Menopause refers to the permanent cessation of menstruation resulting from the loss of ovarian activity. Studies have shown that menopause has an impact on the life quality of women as well as their sexual function. In this study, we sought to characterise the differences in the sexual function of women with iatrogenic menopause and those with natural menopause.
MethodsData were collected from 300 women in this study. The Symptom Check List and the Female Sexual Function Index were the main data collection instruments. Forty-eight patients with a Symptom Check List score ≥0.5 were not included in the study. Therefore, we enrolled a cohort of 252 menopausal women at a tertiary care setting in Turkey. The independent sample t-test, one-way analysis of variance, Pearson correlation and logistic regression analysis were used in this study and p value of <0.05 was considered statistically significant.
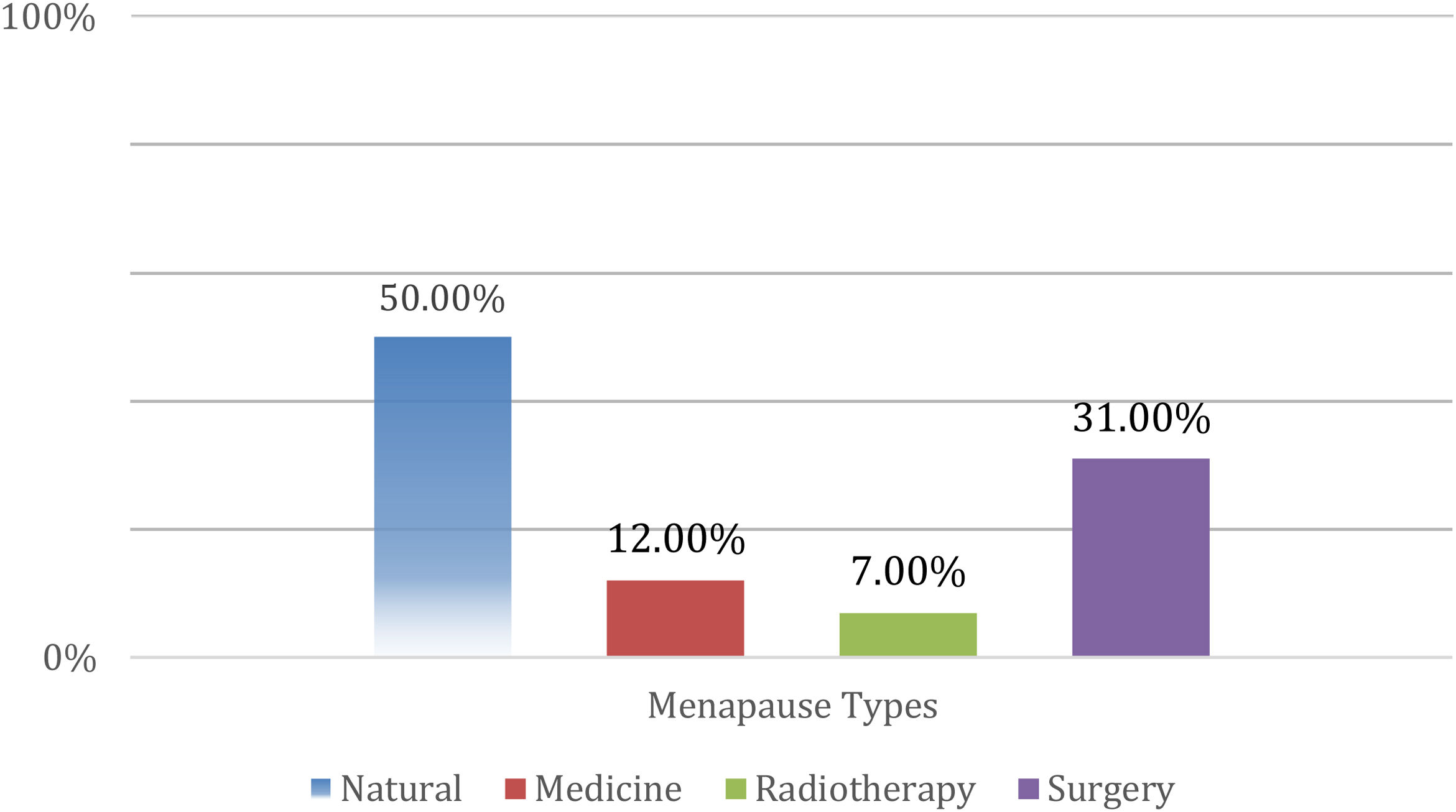
ResultsIn our study, menopause women were divided into two equal groups based on the type of menopause (natural vs. iatrogenic). The iatrogenic group was further divided into 3 sub-groups; drug-induced 30 (12%), radiotherapy-induced 18 (7%) and surgical 78 (31%). No significant difference in sexual function between groups were observed with respect to mean scores for desire, arousal, lubrication, orgasm, satisfaction, pain and sexual function (p>0.05).
ConclusionsOur results suggest that sexuality-specific problems during menopause are multifactorial and not solely attributable to biological or psychological factors. Our findings call for comprehensive interventions to address the psychological and biological effects of menopause in order to improve the life quality of women.
La menopausia se refiere al cese permanente de la menstruación como resultado de la pérdida de la actividad ovárica. Los estudios han demostrado que la menopausia tiene un impacto en la calidad de vida de las mujeres, así como en su función sexual. En este estudio, buscamos caracterizar las diferencias en la función sexual de las mujeres con menopausia iatrogénica y aquellas con menopausia natural.
MétodosSe recopilaron datos de 300 mujeres en este estudio. La lista de verificación de síntomas y el índice de función sexual femenina fueron los principales instrumentos de recolección de datos. Cuarenta y ocho pacientes con una puntuación de la lista de verificación de síntomas ≥0,5 no fueron incluidas en el estudio. Por lo tanto, inscribimos una cohorte de 252 mujeres menopáusicas en un entorno de atención terciaria en Turquía. En este estudio se utilizó la prueba t de muestra independiente, el análisis de varianza unidireccional, la correlación de Pearson y el análisis de regresión logística, y se consideró estadísticamente significativo un valor de p<0,05.
ResultadosEn nuestro estudio, las mujeres con menopausia se dividieron en dos grupos iguales según el tipo de menopausia (natural versus iatrogénica). El grupo iatrogénico se dividió en tres subgrupos: inducida por fármacos 30 (12%), inducida por radioterapia 18 (7%) y quirúrgica 78 (31%). No observamos ninguna diferencia significativa en la función sexual entre los grupos con respecto a las puntuaciones medias de deseo, excitación, lubricación, orgasmo, satisfacción, dolor y función sexual (p>0,05).
ConclusionesNuestros resultados sugieren que los problemas específicos de la sexualidad durante la menopausia son multifactoriales y no solo atribuibles a factores biológicos o psicológicos. Nuestros hallazgos requieren intervenciones integrales para abordar los efectos psicológicos y biológicos de la menopausia a fin de mejorar la calidad de vida de las mujeres.
Menopause refers to the permanent cessation of menstruation resulting from the loss of ovarian activity. Owing to prolonged life expectancy, women spend almost one-third of their lives in the postmenopausal phase with physical, mental and social changes that require adaptation.
Studies have shown that menopause has an impact on the life quality of women as well as their sexual function.1 Sexuality is one of the key determinants of the life quality and general health. Sexual dysfunction is a complex issue that is affected by several biological, psychological and individual factors. Female sexual dysfunction is described in the DSM-IV-TR (Diagnostic and Statistical Manual of Mental Disorders) as a distressing condition characterised by desire disorder and psychophysiological changes in the sexual cycle.2
Hormone level changes, psychological disorders and physical disorders are the main causes of sexual dysfunction in menopausal women.3 These changes related to sexuality have psychological, physical and anatomical effects. Besides the psychological effects, oestrogen deficiency directly affects sexual intercourse by causing atrophy and dryness of the vaginal epithelium. Sexual ageing decreases blood flow and secretions in the vagina and cervix as well as leads to a decrease in sexual arousal and intercourse frequency.4
Studies have shown that behavioural and couple therapies or treatments, such as lubricants and local oestrogen therapy, may help improve sexual function during this period.5
Owing to the decrease in hormone levels, depression and anxiety are particularly common during menopause.6 Although some women consider menopause as a natural process of life, most women perceive it as a distressing and life-changing event. Therefore, this behavioural disorder negatively affects sexual satisfaction.7
Menopause can occur naturally or as a result of treatment administered for various reasons. When natural menopause is compared to iatrogenic, natural menopause is caused by depletion of follicles, whereas, iatrogenic is caused by external interventions to stop ovarian functions, regardless of age. Particularly, oophorectomy, radiotherapy and some chemotherapeutic agents used for treatment of gynaecological or non-gynaecological malignancies may cause iatrogenic menopause. Furthermore, women who develop iatrogenic menopause as a result of surgical interventions (such as hysterectomy and bilateral oophorectomy) or other treatments are more likely to experience psychological issues, such as anxiety and depression, and negative effects related to sexual life; in addition, they may exhibit more severe symptoms and have reduced body image and self-esteem.8
The aim of this study was to assess whether there is a difference in sexual function of women with natural menopause and compare it with those with iatrogenic menopause (due to surgery, medicine or radiotherapy). Our findings may help inform supportive interventions for women who are at risk of iatrogenic menopause to mitigate its adverse effects.
Materials and methodsPatient selectionOverall, 300 sexually active menopausal women who were not menstruating for at least 1 year and who visited the Gynaecology and Obstetrics outpatient clinic between 1st March 2019 to 2nd March 2020 were included in the survey study. The study was approved by the Institutional Review Board (20th February 2019/87). Written informed consent was obtained from all subjects prior to their enrolment. Age, cause of menopause (surgery, medication or radiotherapy), duration of menopause and questionnaire responses of the participants were recorded using the case form.
Exclusion criteriaSexually inactive women, women with comorbidities (hypertension, diabetes, coronary artery disease, etc.), women with ‘Symptom Check List (SCL-90)’ score of ≥0.5 and women who failed to answer at least one question in the ‘Female Sexual Function Index (FSFI)’ questionnaires were excluded from the study.
Symptom Check List (SCL-90)Women who volunteered to participate in the study were asked to complete the SCL-90 questionnaire consisting of 90 items. This scale is a tool used to determine the presence and severity of psychological symptoms in an individual. All participants first completed the SCL-90 questionnaire. Participants with a score of ≥0.5 were recommended psychiatric consultation at the outpatient clinic and were excluded from the study. Those with a score of <0.5 were asked to complete the FSFI questionnaire.
Female sexual function indexFemale sexual dysfunction is characterised by sexual pain, impaired sexual desire, sexual arousal, orgasm, lubrication and/or satisfaction. FSFI is a Likert type scale that evaluates sexual dysfunction in women using 19 items. It consists of six sub-categories: desire, arousal, lubrication, orgasm, satisfaction and pain. Each sub-category is scored on a scale of 0–5. Women with an FSFI score of ≤26.5 are considered to have female sexual dysfunction.
After all these evaluations, the subjects were divided into two groups: iatrogenic menopause and natural menopause.
Statistical analysesAll analyses were performed using the SPSS 20 program. Frequency analysis was performed, and descriptive statistics related to demographic variables were generated. Between-group differences were assessed using the independent sample t-test; one-way analysis of variance was used to compare three or more groups. In addition, the relationship between sexual function and its sub-categories was examined using Pearson correlation analysis. Finally, logistic regression analysis was performed to investigate the effect of sexual function sub-categories on menopause type. p value of <0.05 was considered statistically significant.
ResultsData were collected from 300 women in this study. Forty-eight patients with an SCL-90 score ≥0.5 were not included in the study. Therefore, a total of 252 women were included in the analysis.
As shown in Fig. 1, 126 (50%) out of 252 women had natural menopause, whereas the remaining 126 women had iatrogenic menopause; of these, 78 (31%) had iatrogenic menopause due to surgery, 30 (12%) due to medication and 18 (7%) due to radiotherapy. Women with natural menopause accounted for the highest proportion of subjects, whereas those with radiotherapy-induced menopause accounted for the lowest proportion of subjects.
The mean age of women in the natural and iatrogenic menopause groups was 52.30±4.73 years and 51.10±4.96 years, respectively; there was no significant between-group difference in this respect (p>0.05). However, the mean duration of menopause in the natural menopause group (4.39±3.707) was significantly shorter than that in the iatrogenic menopause group (6.09±3.962) (p=0.001).
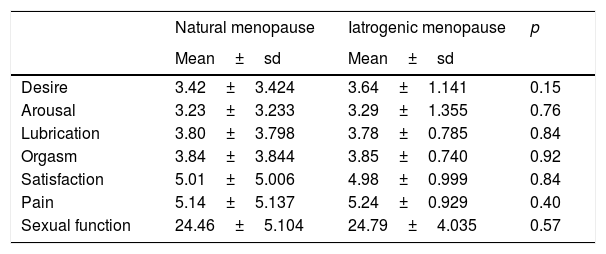
The sub-category measurements in the natural menopause group and the iatrogenic menopause group were investigated. No significant between-group differences were observed with respect to mean scores for desire, arousal, lubrication, orgasm, satisfaction, pain, or sexual function (p>0.05) (Table 1).
Sexual function parameters of women in the natural and iatrogenic menopause groups.
| Natural menopause | Iatrogenic menopause | p | |
|---|---|---|---|
| Mean±sd | Mean±sd | ||
| Desire | 3.42±3.424 | 3.64±1.141 | 0.15 |
| Arousal | 3.23±3.233 | 3.29±1.355 | 0.76 |
| Lubrication | 3.80±3.798 | 3.78±0.785 | 0.84 |
| Orgasm | 3.84±3.844 | 3.85±0.740 | 0.92 |
| Satisfaction | 5.01±5.006 | 4.98±0.999 | 0.84 |
| Pain | 5.14±5.137 | 5.24±0.929 | 0.40 |
| Sexual function | 24.46±5.104 | 24.79±4.035 | 0.57 |
Data presented as mean±standard deviation.
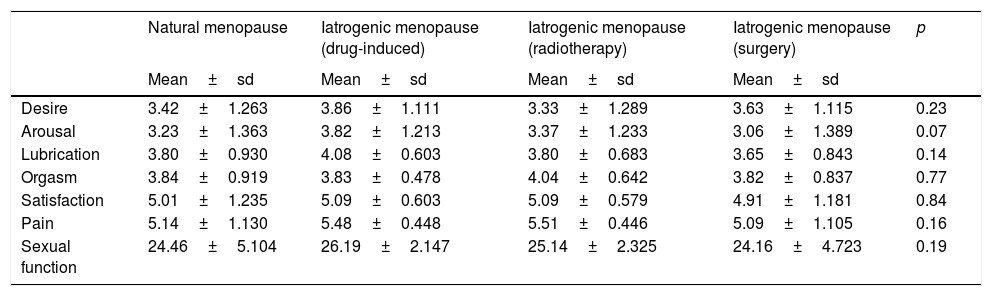
There was no significant difference between iatrogenic menopause types with respect to desire, arousal, lubrication, orgasm, satisfaction, pain, or sexual function values (p>0.05) (Table 2).
Sexual function parameters of women in subgroups disaggregated by cause of menopause.
| Natural menopause | Iatrogenic menopause (drug-induced) | Iatrogenic menopause (radiotherapy) | Iatrogenic menopause (surgery) | p | |
|---|---|---|---|---|---|
| Mean±sd | Mean±sd | Mean±sd | Mean±sd | ||
| Desire | 3.42±1.263 | 3.86±1.111 | 3.33±1.289 | 3.63±1.115 | 0.23 |
| Arousal | 3.23±1.363 | 3.82±1.213 | 3.37±1.233 | 3.06±1.389 | 0.07 |
| Lubrication | 3.80±0.930 | 4.08±0.603 | 3.80±0.683 | 3.65±0.843 | 0.14 |
| Orgasm | 3.84±0.919 | 3.83±0.478 | 4.04±0.642 | 3.82±0.837 | 0.77 |
| Satisfaction | 5.01±1.235 | 5.09±0.603 | 5.09±0.579 | 4.91±1.181 | 0.84 |
| Pain | 5.14±1.130 | 5.48±0.448 | 5.51±0.446 | 5.09±1.105 | 0.16 |
| Sexual function | 24.46±5.104 | 26.19±2.147 | 25.14±2.325 | 24.16±4.723 | 0.19 |
Data presented as mean±standard deviation.
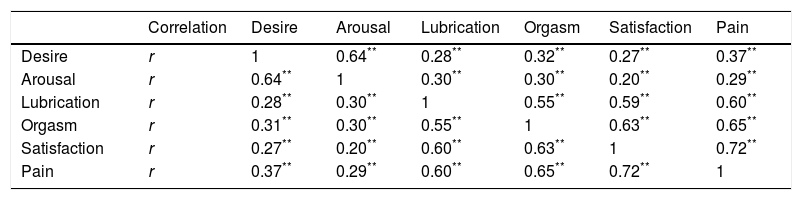
A significant positive correlation was observed between all sub-categories (p<0.01) (Table 3).
Correlation between sub-dimensions.
| Correlation | Desire | Arousal | Lubrication | Orgasm | Satisfaction | Pain | |
|---|---|---|---|---|---|---|---|
| Desire | r | 1 | 0.64** | 0.28** | 0.32** | 0.27** | 0.37** |
| Arousal | r | 0.64** | 1 | 0.30** | 0.30** | 0.20** | 0.29** |
| Lubrication | r | 0.28** | 0.30** | 1 | 0.55** | 0.59** | 0.60** |
| Orgasm | r | 0.31** | 0.30** | 0.55** | 1 | 0.63** | 0.65** |
| Satisfaction | r | 0.27** | 0.20** | 0.60** | 0.63** | 1 | 0.72** |
| Pain | r | 0.37** | 0.29** | 0.60** | 0.65** | 0.72** | 1 |
Of the 252 women included in the study, 174 (69%) women with an FSFI total score ≤26.55 were examined. Of these, 86 (49.4%) were in the natural menopause group and 88 (50.6%) were in the iatrogenic menopause group. There were no significant differences between the groups with respect to sexual function and mean scores for desire, arousal, lubrication, orgasm, satisfaction, or pain (p>0.05).
Out of 78 (31%) women with an FSFI total score >26.55, 40 (51.3%) were in the natural menopause group and 38 (48.7%) were in the iatrogenic menopause group. There were no significant differences between the groups with respect to sexual function and mean scores for desire, arousal, lubrication, orgasm, satisfaction, or pain (p>0.05).
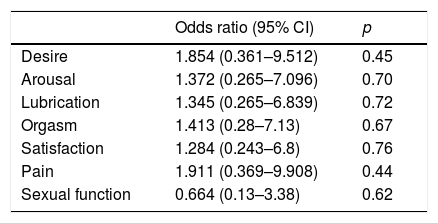
The effect of sexual function and its sub-categories on menopause was examined by logistic regression analysis. None of these variables showed a significant effect on menopause (p>0.05) (Table 4).
Effects of sexual function and sub-categories to menopause patients with logistic regression analysis.
| Odds ratio (95% CI) | p | |
|---|---|---|
| Desire | 1.854 (0.361–9.512) | 0.45 |
| Arousal | 1.372 (0.265–7.096) | 0.70 |
| Lubrication | 1.345 (0.265–6.839) | 0.72 |
| Orgasm | 1.413 (0.28–7.13) | 0.67 |
| Satisfaction | 1.284 (0.243–6.8) | 0.76 |
| Pain | 1.911 (0.369–9.908) | 0.44 |
| Sexual function | 0.664 (0.13–3.38) | 0.62 |
CI; confidence interval.
Tabachnick, B.G. & Fidell, L.S. (2013). Using Mutivariate Statistics (6th Edition). Boston: Pearson.
The life span of a woman consists of five distinct phases: childhood, adolescence, sexual maturity, menopause and old age. Owing to increased life expectancy, the postmenopausal period covers approximately one-third of a woman's life. Although there is considerable inter-individual variability in this respect, menopause generally occurs between the age of 45 and 55 years. The physiological, mental, cultural and sexual implications of menopause tend to adversely affect the quality of life.9 These adverse effects are typically more severe in case of iatrogenic menopause and menopause caused by environmental factors.
A study documented high rate of sexual dysfunction among peri-menopausal Turkish women; in addition, there was a negative correlation between sexual dysfunction and the quality of life scores.10 In a previous study, sexual problems and orgasmic disorders in women aged >40 years were more common for Asian women compared to Europeans.11 This finding illustrates the impact of ethnicity on sexual function. The psychological, anatomical and physical effects of menopause inevitably affect the sexual life of women. Moreover, the psychological effects of menopause may in turn induce sexual dysfunction. Therefore, of the 300 menopausal women included in the present study, 48 women with a SCL-90 score ≥0.5 were excluded from the study and referred to a psychiatric outpatient clinic. Only 252 women were included in the analysis.
Iatrogenic menopause is known to be more frequently associated with psychological problems such as anxiety and depression. These women also tend to experience more negative effects related to sexual life, exhibit more severe symptoms and have reduced body image and self-esteem.8
Three-quarters of all peri menopausal women and one-half of all postmenopausal women experience one or more sexual problems.12 In a study, approximately 10%–15% of peri-menopausal women reported a lack of sexual desire and <5% were unable to reach orgasm.13 In another study, >60% of postmenopausal women reported loss of sexual desire, inability to reach orgasm and lack of pleasure from sex.14 Apart from natural menopause, iatrogenic causes that induce a hypoestrogenic state may also cause sexual dysfunction. The main underlying cause in this group is the sudden decrease in the production of oestrogen and androgen.15,16 Especially in this younger group with longer menopause period, the effects of early menopause are more severe in the absence of hormone therapy.17
In the present study, the mean age of women in the natural and iatrogenic groups was comparable. However, the mean duration of menopause in the natural menopause group was significantly shorter than that in the iatrogenic menopause group. This shows that menopausal stage due to iatrogenic causes was longer in the present study.
Several studies have examined the causes of iatrogenic menopause. In a study, women who used chemotherapeutic agents more frequently experienced sexual problems such as decreased sexual interest, decreased vaginal lubrication, inability to reach orgasm and dyspareunia.18 On the other hand, radiotherapy was reported to indirectly affect sexuality and cause sexual dysfunction due to changes in body image, pain, fatigue, cessation of ovarian function, irreversible sterility and vaginal dryness.19 Studies have also examined the effect of surgical treatment on sexuality. In women with surgically-induced menopause, surgery was found to adversely affect body image, self-esteem and sexual health status, regardless of the type of surgical intervention. Moreover, the age of women with surgical menopause was lower than that of women with natural menopause, and although follicle depletion occurred progressively in natural menopause, the symptoms in surgical menopause were acute and more severe without a transition period.20
In another study, spontaneous, surgical and premature menopauses lead to decrease intercourse frequency. Additionally, it was found that surgical menopause increase the risk of sexual dysfunction when compared to spontaneous and premature menopause.10 In a large study of 1805 postmenopausal women, 34% women reported reduced sexual desire and 54% reported decreased sexual interest.21 In another study vaginal atrophy and dryness in postmenopausal women was found to induce erectile dysfunction in partners, which had a negative effect on their relationship.22
In the present study, 174 (69%) women had sexual dysfunction according to the FSFI total score. Of these, 86 (49.4%) had natural menopause and 88 (50.6%) had iatrogenic menopause. According to the FSFI, there was no significant difference between the groups with respect to sexual function, desire, arousal, lubrication, orgasm, satisfaction and pain (p>0.05). We also compared the natural and iatrogenic menopause groups and the various iatrogenic menopause subgroups; contrary to other studies, we observed no significant differences (p>0.05). Although there were no significant between-group differences, the fact that the majority of the subjects had sexual dysfunction illustrates the importance of sexuality on the quality of life in the postmenopausal period. Developing preventive interventions against the widespread perception that sexuality is not a priority in this stage of life is a key imperative. In addition, education and counselling to influence personal attitudes and beliefs in this respect are also required.
Furthermore, it is our conviction that menopause-specific problems are not only biological; detailed evaluation and appropriate counselling of individuals during the premenopausal phase may help increase sexual satisfaction and improve the life quality.
The absence of a significant difference between the causes of menopause in the present study suggests a need for more comprehensive causal studies to understand the multifaceted nature of sexual dysfunction in menopausal women.
Furthermore, a detailed comparison should be executed by grouping the women with iatrogenic and normal menopause based on their menopause durations recorded at the beginning of the menopause, to understand the effect of time over menopause type.
One of the limitations of the current study is the application of questionnaires in a single tertiary centre and inclusion of only group of low and medium social cultural levelled menopausal women. Larger, multi-centre studies with a more representative sample may help provide more definitive evidence. Another limitation is the lack of detailed evaluation of other factors that may affect sexual dysfunction, i.e., sociocultural status, educational status, educational status at the time of transition into menopause, information concerning their partners, as well as other factors such as age, cause of menopause, menopause duration and psychological state of individuals.
ConclusionsIn the present study, we sought to characterise the multifaceted causes of sexual dysfunction in Turkish menopausal women. By excluding psychiatric causes, we examined the biological causes according to the modes of transition to menopause and its effects on sexual function. We did not observe any significant difference between the groups. Our results suggest that sexuality-specific problems during menopause are not solely of biological or psychological origin. We believe that many causes such as the preparation process, sociocultural factors, education level, partner solidarity and ethnicity should be evaluated in detail during menopause. Women tend to perceive that their body image will diminish, their feminine functions will end and their sexual attraction will disappear because of menopause. Our findings call for comprehensive interventions to address the psychological and biological effects of menopause in order to improve the life quality of women.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Author contributionsAysegul Gulbahar was responsible of writing-original draft, conceptualisation and methodology of the manuscript.
Seda Akgun Kavurmaci contributed writing-review & editing and validation of the manuscript.
Conflict of interestThe authors declare that they have no conflict of interest.
The authors thank, MD Duru Saygín Gulbahar for the advisory about the surveys included in the study and assistance for the preparation of the manuscript.