment,9,10 and others11–13 including topical testosterone, enoxaparin, antiplatelet, corticosteroids, and iloprost.
Glans ischemia after IPP implantation is very uncommon. In our case, several possible risk factors may have triggered the presence of glans ischemia, such as the fact that the patient was diabetic, in addition to presenting mastocytosis14 (a link between mast cell-mediated allergic reactions and cardiovascular disorders has been recently proposed). Moreover, the infrapubic approach to the placement of the penile prosthesis, which could increase the risk of small iatrogenic arterial lesions by exposing the dorsal neurovascular bundle. As our patient showed superficial non-necrotic glans ischemia, salvage management was attempted.
ConclusionGlans ischemia after IPP implantation is rare. In some selected cases, conservative management can be attempted before considering the removal of the device. Patients who are at risk for compromised blood flow to the glans should avoid high-risk concomitant surgical maneuvers during IPP.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Conflict of interestNone.