Partial thrombosis of corpus cavernosum is an uncommon condition that needs a high level of suspicious to be diagnosed. Imaging techniques may be very useful, and MR is the state-of-the-art technique. We present a case of a young male who presented to the emergency department with perineal and painful mass. MR imaging clearly depicted a thrombosed corpus cavernosum and a bilateral membrane that is possibly the underlying predisposing condition. With only conservative treatment the patient had an excellent outcome.
La trombosis parcial del cuerpo cavernoso es una rara entidad que necesita de un alto grado de sospecha para su diagnóstico. Las técnicas de diagnóstico por la imagen pueden ser de gran utilidad y la resonancia magnética (RM) es la mejor modalidad disponible. Presentamos el caso de un joven varón que acude al servicio de urgencias con una masa perineal dolorosa. La RM diagnostica trombosis del cuerpo cavernoso y la existencia de una membrana bilateral, un posible factor predisponente. Con apenas tratamiento conservador, el paciente tuvo una excelente evolución clínica.
Partial thrombosis of the corpora cavernosa is a rare entity, also known as “partial segmental thrombosis of the corpus cavernosum” or even as “idiopathic partial thrombosis of corpus cavernosum”.
It occurs mainly in young men, as a painful perineal mass.
Despite its unclear aetiology, the presence of a transverse membrane on the proximal portion of the corpus cavernosum (CC) seems to be one important triggering factor. Such membrane can be easily diagnosed using MR images, providing a prompt diagnosis of condition and cause.
Case reportA 30-year-old male, with no past medical history of interest, presents to the emergency department complaining of perineal tenderness in the last 3 days. Urinary symptoms such as polachiuria and vesical tenesmus were also present. There is no fever, nausea or vomiting and no complains about erectile dysfunction. At physical examination, a stiff and painful mass in the left perineal region of approximately 6×3cm was identified, with tenderness around the left scrotum and at the penis base. There were no signs of priapism. Blood tests and urine analysis were unremarkable. With the initial diagnosis of a perineal mass, the patient was remitted to MR study for further characterization.
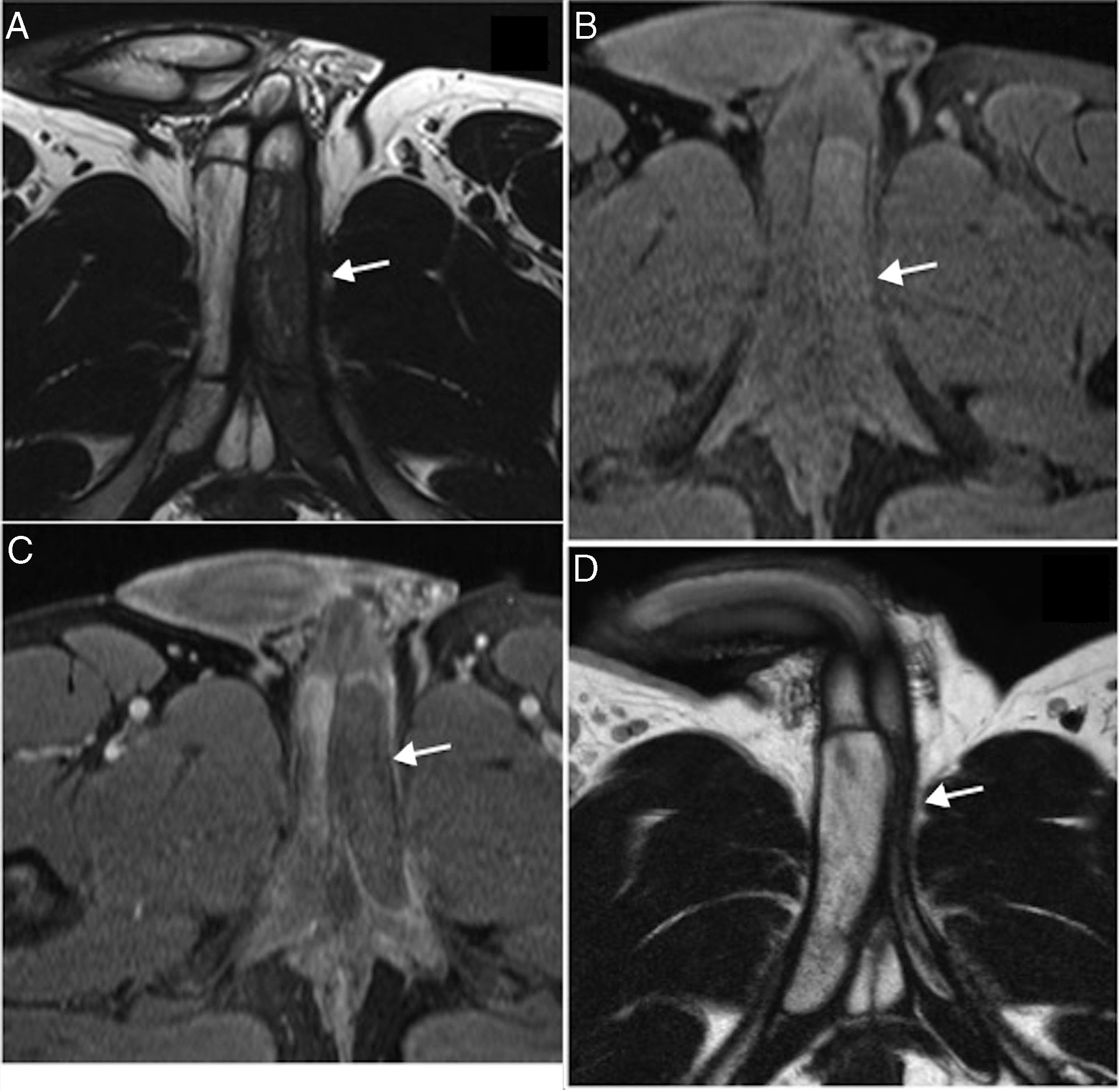
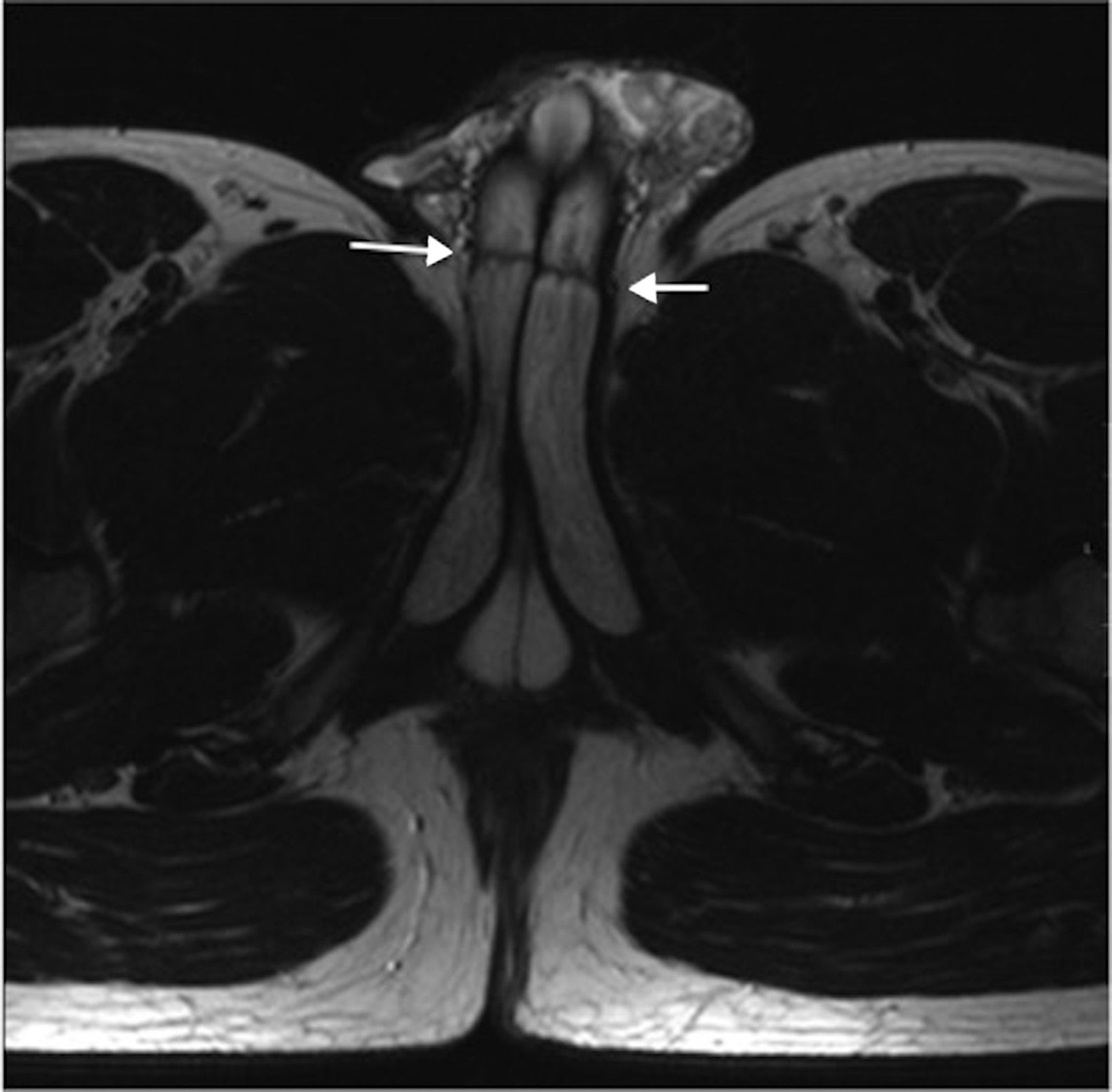
At MR there was a diffuse thickening of the left corpus cavernosum (CC), approximately 8cm long, extending from the crura to the mid portion of the penis. It was hypointense in T2 weighted images and slightly hyperintense in T1 weighted images, with no enhancement after intravenous gadolinium-based contrast administration, as opposed to the right normal CC (Fig. 1). In the distal extremity of the thrombosed CC and at same level on its contralateral, a thin hypointense stripe was seen in both CC consistent with a membrane (Fig. 2). Erection was not inducted with intracavernous prostaglandin injection. There were no other relevant findings.
MR imaging. At diagnosis, T2 weighted axial imaging (A) shows a left corpus cavernosum (CC) hypointense in comparison with its contralateral (arrow). Same image in T1W (B) shows a slightly hyperintense CC (arrow). (C) Post-gadolinium administration axial imaging shows no contrast enhancement in the left CC (arrow). In a 2 years control (D), T2W axial images shows an atrophic left CC (arrow).
With such MR findings and clinical data, the diagnosis of thrombosis of the left corpus cavernosum was made and the patient was treated with 100,000IU of low-molecular weight heparin during the following 6 weeks.
The patient was remitted for hematologic assessment, and genetic tests revealed he was heterozygotic for the G1691A mutation, which is associated with Factor V Leiden. Such mutation carries only a small increase in the risk of thrombosis and did not changed its clinical management.
In MR follow-ups, images showed a progressive resolution of the left thrombosed CC, which showed a volume loss probably secondary to atrophy (Fig. 1D).
At 3 years follow-up, the patient refers no erectile dysfunction, is free of symptoms and a MR control shows no recurrence.
DiscussionPartial thrombosis of corpus cavernosum is a rare condition with an unclear aetiology. It was formerly named as partial priapism after the rigidity of the CC.1 Nevertheless, these two entities differ because unlike in priaspim, in partial thrombosis only the proximal portion of CC is affected; therefore the distal portion of the penis is flaccid.
It is reported to occur mainly in young men with a 30 year old mean age, many of which have a previous history of microtrauma, such as cyclists, oncologic conditions or some coagulability disorder,2 which is believed to be one of the triggers in our patient.
Clinically, it presents as a perineal mass, which is painful, and may be associated with other symptoms such as erectile dysfunction.3 The presence of urinary symptoms is also reported,1,4–6 and although there is not a clear explanation, we believe that it may be due to the mass effect of the thrombosed CC on neighbour structures. It usually is a unilateral condition, although there a few cases reported as bilateral thrombosis.1
Imaging techniques can be of great help in diagnosing such conditions. Doppler ultrasound is readily available, and may be diagnostic when able to depict changes in volumen, echogenicity and an absent vascular flow inside the CC.7,8 The drawbacks are that it may not depict the membrane and its dependence on the operator: the lack of experience may greatly impair its performance. In our case, the patient was not studied with ultrasound because of the initial diagnosis of a tumour. In the other hand, CC thrombosis is easily seen in MR images. A technique that lacks ionizing radiation, is increasingly available, and also allows excluding others conditions such as tumours, Peyronie disease, and penile fracture. Typical and easily spotted imaging features are: an increase in CC volume that may displace the contralateral CC; a change in its MR signal, classically hypointense in T2W images and hyperintense in T1; lack of contrast-enhancement.4 The presence of a hypointense membrane can be the clue to the diagnosis and to propose the aetiology of the thrombosis.1 In most cases reported, such membrane was seen only in the thrombosed CC. Yet, in our patient we clearly identified the membrane bilaterally, as in a few previous reports.9,10 We could not find in the literature reports regarding the incidence of this membrane, nevertheless it s consistently mentioned in CC thrombosis reports. Its aetiology is not well defined, but is believed to be congenital either post-traumatic, and has been studied histologically only in a few cases, revealing fibrous connective tissue.11 We believe that if clinically suspected such patients must be studied with MR, as the membrane may be very difficult to see with ultrasound, and its presence carries prognostic value and should require prophilatic measures.1
It should stay clear that this condition does not mean an urologic emergency and that it can be treated in a non-preferential way. Historically, it was treated with surgical interventions, such as surgical corporotomy and clot evacuation, or perineal exploration with heparin irrigation of the CC. Although, the last reports show a change on its management, clearly supporting a conservative management mostly based on the administration of anticoagulants, leaving surgical approach only to those complicated and refractory cases.2,12-14
Clinical outcome usually shows a good prognosis, with almost no recurrence reported. Yet, some patients do complain of erectile dysfunction at long-term outcome.
ConclusionA high-suspicious rate may be needed to request further study for those patients with a possible diagnosis of corpus cavernosum thrombosis, which seems to be more frequent than previously stated. MR images are very helpful in this setting and its increasing availability can help in clearly diagnosing and treating such patients.
Financial supportNone.
Conflict of interestsThe authors declare no conflict of interests.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.